Summary
Background:
Injury to facial soft tissues as a complication of skeleton fractures is an important problem among patients with facial trauma.
The aim of this work was to assess the value of multiplanar and three-dimensional (3D) reconstruction computed tomography (CT) images obtained by using multi-detector row technology in spiral data acquisition in patients with facial injuries of soft tissue.
Material/Methods:
Sixty-seven patients diagnosed with injury to the facial skeleton underwent a CT scan with the use of GE Hispeed Qx/i scanner. For each patient: a two-dimensional (2D) multiplanar reconstruction (MPR), maximum intensity projection (MIP), and 3D volume rendering (VR) were conducted.
Post-injury lesions of soft tissues were assessed. During the assessment of the post-injury lesions of soft tissues, the following features were evaluated:
Extraocular muscle and fat tissue herniation through fractures in the medial and inferior orbital walls. Fluid in the sinuses and in the nasal cavity. Subcutaneous tissue emphysema.
Results:
For subcutaneous emphysema and sinus fluid imaging, both the axial and the 2D image reconstruction proved comparably effective. However, 2D reconstructions were superior to transverse plane images with regard to herniations into fractures of the inferior orbital wall. 3D reconstruction has no importance in diagnosing soft tissue injuries.
Conclusions:
Multiplanar CT reconstructions increase the effectiveness of imaging of orbital tissue herniations, especially in case of fractures in the inferior orbital wall.
In suspected soft tissue herniations, as well as prior to surgical treatment, spiral CT with 2D multiplanar reconstructions should be the method of choice.
Keywords: facial injuries, soft tissue injuries, computed tomography, CT
Background
The most common locations of the fractures within facial bones are: the mandible (incidence of 15–76%), nasal bones (28–44%), bones of the medial part of the face (approx. 30%), isolated fractures of zygomatic bones (approx. 20%), orbital fractures (approx. 10%) [1–4]. The traumatic lesions within the face may be isolated. However, very often, in up to 80% of cases, they are one of many post-traumatic pathological lesions [5–7]. The extent, severity, and location of coexisting traumatic lesions depends on the mechanism and force of the injury. Most frequently, these lesions involve the central nervous system, cervical spine, chest, and limbs.
The most common classification of the facial fractures is the Le Fort classification. Fractures of this type are bilateral. However, they not always concern the same bone structures on both sides of the face, symmetrically.
A special type of facial fractures is the expanding orbital fracture of blow-out type. It appears when the force is applied directly to the eye-ball, and is transmitted through the eye-ball and soft tissues of the orbit, on its walls, which results in the fracture of fragile walls of the orbit (medial and lateral one – together or separately), with sparing of a more massive edge of the orbital cavity [9].
A common complication of such fractures is the herniation of the orbital soft tissues (both the adipose tissue and muscles) through the fracture, to the lumen of the maxillary sinus, with their incarceration [10,11].
Other complications within facial soft tissues include first of all those that cause a significant risk of permanent defects or pose a direct risk to life, such as disturbed patency of the upper airways, accompanying fractures of this area. The type of these fractures is connected with fracture location. Fractures of the upper orbital wall and frontal sinuses carry a risk of meningeal disruption with a risk of CNS infection and injury of the brain lobes. In extreme cases, the fracture may reach the canal of the optic nerve and result in its injury [12]. Fracture of the lateral orbital wall may reach to the upper orbital fissure, damaging the III, IV, and VI cranial nerve, or to the lower orbital fissure, damaging or compressing the suborbital nerve [13,14]. Only a rapid introduction of surgical treatment and decompression of these structures may restore a normal function of the nerves in such cases [10]. Fracture of a cribriform plate of the ethmoid bone may lead to an injury of the meninges, followed by an outflow of the cerebrospinal fluid. Surgery of these injuries is simpler if it is possible to visualise an exact location of the fracture. Massive, difficult to control bleedings from the nasal cavity or other locations may be connected with disruption of a blood vessel running along the fissure of the fracture [15], e.g. fracture of the nasal septum, may injure the adjacent vascular-nervous bundle and result in haematoma. Fractures in the regions of the orifices of the paranasal sinuses may disturb their drainage, leading to secondary chronic inflammatory lesions and mucocele.
The symptoms of facial injuries include: pain, oedema, haematomas of the soft tissues of the facial area, face asymmetry and deformations, impaired mobility (of the mandible mainly), decreased patency or obstruction of the nasal ducts, impaired visual acuity, olfaction disturbances [4,16–18].
Physical examination includes the condition of soft tissues, asymmetry, local pain, abnormal mobility of the bones, sensory disturbances. Murmur in harmony with the heart rate, heard above the orbit, may be suggestive of a post-traumatic arteriovenous fistula. A detailed physical examination can provide us with a good insight into the patient’s condition. However, there is often a lack of cooperation from the patient’s side, his/her general health state is usually severe, or there exist other multiple injuries with a direct risk to patient’s life [18]. In such cases, a skilful diagnostic work-up may provide necessary information on the extent of pathological lesions, and reduce the time to treatment onset.
Aim of the work
The evaluation of the usefulness of multiplanar and three-dimensional reconstructions of CT images obtained with the use of a spiral, multi-row technique of data acquisition in the assessment of post-traumatic soft-tissue injuries of the face.
Determination which type of reconstruction of CT image is the most precise in assessing the severity and extent of injuries of facial soft tissues.
Material and Methods
The material was analysed as a part of a doctoral dissertation supervised by Stanislaw Skrzeklewski, MD PhD.
The clinical material included 67 patients referred for an emergency CT with a diagnosed facial injury, in order to have the location and extent of post-traumatic lesions assessed.
Among the study patients there were 58 men aged 8–71 years (mean of 34.7 years) and 9 women aged 21–74 years (mean of 42.7 years). In general, patients’ age ranged from 8 to 74 years (mean of 35.8 years).
Every patient underwent a CT with a Hispeed Qx/i unit made by GE. Due to planned secondary reconstructions in every case, a spiral technique of data acquisition in trans-verse plane was used.
The CT included the area of the face, from the upper border of frontal sinuses to the level of the chin.
Raw data were obtained by using the following technical parameters: voltage of the lamp – 120 kV, amperage of up to 200 mA, collimation – 1.25 to 2.5 mm, and pitch (the rate of table translation during a 360° rotation of the lamp to the thickness of the slice) of 1.5. Rotation time of 0.5–0.7 sec. Acquisition time did not exceed 30 sec. The speed of the table – 7.5 mm per one turn of the X-ray lamp.
In every patient, the initial evaluation was based on sections acquired in the transverse plane. The images were reviewed in soft-tissue windows (window parameters – 350/35 HU) and bone windows (window parameters – 2200/200 HU). The following field of view was used: 180–250 mm.
Next, in all cases, the following secondary reconstructions were conducted: secondary, 2D, multiplanar reconstructions (MPR) and 3D volume rendering on a graphical console ADW 4.0.
During the evaluation of post-traumatic lesions of soft tissues, the following was found:
- Herniations through fractures within medial and inferior orbital walls,
- – herniated oculomotor muscles,
- – herniated fat tissue,
Fluid in sinuses and nasal cavity,
Subcutaneous emphysema of soft tissues.
The clinical material including all patients was analysed three times, in different methodical groups, reflecting different methods of imaging and reconstruction.
In the first group, we assessed mainly the transverse sections, in the second group – 2D reconstructions, and in the third group – 3D reconstructions. Next, the sensitivity of transverse, planar, and 3D reconstructions in imaging soft-tissue pathologies in different locations was compared.
Statistical method
The statistical analysis of the obtained results was based on the Pearson’s chi2 test, which defined the differences between the incidence of positive diagnoses in the studied semiotic groups and the severity of the lesions. In order to test the hypothesis on correlation between the method of imaging of different facial post-traumatic lesions and their location, we selected (on the basis of the analysis of incidence) a reference study or studies (the highest number of diagnosed anatomical symptoms) with regard to which the following parameters were defined, characterising the remaining imaging techniques:
Diagnostic sensitivity is the rate (%) of patients in a study group with a positive test result. This reflects the ability of a given test to diagnose a disease:
Diagnostic specificity is the rate (%) of healthy individuals in a study group that obtained a negative test result.
Negative predictive value (NPV) is used to evaluate the probability of disease exclusion on the basis of negative study results:
Positive predictive value (PPV) allows for qualification (on the basis of a positive test result) of a given patient to a group of patients (with a certain probability).
PD – true positive results;
PU – true negative results;
FD – false positive results;
FU – false negative results.
The results were presented as ‘absolute incidence’. P of <0.05 was considered statistically significant.
The results obtained on the basis of the statistical analysis were used to test the hypothesis on the presence of a strict correlation between the selected method of imaging of different anatomical facial structures and the location of post-traumatic facial lesions (both of soft tissues and bones). The aim was to establish and confirm the value and place of different imaging techniques in the diagnostic algorithm, because some of them are perfect in diagnosing bone lesions, and others are irreplaceable when it comes to the evaluation of soft tissues.
Results
CT study of the facial cranium was conducted in every case. The obtained data were presented in the transverse presentation (TP). Multiplanar (2D) and volumetric (3D) reconstructions were performed secondarily.
In 25 cases (37.3%), there were herniations of soft-tissue elements through fractures to the paranasal sinuses. In 10 patients from this group (14.9%), there was herniation of fat tissue and oculomotor muscles, while in 15 patients (22.4%) there was herniation of fat tissue only. Fluid in paranasal sinuses and nasal cavity was observed in 48 (71.6%) cases. The presence of subcutaneous emphysema of soft tissues was present in 29 patients (43.3%).
The method (or methods) of image presentation and reconstruction with the highest absolute and significantly different number of diagnosed symptoms as compared to other methods of CT image processing, was considered to be the most useful from the diagnostic point of view. It was called a ‘reference’ method.
The evaluation of the location of soft-tissue complications
There was no difference found in the sensitivity of imaging of soft-tissue subcutaneous emphysemas and fluid in the sinuses, between the transverse plane and 2D multiplanar reconstruction, irrespective of the anatomical location of these pathologies.
In case of evaluation of herniations of soft tissues and oculomotor muscles to orbital fractures, a higher sensitivity was presented by 2D reconstructions than by transverse imaging. This was especially true for herniations of fat tissue and oculomotor muscles to fractures within the inferior wall of the orbit, with sensitivity for every above mentioned location amounting to 0.157895, 0.842105, and 0.75, respectively.
Only in case of herniation of a muscle to a fracture in the medial orbital wall, the 2D reconstruction and TP imaging revealed a similar sensitivity. The three-dimensional reconstruction was useless in imaging post-traumatic lesions of soft tissues (Tables 1–4).
Table 1.
Number of cases of soft tissue emphysema in a particular location, observed in different methods of reconstruction. Statistical significance.
| Location | Presentation | p | ||||
|---|---|---|---|---|---|---|
| TP | 2D | 3D | TP: 2D | TP: 3D | 2D: 3D | |
| Orbit | 19 | 19 | 0 | NS | p<0.05 | p<0.05 |
| Maxillary sinus | 11 | 11 | 0 | NS | p<0.05 | p<0.05 |
| Frontal sinus | 6 | 6 | 0 | NS | p<0.05 | p<0.05 |
| Mandible and temporomandibular joint | 4 | 4 | 0 | NS | p<0.05 | p<0.05 |
Table 4.
Number of cases of extraocular muscle impingement into fracture observed in different methods of reconstruction. Statistical significance.
| Location | Presentation | p | ||||
|---|---|---|---|---|---|---|
| TP | 2D | 3D | TP: 2D | TP: 3D | 2D: 3D | |
| Medial orbital wall | 3 | 3 | 0 | NS | p<0.05 | p<0.05 |
| Inferior orbital wall | 4 | 14 | 0 | p<0.05 | p<0.05 | p<0.05 |
Discussion
There was no difference in the sensitivity of imaging of soft-tissue subcutaneous emphysemas and fluid in the sinuses, between the transverse plane and 2D multiplanar reconstruction, irrespective of the anatomical location of these pathologies.
In case of evaluation of herniations of soft tissues and oculomotor muscles to fractures within the orbit, a higher sensitivity was presented by 2D reconstructions than by transverse imaging. This was especially true for herniations of fat tissue and oculomotor muscles to fractures within the inferior wall of the orbit.
Only in case of herniation of a muscle to a fracture in the medial orbital wall, the 2D reconstruction and TP imaging reveal a similar sensitivity. The three-dimensional reconstruction was useless in imaging post-traumatic lesions of soft tissues.
Three-dimensional reconstructions allow only for visualisation of bone structures. They do not visualise soft tissues and their fractures, that commonly accompany fractures of bone elements. At this point, we may risk a statement (that has already been presented by other authors [44]) that 3D reconstructions are useless in imaging of soft tissues. Although technically it is possible to visualise soft tissues with this method, image quality is definitely unsatisfactory for the operator. Physical density of the visualised tissues is connected with it. This kind of reconstructive imaging is useful in showing structures with maximally different physical densities (calcified bone elements in our case). Maybe in the future, with technological advancement of X-ray units, higher computing power of computers of the new generation, and the use of reconstructive software of a new quality, these disadvantages will be successfully overcome.
This limitation was also mentioned by Olszycki et al. [19]. The authors (analysing the cases of coexistent bone injuries and soft tissue injuries) define the 3D reconstruction as an auxiliary method of MPR reconstruction.
The efficacy of imaging of subcutaneous emphysemas and fluid in paranasal sinuses was similar for transverse presentations and 2D reconstructions (Figures 1, 2). Raw images allowed for measuring density of the examined tissues, which provided us with additional diagnostics data, helping in i.a. differentiation of the type of fluid contained in the sinuses. Differences in the diagnostic efficacy between the transverse presentation and 2D reconstruction were found during imaging of herniations of fat tissue and oculo-motor muscles into fractures running through the orbit, and especially through the inferior orbital wall. This phenomenon was confirmed by other authors [19–21]; (Figures 3–7). It should therefore be underscored that the 2D reconstruction performed in a plane freely selected by the operator allows in these cases for visualisation of the herniated soft tissues in their whole length, for evaluation of the extent of herniations and for diagnosis and localisation of the coexisting post-traumatic lesions, e.g. haematoma. Imaging of herniations within the lower orbital wall in the transverse plane, due to the parallel course of the bone lamella with regard to the examined plane, makes this method not too successful, and thus it is not recommended. However, when it comes to the assessment of herniations of the oculomotor muscle into fractures running through the medial orbital wall, 2D reconstruction and transverse imaging reveal a similar sensitivity (Figure 8). The usefulness of CT in the assessment of short- and long-term results of surgeries of facial injuries is also worth mentioning. This matter was discussed by Olszycki et al. [19,22]. In the available clinical material, there were cases of bone fragment repositioning and fixation with micro-plates, filling of the defects with bone slivers, disinvagination of soft tissues of the orbit, reconstruction of the defects of the inferior orbital wall with bone allografts or synthetic grafts. In the assessment of the location of bone fragments and grafts, the most useful method turned out to be the 3D reconstruction. The usefulness of 2D reconstructions was only slightly lower. However, in the assessment of soft tissue disinvaginations, the planar reconstruction had a considerable supremacy over other techniques of raw data processing.
Figure 1.

Axial CT scan. Left maxillary sinus filled with liquid. Soft tissue emphysema.
Figure 2.
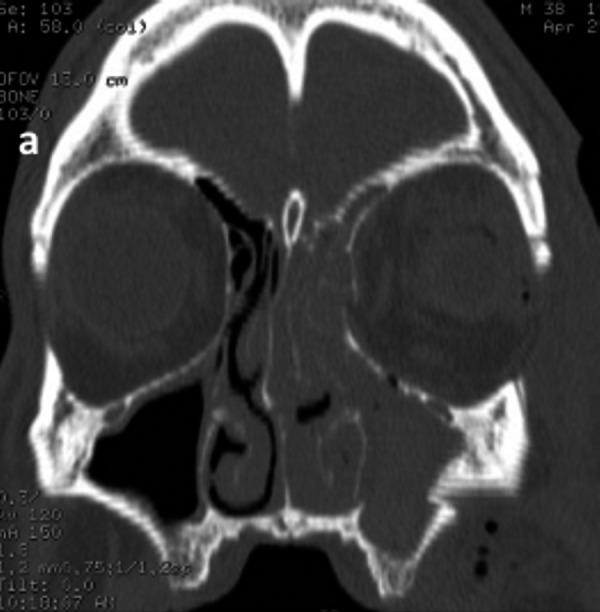
Multiplanar coronal reconstruction. Left maxillary sinus filled with liquid. Soft tissue emphysema.
Figure 3.
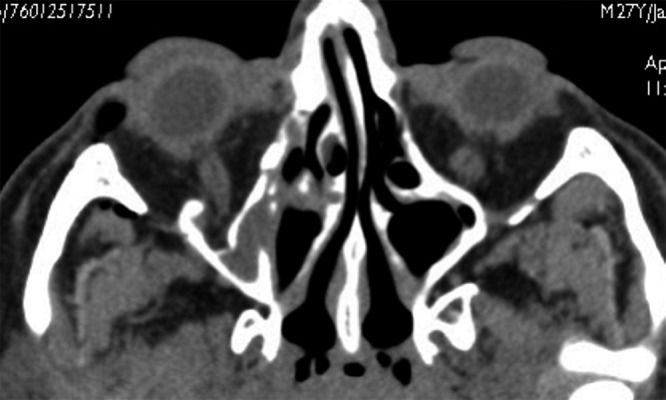
Axial CT scan. Fracture of the inferior wall of the right orbit with herniation of the orbital fat.
Figure 7.

Multiplanar sagittal reconstruction. Fracture of the inferior wall of the left orbit with herniation of the inferior rectus muscle.
Figure 8.

Axial CT scan. Fracture of the medial wall of the right orbit with herniation of the medial rectus muscle.
Conclusions
In the imaging of herniations of the orbital structures to the fractures (especially fractures within the inferior orbital wall), multiplanar reconstructions increase the diagnostic efficacy of CT.
In case of suspected herniations of the orbital soft tissues into the fractures, and before an elective surgery, the spiral CT with multiplanar 2D and 3D reconstructions should be the examination of choice in the diagnostic process.
Figure 4.
Multiplanar sagittal reconstruction. Fracture of the inferior wall of the right orbit with herniation of the orbital fat.
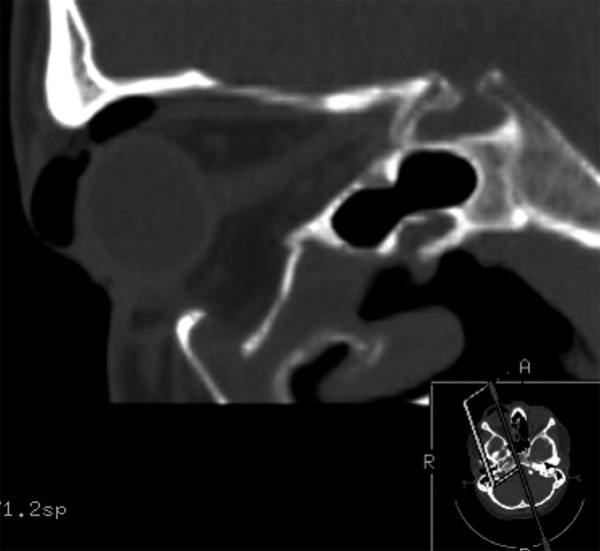
Figure 5.

Axial CT scan. Fracture of the inferior wall of the left orbit with herniation of the inferior rectus muscle.
Figure 6.
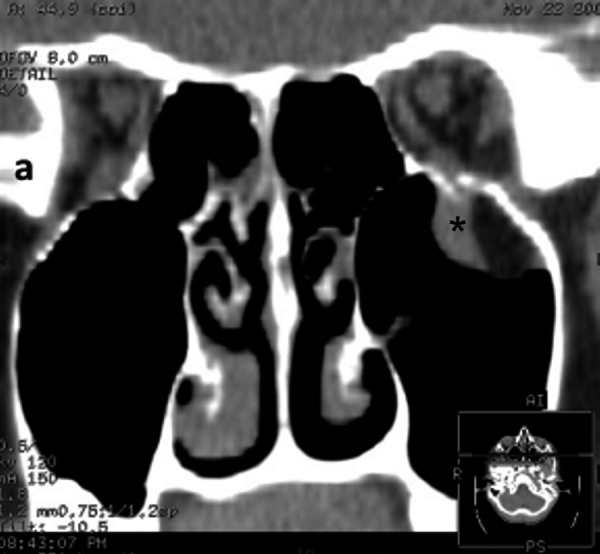
Multiplanar coronal reconstruction. Fracture of the inferior wall of the left orbit with herniation of the inferior rectus muscle.
Table 2.
Number of paranasal sinuses containing liquid observed in different methods of reconstruction. Statistical significance.
| Location | Presentation | p | ||||
|---|---|---|---|---|---|---|
| TP | 2D | 3D | TP: 2D | TP: 3D | 2D: 3D | |
| Frontal sinus | 23 | 23 | 0 | NS | p<0.05 | p<0.05 |
| Maxillary sinus | 48 | 48 | 0 | NS | p<0.05 | p<0.05 |
Table 3.
Number of cases of orbital fat tissue herniation observed in different methods of reconstruction. Statistical significance.
| Location | Presentation | p | ||||
|---|---|---|---|---|---|---|
| TP | 2D | 3D | TP: 2D | TP: 3D | 2D: 3D | |
| Medial orbital wall | 5 | 7 | 0 | NS | p<0.05 | p<0.05 |
| Inferior orbital wall | 6 | 22 | 0 | p<0.05 | p<0.05 | p<0.05 |
References:
- 1.Ellis E, III, Moos KF, El-Attar A, et al. Ten year of mandibular fractures: An analysis of 2,137 cases. Oral Surg. 1985;59:120. doi: 10.1016/0030-4220(85)90002-7. [DOI] [PubMed] [Google Scholar]
- 2.Haug RH, Prather J, Indresano AT. An Epidemiologic Survey of Facial Fractures and Concomitant Injuries. J Oral Maxillofac Surg. 1990;48:926–32. doi: 10.1016/0278-2391(90)90004-l. [DOI] [PubMed] [Google Scholar]
- 3.Turvey TA. Midfacial fractures: a retrospective analysis of 593 cases. J Oral Surg. 1977;35:887. [PubMed] [Google Scholar]
- 4.Wiesenbaugh JM., Jr Diagnostic evaluation of zygomatic complex fractures. J Oral Surg. 1970;28:204. [PubMed] [Google Scholar]
- 5.Helmy ES, Koh ML, Bays RA. Management of frontal sinus fractures. Oral Surg Oral Med Oral Pathol. 1990;69:137. doi: 10.1016/0030-4220(90)90314-i. [DOI] [PubMed] [Google Scholar]
- 6.Lynham AJ, Monsour FNT, Chapman PJ. Management of orbitozygomatic fractures. ANZ J Surg. 2002;72:364–66. doi: 10.1046/j.1445-2197.2002.02434.x. [DOI] [PubMed] [Google Scholar]
- 7.Lynham AJ, Hirst JP, Cosson JA, et al. Emergency department management of maxillofacial trauma. Emerg Med Austral. 2004;16:7–12. doi: 10.1111/j.1742-6723.2004.00536.x. [DOI] [PubMed] [Google Scholar]
- 8.Tadj A, Kimble FW. Fractured Zygomas. ANZ J Surg. 2003;73:49–54. doi: 10.1046/j.1445-2197.2003.02595.x. [DOI] [PubMed] [Google Scholar]
- 9.Bartkowski SB, Wyszyńska-Pawelec G, Zapała J. Patomechanizm, symptomatologia i diagnostyka złamania rozprężającego oczodołu. Okul. 2002;1:7–12. [in Polish] [Google Scholar]
- 10.Larsen M, Wieslander S. Acute orbital compartment syndrome after lateral blow-out fracture effectively relieved by lateral cantholysis. Acta Ophthalmol Scand. 1999;77:232–33. doi: 10.1034/j.1600-0420.1999.770225.x. [DOI] [PubMed] [Google Scholar]
- 11.Kubal WS. Imaging of Orbital Trauma. RadioGraphics. 2008;28:1729–39. doi: 10.1148/rg.286085523. [DOI] [PubMed] [Google Scholar]
- 12.Letson RD. Ocular injury. Otolaryngol Clin North Am. 1976;9:465–76. [PubMed] [Google Scholar]
- 13.Gentry LR, Manor WF, Turski PA, et al. High-resolution CT analysis of facial struts in trauma: 2 Osseous and Soft Tissue Complications. AJR. 1983;140(3):523–32. doi: 10.2214/ajr.140.3.533. [DOI] [PubMed] [Google Scholar]
- 14.Lund K. Fractures of the zygoma: a follow-up study on 62 patients. J Oral Surg. 1971;29:557–60. [PubMed] [Google Scholar]
- 15.Frable MA, El-Roman N, Lenis A, et al. Hemorrhagic complications of facial fractures. Laryng. 1974;84:2051–57. doi: 10.1002/lary.5540841119. [DOI] [PubMed] [Google Scholar]
- 16.Helmy ES, Koh ML, Bays RA. Management of frontal sinus fractures. Oral Surg Oral Med Oral Pathol. 1990;69:137. doi: 10.1016/0030-4220(90)90314-i. [DOI] [PubMed] [Google Scholar]
- 17.Niedzielska I, Łangowska-Adamczyk H, Borgiel-Marek H. Obrażenia części twarzowej czaszki doznane w wypadkach rowerowych. Czas Stomatol. 2000;53(3):181–87. [in Polish] [Google Scholar]
- 18.Holmgren EP, Dierks EJ, Bell RB, et al. Facial Soft Tissue Injuries as an Aid to Ordering a Combination Head and Facial Computed Tomography In Trauma Patients. J Oral Maxillofac Surg. 2005;63:651–54. doi: 10.1016/j.joms.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 19.Olszycki M, Kozakiewicz M, Arkuszewski P, et al. Wtórne rekonstrukcje obrazowe TK i MR zmian pourazowych części twarzowej czaszki. Pol J Radiol. 2004;69(3):94–99. [in Polish] [Google Scholar]
- 20.Novelline R, Rhea JT, Rao PM, et al. Helical CT in Emergency Radiology. Radiology. 1999;213:321–39. doi: 10.1148/radiology.213.2.r99nv01321. [DOI] [PubMed] [Google Scholar]
- 21.Sanderow B, Viccelio P. Fracures of the Medical Orbital Wall. Ann Emerg Med. 1988;17:973. doi: 10.1016/s0196-0644(88)80681-4. [DOI] [PubMed] [Google Scholar]
- 22.Olszycki M, Kozakiewicz M, Arkuszewski P. Evaluation of the post-traumatic lesions to the maxillary sinuses based on spiral CT reconstructions. Neurol suppl. 2001;1:77–78. [Google Scholar]


