Summary
Background:
Ewing sarcoma is a malignant, small round cell bone tumor, presenting predominantly in children and adolescents. Ewing sarcoma may develop in every bone; diaphyses of long bones, ribs and flat bones are the main locations. Local and systemic clinical symptoms are nonspecific - pain, swelling, fever or ill-being.
The aim of the study was to assess the role of radiography, computed tomography and magnetic resonance imaging in the analysis of bone lesions in children and young adults with Ewing sarcoma.
Material/Methods:
Twenty-seven patients, aged between 1 year and 10 months, and 17 years and 2 months, with histologically verified Ewing sarcoma of the bone, referred to the Radiological Department of University Hospital No 6., John Paul II Upper Silesian Centre for Child Health Katowice, in the period from 1996 to 2007, were included in the study.Plain radiography was performed in every child, CT in 20 and MRI in 12 individuals. Tumour location, extension of the tumour, soft tissue mass, and periosteal reaction were taken into consideration in the evaluation of the lesion. In some cases, pathological features of the MRI and CT were compared. The prevalence of some radiological features was compared to the literature data.
Results:
The most common site of tumor was: ribs (6 children), femoral bone (6 children), pelvis (4 children) and tibia (3 children). In 2 children, a primary tumor was diagnosed in the spine (multifocal in 1 child).
X-rays revealed: periosteal reaction in 17 children (63%), soft tissue involvement in 19 children (70%), permeative component in 16 children (59%), and sclerotic component in 5 children (19%). In 10 children (37%), periosteal reaction was not detected. The examination revealed: soft tissue calcifications in 7 cases (26%), a well-delineated focus of destruction within bones in 3 children (11%), cortical thickening in 4 children (15%), cortical destruction in 4 children (15%), saucerisation in 3 children (11%), bone expansion in 3 children (11%), pathological fracture in 2 children (7%), cystic component in 1 child (4%), and vertebra plana in 1 child (4%).Reaction of tumors after i.v. contrast administration, shown on CT, was visible in 16 children – it was useful for a better description of the tumor and extension of the mass within the soft tissue. All MRI examinations (12 children) showed a heterogenous mass with ill-defined borders and a violated cortex. Low signal intensity of the tumor in a T1-weighted image and high signal intensity in a T2-weighted image was shown as well.
Heterogenous enhancement of signal intensity on T1-weighted images could be observed after i.v. contrast administration.
MRI examinations showed: tumor in an adjacent soft tissue in 11 children, and involvement of the epiphyseal plate or of the joint cavity in 6 children.
Conclusions:
X-ray and MRI are essential in diagnostics. CT examination is more useful to estimate periosteal reactions and destruction of bone and marrow cavity, especially in flat bones. However, to recognise a malignancy, it is necessary to perform a histopathological examination. In doubtful cases, the examination has to be verified as well.
Keywords: Ewing sarcoma, bone tumour, children, X-rays, CT, MRI
Background
Ewing sarcoma constitutes approximately 10% of all malignancies of the bones and 1–3% of all paediatric cancers. It is second the most frequent malignancy of the bones in children [1,2]. Among all malignant cancers of the bones in children, Ewing sarcoma accounts for approx. 41% of the cases in children of up to 14 years of age, and approx. 28% in children aged 15–19 years [3,4].
Clinical symptoms of the tumour are not specific. They include pain – often at night and disrupting sleep – swelling, fracture – often associated with a suspected injury – limited mobility and impaired walking ability. Local symptoms depend on tumour location. Primary focus located in the spine, proliferation of the tumour into the vertebral canal, or involvement of the intervertebral foramen may lead to radiculalgia, paresis of paralysis. Tumours located in the bones of the thoracic cavity (ribs, spine) or in the pelvic bones may be associated with an elevated body temperature, cough, or urinary tract infections – which delays the diagnosis. Involvement of the cranium, infiltration of the meninges, or metastases to the brain may induce changes in child’s mood and behaviour. Fever, advancing marasmus, cough, difficulties in breathing – may be the symptoms of metastases to the thorax [5–9].
Clinical diagnosis of the bone cancer becomes possible after a plain X-ray, which is essential for further diagnostics and therapeutic management. Plain X-ray revealing a focus of inhomogeneous, osteolytic and ill-delineated lesion, as well as malignant periosteal reactions constitutes a basis of ‘malignant bone cancer’ diagnosis. Periosteal reactions may be absent in flat bones. Typical features of Ewing sarcoma include: foci of permeative degeneration or foci of ‘eaten by moths’ type, periosteal reactions – of ‘onion bulbs’ type in most of the cases (rarely of ‘sunbeam’ type, i.e. so called spiculated), and a concomitant tumour of soft tissues.
In order to visualise a malignancy, it is necessary to widen X-ray diagnostics by an MRI or a CT. MRI is the most detailed method of tumour visualisation. It may be used for visualisation of the following pathologies: tumour and its structure, as well as neoplastic involvement of the marrow cavity and of the adjacent tissues. CT images are most useful in evaluating the degree of bone destruction and concomitant malignant periosteal reactions. Owing to the measurements of tissue density, it is also possible to assess the marrow cavity.
The role of laboratory tests is insignificant (elevated ESR, alkaline phosphatase).
The final diagnosis of the type of malignancy requires a histopathological confirmation, in order to exclude inflammation and to differentiate with other small round cell carcinomas found in children: sympathoblastoma, primitive neuroendodermal tumour (PNET), microcellular osteogenic sarcoma or non-Hodgkin’s malignant lymphoma [6,10,11]. Ewing sarcoma, PNET tumours, Askin tumour (PNET tumour of the thoracic cavity) belong to Ewing family of tumours. In cytogenetic examinations, they reveal a chromosomal translocation t(11;22)(q24;q12), which indicates their common histogenesis [3].
The aim of the work was to assess the usefulness of the imaging methods (X-ray, CT, MRI) in the diagnostics of Ewing’s sarcoma in children.
Material and Methods
A retrospective analysis involved X-ray, CT, and MRI images of bone tumours, performed in the years 1996–2007, at the Institute of Imaging Diagnostics, Public Hospital No. 6 of the Upper Silesian Centre for Child Health in Katowice, as well as MRI images carried out at the Laboratory of HELIMED. The examinations involved 27 children (13 girls and 14 boys), at the age from 1 year and 10 months to 17 years and 2 months (mean age 12 years and 3 months) (Table 1).
Table 1.
Prevalance of Ewing’s sarcoma in age groups (n=27).
| Below 10 yrs | 10–15 yrs | ≥15 yrs | |
|---|---|---|---|
| Number of children | 11 | 9 | 7 |
| Percent | 40.74 | 33.33 | 25.93 |
In all cases, the final diagnosis based on the results of a histopathological examination.
All the children underwent plain X-ray imaging of the involved bones. MRI examination was carried out in 12 children, and CT of the involved bones – in 20 children. In accordance with the current protocol for diagnosis and treatment, all the children underwent chest CT. Bone scintigraphy was performed in 13 cases, and USG of the bone-joint system in 6 children.
We measured the time period from the moment of clinical symptom onset, to the first X-ray of an involved bone.
The analysis of bone tumour X-ray images included the following radiological features:
Location of the tumour within bones.
Tumour boundaries (ill- or well-delineated).
Type of bone destruction.
Type of periosteal reactions: onion bulbs, picture of ‘sunbeams’ – spiculated, presence of Codman’s spur (Codman’s triangle).
Soft tissue mass.
Soft tissue calcifications.
Sclerotic lesions.
Cortical thickening or destruction.
Presence of saucerisation.
Bone expansion.
Pathological fracture.
Lesions of ‘vertebra plana’ type, in the spine.
CT was performed before and after i.v. contrast administration. Reaction to the contrast medium was assessed according to the following scale:
0 – no reaction.
1 – signal intensification within the tumour.
2 – intensification of the signal within the tumour and adjacent soft tissues.
MRI examination, in T1, T2 FAT-SAT (or STIR), T1 FAT-SAT sequence of the spin echo, before and after i.v. contrast administration, evaluated signal characteristics within the tumour and adjacent tissues. The following elements were assessed on the basis of the MRI images:
Tumour extension – within and outside the bones.
Tumour infiltration within the metaphyseal growth cartilage and / or the articular cavity.
Tumour boundaries.
Bone cortex.
Homogeneity / inhomogeneity of the tumour structure.
Signal intensity in T1-weighted and T2-weighted images.
Results
In 19 children (70%), the first clinical symptom was pain of the involved site (Table 2). In 5 children, it was associated by a local swelling and a palpable tumour. Nyctalgia appeared in 3 cases. Four of the children (15%) had a palpable tumour or oedema, not associated with any pain. In one case, the tumour was found by accident, after a casual injury. Two children (7%) were diagnosed with a pathological fracture. There were single cases of an elevated body temperature, weakness, decreased body mass, changes of behaviour, urinary tract infections and persistant bronchitis.
Table 2.
Clinical symptoms (n=27).
| Clinical symptom | Number of children |
|---|---|
| Pain / with concomitant swelling / nyctalgia | 19 / 5 / 3 |
| Swelling/tumour | 4 |
| Pathological fracture | 2 |
| Weakness | 1 |
| Increased body temperature | 1 |
| Loss of body mass | 1 |
| Change of behaviour | 1 |
| Infection of the urinary tract | 1 |
| Therapy-resistant bronchitis | 1 |
| Injury/ Previously unnoticed tumour | 1 |
Time that passed from the onset of clinical outcomes till the first X-ray was not always the same. There were two asymptomatic cases in which the tumour was diagnosed by accident, during an X-ray for a sustained injury. In one case, the tumour involved the fibula, and in the other one, the pathologically fractured femur only. In case of Ewing sarcoma originating from the clavicle, the first image was taken after 7 months from the onset of pain. Mean time that passed from the first X-ray amounted to 3 months (2.95 months).
In the study material, the primary focus of Ewing sarcoma was revealed in the ribs of 6 children, in the femoral bone of 6 children, in the pelvic bones of 4 children (iliac, pubic, sciatic), and in the tibial bone in 3 children. Tumour of the spine was present in 2 cases – in the first case it was only one vertebra – L2, and in the other child it was multifocal (lesions in the thoracic, lumbar, and sacral spine, as well as in the temporal bone and within the clavicle). The locations of the tumour were presented in Table 3.
Table 3.
Location of Ewing’s sarcoma within the skeletal system (n=27).
| Tumour location within the bones | Number of children (n=27) |
|---|---|
| Rib | 6 |
| Femoral bone | 6 |
| Tibial bone | 3 |
| Iliac bone | 3 |
| Iliac bone + spine | 1 |
| Spine | 1 |
| Ulnar bone | 1 |
| Fibular bone | 1 |
| Finger | 1 |
| Temporal bone | 1 |
| Clavicle | 1 |
| Pubic bone + Ischium | 1 |
| Ischium | 1 |
In the studied group of 27 children, there were 19% of cases with Ewing tumour originating from the pelvic bones, and 44% of cases in which the tumour originated from the long bones. The most common location within the long bones was the diaphysis and the metaphysis (Table 4).
Table 4.
Location of Ewing’s sarcoma within the long bone (n=12).
| Location | Number of children (n=12) | Proportion (n=12) |
|---|---|---|
| Epiphysis | 0 | 0 |
| Metaphysis | 1 | 8 |
| Metaphysis/diaphysis | 8 | 67 |
| Diaphysis | 3 | 25 |
At the moment of diagnosis, in 8 cases, the tumour involved only bones, without any infiltrations of the soft tissues. The involved bones included: ulna, femur, tibia, ilium, ischium, temporal bone, and lumbar vertebra. In the remaining 19 cases, the tumour infiltrated the adjacent tissues.
Distant metastases were found in only 3 children (11%): one in lungs (with the primary location being vertebra L2), one in lungs and the temporal bone (primary location: clavicle), and the last one in vertebra Th11, complicated by a pathological fracture (primary location: tibia).
X-rays of 17 children (63%) showed malignant periosteal reactions (Figure 1). In 19 cases (70%) there was involvement of soft tissues, and in 16 children (59%) – a diffuse destruction of the bones.
Figure 1.

A boy, 13 years old, conventional radiography of the femoral bone – spiculated periosteal reaction, Codman’s triangle.
In 10 children (37%), periosteal reaction was not detected. The examination revealed: soft tissue calcifications in 7 cases (26%), a well-delineated focus of destruction within bones in 3 children (11%), cortical thickening in 4 children (15%), cortical destruction in 4 children (15%), saucerisation in 3 children (11%), bone expansion in 3 children (11%), pathological fracture in 2 children (7%), cystic component in 1 child (4%), and vertebra plana in 1 child (4%).
CT examination was performed in 20 children (Figure 2). CT before and after contrast administration was carried out in 16 children. In four children, the contrast medium was not injected. All 16 children were proved to show a reaction of the tumour to the intravenous contrast agent – which allowed for a better morphological assessment of the tumour and of extension of the infiltration within the soft tissues. CT examination enabled a precise evaluation of the degree of bone destruction and periosteal reactions. In four cases, the tumour was not surpassing the outline of the bones. In 12 cases (60%), it was infiltrating the adjacent soft tissues.
Figure 2.

A boy, 12 years old, CT of the pelvis – a tumor in left iliac bone, with an extensive bone destruction, spiculated periosteal reaction and soft tissue mass, bone window
In all analysed MRI images (12 children), Ewing sarcoma revealed an inhomogeneous structure and ill-delineated borders; it caused thinning and cortex discontinuation. MRI results of 11 children showed tumour in the adjacent soft tissues. In 6 cases, the tumour involved the epiphyseal plate or of the joint cavity. In all children, the lesion showed a decreased signal intensity in T1-weighted images, and an increased signal intensity in T2-weighted sequences. An important role in bone tumour imaging is played by sequences with fat saturation – STIR, FAT SAT. T2-weighted images with fat saturation allow for an exact determination of the tumour borders, the presence of infiltrations of the marrow cavity and of the fatty tissue adjacent to the tumour, as well as the presence of the necrotic spheres (Figure 3A,B).
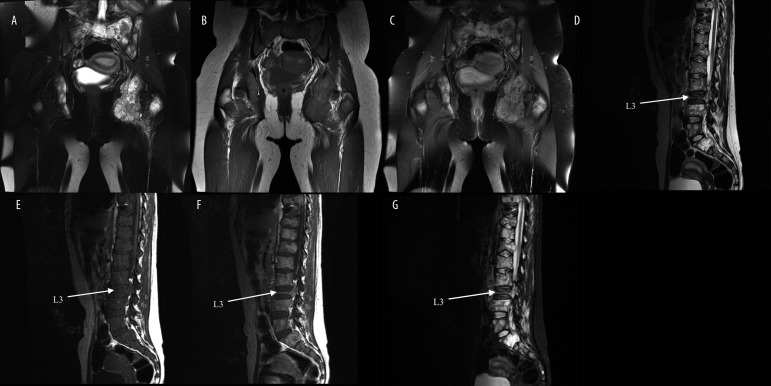
Figure 3.
A boy, 12 years old, MRI of the pelvis – infiltrative tumour of left iliac bone with an extensive bone destruction and soft tissue mass. (A) axial plane FSE T2. (B) axial plane SE T1. (C) axial plane SE T1+C. (D) coronal plane SE T1 FSAT+C.
Moreover, T1-weighted images with fat tissue saturation, after i.v. contrast administration, enable an exact distinction of the enhanced tumour mass, infiltrations of the surrounding fatty tissue, and soft tissue structures that do not reveal an increased signal intensity (Figures 4–6).
Figure 4.
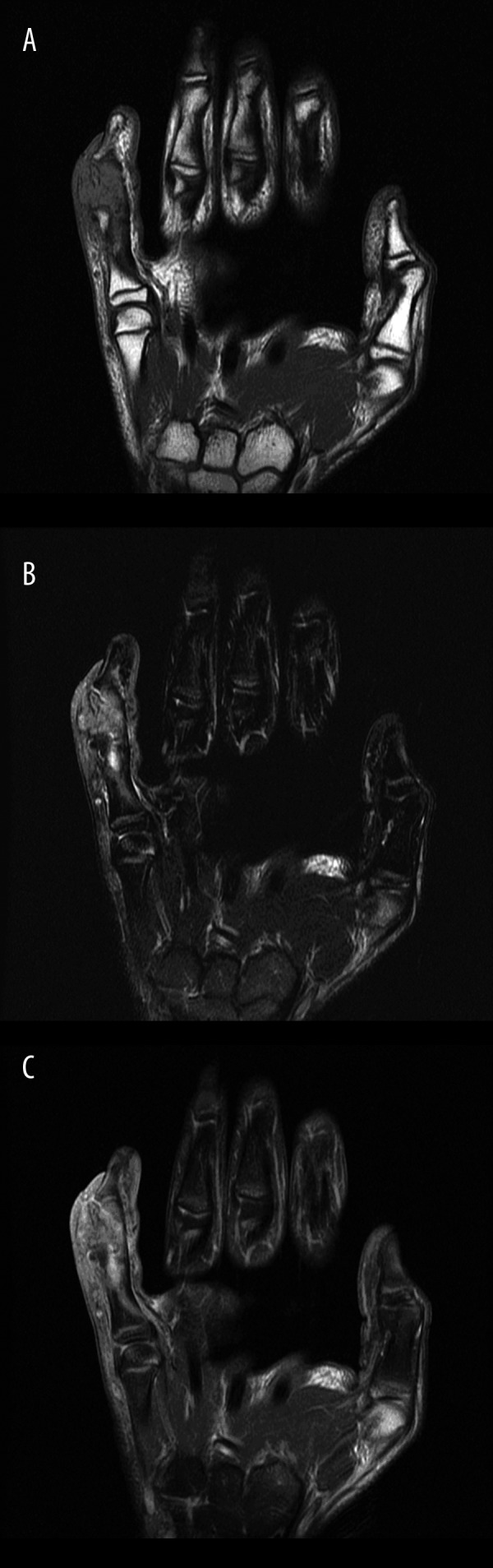
A boy, 12 years old; MRI of the hand – inhomogeneous mass in the middle phalanx of the Vth digit of the hand, with soft tissue mass and involvement of the interphalangeal joints. (A) coronal plane T1. (B) coronal plane T2 FAT-SAT. (C) coronal plane T1 FAT-SAT+C.
Figure 6.
A girl, 16 years old, MRI of the spine and pelvis: multiple diffuse, infiltrative lesions of the spine (abnormal shape of the vertebral bodies, inhomogeneous intensity of signals) with destruction of vertebral body L3 – vertebra plana, and in the bones of the pelvis. (A) Cor FSE T2 FSAT. (B) Cor SE T1. (C) Cor SE T1 FSAT +C. (D) Sag FSE T2. (E) Sag SE T1. (F) Sag SE T1 + C. (G) Sag STIR.
In a few cases, X-ray image was not suggestive of malignancy. Special attention should be paid to cases of a suspected inflammatory lesion of the bones.
Diagnosis of Ewing sarcoma requires a histopathological confirmation. In this diagnostic test, Ewing sarcoma is shown as a light grey or white, well-vascularised, soft tumour, often with concomitant haemorrhages and with necrotic foci which may resemble inflammatory purulate exudates. The cancer consists mostly of tiny, round cells, including small amounts of bright or eosinophilic cytoplasm with indistinct borders, merging with adjacent cells. The nuclei are oval or round, with fine-grained chromatin, without visible or with single nucleoli. The cancer is atypical in approx. 5% of all cases. It is then built of slightly larger cells with pleomorphic nuclei, with distinct nucleoli. The tumour is characterised by a low mitotic activity (slightly higher in the atypical form). It proliferates in the form of solid fields, separated by a meagre stroma. It may also infiltrate adjacent tissues with thin strands of cells (Figure 7).
Figure 7.
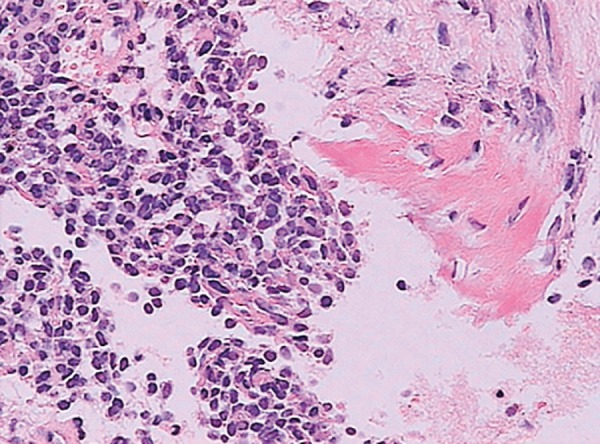
Histopathological examination – Ewing’s sarcoma.
Discussion
The study group included 27 children – 13 girls and 14 boys. According to the literature, this tumour is more frequent in boys (ratio ranging from 1.5:1 to 2:1) [3,12]. Our material did not confirm this quantitative predominance of male subjects, which was most probably connected with an insufficient number of children included in the study.
Patient’s age and location of the tumour within all bones or one bone constitutes an important fact for the differential diagnosis [13,14].
The analysis of some chosen clinical data showed that, similarly to other primary bone tumours, there was no clinical symptoms characteristic for Ewing sarcoma, which was in accordance with the literature [3,8]. In the study group, 19/27 patients (70%) experienced pain of the involved area. In five cases out of 27, the examination revealed a tumour or oedema, without concomitant pain. Night pains were present in 3 children (3/27). Four children out of 27 were diagnosed with tumour or swelling without concomitant pain. There were single cases of an elevated body temperature, weakness, loss of body mass, changes in child’s behaviour, urinary tract infections, and persistant bronchitis.
In the analysed group of children, the time period from the moment of clinical symptom onset, to the first X-ray examination ranged from 1 day to 7 months (mean time of approx. 3 months). According to the literature, the mean time from symptom onset to the diagnosis amounted to approximately several months [3,4,6].
Ewing sarcoma may develop in every bone [3]. In the long bones, it is typical for Ewing sarcoma to locate its primary foci in the bone shafts. The second most frequent location (apart from the diaphysis) is the spine and the flat bones. The primary foci are less frequent in soft tissues [12].
In the studied group, Ewing sarcoma originated from the pelvic bones in 6 cases and from the long bones in 12 individuals (including 6 cases of the femoral bone). In the long bones, the most common location was the diaphysis (11 children), including the metaphysis – in 8 cases out of 12. In one child, the primary site of origin was the metaphysis only. Location of the primary focus within bones in the analysed paediatric group did not differ from the literature data [3,12,15]. There were no cases of the tumour involving the epiphysis of the long bone, which is consistent with the literature [3]. In the Intergroup Ewing’s Sarcoma Study (IESS) published in 1984 [12], carried out by Mallinckrodt Institute of Radiology (Washington University) and including 373 patients, there was only one lesion of the epiphysis, found in the group of 206 tumours of the long bones.
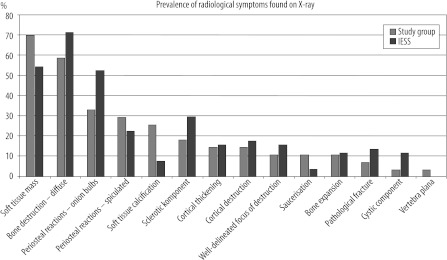
X-ray visualisation of malignant periosteal reactions, diffuse bone destruction, and soft tissue involvement allowed for the diagnosis of malignancy. In our material, X-ray images showed a diffuse degeneration of bones in 16/27 children (59%), and a well-delineated pattern of bone destruction in 3 children (11%) – as compared to the literature data: 72% and 16%, respectively [12]. Malignant periosteal reactions were found in 17 cases; soft tissue involvement was observed in 19 children. In 10 cases out of 27 (37%) there was no malignant periosteal reactions. Three cases out of 27 (11%) revealed a well-delineated focus of destruction. In four children out of 27 (15%) there was only a thickening (without any distruction) of the cortex. Three children (11%) were diagnosed with bone expansion.
Periosteal reactions were observed in 63% of children in total. The ‘onion bulb’ type was found in 9 children (33%), while the ‘sunbeam’ type in 8 individuals (30%). The IESS study [12] showed a predominance of the ‘onion bulb’ periosteal reactions. They were found in 53% of cases.
Three of the children (11%) from our study group were diagnosed with saucerisation, described in the literature in approx. 4% of cases only [12,16].
Two children (7%) were found to have a pathological fracture. Cystic component of the tumour was found in one case (4%). Moreover, our material revealed one case of a flat vertebra ‘vertebra plana’ – an extremely rarely observed finding in Ewing sarcoma (Figure 6D–G). The IESS study found only one such case in the group of 373 patients, which constituted 0.3% (Table 5, Figure 8).
Table 5.
Radiographic features on X-rays, compared with Intergroup Ewing’s Sarcoma Study (IESS).
| Number of children in the study group | % in the study group (n=27) | % according to IESS (n=373) | |
|---|---|---|---|
| Soft tissue involvement | 19 | 70 | 55 |
| Bone destruction – diffuse | 16 | 59 | 72 |
| Periosteal reactions – onion bulbs | 9 | 33 | 53 |
| Periosteal reactions – spiculated | 8 | 30 | 23 |
| Soft tissue calcification | 7 | 26 | 8 |
| Sclerotic component | 5 | 19 | 30 |
| Cortical thickening | 4 | 15 | 16 |
| Cortical destruction | 4 | 15 | 18 |
| Well-delineated focus of destruction | 3 | 11 | 16 |
| Saucerisation | 3 | 11 | 4 |
| Bone expansion | 3 | 11 | 12 |
| Pathological fracture | 2 | 7 | 14 |
| Flat vertebra – vertebra plana | 1 | 4 | 0,3 |
| Cystic component | 1 | 4 | 12 |
Figure 8.
Prevalence radiographic features on X-rays compared with Intergroup Ewing’s Sarcoma Study (IESS).
At the moment of diagnosis, the tumour frequently infiltrates the adjacent soft tissues. This happens, according to the literature, in 55–75% cases [12]. In the study group, involvement of the soft tissues at the moment of diagnosis was found in 19/27 cases (70.37%). No such an involvement was found in 8/27 children.
Soft tissue calcifications were present in approx. 26% of children, which is in accordance with the literature: from 8% to 55% [12].
Two children were treated for the inflammation of the clavicle and of the middle phalanx of the V{th digit of the left hand. X-ray was not suggestive of malignancy. It should be remembered to exclude malignancy in case of persistant inflammations. If other imaging methods and histological examinations are not included in the diagnostic work-up, the time to diagnosis (of malignancy) will be longer.
The number of children with distant metastases in the study group accounted for approx. 11%. According to the literature, this proportion ranges from 10% to over 20% [3,5,13].
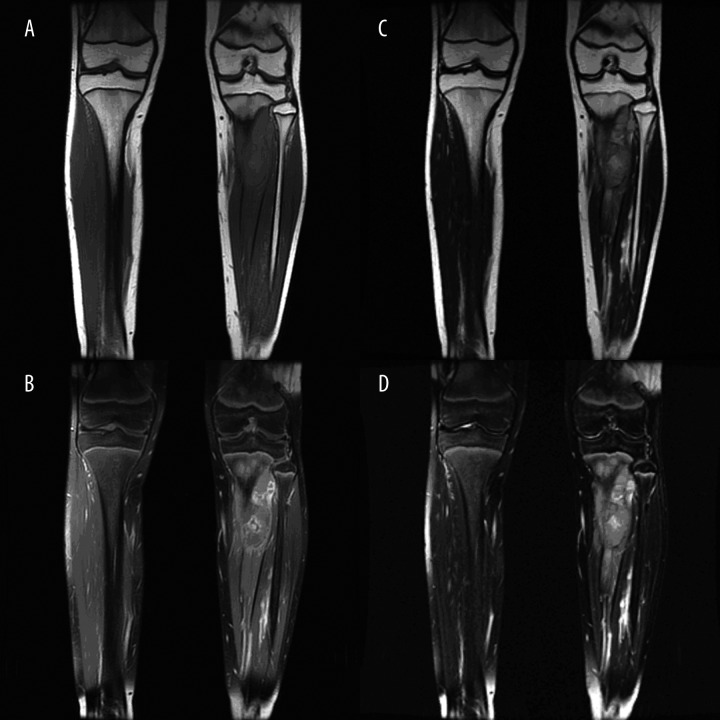
Magnetic resonance imaging allows for a detailed evaluation of: tumour borders, soft tissue involvement (including the vascular-neural structures), destruction of bones and epiphyseal plate, and penetration to the articular cavity (Figure 5A–D). It is also useful in the determination of the lesion border, i.e. in treatment planning process. Ewing sarcoma reveals a low signal intensity in T1-weighted MRI images. In T2-weighted images, the tumour shows an inhomogeneous, increased signal intensity.
Figure 5.
A boy, 13 years old; MRI of the calf – a lesion in the proximal part of the diaphysis and in the metaphysis of the left tibia, with extensive bone destruction and soft tissue mass; heterogeneous enhancement after contrast administration. (A) coronal plane T1. (B) coronal plane T1 FAT-SAT+C, (C) coronal plane T2. (D) coronal plane T2 FAT-SAT.
In all MRI examinations (12 children), Ewing sarcoma showed an inhomogeneous structure and blurred borders. It caused tissue thinning and cortex discontinuation. In 11 out of 12 children, the tumour was found in adjacent soft tissues, and in 6 out of 12 cases – the epiphyseal plate or the articular cavity was involved. The evaluation of the presence or the structure of the tumour is easier in the following sequences: fat saturation (STIR, FAT SAT), T2-weighted and T1-weighted after intravenous contrast administration. Comparison of the CT and MRI images of the pelvis of one patient showed that CT examination of the involved bones is more detailed in the visualisation of bone destruction and calcifications of the tumour and of adjacent soft tissues. CT imaging is especially important in case of tumours of the flat bones, in which the periosteal reaction may be limited.
In a detailed evaluation of the primary foci and of the extension of the neoplasmatic process, each of the imaging methods – X-ray, CT, MRI – provides us with significant and complementary information. According to the literature, both a plain X-ray, and an MRI is recommended in the course of the diagnostic work-up of Ewing sarcoma [16].
At present, the literature underscores the role of Doppler USG in the evaluation of tumours within soft tissues, periosteal reactions and the degree of vascularisation or necrosis. Follow-up USG examinations carried out in the treatment process, for the evaluation of the range of necrosis, are of particular importance [17,18]. A 99mTc scintigraphy, being a sensitive but not specific examination, is useful in the evaluation of the disease extension within the bones, in the localisation of metastases and in the monitoring of the disease course [19]. To evaluate metastases within lungs, it is necessary to perform a chest CT [20]. To exclude a bone tumour, it is always necessary to perform and to verify the results (in uncertain cases) with the use of a histopathological examination [21,22].
Conclusions
The diagnostic work-up of Ewing sarcoma is initiated by a plain X-ray of an involved bone.
MRI is the most useful examination in the evaluation of tumour extension and involvement of the articular cavity.
CT is a supplementary examination, performed in order to evaluate bone destruction, especially the lesions of flat bones, in which the periosteal reactions may be absent or limited.
The final diagnosis of Ewing sarcoma requires histopathological verification.
References:
- 1.Yaw KM. Pediatric bone tumors. Semin Surg Oncol. 1999;16(2):173–83. doi: 10.1002/(sici)1098-2388(199903)16:2<173::aid-ssu8>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 2.Li WY, Brock P, Saunders DE. Imaging characteristics of primary cranial Ewing sarcoma. Pediatr Radiol. 2005;35(6):612–18. doi: 10.1007/s00247-005-1438-2. [DOI] [PubMed] [Google Scholar]
- 3.Ivamoto Y. Diagnosis and treatment of Ewing’s Sarcoma. Jpn J Clin Oncol. 2006;37(2):79–89. doi: 10.1093/jjco/hyl142. [DOI] [PubMed] [Google Scholar]
- 4.Stiller CA, Bielack SS, Jundt G, et al. Bone tumours in European children and adolescents, 1978–1997. Report from the Automated Childhood Cancer Information System project. Eur J Cancer. 2006;42(13):2124–35. doi: 10.1016/j.ejca.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 5.Vukasinović Z, Stevanović V, Spasovski D, et al. Ewing sarcoma – current opinion. Srp Arh Celok Lek. 2006;134(7–8):348–55. [PubMed] [Google Scholar]
- 6.Ewerbeck V, Mau H. Differential diagnosis of benign bone tumors. Clinical aspects and imaging procedures. Orthopade. 1995;24(1):15–23. [PubMed] [Google Scholar]
- 7.Paz-Priel I, Long L, Helman LJ, et al. Thromboembolic events in children and young adults with pediatric sarcoma. J Clin Oncol. 2007;25(12):1519–24. doi: 10.1200/JCO.2006.06.9930. [DOI] [PubMed] [Google Scholar]
- 8.Kluczewska, Kuleta-Bosak E, Madziara W, et al. Symptoms of bone tumors in children. J Orthop Trauma Sur Rel Res. 2007;7(3):82–89. [Google Scholar]
- 9.Kuleta-Bosak E, Kluczewska E, Madziara W, et al. Specifics of diagnosis and therapy of bone tumors in children. J Orthop Trauma Sur Rel Res. 2007;7(3):75–81. [Google Scholar]
- 10.Hameed M. Small round cell tumors of bone. Arch Pathol Lab Med. 2007;131(2):192–204. doi: 10.5858/2007-131-192-SRCTOB. [DOI] [PubMed] [Google Scholar]
- 11.Girschick HJ, Mornet E, Beer M, et al. Chronic multifocal non-bacterial osteomyelitis in hypophosphatasia mimicking malignancy. BMC Pediatr. 2007;7:3. doi: 10.1186/1471-2431-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reinus WR, Gilula LA. Radiology of Ewing’s sarcoma: Intergroup Ewing’s Sarcoma Study (IESS) RadioGraphics. 1984;4:929–44. [Google Scholar]
- 13.Stevanovic V, Vukasinovic Z, Spasovski D. Ewing’s sarcoma in children: prognosis in relation to the method of treatment. Srp Arh Celok Lek. 2006;134(9–10):420–46. doi: 10.2298/sarh0610420s. [DOI] [PubMed] [Google Scholar]
- 14.Lopes SL, Almeida SM, Costa AL, et al. Imaging findings of Ewing’s sarcoma in the mandible. J Oral Sci. 2007;49(2):167–71. doi: 10.2334/josnusd.49.167. [DOI] [PubMed] [Google Scholar]
- 15.Skotakova J, Mach V, Bajciova V, et al. Malignant tumors of long bones in children: differential diagnosis and the role of imaging methods. Acta Chir Orthop Traumatol Cech. 2006;73(3):183–89. [PubMed] [Google Scholar]
- 16.Mueller DL, Grant RM, Riding MD. Cortical saucerization: an unusual imaging finding of Ewing sarcoma. AJR Am J Roentgenol. 1994;163(2):401–3. doi: 10.2214/ajr.163.2.8037040. [DOI] [PubMed] [Google Scholar]
- 17.Saifuddin A, Burnett SJ, Mitchell R. Pictorial review: ultrasonography of primary bone tumours. Clin Radiol. 1998;53(4):239–46. doi: 10.1016/s0009-9260(98)80119-0. [DOI] [PubMed] [Google Scholar]
- 18.Orbach D, Glorion C, Mary P, et al. Malignant tumours of the locomotor apparatus in children: an “intermediate” prognosis. Rev Prat. 2007;57(10):1080–86. [PubMed] [Google Scholar]
- 19.Cummings JE, Ellzey JA, Heck RK. Imaging of bone sarcomas. J Natl Compr Canc Netw. 2007;5(4):438–47. doi: 10.6004/jnccn.2007.0038. [DOI] [PubMed] [Google Scholar]
- 20.Grampp S, Bankier AA, Zoubek A, et al. Spiral CT of the lung in children with malignant extra-thoracic tumors: distribution of benign vs malignant pulmonary nodules. Eur Radiol. 2000;(10):1318–22. doi: 10.1007/s003300000359. [DOI] [PubMed] [Google Scholar]
- 21.Ewerbeck V, Mau H. Differential diagnosis of benign bone tumors. Clinical aspects and imaging procedures. Orthopade. 1995;24(1):15–23. [PubMed] [Google Scholar]
- 22.Papagelopoulos PJ, Mavrogenis AF, Benetos IS, et al. Ewing’s sarcoma of the hip presenting as a benign cystic lesion. J Surg Orthop Adv. 2007;16(2):84–88. [PubMed] [Google Scholar]