Abstract
Fibrovascular polyps (FVPs) of the esophagus are rare, and their course is usually indolent until reaching enormous proportions. It is a dramatic entity owing to its tendency to cause bizarre complications. We describe a 49-year-old female patient with sudden dyspnoea that required digital maneuvers to clear the airway. After diagnosing, an FVP of the esophagus, a video-assisted endocavitary surgery was made. Histopathological examination revealed a fibrovascular polyp. Endoscopic controls after excision show no mass or symptoms recurrence.
1. Introduction
Fibrovascular polyps (FVPs) of the esophagus are benign, rare, intraluminal tumors [1–8] and represent less than 2% of esophageal tumors [1–3, 5–7]. The most common complaints include dysphagia, foreign body sensation, weight loss, regurgitation of the mass, sudden death, and asphyxiation when the polyp regurgitates and occludes the larynx [1–9].
2. Case Report
A 49-year-old female patient described an episode of sudden dyspnoea that required digital maneuvers to clear the airway. She described that during the maneuver a smooth mass was detached from the pharynx and swallowed. Similar episodes were repeated in two occasions. During examination a progressive dysphagia to solids was noted. No history of loss weight, cough, or hematemesis was noted. She had no comorbidity of interest.
A CT scan was performed revealing a soft tissue mass in the esophagus, extending from the level of the cervical esophagus to the lower esophagus with no clear relation to the esophagus wall.
The upper endoscopy showed a sausage-shaped mass obstructing the esophageal lumen, arising from the upper esophageal sphincter and ending 13 cm below (Figure 1).
Figure 1.
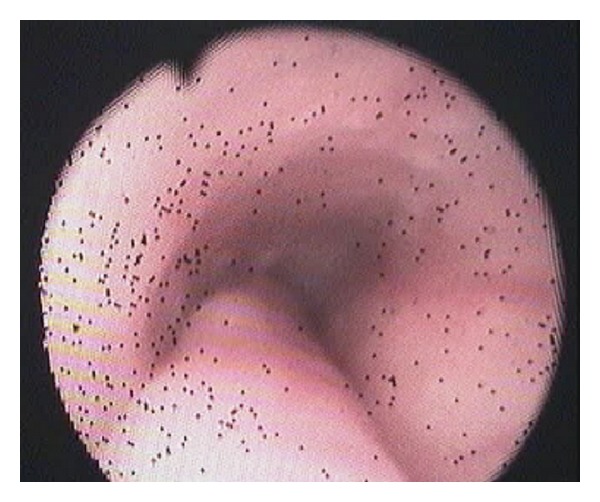
Sausage-shaped mass obstructing the esophageal lumen.
Technical Approach —
Tracheal intubation previous to upper endoscopy was made; the mass measured 13 × 1,5 cm and was sneared from his distal portion (Figure 2) and pulled into the mouth giving a clear image of the implantation base at the Killian's triangle. Once the distal portion of the tumor was fixed into the mouth and the base trapped by means of Kantrowitz forceps, the video-assisted endocavitary surgery started. The tumor was pulledby means of Magill forceps, and using laparoscopic surgical instrumentation and video assistance during the procedure the base of the tumor was electrocoagulated with the hook right above the Kantrowitz forceps (Figure 3) providing a clear control of possible hemorrhage (Figure 4). Immediate endoscopy was performed looking for possible complications of the procedure with negative results.
Twenty-four hours later the patient was able to eat soft meals and 48th hours after the procedure she was discharged.
Histopathological examination revealed a polypoid lesioncoveredbysquamous epithelium withacanthosis liningedematousstromawith areas offibrosis.Blood vessels andabundantlymphoplasmacytic infiltrate (Figure 5), concluding fibrovascular polyp.
Endoscopic controls were made 4 months and 24 months after excision with no mass or symptoms recurrence.
Figure 2.
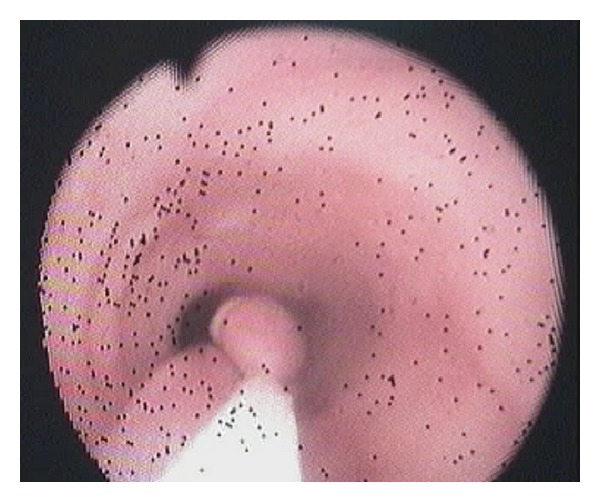
Sneared mass from his distal portion.
Figure 3.
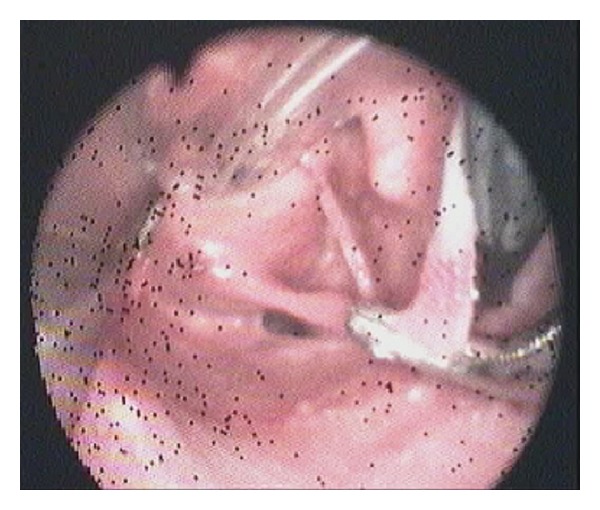
Base of the tumor electrocoagulated.
Figure 4.

Sausage shaped mass after sugery.
Figure 5.
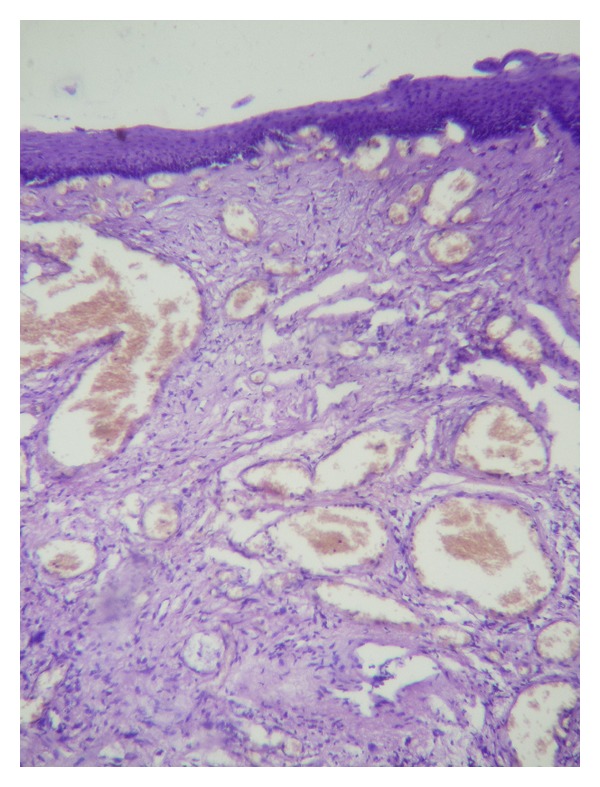
Polypoid lesion covered by squamous epithelium with acanthosis lining edematous stroma with areas of fibrosis. Blood vessels and abundant lymphoplasmacytic infiltrate.
3. Discussion
Despite its benign condition, it has a life threatening feared complication. This is an unusual tumor and different approaches have being proposed, including transverse cervical incision, transoral resection under direct visualization, endoscopic ligation and electrocoagulation of the pedicle (small size FVP), biapproach surgical technique (eoesophagostomy plus gastrostomy) and CO2 laser under laryngoscope [1–9].
The novel technical approach that we propose includes the safety and accuracy of transverse cervical incision, the simplicity of an endoscopic procedure, scarless, with early discharge and recovery.
It is important to consider that if FVP has become giant, it means we have got late to the patient, and this may be either because the patient shows no complaints, or because its symptoms have not been studied enough due to their nonspecificity.
Conflict of Interests
The authors have no conflict of interests to disclose.
Acknowledgments
Special thanks to Fernanda Cúneo and Fernando Bazan from the library of Universidad Católica de Córdoba for helping with the database and Daniela Trakál with the syntax.
References
- 1.Wang J, Han DM, Ni X, Ma LJ, Ye JY, Xiao Y. Fibrovascular polyp of the hypopharynx and esophagus. Chinese Medical Journal. 2011;124(19):3182–3184. [PubMed] [Google Scholar]
- 2.Ozdemir S, Gorgulu O, Selcuk T, Akbas Y, Sayar C, Sayar H. Giant fibrovascular polyp of the hypopharynx: per-oral endoscopic removal. Journal of Laryngology and Otology. 2011;125(10):1087–1090. doi: 10.1017/S0022215111001034. [DOI] [PubMed] [Google Scholar]
- 3.Goenka AH, Sharma S, Ramachandran V, Chattopadhyay TK, Ray R. Giant fibrovascular polyp of the esophagus: report of a case. Surgery Today. 2011;41(1):120–124. doi: 10.1007/s00595-009-4212-5. [DOI] [PubMed] [Google Scholar]
- 4.Goto A, Suzuki M, Iizuka K, et al. Regurgitation of a mass into the mouth: a fibrovascular polyp of the esophagus. Endoscopy. 2010;42(supplement 2):E248–E249. doi: 10.1055/s-0030-1255618. [DOI] [PubMed] [Google Scholar]
- 5.Peltz M, Estrera AS. Resection of a giant esophageal fibrovascular polyp. Annals of Thoracic Surgery. 2010;90(3):1017–1019. doi: 10.1016/j.athoracsur.2010.02.049. [DOI] [PubMed] [Google Scholar]
- 6.Dutta R, Kumar A, Handa KK, Dinda AK. Large pedunculated fibrovascular polyp of oesophagus in a young woman. Interactive Cardiovascular and Thoracic Surgery. 2009;9(2):352–353. doi: 10.1510/icvts.2009.207696. [DOI] [PubMed] [Google Scholar]
- 7.Blacha MM, Sloots CE, Van Munster IP, Wobbes T. Dysphagia caused by a fibrovascular polyp: a case report. Cases Journal. 2008;1, article 334 doi: 10.1186/1757-1626-1-334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chourmouzi D, Drevelegas A. Giant fibrovascular polyp of the oesophagus: a case report and review of the literature. Journal of Medical Case Reports. 2008;2, article 337 doi: 10.1186/1752-1947-2-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chauhan S, Draganov P. Endoscopic removal of two giant fibrovascular polyps of the esophagus using the "two channel, two devices technique". Gastrointestinal Endoscopy. 2011;73(5):1036–1037. doi: 10.1016/j.gie.2010.11.026. [DOI] [PubMed] [Google Scholar]


