Abstract
Background
The present study investigated the prognostic value of medical comorbidities at admission for 30-day in-hospital mortality in patients with acute myocardial infarction (AMI).
Methods
A total of 5161 patients with AMI were admitted in Chinese PLA General Hospital between January 1, 1993 and December 31, 2007. Medical comorbidities including hypertension, diabetes mellitus, previous myocardial infarction, valvular heart disease, chronic obstructive pulmonary disease (COPD), renal insufficiency, previous stroke, atrial fibrillation and anemia, were identified at admission. The patients were divided into 4 groups based on the number of medical comorbidities at admission (0, 1, 2, and ≥ 3). Cox regression analysis was used to calculate relative risk (RR) and 95% confidence intervals (CI), with adjustment for age, sex, heart failure and percutaneous coronary intervention (PCI).
Results
The mean age of the studied population was 63.9 ± 13.6 years, and 80.1% of the patients were male. In 74.6% of the patients at least one comorbidity were identified. Hypertension (50.7%), diabetes mellitus (24.0%) and previous myocardial infarction (12%) were the leading common comorbidities at admission. The 30-day in-hospital mortality in patients with 0, 1, 2, and ≥ 3 comorbidities at admission (7.2%) was 4.9%, 7.2%, 11.1%, and 20.3%, respectively. The presence of 2 or more comorbidities was associated with higher 30-day in-hospital mortality compared with patients without comorbidity (RR: 1.41, 95% CI: 1.13-1.77, P = 0.003, and RR: 1.95, 95% CI: 1.59-2.39, P = 0.000, respectively).
Conclusions
Medical comorbidities were frequently found in patients with AMI. AMI patients with more comorbidities had a higher 30-day in-hospital mortality might be predictive of early poor outcome in patients with AMI.
Keywords: acute myocardial infarction, comorbidity, mortality
1. Introduction
In the past five decades, we have witnessed major breakthroughs in the management of acute myocardial infarction (AMI).[1] However, AMI remains a leading cause of death worldwide, and the mortality rate from AMI is still unacceptably high.[2],[3] Many challenges remain in the risk stratification and management of patients with AMI, such as optimal risk stratification of patients, with comorbidities. Comorbidities may affect multiple clinical outcomes, including mortality, quality of life, and cost.[4] Comorbidities in patients with AMI, such as renal insufficiency, diabetes mellitus and stroke, may reduce the patient's physiologic reserve and thereby increase the risk of adverse outcome. Therefore the assessment of comorbidity is important for risk stratification of AMI. To date, little information is available on the effects of patients' comorbidity on the outcome of patients with AMI. In the present study, we investigated whether medical comorbidities at admission might be predictive for the 30-day in-hospital mortality of patients with AMI hospitalized in a single medical center.
2. Methods
2.1. Data sources
Since 1992 a computerized medical record database has been established in the Chinese PLA General Hospital, with the diagnostic codes based on the ninth revision of the International Classification of Diseases developed by the World Health Organization, commonly referred to as ICD9. The medical records of the patients with a primary diagnosis of AMI who were admitted between January 1, 1993 and December 31, 2007 were identified through discharge diagnosis of ICD9 code 410. A total of 5161 patients were identified, and the medical records of these patients were then reviewed, with emphasis on age, gender, medical comorbidities at admission, clinical, electrocardiographic, and laboratory evidence of AMI, heart failure, percutaneous coronary intervention (PCI), and death in 30 d after admission. All these patients met at least two of the criteria: (1) clinical symptoms consistent with AMI (chest pain, arm or shoulder pain, dyspnea, diaphoresis, nausea or vomiting); (2) dynamic electrocardiographic changes consistent with AMI; and (3) elevation of cardiac biomarkers, such as cardiac troponine, creatinine kinase and its isoenzyme muscle-brain subfractions. Patients were categorized into 4 groups based on the number of medical comorbidities (0, 1, 2, ≥ 3). Patients without medical comorbidity were defined as the reference group. The 30-day in-hospital mortality was calculated for each group.
2.2. Comorbidity
Medical comorbidities at admission included hypertension, diabetes mellitus, previous myocardial infarction, valvular heart disease, chronic obstructive pulmonary disease (COPD), renal insufficiency, previous stroke, atrial fibrillation and anemia. These coexisting medical conditions at admission were identified, and the number of medical comorbidities was calculated for each patient.
2.3. Statistical analysis
The gender and mortality rate were treated as categorical variables. Cox regression analysis was used to examine the relationship between the number of medical comorbidities at admission and 30-day in-hospital mortality. Relative risks (RRs) and 95% confidence intervals (CIs) were calculated with adjustment for age, gender, heart failure and PCI using SPSS 16.0 software (SPSS, Chicago, IL, USA). A P value of < 0.05 was considered statistically significant.
3. Results
3.1. Characteristics of patients
The 5161 AMI patients aged from 18-103 years, with a mean age of 63.9 ± 13.6 years. Of the 5161 AMI patients, 4133 patients were male, and 1028 patients were female; 74.6% of the patients had at least one medical comorbidity; 2 615 (50.7%) patients had hypertension, 1 237 (24.0%) had diabetes mellitus, 619 (12%) had old myocardial infarction, 366 (7.1%) had atrial fibrillation, 223 (4.4%) had renal insufficiency, 218 (4.2%) had valvular heart disease, 172 (3.3%) had old cerebral infarction, 60 (1.2%) had anemia, and 52 (1%) had pulmonary heart disease.
3.2. 30-day in-hospital mortality
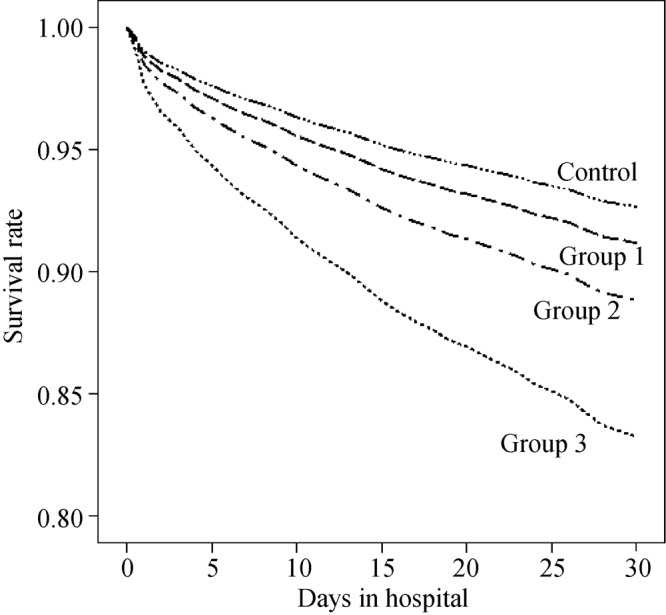
The 30-day in-hospital mortality of all 5161 AMI patents was 9.3%. The 30 d in-hospital mortality in patients with only one comorbidity at admission was 7.2%, which was higher compared with that in patients without comorbidity (4.9%), but the difference was not statistically significant (RR: 1.21, 95% CI: 0.90–1.64, P = 0.209). The 30-day in-hospital mortality in AMI patients with 2 comorbidities was 11.1%, which was significantly higher than that in patients without comorbidity (RR: 1.41, 95% CI: 1.13–1.77, P = 0.003). The 30-day in-hospital mortality in AMI patients with ≥ 3 comorbidities was 20.3%, which was even higher than that in patients without comorbidity (RR: 1.95, 95% CI: 1.59–2.39, P = 0.000) (Table 1, Figure 1).
Table 1. The 30-day in-hospital mortality in AMI patients with or without comorbidities.
| Group | Number of medical comorbidities | Number of patients (n) |
Number of 30-day in-hospital death (n) |
30-day in-hospital mortality (%) |
||||||
| Total | Male | Female | Total | Male | Female | Total | Male | Female | ||
| Control | 0 | 1 312 | 1 125 | 187 | 62 | 40 | 22 | 4.7 | 3.6 | 11.8 |
| Group 1 | 1 | 1 914 | 1 583 | 331 | 137 | 107 | 30 | 7.2 | 6.8 | 9.1 |
| Group 2 | 2 | 1 225 | 923 | 302 | 136 | 103 | 33 | 11.1 | 11.2 | 10.9 |
| Group 3 | ≥3 | 710 | 502 | 208 | 144 | 101 | 43 | 20.3 | 20.1 | 20.7 |
AMI: acute myocardial infarction.
Figure 1. Survival rates of AMI patients with or without comorbidities.
4. Discussion
AMI is a common health problem worldwide and the incidence of AMI increased with age.[5] Patients hospitalized with AMI, especially the elderly patients, tend to have multiple chronic cardiac or noncardiac medical conditions, such as hypertension, diabetes mellitus, renal insufficiency or chronic COPD. Untill now, how these comorbid diseases affect the early outcome of patients with AMI has not been fully investigated. As previously reported, renal insufficiency[6],[7] and anemia[8] were considered as an independent predictors for poor prognosis of AMI. However, the previous studies had focused on the effect of one single comorbidity on the outcome of patients with AMI, which was not consistent with the fact that patients with AMI often had more than one comorbidity. In the present study, we sought to better understand the scope of this problem in the real-world setting.
The present study showed that 74.6% of the AMI patients had at least one comorbidity, with hypertension, diabetes mellitus and old myocardial infarction as the most common comorbidities at admisssion. The number of comorbidities increased with increasing age. It was reported that age,[9],[10] gender,[10]–[14] percutaneous coronary intervention[15] and heart failure[16] might be the prognostic factors for the early outcome of patients with AMI. Therefore, in the present study, these four factors were adjusted in Cox regression analysis. Our study showed that the 30-day in-hospital mortality in AMI patients with only one comorbidity at admission (7.2%) were higher compared with that in patients without comorbidity (4.9%), but the difference was not statistically significant (RR: 1.21, 95% CI: 0.90–1.64, P = 0.209). Compared with patients without comorbidity, the 30-day in-hospital mortality with 2 comorbidities (11.1%) were significantly higher (RR: 1.41, 95% CI: 1.13–1.77, P = 0.003); the 30-day in-hospital mortality in AMI patients with 3 or more comorbidities (20.3%) was even higher (RR: 1.95, 95% CI: 1.59–2.39, P = 0.000). These results suggested that AMI patients with more comorbidities were more likely to have higher 30-day in-hospital mortality, and the number of medical comorbidities might be predictive for the early mortality rate of patients.
The number of medical comorbidities at admission might be a simple and easy way for heath care professionals to predict the early mortality rate for patients admitted with AMI. How many problems are on the problem list? How many prescription medications does the patient take? After detailed history taking and physical examination, the clinicians might obtain the information on the medical comorbidities without much difficulty. Based on the number of medical comorbidities at admission, the clinicians might preliminarily assess the risk of 30-day in-hospital mortality. Special attention should be paid to those patients with 3 or more comorbidities, whose 30-day in-hospital mortality rate might be high, and medical therapy and nursing care should be intensified and their medical condition should be carefully observed. The health care professionals should also bear in mind that chronic medical comorbidities might have an impact on physicians' decision making regarding standard therapeutic options for AMI. Complete adherence to therapeutic guidelines for AMI is suboptimal in patients with comorbidities. As a result, patients with more severe comorbidities were less likely to receive evidence-based medications or percutaneous coronary intervention recommended by AMI treatment guideline.[17]–[19] For example, β blockers might be underused in AMI patients complicated with chronic obstructive pulmonary disease. Therefore, the physicians should evaluate multiple organ functions to ascertain whether there were any contraindications for standard therapy recommended by AMI treatment guideline. On the other hand, less medical and nursing services might be considered for AMI patients without comorbidity or with a single comorbidity, so as to reduce the medical burden of the patients.
4.1. Study limitations
In the present study, the effect of comorbid conditions on short-term outcome of patients with AMI were gauged by counting the number of comorbidities. However, a simple count of medical comorbidities implicitly assumed that the 30-day mortality of AMI patients was equally affected by hypertension as by valvular heart disease, which seemed implausible. A better method would be to construct an index that weighed medical comorbidities according to their impact on 30-day in-hospital mortality so that hypertension counted more heavily than valvular heart disease. Therefore, a properly weighted index would be built to precisely measure the effects of medical comorbidities on 30-day in-hospital mortality, which might help in clinical practice.
In conclusion, this retrospectively study provided evidence that AMI patients with more comorbidities were more likely to have 30-day in-hospital mortality. However, further studies are needed to construct a properly weighted index to precisely measure the association between medical comorbidities at admission and 30-day in-hospital mortality in patients with AMI.
References
- 1.Kumar A, Cannon CP. Acute coronary syndromes: diagnosis and management, Part I. Mayo Clin Proc. 2009;84(10):917–938. doi: 10.4065/84.10.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuch B, Bolte HD, Hoermann A, et al. What is the real hospital mortality from acute myocardial infarction? Epidemiological vs clinical view. Eur Heart J. 2002;23:714–720. doi: 10.1053/euhj.2001.2947. [DOI] [PubMed] [Google Scholar]
- 3.Krumholz HM, Wang Y, Chen J, et al. Reduction in acute myocardial infarction mortality in the United States: risk-standardized mortality rates from 1995–2006. JAMA. 2009;302(7):767–773. doi: 10.1001/jama.2009.1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hlatky MA. Comorbidity and outcome in patients with coronary artery disease. J Am Coll Cardiol. 2004;43:583–584. doi: 10.1016/j.jacc.2003.11.021. [DOI] [PubMed] [Google Scholar]
- 5.Fang J, Alderman MH, Keenan NL, et al. Acute myocardial infarction hospitalization in the United States, 1979 to 2005. Am J Med. 2010;123(3):259–266. doi: 10.1016/j.amjmed.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 6.Lekston A, Kurek A, Tynior B. Impaired renal function in acute myocardial infarction. Cardiol J. 2009;16(5):400–406. [PubMed] [Google Scholar]
- 7.Lazzeri C, Valente S, Chiostri M, et al. Evaluation of acid-base balance in ST-elevation myocardial infarction in the early phase: a prognostic tool? Coron Artery Dis. 2010;21(5):266–272. doi: 10.1097/mca.0b013e32833b20c6. [DOI] [PubMed] [Google Scholar]
- 8.Anker SD, Voors A, Okonko D, et al. Prevalence, incidence, and prognostic value of anaemia in patients after an acute myocardial infarction: data from the OPTIMAAL trial. Eur Heart J. 2009;30(11):1331–1339. doi: 10.1093/eurheartj/ehp116. [DOI] [PubMed] [Google Scholar]
- 9.Shao YH, Croitor SK, Moreyra AE, et al. Comparison of hospital versus out of hospital coronary death rates in women and men. Am J Cardiol. 2010;106(1):26–30. doi: 10.1016/j.amjcard.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 10.Vaccarino V, Parsons L, Peterson ED, et al. Sex differences in mortality after acute myocardial infarction: changes from 1994 to 2006. Arch Intern Med. 2009;169:1767–1774. doi: 10.1001/archinternmed.2009.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Venskutonyte L, Malmberg K, Norhammar A, et al. Effect of gender on prognosis in patients with myocardial infarction and type 2 diabetes. J Intern Med. 2010;268:75–82. doi: 10.1111/j.1365-2796.2010.02215.x. [DOI] [PubMed] [Google Scholar]
- 12.de Boer MJ, Ottervanger JP, Suryapranata H, et al. Old age and outcome after primary angioplasty for acute myocardial infarction. J Am Geriatr Soc. 2010;58(5):867–872. doi: 10.1111/j.1532-5415.2010.02821.x. [DOI] [PubMed] [Google Scholar]
- 13.Roncalli J, Elbaz M, Dumonteil N, et al. Gender disparity in 48-hour mortality is limited to emergency percutaneous coronary intervention for ST-elevation myocardial infarction. Arch Cardiovasc Dis. 2010;103:293–301. doi: 10.1016/j.acvd.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 14.Park JS, Kim YJ, Shin DG, et al. Gender differences in clinical features and in-hospital outcomes in ST-segment elevation acute myocardial infarction: From the Korean Acute Myocardial Infarction Registry (KAMIR) Study. Clin Cardiol. 2010;33(8):E1–6. doi: 10.1002/clc.20557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mahon NG, O'rorke C, Codd MB, et al. Hospital mortality of acute myocardial infarction in the thrombolytic era. Heart. 1999;81:478–482. doi: 10.1136/hrt.81.5.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Francisco AR, Sousa M, Amador P, et al. Chronic medical comorbidities in patients with acute coronary syndrome. Rev Port Cardiol. 2010;29:7–21. [PubMed] [Google Scholar]
- 17.McLaughlin TJ, Soumerai SB, Willison DJ, et al. The effect of comorbidity on use of thrombolysis or aspirin in patients with acute myocardial infarction eligible for treatment. J Gen Intern Med. 1997;12:1–6. doi: 10.1046/j.1525-1497.1997.12105.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Passman R, Kimmel S. Do comorbidities influence the treatment of myocardial infarction? J Gen Intern Med. 1997;12:73–74. doi: 10.1046/j.1525-1497.1997.1217101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee JH, Yang DH, Park HS, et al. Suboptimal use of evidence-based medical therapy in patients with acute myocardial infarction from the Korea Acute Myocardial Infarction Registry: prescription rate, predictors, and prognostic value. Am Heart J. 2010;159:1012–1019. doi: 10.1016/j.ahj.2010.03.009. [DOI] [PubMed] [Google Scholar]


