Summary
Background:
Distal femoral physis fractures with displacement are rare injuries seen in adolescents related with high incidence of complication. They may lead to premature physeal closure consequently, to growth arrest and bone deformity.
Case Report:
The case of a 14-year-old boy with Salter-Harris type II displaced fracture underwent surgery with open reduction has been described. CT examination with multiplanar reconstruction was used in pre-operative assessment of distal femur growth plate fracture.
Conclusions:
Knowledge of classification, prognosis and methods of treatment is necessary in accurate pre- and postoperative assessment of physial fractures in adolescents. CT and multiplanar reconstruction improve the understanding of patterns of injury, relative prevalence and accuracy of pre-operative planning.
Keywords: fracture, growth plate, femoral bone, classification
Background
Fractures of long bones in children are frequent traumas, often leading to the injury of the growth plate and, as a consequence, to potential severe complications. In practice, such fractures are most frequently diagnosed with a standard X-ray examination.
We presented the case of a 14-year-old boy with a diagnosed posttraumatic supracondylar fracture of the femoral bone, with lysis along the growth plate, and concomitant dislocation. The diagnosis was based on X-ray and CT examinations of the femoral bone. The aim of the case report was to make the target readers more familiar with the treatment methods and classification of growth plate fractures in children, as well as to show the usefulness of CT in preoperative planning.
Case Report
The injury occurred when the child was playing. The boys were jumping over the benches. Due to a fall from height, the boy suffered a right knee injury. An ambulance was called. After fixation of the right limb with the Kramer splint, the child was brought to the emergency room. Physical examination revealed a compulsory, flexed position of the right knee joint, in a 25-degree contracture, with a laterally dislocated inferior part of the femoral bone. The boy complained of a severe pain. No dysaesthesia or disorders of limb perfusion were found. The boy had an X-ray examination of the right femoral bone which revealed supracondylar fracture of the femoral bone with distal epiphysolysis of the right femoral bone, graded as type II fracture, according to the Salter-Harris classification. The medial condyle was chipped off and the distal end of the femoral bone was dislocated superiorly and laterally (Figures 1,2). CT examination of the right supracondylar femoral region and the right knee joint was performed, with subsequent postprocessing multi-planar reconstructions (MPR) of 2D images in frontal and sagittal planes, as well as 3D volume rendering – VR (Figure 3A–C).
Figure 1.

Radiograph performed on the day of trauma. Femoral bone axis dislocation.
Figure 2.

Lateral radiograph demonstrate unnormal placement of bones fragments.
Figure 3.
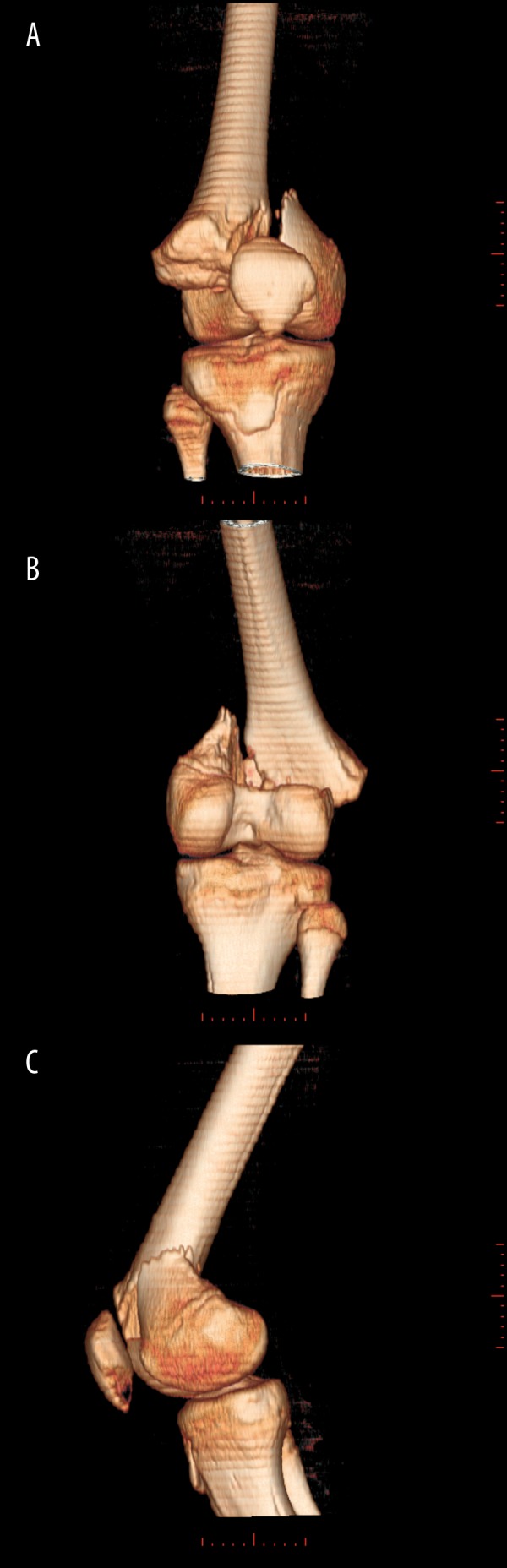
CT examination of right knee – volume rendering (VR) reconstruction. Frontal view (A), posterior view (B), lateral view (C).
CT revealed a supracondylar fracture of the right femoral bone. The fissure of the fracture was passing vertically, between the condyles, reaching the growth plate. The chipped off wedge-shaped fragment of the medial condyle did not change its location, but the femoral shaft with its lateral condyle dislocated along the growth plate, laterally and superiorly. The boy suffered type II Salter-Harris injury with distal epiphysolysis. He was admitted to the Orthopaedic Department where he underwent a reconstructive procedure: open reduction of the right femoral distal epiphysolysis and fixation with the use of 2 AO screws and the Kirschner wire.
A follow-up postoperative X-ray revealed a satisfactory surgical effect and restoration of a normal axis of the right femoral bone (Figure 4A,B). Subsequent follow-up studies, performed after 4 (Figure 5A,B) and 8 months (Figure 6A,B), confirmed the correct alignment of the limb axis and no significant postoperative complications.
Figure 4.
Anteroposterior (A) and lateral (B) radiographic view after operation demonstrate correct orientation of bones fragments.
Figure 5.
Anteroposterior (A) and lateral (B) radiographic views 4 months after operation. Kirschners pin was removed.
Figure 6.
15 years old child. Anteroposterior (A) and lateral (B) radiographs performed 8 months after operation shows absence of bone deformity.
Discussion
Supracondylar fractures of femoral bones in adolescents are most frequently caused by traffic accidents connected with high driving speed. The main reason is the anterior or lateral impact forces on a flexed knee. In older patients, these fractures are connected with osteoporosis most of the time.
Fractures of the distal femoral end in children may involve the metaphysis, epiphysis and femoral shaft. They often lead to lysis along the growth plate, which is the most fragile part of the bone. The majority of these fractures concern children in the age of 12–14 years. These childhood fractures are categorised by Salter-Harris classification, which is helpful in radiological evaluation and is highly correlated with the prognosis [1,2]. This classification does not include three types of childhood fractures regarding the distal part of the tibial bone: biplane fracture of Tillaux, triplane fracture, and type IV Rang fracture [3]. Lower limb fractures are connected with much worse prognosis than upper limb fractures. Shortenings and deformations of the lower limbs are much worse tolerated than the ones in the upper limbs, due to a higher physiological load [4].
Salter-Harris classification names five types of growth plate fractures – Table 1 [1]. They all take place before the physeal closure and may lead to bone deformities, growth arrest and disability.
Table 1.
Salter-Harris Classification (from “Caffey’s Pediatric Diagnostic imaging”, Mosby Elsvier, 2007).
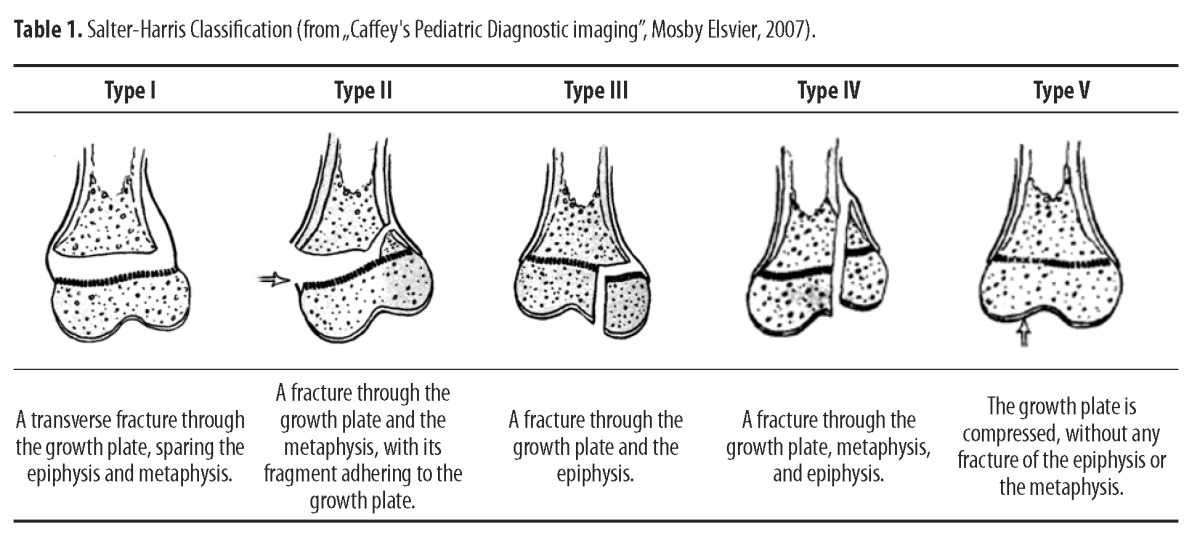
Type I – A transverse fracture through the hypertrophic part of the growth plate. The epiphysis is completely separated from the end of the bone and its metaphysis. The living part of the cartilage remains connected to the epiphysis. Type I fractures are hard to diagnose with X-ray, as this is only the cartilage that is broken. Sometimes, a minor dislocation of the epiphysis may become visible as late as during the recovery period. The complications are rare and most commonly associated with the injuries of bone-supplying vessels.
Type II – the most frequent – constitutes 85% of the fractures. The fracture line passes through the growth plate and the metaphysis. The Epiphysis and the growth plate are partially separated from chipped methaphyseal fragments. In most of the cases, a small part of the metaphysis is broken off partially, forming a wedge-shaped ‘corner sign’ at the edge of the metaphysis. Complications are rare. The only exception is type II fractures of the distal part of the femoral bone, as in the case described above. Their prognosis is poor and 43–70% of the fractures result in complications. [2,5,6]
Type III – concerns the distal parts of long bones in lower limbs: the tibial and femoral bone. The fracture passes through the epiphysis, separating a part of it, together with the growth plate, from the metaphysis. In this type of fracture, the articular cartilage gets partially fractured as well. The prognosis is good if the blood supply of the split epiphyseal fragment is remained, if there are no dislocations, and a layer of the regenerating bone is being created in the region of the fracture. Some cases require a surgical reduction and a fixation of bone fragments.
Type IV – the fracture goes through the epiphysis, the growth plate, and the metaphysis. Surgical treatment is compulsory for a proper reduction of the articular surfaces and a precise alignment of the growth plate. Prognosis is bad and connected with growth disorders when no precise recreation of the bone axis is performed and when such a state continues into the healing process.
Type V – its prognosis is the worst (as compared to the previous ones) but, luckily, this type of fracture is less frequent. The trauma results in compression and crush of the growth plate. Most of the time, the fracture concerns the distal parts of the femoral bone and both tibial growth plates, often with a concomitant fracture of the femoral, tibial or fibular shaft. The prognosis is bad because the premature growth arrest is nearly inevitable. Diagnosis with a standard X-ray is difficult and frequently retrospective, made at the moment of growth disturbances and angular deformities.
In the treatment of type I and type II fractures, a simple fixation suffices, as the bone returns to its normal shape during the growth process. However, a marked lysis with a dislocation (as found in our case) requires surgical treatment. It has been revealed that in 60% of the patients subjected to a closed reduction of type I and type II fractures, a cartilage fracture fissure exceeding 3 mm and invisible on X-rays, may lead to a premature physeal closure, although no fissure seen on X-ray images decreases the frequency of this severe complications up to 17% [7] This fact can be explained by an indentation of a dissected and disrupted periosteum into the fracture fissure and inhibition of a normal healing process of the cartilage, which all could be observed in the presented case. Although the conservative treatment leads to a lower number of complications, in comparison to the operative surgery, the above mentioned cases of type I and II fractures, as well as the fractures of the distal femoral bone, with dislocation, may be an indication for surgical treatment [2,5,7]. The direction and degree of bone fragment dislocation in type II fractures of the distal femoral end does not correlate with the prognosis, but the number of complications is over two times higher (65% vs. 30%) than the frequency of complications in mechanical injuries of the growth plate resulting from surgery [5].
Treatment of type III and type IV fractures requires a precise reduction to minimise the risk of complications. Due to the injury of the articular surface in these fractures, the preferred method of treatment is an open surgical procedure [5,6].
Growth arrest, being the consequence of type V fractures, is normally only partial and may be surgically treated by the resection of bone bridges, which allows for optimisation of surgical treatment results and reduction of late complications [8].
Standard X-ray images are the first and sometimes also the only method of diagnostic imaging. However, in children, they may have a substantially limited value. Type I Salter-Harris fractures involving the uncalcified epiphyseal cartilage may be hard to differentiate from articular dislocations. Similarly, in type III and type IV fractures, the course of the fracture fissure cannot be precisely evaluated due to only partial calcification of the epiphyses. As already mentioned above, in type V fractures, the value of X-ray is substantially limited. In such cases USG and MRI may visualise the exact course of the fracture line in the uncalcified cartilage and the location of the uncalcified epiphysis. An additional advantage of these diagnostic tools is the possibility of local soft tissue evaluation and assessment of regional complications. In high-risk fractures, the MRI may play a role in acute states, in visualising the early vascular and cartilaginous abnormalities, which reflect the state of the growth plate [9,10]. However, in the presented case, due to the complex arrangement of the bone fragments, the age of the child and no clinical symptoms suggestive of vascular complications, it was decided to carry out the CT, as the best method for bone structure visualisation. In practice, the fact that MRI is hard to approach (especially in emergency conditions) and expensive remains an important issue.
Multi-row spiral computed tomography with secondary presentation techniques is used for a more precise diagnosis of complicated fractures revealed on X-ray. The preoperative evaluation of fracture morphology with CT is particularly useful in ankle and knee joint fractures. It also significantly influences the precision of the operational procedure [11]. The multiplanar reconstruction and/or 3D volume rendering is the most useful diagnostic tool in multiplane and type IV Salter-Harris fractures, allowing for a precise assessment of the course of the fracture and the width of the fracture fissure along the articular surface [12]. According to the recent directives, the width of the fracture fissure exceeding 2 mm should be a practical criterion for surgical reduction [12,13].
Most fractures of the growth plate show a positive prognosis. However, growth disturbances may occur unless a proper alignment of the growth plate is obtained, especially when the rotation is not eliminated and the growth is inhibited by creation of abnormal callus. An alternative injury may result from the epiphyseal cartilage ischaemia and, as a consequence, from growth disturbances. Growth disturbances may be revealed with radiograms only after 3–4 months following the injury. Growth arrest is visible on X-ray as sclerotic bounds parallel to the line of the growth plate. Controversial fracture should be followed for up to two years after the injury. A normal radiological picture of the growth plate, two years after the injury, makes the consequent growth arrest hardly possible.
Conclusions
Typical X-ray images are not always able to show the precise type of fracture, slight dislocations of bone fragments, or growth plate injuries. All these abnormalities would be best visualised with a hardly accessible and costly MRI. We presented the above case of an injury suffered by a 14-year-old boy to bring closer the characteristics of childhood injuries which may damage the growth plate, their treatment method and prognosis. We would like to underscore the value of the CT examination and of the secondary reconstructions in the preoperative evaluation of the complicated fractures that may lead to bone deformities, growth disturbances and disability. When knowing the morphology of the fracture, visualised with CT, the orthopaedist may decide correctly on the type of procedure and the method of bone fragment fixation, and thus influence the end effect of the treatment process.
References:
- 1.Brown JH, DeLuca SA. Growth plate injuries: Salter-Harris classification. Am Fam Physician. 1992;46:1180–84. [PubMed] [Google Scholar]
- 2.Ilharreborde B, Raquillet C, Morel E, et al. Long-term prognosis of Salter-Harris type 2 injuries of the distal femoral physis. J Pediatr Orthop B. 2006;15:433–38. doi: 10.1097/01.bpb.0000228384.01690.aa. [DOI] [PubMed] [Google Scholar]
- 3.Duchesneau S, Fallat LM. The Tillaux fracture. J Foot Ankle Surg. 1996;35:127–33. doi: 10.1016/s1067-2516(96)80029-9. [DOI] [PubMed] [Google Scholar]
- 4.Chadwick CJ, Bentley G. The classification and prognosis of epiphyseal injuries. Injury. 1987;18:157–68. doi: 10.1016/0020-1383(87)90128-8. [DOI] [PubMed] [Google Scholar]
- 5.Arkader A, Warner WC, Jr, Horn BD. Predicting the outcome of physeal fractures of the distal femur. J Pediatr Orthop. 2007;27:703–8. doi: 10.1097/BPO.0b013e3180dca0e5. [DOI] [PubMed] [Google Scholar]
- 6.Eid AM, Hafez MA. Traumatic injuries of the distal femoral physis. Retrospective study on 151 cases. Injury. 2002;33:251–55. doi: 10.1016/s0020-1383(01)00109-7. [DOI] [PubMed] [Google Scholar]
- 7.Barmada A, Gaynor T, Mubarak SJ. Premature physeal closure following distal tibia physeal fractures: a new radiographic predictor. J Pediatr Orthop. 2003;23:733–39. doi: 10.1097/00004694-200311000-00010. [DOI] [PubMed] [Google Scholar]
- 8.de Sanctis N, Della Corte S, Pempinello C. Distal tibial and fibular epiphyseal fractures in children: prognostic criteria and long-term results in 158 patients. J Pediatr Orthop B. 2000;9:40–44. doi: 10.1097/01202412-200001000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Hübner U, Schlicht W, Outzen S, et al. Ultrasound in the diagnosis of fractures in children. J Bone Joint Surg Br. 2000;82:1170–73. doi: 10.1302/0301-620x.82b8.10087. [DOI] [PubMed] [Google Scholar]
- 10.Close BJ, Strouse PJ. MR of physeal fractures of the adolescent knee. Pediatr Radiol. 2000;30:756–62. doi: 10.1007/s002470000319. [DOI] [PubMed] [Google Scholar]
- 11.Cutler L, Molloy A, Dhukuram V, et al. Do CT scans aid assessment of distal tibial physeal fractures? J Bone Joint Surg Br. 2004;86:239–43. doi: 10.1302/0301-620x.86b2.13624. [DOI] [PubMed] [Google Scholar]
- 12.Brown SD, Kasser JR, Zurakowski D, et al. Analysis of 51 tibial triplane fractures using CT with multiplanar reconstruction. AJR Am J Roentgenol. 2004;183:1489–95. doi: 10.2214/ajr.183.5.1831489. [DOI] [PubMed] [Google Scholar]
- 13.Slongo TF. The choice of treatment according to the type and location of the fracture and the age of the child. Injury. 2005;36:A12–19. doi: 10.1016/j.injury.2004.12.008. [DOI] [PubMed] [Google Scholar]





