Summary
Background:
A suspicion of ventriculo–peritoneal shunt failure is classified as the most common indication for CT in children with hydrocephalus. The main target of the study was to evaluate the diagnostic value of a low-dose protocol and to compare a total DLP received by patients in compared protocols.
Material/Methods:
Our retrospective analysis included 256 examinations performed in patients aged from 1 month to 18 years, with body mass ranging from 3 to 100 kg. The examinations were conducted in the years 2009–2011. A total number of 128 examinations were performed on the basis of the low-dose protocol and 128 according to a standard protocol using the Siemens SOMATOM Definition AS 128-slice scanner.
Results/Conlusions:
The analysis showed a full value of the diagnostic low-dose protocol with a simultaneous decrease of the total dose of DLP to the average of 40%.
Application protocol with lower mAs in assessing the causes of ventriculo-peritoneal shunt failure in children with hydrocephalus is coherent with the valid principles of radiation protection in pediatrics and reduces the total DLP while maintaining a very good diagnostic value.
Keywords: low-dose protocol, CT, hydrocephalus, children
Background
The incidence of hydrocephalus in children ranges from 1/1000 to 1/500 births. On the basis of ultrasound examination results, hydrocephalus can be diagnosed in approx. 95% of cases. In older children, where the transfontanelle ultrasound is impossible, the examination of choice is CT (computed tomography). Hydrocephalus in children is a result of an increased volume of the cerebrospinal fluid, especially in ventricles (internal hydrocephalus) or in subarachnoid space (external hydrocephalus), due to congenital anomalies of the CNS, posttraumatic or postinflammatory changes, hypoxic-ischemic or postoperative injuries. Hydrocephalus can be accompanied by chromosomal aberrations – in 3% this concerns isolated hydrocephalus, and in 8% hydrocephalus related to other CNS anomalies.
In case of an increased CSF pressure, it is necessary to implant a ventriculo-peritoneal shunt. Misdiagnosed ventriculo-peritoneal shunt failure leads to damage within the cortex and white matter. The final result can be patient’s death. Therefore, a suspicion of an abnormally functioning ventriculo-peritoneal shunt is a very common indication for a head CT, both in emergency and in elective cases before neurosurgical revision. A high number of head CTs in pediatric patients of the Clinic and Department of Pediatric Neurosurgery of the Clinical Hospital in Poznan, an improving access to tomographic examinations, as well as an increasing number of indications for head CTs in children referred by pediatricians and surgeons, induced us to carry out a comparative analysis of head CTs in children with hydrocephalus performed according to a low-dose protocol and a standard protocol.
Aim of the work
The diagnostic value of a low-dose and a standard-dose head CT in children with hydrocephalus was evaluated based on whether it was possible to answer the following questions:
What is the width of the ventricular system and supracerebral fluid spaces?
What is the course of catheters of the ventriculo-peritoneal shunt? Is their continuity preserved?
Are there any symptoms of recent bleeding?
Material and Methods
The authors conducted a retrospective analysis of 256 CTs of the head in children aged from 1 month to 18 years with hydrocephalus or suspected ventriculo-peritoneal shunt failure. Group A included 128 examinations performed according to the low-dose protocol (lower mAs settings) and group B included 128 examinations performed with the use of standard parameters (Table 1). In 9 cases, the CT was conducted according to both the low-dose protocol and the standard method, and in 6 of them the examination was repeated a few times. The analysed examinations were carried out in the years 2009–2011 at Pediatric Radiology Department with the use of a 128-slice CT scanner Somatom Definition AS by Siemens. CT examinations were preceded by a physical examination conducted by the neurosurgeon on call. The choice of examination protocol, i.e. with a lower or with a standard mAs value was made by the radiologist.
Table 1.
Specifications of protocols.
| Children with a body mass of less than 20 kg | |
| Low-dose protocol | Standard protocol |
| CareDose 4D function – on Eff. mAs – 100 KV – 120 |
CareDose 4D function – on Eff. mAs – 190 KV – 120 |
| Children with a body mass of 20 kg and more | |
| Low-dose protocol | Standard protocol |
| CareDose 4D function – off Eff. mAs – 200 KV – 120 |
CareDose 4D function – off Eff. mAs – 350 KV – 120 |
We also compared the values of maximum, mean, and minimum doses in two subgroups of children: with a body mass below 20 kg and above 20 kg. The minimum body mass was 3 kg, while the maximum 100 kg.
Due to patients’ clinical condition and age, 60% of them required a short-term sedation.
Results
All the performed examinations, both in group A (low-dose protocol) and in group B (standard protocol), i.e. 256 examinations in total, were evaluated by radiologists. The analysis showed that the obtained images allowed for answering the questions asked by the neurosurgeon, and thus for classifying the examinations as fully diagnostic.
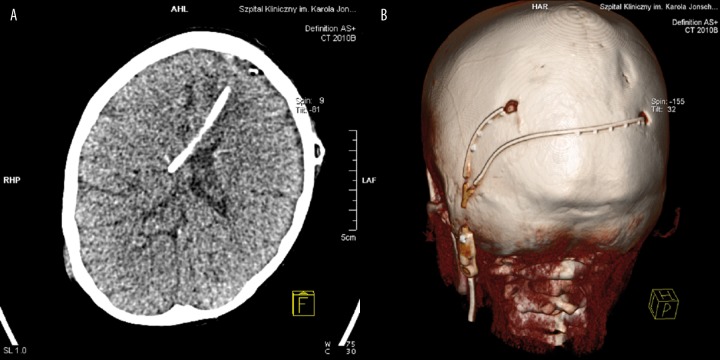
In all patients, the examinations allowed for evaluating the width of the ventricular system, localising the intraventricular tip of the ventriculo-peritoneal shunt catheter, and analysing the course and continuity of the catheter (both in the intracranial and in the examined extracranial section) (Figure 1). No significant differences were found in imaging of supracerebral fluid spaces between both groups. The obtained images allowed also for excluding recent bleeding. However, according to the evaluating radiologists, the fact of blurred cortico-subcortical junction in the examinations with a lower mAs value was important, as it hindered the diagnostics of oedematous lesions in e.g. rapidly progressing hydrocephalus. However, the radiologists and neurosurgeons concluded that despite an increased amount of noise producing film grain, the examinations helped to solve significant clinical problems.
Figure 1.
Nonenhanced computed tomography. (A) axial brain CT, position of the ventriculo – peritoneal shunt catheter, (B) course of the catheters outside the skull in VRT. Both images were obtained in the low-dose protocol.
Minimum, mean, and maximum doses of DLP were also compared, which expressed the total radiation dose (Table 2). According to the conducted analysis, the total radiation dose received by every patient was much lower in the examinations using lower mAs values. Especially the evaluation of doses received by the same patient in repeated examinations, conducted according to the compared protocols, allowed for defining differences between low-dose and a standard examinations (Table 3). The difference in doses was calculated by subtracting the mean dose used in examinations with reduced mAs values from the mean dose of standard CT examinations of the head. A percentage difference was also calculated (Table 4).
Table 2.
Comparison of the total doses of DLP* received by patients in both groups covered by the analysis.
| Total dose of DLP (mGy*cm) | Low-dose protocol | Standard protocol | Difference in mGy*cm |
|---|---|---|---|
| Max. | 1333 | 2087 | 754 (36%) |
| Min. | 156 | 234 | 78 (33%) |
| Mean | 563 | 933 | 370 (40%) |
DLP is a measure of accumulated dose (total energy of radiation) received by the patient. The unit of this index is mGy × cm. It incorporates not only the mean radiation dose in the visualised volume (CTDIvol) but also the length of the scanned area L.
Table 3.
Comparison of total doses of DLP received by patients during head CTs with standard and low-dose protocols.
| Patient | Mean dose mGy*cm | Difference in doses | Number of low-dose examinations | Number of standard examinations | |
|---|---|---|---|---|---|
| Low-dose examination | Standard examination | ||||
| A | 687 | 1193 | 506 | 1 | 2 |
| B | 844 | 1333 | 489 | 6 | 1 |
| C | 601 | 1089 | 488 | 2 | 2 |
| D | 247 | 311 | 64 | 3 | 1 |
| E | 225 | 837 | 612 | 3 | 3 |
| F | 208 | 380 | 172 | 1 | 1 |
| G | 680 | 1284 | 604 | 1 | 1 |
| H | 439 | 593 | 154 | 1 | 1 |
| I | 208 | 397 | 189 | 2 | 1 |
Table 4.
The difference in doses between the low – dose protocol and the standard protocol in the same patient.
| Patient | Mean total dose of DLP (mGy*cm) | Difference in doses (mGy*cm) | % difference in doses | |
|---|---|---|---|---|
| Low-dose examination | Standard examination | |||
| A | 687 | 1193 | 506 | 42% |
| B | 844 | 1333 | 489 | 37% |
| C | 601 | 1089 | 488 | 45% |
| D | 247 | 311 | 64 | 21% |
| E | 225 | 837 | 612 | 73% |
| F | 208 | 380 | 172 | 45% |
| G | 680 | 1284 | 604 | 47% |
| H | 439 | 593 | 154 | 26% |
| I | 208 | 397 | 189 | 48% |
Percentage comparison showed their reduction by 20–70%, with maintained diagnostic value.
Discussion
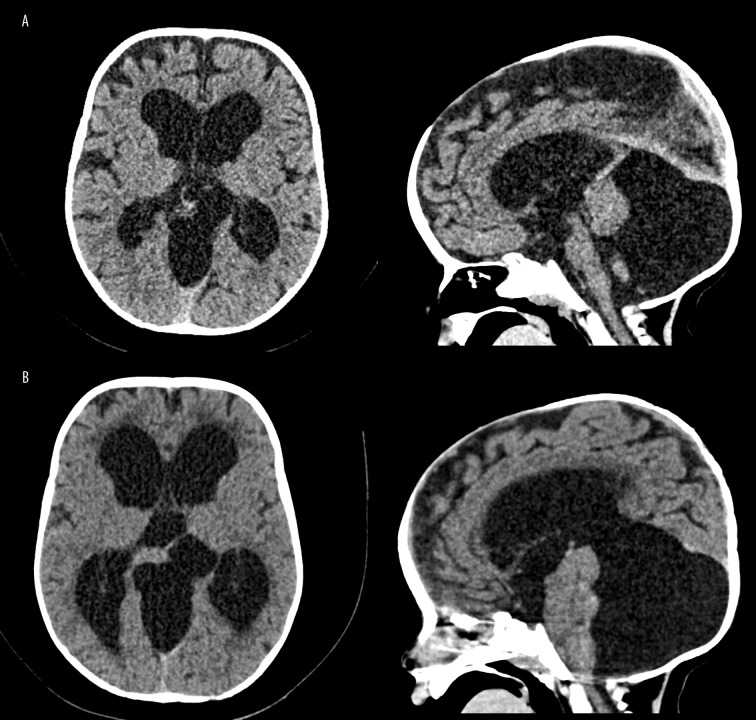
CT examinations according to the low-dose protocol allow for obtaining images of sufficient sensitivity and specificity. It should be pointed out that although the quality of images obtained in examinations with lower mAs values is slightly worse (Figure 2), it is still sufficient for the evaluation of basic brain structures, the degree of widening of the ventricular system, location of the catheter or recent bleeding. Such examinations are in accordance with the ALARA principle which, especially in children, should be taken into account when choosing the diagnostic protocol. Patients with suspected ventriculo-peritoneal shunt failure constitute a group frequently subjected to diagnostic imaging, and after the infancy, CT remains the only ‘method of choice’. According to Goeser et al., the most common causes of such a failure include obstruction of the central end of the catheter, as well as catheter damage in the cervical segment [1]. It is possible to diagnose the above mentioned causes of failure and a less common slit ventricle syndrome, recent bleeding or increased density of the cerebrospinal fluid (which may accompany infection) with the use of examinations with lower mAs values. Images obtained with the low-dose protocol in our work were considered by both radiologists and neurologists as fully diagnostic, as in the studies conducted by other centers, where similar procedures were used [2–4]. Patients with hydrocephalus need to undergo repeated tests at short time intervals. This reduces the risk of dose accumulation. At the same time, as mentioned by other authors, the age of the discussed patients significantly enhances their long-term exposure and their sensitivity to radiation, which is even 10-times higher than in adults [5–7]. Despite the increasing availability of CT, we should not make exceptions to the rule of reasonableness of such examinations. An intentional choice of optimal diagnostic methods, protocols with lower mAs values, adjusted to patient’s body mass (which is very diverse, especially in the youngest age groups) allows for lowering the absorbed dose by up to 70% [3]. Thanks to the modified protocol used in our CT Laboratory, we obtained a dose reduction of approximately 40%, and in one patient, who underwent the examination 6 times, the difference in the absorbed dose between the standard method and the low-dose protocol was 70%. It is difficult to evaluate the radiation risk in children subjected to CT, including head CT. On the basis of the literature review it may be concluded that due to an increasing number of examinations, patients’ irradiation (though not substantial) may be connected with quite a low but statistically significant (for the study population) risk of neoplasm development [7,8]. Due to the above mentioned risks, the role of radiologists consists not only in evaluating the examinations but also in defining the examined area and in choosing correctly the possibly most dose-saving protocol of head CT examination in a child, adjusted to a specific clinical situation [9–14].
Figure 2.
Nonenhanced computed tomography, axial and sagittal brain CT. (A) image in the low-dose protocol, (B) image in the standard protocol.
Conclusions
Computed tomography belongs to the most common imaging methods in case of suspected ventriculo-peritoneal shunt failure in children with hydrocephalus.
The use of the low-dose protocol (with lower mAs values) allows for a significant (by approx. 40%) reduction of the absorbed dose, with the full diagnostic value being maintained.
An increasing number of CTs in pediatric patients enhances the risk of accumulation of the absorbed dose, which requires the radiologists to follow procedures in accordance with the rules of radiological protection and to optimise examination protocols.
References:
- 1.Goeser CD, McLeary MS, Young LW. Diagnostic imaging of ventriculoperitoneal shunt malfunctions and complications. Radiographics. 1998;8(3):635–51. doi: 10.1148/radiographics.18.3.9599388. [DOI] [PubMed] [Google Scholar]
- 2.Udayasankar UK, Braithwaite K, Arvaniti M. Low-Dose Nonenhanced Head CT Protocol for Follow-Up Evaluation of Children with Ventriculoperitoneal Shunt: Reduction of Radiation and Effect on Image Quality. Am J Neuroradiol. 2008;29:802–6. doi: 10.3174/ajnr.A0923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rybka K, Staniszewska MA, Biegański T. Low-dose protocol for head CT in monitoring hydrocephalus in children. Med Sci Monit. 2007;13(Suppl.1):147–51. [PubMed] [Google Scholar]
- 4.Mullins ME, Lev MH, Bove P, et al. Comparison of Image Quality Between Conventional and Low-Dose Nonenhanced Head CT. Am J Neuroradiol. 2004;25:533–38. [PMC free article] [PubMed] [Google Scholar]
- 5.Holmedal LJ, Friber EG, Borretzen I. Radiation doses to children with shunt-treated hydrocephalus. Pediatr Radiol. 2007;37:1209–121. doi: 10.1007/s00247-007-0625-8. [DOI] [PubMed] [Google Scholar]
- 6.Slovis TL. CT and Computed Radiography: The Pictures Are Great, But Is the Radiation Dose Greater Than Required? Am J Roentgenol. 2002;179:39–41. doi: 10.2214/ajr.179.1.1790039. [DOI] [PubMed] [Google Scholar]
- 7.Frush DP, Donnely LF, Rosen NS. Computed Tomography and Radiation Risks: What Pediatric Health Care Providers Should Know. Pediatrics. 2003;112(4):951–57. doi: 10.1542/peds.112.4.951. [DOI] [PubMed] [Google Scholar]
- 8.Brenner DJ, Elliston CD, Hall EJ, Berdon WE. Estimated Risk of Radiation –Induced Fatal Cancer from Pediatric CT. Am J Roentgenol. 2001;176:289–96. doi: 10.2214/ajr.176.2.1760289. [DOI] [PubMed] [Google Scholar]
- 9.Brody AS, Frush DP, Huda W, et al. Radiation Risk to Children From Computed Tomography. Pediatrics. 2007;120(3):677–82. doi: 10.1542/peds.2007-1910. [DOI] [PubMed] [Google Scholar]
- 10.Mayo JR. Radiation Dose Issues in Longitudinal Studies Involving Computed Tomography. Proc Am Thorac Soc. 2008;5(9):934–39. doi: 10.1513/pats.200808-079QC. [DOI] [PubMed] [Google Scholar]
- 11.King MA, Kanal M K, Relyea-Chew A, et al. Radiation exposure from pediatric head CT: a bi-institutional study. Pediatr Radiol. 2009;39:1059–65. doi: 10.1007/s00247-009-1327-1. [DOI] [PubMed] [Google Scholar]
- 12.Bernier MO, Rehel JL, H Brisse J. Radiation exposure from CT in early childhood: a French large – scale multicentre study. Br J Radiol. 2012;85:53–60. doi: 10.1259/bjr/90758403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karabulut N, Ariyurek M. Low dose: practices and strategies of radiologists In university hospitals. Diagn Interv Radiol. 2006;12:3–8. [PubMed] [Google Scholar]
- 14.Watson DJ, Coakley KS. Paediatric CT reference doses based on weight and CT dosimetry phantom size: local experience using a 64-slice CT scanner. Pediatr Radiol. 2010;40:693–70. doi: 10.1007/s00247-009-1469-1. [DOI] [PubMed] [Google Scholar]