Summary
Background:
Peyronie’s disease (PD) is characterized by the formation of fibrous tissue plaques within the tunica albuginea, usually causing a penile deformity and a subsequent erectile dysfunction. Diagnosis of PD is based on medical and sexual history, physical examination and imaging examinations, i.e.: ultrasound, color Doppler ultrasound, magnetic resonance and X-ray mammography.
Material/Methods:
Ultrasound appears superior to all other methods for depicting calcifications, with the detection rate of 100%. It is safe, non-invasive, repeatable and reliable. It should be a method of choice in most standard cases of Peyronie’s disease.
With color Doppler ultrasound (CDU), one can find hyperperfusion around the plaques as a sign of inflammation in the active state of the disease. CDU is useful in diagnosing erectile dysfunction which is observed in most cases of PD.
Results:
MR is superior to US and X-ray as regards the detection of periplaque inflammation, though this information can be obtained from medical history and penile plaque palpation. MR, being an expensive imaging modality, should be reserved for special cases, i.e.: plaques located at the penile basis, a suspicion of malignant disease, and prior penile surgery.
Conclusions:
X-ray mammography is the most accurate in showing calcifications as well as the angle of penile curvature. However, the possibility of obtaining this information does not justify the use of ionizing radiation for that purpose.
Keywords: Peyronie’s disease, imaging modalities, ultrasonography, Color Doppler, Magnetic Resonance, X-ray mammography
Definition and Etiology
Peyronie’s disease (induratio penis plastica, penile fibromatosis) is an inflammatory condition characterized by a hard fibrous layer of scar tissue (plaque) that develops in the tunica albuginea of the penis. The plaque causes a painful penis deviation and erectile dysfunction.
The disease was fully described in 1561 by Francois Gigot de la Peyronie [1]. The incidence of Peyronie’s disease (PD) ranges from 1% to 3.2%. Its etiology is unknown. Common, suspected causal factors include sexual trauma in individuals with a genetic predisposition to aberrant wound healing, as a part of generalized disease of the connective tissue, autoimmune system or arteries.
The disease affects men in their mid-age, usually between 40 and 60 years old. The oldest diagnosed patient presented in the literature was 80 years old, while the youngest 18 [2].
Diagnostics of Peyronie’s Disease
The diagnosis is based on medical history, symptomatology, penis palpation, ultrasonography, magnetic resonance imaging (MRI), and X-ray in mammographic technique.
The most characteristic symptoms are:
presence of a plaque or thickening of the tunica albuginea,
penile deviation,
pain of a flaccid and/or erect penis,
erectile dysfunction [3].
The plaque is usually located in the penile dorsum or lateral dorsum, causing typical dorsal or lateral-dorsal deviation. Rarely it is located on the ventral side of the penis. Morphologically, an inflammatory reaction with thickening of the tunica albuginea in the beginning and formation of a fibrotic, often calcified plaque at later stages are typical [4]. Sometimes, the plaque can be missed during palpation, even when calcified. In more advanced stages, penile fibrosis may occur.
In the initial acute phase, the patient may suffer from pain of a flaccid and/or erect penis. Sexual intercourse is impossible when penile deviation exceeds 45 degrees. Although an extensive angulation, painful erection, tenderness of the plaque and performance anxiety may all contribute to erectile dysfunction (ED), it was shown that veno-occlusive dysfunction and arterial disease are responsible for ED in the majority of cases [5,6].
The natural history of PD is variable. It usually starts with an acute phase and, after a few months, it tends to develop into a non-inflammatory, chronic state. Spontaneous resolutions have been described (but most of patients experience disease progression). Treatment depends on the stage of the disease [7].
Ultrasonography
This technique can accurately identify and measure calcifications. Fibrous plaques can sometimes be visualized, but they can be easily mistaken for a thickening of the tunica albuginea. In ultrasound technique with density profiles, three distinct patterns can be identified. Type 1: The plaque appeared as a thickening of the tunica albuginea without acoustic shadowing. Type 2: A moderately calcified plaque with a typical ultrasound shadow. Type 3: A severely calcified plaque with typical ultrasound shadowing (Figure 1). Other imaging techniques, i.e. X-ray and MR, can only differentiate between the calcified and noncalcified plaques [8]. Calcifications are signal-free on MR (Figure 2). Tunica albuginea also shows a very low signal intensity or is nearly signal-free and thus the identification of calcified structures in and around the tunica albuginea is practically impossible with MR. Ultrasound appears to be superior to all other methods in depicting calcifications, with the detection rate of 100% [9]. It has a sensitivity of 100% in detecting calcified plaques. Non-calcified plaques can also be seen. Moreover, the plaque can be measured precisely. In standard cases of Peyronie’s disease, one can rely upon ultrasound examination which visualizes the tunica albuginea in all stages of the disease.
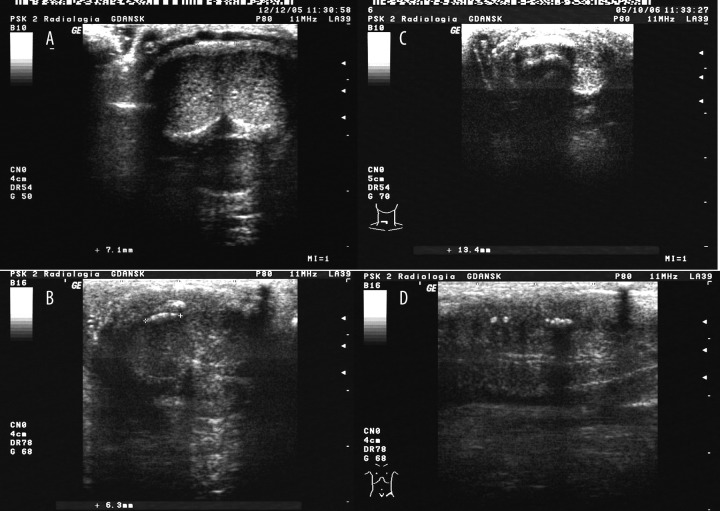
Figure 1.
Ultrasound image of the penis in a patient with Peyronie’s disease. (A) a plaque of type 1 – a typical thickening of the tunica albuginea without acoustic shadowing. (B) a plaque of type 2 – a moderately calcified plaque with slight acoustic shadowing. (C) a plaque of type 1 – a severely calcified plaque with typical shadowing. (D) 2 plaques – one of type 2 and one of type 3.
Figure 2.

(A) T1-weighted MR image of a calcified plaque showing a typical signal-free structure at the dorsum of the penis. (B) T2-weighted MR image of the same plaque. (C) Ultrasound image of the same plaque showing a typical calcified plaque with acoustic shadowing.
Color Doppler Ultrasound
With the power mode, it is possible to detect hyperperfusion around the plaques as a sign of inflammation in the active state of the disease. This is in contrast to the so called ‘burnt-out’ situation in which inactive plaques show no sign of hyperperfusion [10].
However, the most important role of Color Doppler is erectile dysfunction (ED) evaluation. As many as 70.6% of PD patients complain of ED. Penile vascular disease can be detected with Color Doppler in 60–70% of PD patients. Arterial disease was found in 44–52% of Peyronie’s patients with ED, while veno-occlusive dysfunction (VOD) in 30–86% (Figure 3). It seems uneasy to find the predominant pathology determining the erectile status in every case [5].
Figure 3.
(A) Color Doppler examination after intracavernous injection of 10 μg of prostaglandin E1 in a healthy man. (B) Color Doppler examination after intracavernous injection of 10 μg of prostaglandin E1 in Peyronie’s patient having mixed (arterial and venous) vascular disease. The PSV value of 16 cm/s is below the cut-off value of 35 cm/s and is considered to be diagnostic for penile arterial disease. VOD was conducted in patients with both EDV >5 cm/s and RI <0.9.
Penile CDU provides reliable information on hemodynamic changes involved in ED, and allows to individualize therapeutic options in patients with Peyronie’s disease and concomitant erectile dysfunction [5,6,10].
Magnetic Resonance Imaging
In Peyronie’s disease, MR is a non-invasive imaging method which provides additional information about inflammatory changes. [11] MRI is superior to US and X-ray concerning the detection of inflammation and it might be carried out using gadolinium-DTPA to show inflammation as perifocal signal enhancement in cases of calcified plaques, and diffuse enhancement in cases of non-calcified plaques (Figure 4). MR provides a detailed evaluation of penile anatomy, an extremely accurate presentation of irregularities of the tunica albuginea, as well as deformities of corporal bodies [8]. MR should be a modality of choice when penile prosthesis implantation is planned.
Figure 4.

(A) T2-weighted MR image of a calcified plaque on the right side, at the dorsum of the penis. (B) T2-weighted MR image after intravenous gadolinium administration showing its mild enhancement corresponding to inflammatory plaque.
MRI can expose more plaques at the penile basis. They can be missed on palpation and US because the cavernous structures in this region are partially covered by the pubic bone or the infra-pubic fat.
Moreover, in case of any doubts on the diagnosis of Peyronie’s disease, MR can exclude malignant processes which constitute a rare differential diagnosis [9].
X-ray Mammography
In our opinion, this method shows calcifications and the angle of penis curvature most accurately. However, plaques of mostly fibrous structure cannot be shown accurately (Figure 5). It is generally agreed that US can detect calcifications but not all in one image. Moreover, X-ray pictures showed them more clearly, and it was possible to visualize them with one image and even count them (Figure 6).
Figure 5.
(A) X-ray of a non-calcified plaque, i.e. not visible. (B) Ultrasound examination of the same patient showing a typical thickening of the tunica albuginea (between markers).
Figure 6.
(A) X-ray of the penis with lateral dorsal deviation caused by a strongly calcified plaque at the dorsum. (B) Ultrasound examination of the same patient showing the same plaque with typical shadowing.
Some authors believe that information gained by means of this method does not justify the use of ionizing radiation for that purpose [10].
Conclusions
In our opinion, the best method to diagnose Peyronie’s disease is penis palpation and to study patient’s medical history.
Among various imaging modalities, ultrasound should be the method of choice in diagnosing Peyronie’s disease and treatment planning because it is accurate, easily available, cost-effective, and non-invasive, and it has no side effects as compared to X-ray and MR.
MR should be reserved for special cases, i.e.: plaques located at the penile basis, a suspicion of malignant disease, and prior penile surgery.
References:
- 1.Ralph DJ, Minhas S. The management of Peyronie’s disease. BJU International. 2004;93:208–15. doi: 10.1111/j.1464-410x.2004.04587.x. [DOI] [PubMed] [Google Scholar]
- 2.Chilton CP, Castle WM, Westwood CA, et al. Factors associated in the aetiology of Peyronie’s disease. Br J Urol. 1982;54:748–50. doi: 10.1111/j.1464-410x.1982.tb13640.x. [DOI] [PubMed] [Google Scholar]
- 3.Williams JL, Thomas GG. The natural history of Peyronie’s disease. J Urol. 1970;108:75. doi: 10.1016/s0022-5347(17)61894-9. [DOI] [PubMed] [Google Scholar]
- 4.Gelbard MK, Dorey F, James K. The natural history of Peyronie’s disease. J Urol. 1990;144:1376. doi: 10.1016/s0022-5347(17)39746-x. [DOI] [PubMed] [Google Scholar]
- 5.Kadioglu A, Tefekli A, Erol H, et al. Color Doppler ultrasound assessment of penile vascular system in men with Peyronie’s disease. Int J of Impot Res. 2000;12:263–67. doi: 10.1038/sj.ijir.3900569. [DOI] [PubMed] [Google Scholar]
- 6.Levine LA, Coogan CL. Penile Vascular Assessment Using Color Duplex Sonography in Men with Peyronie’s Disease. J Urol. 1996;155(4):1270–73. [PubMed] [Google Scholar]
- 7.Miekos E. Stwardnienie plastyczne pracia. Przegl Urol. 2003;4(20):28–32. [in Polish] [Google Scholar]
- 8.Andersen R, Wegner HEH, Miller K, et al. Imaging modalities in Peyronie’s disease. Eur Urol. 1988;34:128–35. doi: 10.1159/000019698. [DOI] [PubMed] [Google Scholar]
- 9.Hauck E, Hackstein N, Vosshenrich R, et al. Diagnostic Value of Magnetic Resonance Imaging in Peyronie’s disease-a comparsion both with palpation and ultrasound in the evaluation of plaque formation. Eur Urol. 2003;43:293–300. doi: 10.1016/s0302-2838(03)00003-4. [DOI] [PubMed] [Google Scholar]
- 10.Fornara P, Gerbershagen HP. Ultrasound in patients affected with Peyronie’s disease. World J Urol. 2004;22:365–67. doi: 10.1007/s00345-004-0424-x. [DOI] [PubMed] [Google Scholar]
- 11.Vosshenrich R, Schroeder-Printzen I, Weidner W, et al. Value of magnetic resonance imaging in patients with penile induration (Peyronie’s disease) J Urol. 1995;153:1122–25. [PubMed] [Google Scholar]