Summary
Background:
The aim of the paper was to evaluate the usefulness of ultrasonographic examination in diagnosing laryngeal traumas, and monitoring the progress or complications in its treatment.
Material/Method:
In the years 2004–2009, 12 children, including 5 girls and 7 boys with laryngeal injuries, aged 5–12 years, were diagnosed and treated. In all the children, US examination of the neck and larynx, using a high-frequency linear transducer, as well as laryngoscopy and radiological examination of the cervical spine and chest were performed.
Results:
Blunt injury of the larynx was found in 12 children; in 9 children, the injury had been caused by hitting the neck against an obtuse object, 1 child had been kicked in the neck, and in one there had been an attempt of strangling. One of the children had sustained blunt injuries of the neck and chest in a traffic accident.
In US examinations, the findings included: unilateral lack of vocal cord mobility in 5 children, asymmetry in vocal cord mobility in 1 child, fractured thyroid cartilage with local hematoma in the affected area in 2 children, and thickened vocal cords in 5 children.
In radiological examination, the findings included: subcutaneous emphysema in the cervical area of the chest in 4 children, and mediastinal emphysema in 2 children with traumatic rupture of the trachea shown in laryngoscopy.
Conclusions:
US examination is helpful in the assessment of the extensiveness of laryngeal trauma, especially in the evaluation of vocal cord mobility, cervical cartilage and the soft tissues of the neck. A high level of conformity was demonstrated between the results of cervical US and the respective laryngoscopic findings.
US examination does not allow to differentiate between vocal cord paralysis and their immobilization.
Keywords: larynx, trauma, ultrasound, children
Background
Traumas of the larynx are rare in children. Every trauma of the larynx requires hospitalization and clinical treatment. Even with initially insignificant symptoms, the patient with laryngeal trauma remains exposed to a direct life threat due to the possibility of respiratory occlusion and cardiogenic shock. The clinical symptoms do not always correlate with the severity of the respiratory injury. A blunt injury of the neck (a blow) may lead to injuries of: laryngeal cartilages, vocal cords, mucous membrane with-in the larynx and trachea, with disruption of the mucous membrane and deeper structures, as well as an incomplete dislocation of the crico-arytenoid articulations.
Material and Methods
In the years 2004–2009, 12 children, including 5 girls and 7 boys, aged 5–12 years, were diagnosed and treated for an external, blunt injury of the larynx.
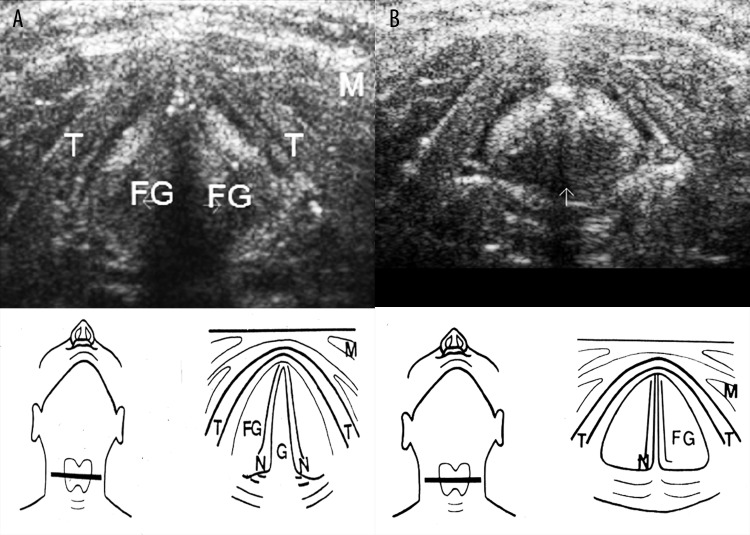
All of the children underwent ultrasonography of the neck and larynx, with a high-frequency linear transducer. The examination was carried out without any special preparation or sedation. The following was evaluated: soft parts of the neck, muscles, presence of abnormal fluid spaces, e.g. hematoma, epiglottis, reverse v-shaped thyroid cartilage, its outline and structure, as well as potential injuries (fractures), location and movements of arytenoid cartilages which are visualized as hypoechoic triangular structures below vocal cords. The mobility of the vocal cords was evaluated and registered (Figure 1) [1].
Figure 1.
Normal vocal cord mobility in US examination: (A) open glottis, (B) closed glottis. T – thyroid cartilage, FG – vocal cords, G – glottis, M – muscles.
All the children with cervical injuries had laryngoscopy. In order to assess the mobility of the vocal cords, the examination was initially performed in slight sedation, without muscle relaxation, and then in deep sedation, in order to evaluate the structures of the larynx macroscopically. X-rays (in selected CT cases) of the cervical spine and chest were carried out.
Clinical observations and follow-up US examinations of the larynx, as well as laryngoscopy in some selected cases were performed within 2 years following injury.
Results
Larynx injury was found in 12 children; in 9 children, the injury had been caused by hitting the neck against an obtuse object (edge of a cabinet or windowsill, back of the chair, metal rail, handlebars of a bicycle or a scooter, hanging rope), 1 child had been kicked in the neck, and in one there had been an attempt of strangling (pressure). One of the children had sustained blunt injuries of the neck and chest in a traffic accident.
The main clinical symptom was the shortness of breath (in 8 children), hoarseness (in 5 cases), low voice (3), change in vocal timbre or aphonia (3), pain (with swallowing in this case) (2), cough and hematoptysis (1). The location of the laryngeal injuries was shown in Table 1.
Tabela 1.
Location of laryngeal injuries in 12 children.
| Location of injury | Complex injury | Numer of children |
|---|---|---|
| Epiglottic | 2 | |
| Glottic level | 3 | |
| Subglottic | 1 | |
| Glotto-epiglotic | 2 | |
| Glotto-subglottic | 3 | |
| Glotto-supra and -subglottic | 1 |
US examinations showed a unilateral paralysis of the vocal cords in 5 children. A bilateral vocal cord immobility was developed in the follow-up period in 1 child. Asymmetry in vocal cord mobility was found in 1 child. Laryngoscopy found a unilateral lack of vocal cord mobility in 5 children, adhesions at the posterior commissure in 3 children, and a partial adhesion of the vocal cords in one case. Abnormal, asymmetric, unilateral position of the arytenoid cartilages was found in US and laryngoscopy in 5 children.
Thickening of the vocal cords was found on US in 5 children. In this group, laryngoscopy found an edema of the vocal cords in 3 children, and a hematoma in 2.
In 2 children, the fracture of the thyroid cartilage with hematoma of this region was revealed with US only.
In 2 children, X-rays showed a mediastinal emphysema, with a post-traumatic fracture of the trachea found in laryngoscopy. Subcutaneous edema of the thorax and neck was found on X-rays of 4 children, with a laryngeal injury of different degree. The severity of laryngeal and tracheal injuries was shown in Table 2.
Tabela 2.
The degree of changes in 12 children with laryngeal injuries, Schaefer's Scale.
| Degree | Symptoms | Numer of children |
|---|---|---|
| I | Small intralaryngeal hematoma, edema without a fracture of the laryngeal cartilage | 4 |
| II | Edema, hematoma, minor damage to the mucosa, fracture without a dislocation of the laryngeal cartilage | 3 |
| III | Massive edema, mucosal disruption, immobilized vocal cords, cartilage damage | 4 |
| IV | I-III changes, massive damage to the mucosa and laryngeal nerves, two or more fractures | 1 |
| V | Complete disruption of the laryngeal structures | – |
All 12 children with laryngeal injury were hospitalized. On the basis of the clinical picture and performed examinations, 4 children with an insignificant laryngeal injury were treated conservatively. In the group of 8 children with a severe laryngeal injury, the following was performed: tracheostomy in 2, a few days of intubation in 4, multiple incisions of the adhesions at the posterior commissure and between the vocal cords in 3.
Good treatment results with symptom resolution were obtained in 6 children. An invasive treatment – intubation, tracheotomy, incision of the scars and adhesions – was introduced in 6 cases with an injury of the 3rd and 4th degree, according to the Schaefer’s scale.
In the group of 5 children with abnormal mobility of the vocal cords, normal mobility was obtained only in 1 child with primarily asymmetric movements of the vocal cords. Treatment results were included in Table 3.
Tabela 3.
Results of treatment in 12 children with laryngeal injury – up to 24 months of a follow-up.
| Degree | Number of children | Regression of symptoms | Improvement | No improvement |
|---|---|---|---|---|
| I–II | 7 | 6 | 1 | – |
| III–IV | 5 | – | 2 | 3 |
Discussion
Laryngeal injury may become a life-threatening condition due to the disturbed patency of the respiratory tracts or cardiogenic shock resulting from bradycardia, arrhythmia, low blood pressure, or circulatory arrest. This is closely connected with tracheal innervation with the vagus nerve, through the laryngeal nerves. The right vagus nerve supplies the sinal node, left atrio-ventricular node. Thus, every patient with larynx injury should be hospitalized [2–4].
Larynx injuries are rare and constitute approx. 1% of all body injuries. Patient’s state, potential complications, and type of treatment depend on the type of injury, which can be classified according to its mechanism, degree, or location [4].
Injuries of the larynx may be divided into the external and internal ones. The external injuries are caused by a blow or pressure on the anterior part of the neck. The internal laryngeal injuries are more frequent in children than the external ones, and are caused by a prolonged or post-traumatic intubation, laryngoscopy, bronchoscopy, foreign body, or a burn. Open injuries (rare in children) are mostly penetrating.
Classification according to the location of the laryngeal injury includes: epiglottic, glottic, subglottic, or complex injury, including more than one location.
Laryngeal injuries in adults result usually from traffic accidents (with motorcycle mostly), sports accidents, e.g. hockey, and accidents connected with the use of firearm [4,5].
In children, laryngeal injuries are less common than in adults. They occur during games, sports (bicycle, scooter), fall with hitting an edge of an object (furniture, handlebars) with a neck. They tend to be initially undiagnosed. Clinical symptoms of the laryngeal injury, such as change in voice timbre, aphonia, may appear with delay. The risk of external laryngeal injuries in children is different than in adults.
Larynx of children, especially the young ones, differs from the larynx in adults. The differences concern its size, structure, and location. In children, the larynx is situated higher than in adults. The smallest diameter of the larynx in children can be observed at the level of C3 spine; in adults – at C7. Owing to this, the larynx is protected in children by the mandible.
The larynx is smaller in children, and the glottis is narrower. That is why, in case of edema of this region, the disorders of airway patency are more frequent in this group of patients [1,5]. The size of the larynx differs individually. The length of the glottis vera in an adult man is approx. 23 mm, while in newborns this is about 6 mm, and 3 mm in width. The larynx grows until the age of 5–6 years, and then the development follows in the period of maturation [1].
In adults over 18 years, the thyroid cartilage undergoes the process of ossification and calcification, starting with its apex, and then its central part. Due to elasticity and resilience of the laryngeal cartilages in children, fractures of the laryngeal cartilages are less frequent than in adults, and the chips are usually not dislocated. However, this also leads to insufficient protection from external injuries of the neck. Due to a fall, blow, or pressure of the anterior neck, the larynx may dislocate towards the rigid spine. In the course of injury, there may follow a mechanical damage of the vocal cords, injury of the laryngeal nerves, vocal cord paralysis, injury of the crico-arytenoid articulation or artyneoid cartilage, disruption of the mucosa, ligaments, and soft tissues [2,6,7].
Primary immobilization or vocal cord paralysis, as well as secondary immobilization of the vocal cords due to adhesions, are relatively common in children. The treatment is difficult and long. Mobility of the vocal cords may show no improvement for many years.
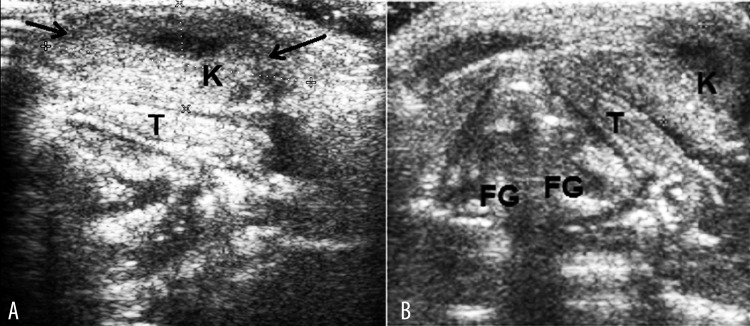
The presented group of 12 cases includes external, blunt injuries of the larynx. Injury location influences its severity. An epiglottic injury (Figure 2) may result in the fracture of the thyroid cartilage and the hyoid bone.
Figure 2.
A 12-year-old boy hit his neck against a rope. Hematoma (K) in the thyroid cartilage (T) area (A, B).
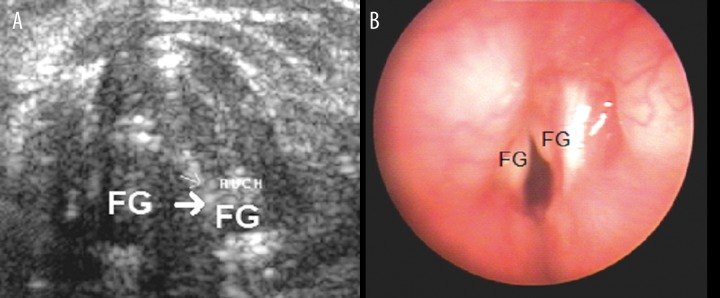
Fracture of the thyroid cartilage is usually horizontal, and causes inspiratory dyspnea. It may also lead to disturbed patency of airways. Usually, there follows also a rupture of the crico-arytenoid ligaments. There may appear a fistula, from false vocal cords to the anterior part of the neck, leading to a subcutaneous edema. A unilateral or bilateral paralysis or immobilization of the vocal cords may develop as well. Laryngeal injury may lead to a fracture of the thyroid cartilage at the level of a fusion of the vocal cords, to dislocation of the chips, and injury of the laryngeal nerves. It usually also leads to the paralysis of the vocal cords. Clinically, there is weakening and change in vocal timbre or aphonia. Disturbed patency of the airways is caused by edema or hematoma of the vocal cords (Figure 3). Circular scars may also appear.
Figure 3.
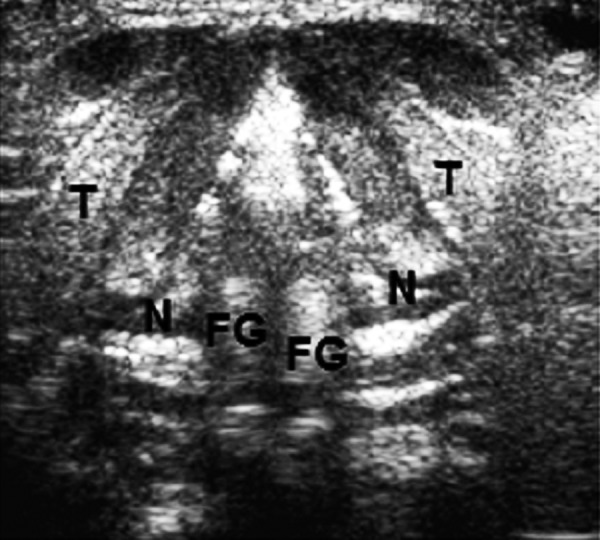
A 6-year-old boy. Injury after his neck hit a bicycle handlebar. US: thickened vocal cords. (FG). Laryngoscopy: extravasations in the laryngeal vestibule, arytenoid cartilage (N) in normal position.
Subglottic injury – fracture of the cricoid cartilage and of the first tracheal cartilages may lead to tracheal injuries, subglottic edema, and paralysis of the vocal cords (Figure 4). Scars and adhesions of this region are common. Impairment of the recurrent laryngeal nerve may lead to hoarseness. Complex injuries (Figure 5), i.e. including more than one level (e.g. glotto-subglottic, glotto-epiglottic), are usually more difficult to treat.
Figure 4.
A 9-year-old boy, neck injury after hitting a cabinet edge. US (A) – the right vocal cord immobilized (FG). Laryngoscopy (B) – lack of mobility and hematoma in the right vocal cord.
Figure 5.
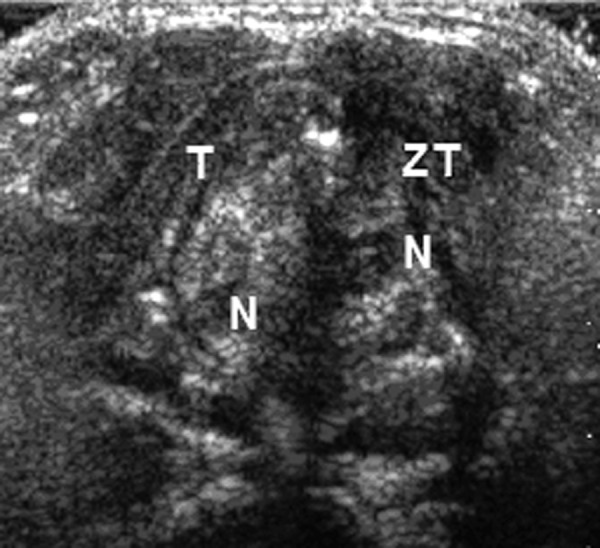
A 5-year-old girl. Injury after her neck hit a scooter handlebar. US – dislocated fracture with hematoma of the thyroid cartilage (ZT); left vocal cord immobilized, dislocation of the left arytenoid cartilage (N).
Types and locations of the laryngeal injuries in 12 children were shown in Table 1. The range of external injury of the larynx on the basis of the Schaefer’s scale [4,5] was presented in Table 2.
In every patient after an injury of the anterior neck, the search for fractures of the laryngeal and tracheal cartilages bases on US and X-ray examinations of the neck.
Fracture of the thyroid cartilage can be well visualized with US (2 children in the study group). Laryngoscopy may reveal only fractures with herniation and dislocation of the chips.
Dislocation of the arytenoid cartilages was found in US examination and laryngoscopy (5 children). Unilateral paralysis (immobilization) of the vocal cords was found in 4 children. There was also one case of a visible asymmetry in vocal cord mobility found on US and confirmed by laryngoscopy under slight narcosis, without muscle relaxation. In the selected group of patients, this was the first stage of examination (laryngoscopy), followed by a deep sedation. We obtained a full conformity between US and laryngoscopy results as regards the mobility of the vocal cords, and location of the arytenoid cartilages.
It should be underscored that laryngoscopy is performed in children under general anesthesia. The evaluation of all levels of the larynx, with subglottic area, and introduction of a potential treatment requires deep sedation, without laryngeal reflexes. However, the evaluation of the vocal cord mobility is unable then.
Ultrasonography does not require any special preparation, and visualizes the mobility of the vocal cords and arytenoid cartilages, asymmetric positioning of arytenoid cartilages, thickening of the vocal cords, fractures of the thyroid cartilage, and hematomas of this region very well.
Not all laryngeal structures can be well visualized on US. Epiglottis is visible only partially – only its apex. The subglottic region is difficult to evaluate because it is filled with air and thus its assessment with this imaging method is limited (only the anterior and lateral walls are visible) [1,8].
Laryngoscopy visualizes very well the following structures: epiglottis, internal structures of the larynx, subglottic region, trachea, scars, and intralaryngeal adhesions. During laryngoscopy, such treatment procedures can be performed as incisions of adhesions and scars. However, the evaluation of vocal cord mobility is very difficult with this method, or even impossible, due to deep sedation. A procedure requiring a slight sedation at the beginning, followed by a deep narcosis, is usually anesthesiologically complicated and thus ultrasonography and laryngoscopy perfectly complement each other.
In diagnostically difficult situations, CT of the neck or MRI can be performed. However, vocal cord mobility is best assessed with US [1,8].
Treatment of the laryngeal injury depends on patient’s state, and range of injury. It is always necessary to keep the patency of airways, to stop hemorrhages and to protect the cervical spine.
In 6 children who were diagnosed with a laryngeal injury of the 1st and 2nd degree according to the Schaefer’s scale, only a conservative treatment was used. Ultrasonography and laryngoscopy showed in this group of patients: a unilateral edema of arytenoid cartilages, extravasations in the laryngeal vestibule and on vocal cords, hematoma in the region of the thyroid cartilage, injury of the mucous membrane without any impairment of the respiratory tract, fracture of the thyroid cartilage without dislocation in this group of children.
Invasive treatment – intubation, tracheotomy, incisions of the scars and adhesions – was introduced in 6 children with an injury of the 3rd and 4th degree according to the Schaefer’s scale.
Tracheostomy to create an open airway was performed in 2 children with extensive adhesions between the vocal cords and within the region of posterior commissure, as well as with vocal cord immobility.
Intubation was maintained for a few days in 4 children, including 2 with post-traumatic rupture of the trachea and scars in the subglottic region, and with vocal cord immobility. Incisions of the scars and adhesions was performed several times in 4 children. Good treatment outcomes with symptom resolution were found in were achieved in 6 out of 7 children with an injury of the 1st and 2nd degree, in the Schaefer’s scale.
The worst treatment results were obtained in the group of 5 children with abnormal mobility of the vocal cords (4 children with unilateral immobilization). Normal mobility was obtained in 1 child with asymmetric movements of the vocal cords. An improvement was found in 1 child. No improvement was observed in 3 children in the long treatment process (up to 24 months since injury). Treatment results were presented in Table 3.
There is no one pattern of medical management in injuries of the larynx in children. Indications are established for every case individually, depending on the general health state, symptoms, and range of injury. In children, a relatively insignificant neck injury during play or due to a fall or blow may cause damage to vocal cords with no return to a normal function.
Thus, an insignificant neck injury may pose a threat to a child’s life and cause many complications which require multiple procedures, treatment, or long-term rehabilitation. An early-introduced treatment may prevent from or decrease the granulation of tissues, as well as the formation of scars and adhesions [2,9–11].
Conclusions
Every injury of the larynx is a clinical condition requiring hospitalization.
Ultrasonography is helpful in the assessment of vocal cord mobility, fractures of the laryngeal cartilages, and post-traumatic lesions of soft tissues.
Significant consistence was demonstrated between the ultrasonography and laryngoskopy findings, both examination results being complementary.
Ultrasonography is not able to differentiate between the paralysis of the vocal cords and a secondary immobilization, e.g. by adhesions between the cords.
In laryngoscopy, the evaluation of vocal cord mobility is limited by anesthesia.
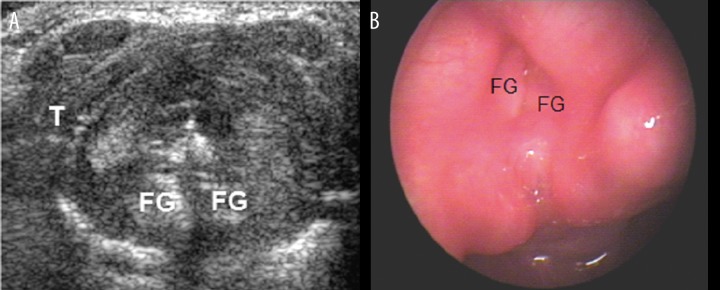
Figure 6.
A 7-year-old girl injured after hitting her neck against a metal bar. US (A) – 6 weeks after injury, bilateral immobilization of vocal cords.(FG), laryngoscopy (B) – scars in the area of posterior commissure; vocal cord adhesion.
References:
- 1.Jakubowska A, Brzewski M, Piórkowska D, et al. Ultrasonografia krtani i jej okolicy u dzieci. Część I. Anatomia ultrasonograficzna. Pol Przegl Radiol. 1998;63(4):337–41. [Google Scholar]
- 2.Myer CM. Trauma of larynx and craniofacial structures: airway implications. Pediatric Anesthesia. 2004;14:103–6. doi: 10.1046/j.1460-9592.2003.01198.x. [DOI] [PubMed] [Google Scholar]
- 3.Andrews T. Laryngeal trauma. In: Cotton R, Myer C, editors. Practical Pediatric Otolarongology. Lippincott-Raven; Philadelphia-New York: 1998. pp. 927–32. [Google Scholar]
- 4.Brown P, Schaefer S. Laryngeal and esophageal trauma. In: Cummings CW, et al., editors. Otolaryngology-Head and Neck Surgery. Mosby; St. Luis: 1993. pp. 1864–73. [Google Scholar]
- 5.Butler A, Wood B, ORourke A, et al. Acute External Laryngeal Trauma: Experience With 112 Patiens. Am Otol Rhino Laryngol. 2005;114:361–68. doi: 10.1177/000348940511400505. [DOI] [PubMed] [Google Scholar]
- 6.Pearson S, Rimmel F. Bluestone CD. Pediatric Otolaryngology. Saunders; Philadelphia: 2003. Injuries to the lower respiratory tract; pp. 1511–18. [Google Scholar]
- 7.Kleinsasser N, Priemer F, Schulze W, et al. External trauma to the larynx: classification, diagnosis, therapy. Eur Arch Otorhinolaryngol. 2000;257:439–44. doi: 10.1007/s004050000263. [DOI] [PubMed] [Google Scholar]
- 8.Friedman EM. Role of ultrasound in assessment of vocal cord function in infants and children. Ann Otol Rhinol Laryngol. 1997;106:199–209. doi: 10.1177/000348949710600304. [DOI] [PubMed] [Google Scholar]
- 9.Gold SM, Gerber ME, Shott SR. Blunt Laryngotracheal trauma in children. Arch Otolaryngol Head Neck Surg. 1997;123(1):83–87. doi: 10.1001/archotol.1997.01900010093014. [DOI] [PubMed] [Google Scholar]
- 10.Kurien M, Zahariah N. External laryngotracheal trauma in children. Int J Otorhinolaryngol. 1999;49(2):115–19. doi: 10.1016/s0165-5876(99)00109-3. [DOI] [PubMed] [Google Scholar]
- 11.Merritt RM, Bent JP, Porubsky ES. Acute laryneal trauma in the pediatric patient. Ann Otol Rhinol Laryngol. 1998;107(2):104–6. doi: 10.1177/000348949810700204. [DOI] [PubMed] [Google Scholar]