1. Why is the demograpy important?
In the half century 2000-2050, there will be a virtual tsunami of aging in the United States. The anticipated increase in the population older than age 65 is 140%, and for the population older than age 85, 389%. More than half of the current U.S. population can anticipate living to age 80, with a contemporary life expectancy at age 75 of 11 years, and at age 85 of 6 years.[1]
The classification of aging is variable. Often, age 65 years is used as a cutpoint, as that is the beginning age for Medicare health insurance coverage in the U.S. Others often use age 75 as the beginning of old age, and 85 years as characteristic of very old age. Perhaps a reasonable approach to old age is the comment by Pascal that “old age is just a time that is farther from the beginning and nearer to the end.”
Nonetheless, contemporary aging is a social phenomenon without historical precedent. Physicians and scientists have an inadequate information base to guide the care of the oldest old. Government and social institutions lack the knowledge as to how to respond to the burgeoning health needs of the oldest old; and information is lacking about the health care values of our oldest old citizens to guide their cardiovascular care.
The contemporary U.S. population older than age 65 accounts for more than 85% of all cardiovascular disease deaths, 65% of cardiovascular disease hospitalizations, 62% of myocardial infarction hospitalizations, and 77% of heart failure hospitalizations.[2],[3]
A survey of cardiovascular procedures performed in the U.S., based on the data report from 2005,[2] documents that the Medicare population, i.e., those older than 65 years of age, accounted for 49.9% of diagnostic cardiac catheterizations, 50.4% of percutaneous coronary interventions, 56.7% of coronary artery bypass graft surgery procedures, 86.1% of permanent pacemaker implantations, 54.6% of implantable defibrillator procedures, and 79.6% of carotid endarterectomy surgery procedures.
2. Aging physiology and geriatric cardiovascular disease
The physiologic changes of aging underlie a number of prominent geriatric cardiovascular syndromes. Isolated systolic hypertension reflects the increase in central arterial stiffness; heart failure with normal systolic function is attributable to the combination of delayed early left ventricular filling, the increase in central arterial stiffness, and the increased neurohormonal regulation; whereas orthostatic hypotension is due to the decrease in baroreflex sensitivity. The excess of atrial fibrillation reflects left ventricular stiffness, engendering an increase in left ventricular pressure and consequent increase in left atrial pressure and size, in combination with increased central arterial stiffness. Coronary artery disease has as its substrate not only the increase in central arterial stiffness, but the prominent endothelial dysfunction.
3. The benefit vs. risk conundrum
The challenge to the clinician is that the attributable risk for cardiovascular disease is highest among seniors, giving any advantageous intervention the greatest potential to favorably improve morbidity and mortality. Recently, among the newer technologic advances, transcutaneous aortic valve implantation (TAVI), affords the ability to substantially improve the symptoms and quality of life for patients with inoperable severe aortic stenosis, with decreased mortality and hospitalizations but a higher incidence of major strokes and vascular events.[4]
But there are complex management challenges within this spectrum[5]–[7]. Characteristically, aged patients have multiple simultaneous cardiovascular problems, as the patient with an acute coronary syndrome who concomitantly presents with heart failure and atrial fibrillation. Additionally, there is frequent concomitant multisystem disease: anemia, renal insufficiency, chronic obstructive pulmonary disease and diabetes, to name a few. Management is complicated by drug-drug interactions and drug-disease interactions. Hospitalization per se presents hazards, and there are the confounding problems of frailty and cognitive decline.
Testing following myocardial infarction, save for echocardiography, declines sharply by age category, as do myocardial revascularization procedures (Figure 1). Is the decreased revascularization appropriate or inappropriate given the increase in adverse outcomes of percutaneous interventions (Figure 2) and coronary artery bypass graft surgery (Figure 3) at very advanced age? Or are the latter attributable to delayed testing and/or delayed and consequent urgent or emergency procedures that entail suboptimal outcomes?
Figure 1. Post-myocardial infarction (MI) testing by age category. Use of cardiac catheterization, stress testing, revascularization, and echocardiography within 60 days of MI. (Source: Alexander, et al[13]).
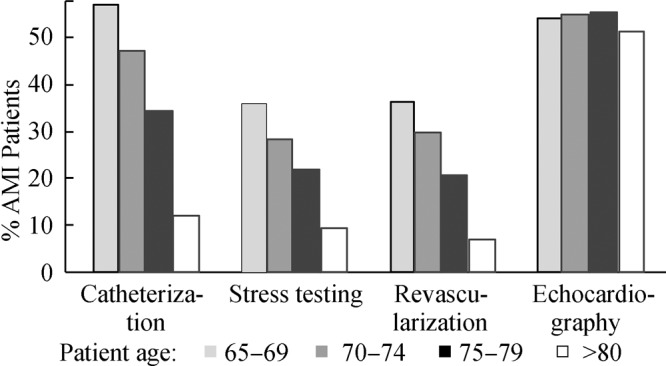
Figure 2. Observed rates of death/MI/CVA (dashed line) and mortality (solid line) according to age. MI: Myocardial infarction; CVA: Cerebrovascular accident. (Source: Batchelor, et al[14]).
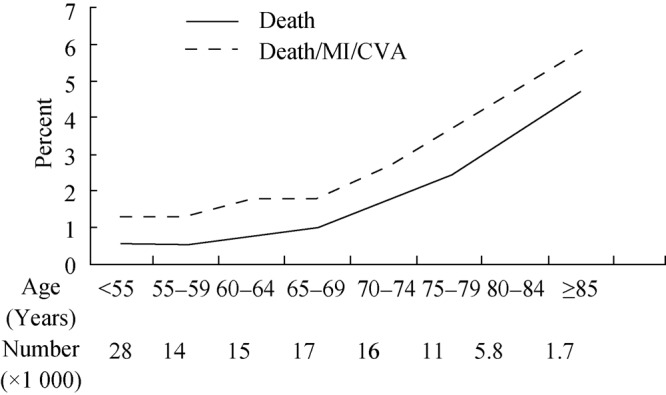
Figure 3. In-hospital mortality, postoperative neurologic complications and postoperative renal failure after coronary artery bypass graft surgery (CABG) by age. Diamond = mortality; Square = renal failure; Triangle = Neurologic events. (Source: Alexander, et al[15]).

The AHA/ACC Unstable Angina/NSTEMI Guidelines offer examples, even considering solely the Class I recommendations for older adults.[8] We are charged to evaluate for acute and long-term therapeutic interventions similarly to our approach to younger patients, with a level of evidence A; and to make decisions not solely on chronologic age, but to consider general health, functional and cognitive status, comorbidities, life expectancy, patient preferences and goals, with a level of evidence B. Unfortunately, many of these variables are unknown in an acute care setting. We are cautioned to pay attention to appropriate dosage of pharmacologic agents, considering creatinine clearance, altered pharmacokinetics, and pharmacodynamics (level of evidence B) – but the latter may not be readily evident. Invasive strategies are recommended despite their early procedural risks, because of the overall equal or greater benefit than encountered among younger patients, with a level of evidence B. Consideration is advocated of patient and family preferences, quality of life issues, end-of-life preferences, and sociocultural differences, to name a few, with the level of evidence C. In optimal clinical practice, these latter issues will have been addressed during the stable phase of the illness, so that such vital aspects are not first introduced to the patient and family at a time of crisis. But even for such Class I recommendations, as one of the authors of the Guidelines, I am aware of the challenges presented.
Contributors to adverse outcomes of acute coronary syndromes relate substantially to the cardiovascular changes of aging on which the acute coronary syndrome is superimposed.[9],[10] These include the increase in central arterial stiffness previously discussed with resultant increase in afterload; the decrease in endothelial function lessening the ability to achieve vasodilation; a decreased and delayed early ventricular diastolic filling leading to increased dependence on the atrial contribution to ventricular filling to maintain cardiac output; and the decrease in sinoatrial node pacemaker cells causing susceptibility to the sick sinus syndrome. The lessened aerobic capacity with aging is manifest by the decrease in VO2 max. Added deleterious features include the decrease in beta adrenergic responsiveness, less benefit of preconditioning [11] and decreased angiogenesis.[12]
4. What have we learned from randomized clinical trials of cardiovascular therapies?
Data at age 80 and older are sparse or absent from most cardiovascular clinical trials, disadvantaging the management of very elderly patients. Many of these trials systematically excluded older patients, and in particular older patients with complexities, but it is the complex elderly patients who constitute a demographic imperative for future randomized clinical trials, as they exemplify the population currently under treatment. For example, if we compare the randomized clinical trial aged population to community older adults, the population in the randomized trials is homogeneous, and that of community older adults is heterogeneous. Patients in the randomized clinical trials had few comorbidities while community older adults have many. Renal function is typically normal among older adults in clinical trials, but compromised among community older adults. Polypharmacy is rare in elderly patients in clinical trials, and common in community older adults. Finally, the characteristic outcomes measured in the randomized clinical trials include death, myocardial infarction, and revascularization; whereas for older adults in the community, important outcomes more likely are independence, morbidities, and functional status. Stated otherwise, mortality endpoints are typically less relevant to seniors than are functional, symptomatic, and quality of life issues.
What we then must require from future randomized clinical trials of cardiovascular therapies in older adults is ascertainment of whether preventive, diagnostic, and therapeutic measures can decrease recurrent costly hospitalizations; improve personal independence; lessen disability and dependency; relieve symptoms; improve functional capacity; decrease medication costs and other financial constraints; and improve the manner and the quality of death.
Patterns of postmyocardial infarction revascularization by age in the U.S. Medicare population are shown in Figure 1.[13] Revascularization procedures, obviously, decline markedly with aging within the Medicare population, but is this disparity appropriate or inappropriate? Figures 2 and Figure 3[14],[15] show the rapidly escalating mortality from revascularization procedures with increasing age, more prominent for coronary artery bypass graft surgery than for percutaneous interventions, but nevertheless prominent for both. The challenge is whether the increased mortality at very elderly age is immutable, or whether it reflects that interventions were not undertaken more electively at younger elderly age, potentially averting delayed emergency-driven procedures.
5. Management challenges: signposts on the road to improved geriatric cardiovascular care
Requisite to optimal management of the geriatric patient with cardiovascular disease is improved communication, with individualization of care and recommendations given to both patient and family. It is vital that healthcare providers coordinate information and planning.
Critical is improvement in the transitions of care,[16]–[19] hospital to rehabilitation unit, rehabilitation unit to home or hospital to home, home to office visits, ensuring that there is timely follow-up, medication consistency, patient education including detailed lifestyle counseling and cardiac rehabilitation when appropriate. End-of-life planning, particularly advance directives, as previously noted, should be addressed during the stable phase of illness in the course of office visits and documented in the medical encounter. This may limit the disproportionate cardiovascular care expenses and personal unfavorable quality of life alterations in the last weeks of life.
Thus, the signposts involve patient-centered care that addresses individual cardiac and noncardiac comorbidities and includes patient goals and preferences, with specific attention to end-of-life preferences. Geriatric syndromes, particularly frailty, disability, and impaired cognitive function, require detailed attention. The pharmacologic regimen must be tailored regarding both ease of dosing and affordability, in addition to standard monitoring of adverse effects. As previously stated, there should be focus on the transitions of care, with emphasis on repeated patient and family education and counseling and the use of rehabilitation services when appropriate.
6. What we must learn about geriatric cardiovascular disease?
Exploration is warranted of the cardiovascular syndromes that predominate at elderly age, in specific isolated systolic hypertension, heart failure with a preserved left ventricular ejection fraction, and calcific degenerative aortic stenosis. For heart failure, needed are better long-term preventive therapies, most prominent among which is blood pressure control; but also better and more precise diagnoses separating systolic from diastolic ventricular dysfunction. Research is needed to inform clinical decision-making on the efficacy of diagnostic tests and of risk stratification at elderly age. Specifically, what level of procedural risk or comorbid illness or cognitive impairment, to name a few, renders an intervention inappropriate? To be examined are the impacts of treatments not solely on mortality but on health status and quality of life, requiring that functional and health status indices be incorporated in both registries and randomized clinical trials. A new generation of clinical trials and registries that address the above issues will enable incorporation of age-related complexities into clinical decision-making and enhance the application of proved beneficial interventions.
7. Research questions: unmet needs
Let me pose six contemporary challenges to the delivery of optimal cardiovascular care at elderly age.[20]–[22] First, are the cardiovascular changes of aging modifiable by exercise, lifestyle, or other interventions undertaken in young and middle age? What are the most effective preventive interventions, given their substantial benefit owing to the increase in attributable risk of any risk factor at elderly age? There is decreased diagnostic testing at elderly age; is this an appropriate clinical practice, or would earlier and improved testing improve outcomes? Contemporary therapy is predominately symptom-driven. Would testing to identify high-risk asymptomatic elderly individuals improve outcomes? And what is the optimal approach to such risk stratification?
What is the optimal drug choice or drug regimen for cardiovascular problems that increase morbidity and are highly prevalent in elderly populations, or where pathophysiologic variables either predominate or are unique to the elderly? As previously cited, these include isolated systolic hypertension, heart failure with preserved left ventricular systolic function, to name a few. Finally, what interventional procedures offer differential benefit or risk at advanced age, and are these benefits those valued by the aged patient?
Contemporary cardiovascular clinical care involves to a major extent the care of aged patients.[23] There is much to be learned to enable optimal levels of care to be delivered to the seniors in our society.
References
- 1.U.S. Census Bureau http://www.census.gov/population/www/projections/popproj.html (accessed on May 1. 2011)
- 2.American Heart Assoociation Heart disease and stroke statistics, 2008 Update. http://www.amhrt.org/statistics/index/html (accessed on May 1. 2011)
- 3.Hall MJ, DeFrances CJ, Williams SN, et al. National hospital discharge survey: 2007 Summary, national center for health statistics reports, Number 29, October 26, 2010. [PubMed]
- 4.Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363:1597–1607. doi: 10.1056/NEJMoa1008232. [DOI] [PubMed] [Google Scholar]
- 5.Alter DA, Manuel DG, Gunraj N, et al. Age, risk-benefit trade-offs, and the projected effects of evidence-based therapies. Am J Med. 2004;116:540–545. doi: 10.1016/j.amjmed.2003.10.039. [DOI] [PubMed] [Google Scholar]
- 6.Avorn J. Medication use in older patients: better policy could encourage better practice. JAMA. 2010;304:1606–1607. doi: 10.1001/jama.2010.1495. [DOI] [PubMed] [Google Scholar]
- 7.Cleveland JC., Jr Frailty, aging, and cardiac surgery outcomes: The stopwatch tells the story. J Am Coll Cardiol. 2010;56:1677–1678. doi: 10.1016/j.jacc.2010.07.021. [DOI] [PubMed] [Google Scholar]
- 8.Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: A Report of the American College of Cardiology/American Heart Association task force on practice guidelines (writing committee to revise the 2002 guidelines for the management of patients with unstable angina/non-ST-Elevation Myocardial Infarction) J Am Coll Cardiol. 2007;50:e1–e157. doi: 10.1016/j.jacc.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 9.James TN. Normal and abnormal consequences of apopotosis in the human heart. Annu Rev Physiol. 1998;60:309–325. doi: 10.1146/annurev.physiol.60.1.309. [DOI] [PubMed] [Google Scholar]
- 10.Fleg JL, Bos AG, Brant LH, et al. Longitudinal decline of aerobic capacity accelerates with age. Circulation. 2000;102(Suppl II):602. doi: 10.1161/CIRCULATIONAHA.105.545459. [DOI] [PubMed] [Google Scholar]
- 11.Abete P, Ferrare N, Cacciatore F, et al. Angina-induced protection against myocardial infarction in adult and elderly patients: A loss of preconditioning mechanism in the aging heart? J Am Coll Cardiol. 1997;30:947–954. doi: 10.1016/s0735-1097(97)00256-8. [DOI] [PubMed] [Google Scholar]
- 12.Rivard A, Febre J-E, Silver M, et al. Age-dependent impairment of angiogenesis. Circulation. 1999;99:111–120. doi: 10.1161/01.cir.99.1.111. [DOI] [PubMed] [Google Scholar]
- 13.Alexander KP, Galanos AN, Jollis JG, et al. Post-myocardial infarction risk stratification in elderly patients. Am Heart J. 2001;142:37–42. doi: 10.1067/mhj.2001.115589. [DOI] [PubMed] [Google Scholar]
- 14.Batchelor WB, Anstrom KJ, Muhlbaier JH, et al. Contemporary outcome trends in the elderly undergoing percutaneous coronary interventions: results in 7472 octogenarians. National Cardiovascular Network Collaboration. J Am Coll Cardiol. 2000;36:723–730. doi: 10.1016/s0735-1097(00)00777-4. [DOI] [PubMed] [Google Scholar]
- 15.Alexander KP, Anstrom KJ, Muhlbaier LH, et al. Outcomes of Cardiac Surgery in Patients Age ≥ 80 Years: Results from the National Cardiovascular Network. J Am Coll Cardiol. 2000;35:731–738. doi: 10.1016/s0735-1097(99)00606-3. [DOI] [PubMed] [Google Scholar]
- 16.Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: Implications for Patient Safety and Continuity of Care. JAMA. 2007;297:831–841. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- 17.Coleman EA, Berenson RA. Lost in transition: Challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;140:533–536. doi: 10.7326/0003-4819-141-7-200410050-00009. [DOI] [PubMed] [Google Scholar]
- 18.Suaya JA, Stason WB, Ades PA, et al. Cardiac rehabilitation and survival in older coronary patients. J Am Coll Cardiol. 2009;54:25–33. doi: 10.1016/j.jacc.2009.01.078. [DOI] [PubMed] [Google Scholar]
- 19.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patients mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300:1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wenger NK, editor. Marion Merrell Dow; Kansas City, USA: 1993. Inclusion of elderly individuals in clinical trials: Cardiovascular disease and cardiovascular therapy as a model. [Google Scholar]
- 21.Avezum A, Makdisse M, Spencer F, et al. Impact of age on management and outcome of acute coronary syndrome: observations from the Global Registry of Acute Coronary Events (GRACE) Am Heart J. 2005;149:67–73. doi: 10.1016/j.ahj.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 22.Alexander KP, Roe MT, Chen AY, et al. Evolution in cardiovascular care for elderly patients with non-ST-segment elevation acute coronary syndromes: results from the CRUSADE National Quality Improvement Initiative. J Am Coll Cardiol. 2005;46:1479–1487. doi: 10.1016/j.jacc.2005.05.084. [DOI] [PubMed] [Google Scholar]
- 23.Forman DE, Rich MW, Alexander KP, et al. Cardiac care of older adults: Time for a new paradigm. J Am Coll Cardiol. 2011;57(18):1801–1810. doi: 10.1016/j.jacc.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]


