Abstract
Coronary heart disease (CHD) is the leading cause of death worldwide and becomes increasingly prevalent among patients aged 65 years and older. Elderly patients are at a higher risk for complications and accelerated physical deconditioning after a cardiovascular event, especially compared to their younger counterparts. The last few decades were privy to multiple studies that demonstrated the beneficial effects of cardiac rehabilitation (CR) and exercise therapy on mortality, exercise capacity, psychological risk factors, inflammation, and obesity among patients with CHD. Unfortunately, a significant portion of the available data in this field pertains to younger patients. A viable explanation is that older patients are grossly underrepresented in these programs for multiple reasons starting with the patient and extending to the physician. In this article, we will review the benefits of CR programs among the elderly, as well as some of the barriers that hinder their participation.
Keywords: Cardiac rehabilitation, Exercise therapy, Elderly patients, Exercise capacity
1. Introduction
Coronary heart disease (CHD) is the leading cause of death worldwide. In the United States alone, 26.0% of all deaths in 2006[1] and 33.6% of all deaths in 2007 were attributed to heart disease.[2] Furthermore, 86.0% of CHD related deaths were among individuals aged 65 and older.[3]
When compared to their younger counterparts, elderly patients are typically at a higher risk of complications from myocardial infarction (MI) and myocardial revascularization procedures, leading to prolonged hospital stays and subsequent deconditioning.[4] Additionally, elderly patients are usually less fit than younger patients before the initial cardiovascular (CV) event, with accelerated deconditioning once CHD is established. Therefore, the elderly population likely represents a perfect population to especially benefit from formal cardiac rehabilitation and exercise training (CRET) programs. Over the past few decades, there has been a keen interest in the role of CRET among CHD patients. As a result, many studies have examined and, subsequently demonstrated, the beneficial role of CR, regular ET, physical activity, and maintenance of cardio- respiratory fitness (CRF) in both the primary and secondary prevention of CHD among the general population,[5] as well as elderly patients with CHD. Consequently, the use and safety of CRET among older patients has gradually gained acceptance over the last decade.[6]
Despite the evidence in favor of CRET in the elderly, this form of treatment and prevention is grossly underutilized for multiple reasons in this age group, including age, bias and poor referral.[7]
Over the years, many studies have demonstrated the benefits of CRET on a number of important clinical factors including exercise capacity, inflammation, diabetic glucose control, autonomic function, behavioral characteristics, quality of life, future hospitalization costs, and major CHD morbidity and mortality after a major CV event.[8]–[11] The goal of this article is to provide a detailed review of the available material involving CRET, especially pertaining to the elderly, by performing a comprehensive literature search on this topic. The information was obtained by reviewing randomized clinical trials, many large observational studies, as well as appropriate review articles and editorials. Finally, we will discuss some of the current barriers that deter CRET referrals, and participation by the elderly.
2. Benefits of CRET in the elderly
“If I knew I was going to live this long, I would have taken better care of myself ” – Eubie Blake.
2.1. Impact on mortality
CRET is an effective intervention in reducing mortality among patients with CHD. Due to this, formal CRET programs are widely recognized as an invaluable resource. Over the last few years there have been meta-analyses, as well as retrospective evaluations, of large cohorts that have consistently demonstrated this point.
O'Connor et al.[12] published a meta-analyses of 22 randomized trials that included 4554 post-MI patients followed for approximately three years. This study demonstrated the odds ratio (OR) was significantly lower among participants in CRET compared to the control group during the tracking period. This included total mortality (OR = 0.80, 95% confidence interval [CI]: 0.66∼0.96), CV mortality (OR = 0.78, 95%CI: 0.63∼0.96), and fatal re-infarction (OR = 0.75, 95%CI: 0.59∼0.95). The OR for sudden death at one year (OR = 0.63, 95%CI: 0.41∼0.97) was also significantly lower in the CRET group compared to the control group. The two and three year follow-up data trended toward a CRET benefit for sudden death, but did not reach statistical significance.
A study published in 2010 examined 30,161 elderly patients who attended at least one CRET session over a five year period.[10] It was found that patients who attended 36 sessions had a 14% lower risk of death (hazard ratio [HR] = 0.86; 95%CI: 0.77∼0.97) and a 12% lower risk of MI (HR = 0.88; 95%CI: 0.83∼0.93) than those who attended 24 or less sessions. Moreover, patients attending 36 sessions had a 22% lower risk of death (HR = 0.78; 95%CI: 0.71∼0.87) and a 23% lower risk of MI (HR = 0.77; 95%CI: 0.69∼0.87) than those who attended 12 or less sessions, and a 47% lower risk of death (HR = 0.53; 95%CI: 0.48∼0.59) and a 31% lower risk of MI (HR = 0.69; 95% CI: 0.58∼0.81) than those who attended only one session.
Another study evaluated the one to five year mortality rates of CRET users and non-users among 601,099 United States (US) Medicare beneficiaries hospitalized for CHD conditions or cardiac revascularization procedures.[11] Only 12.2% of the cohort, averaging 24 sessions, used CRET and showed significantly lower (P < 0.001) 1 to 5-year mortality rates (21% to 34%) in users compared to non-users.
2.2. Aerobic exercise capacity
Simply put, aerobic exercise capacity is the maximum amount of physical exertion an individual can sustain. For proper assessment of exercise capacity, the patient is required to provide maximal exertion for a period of time that creates a stable effect on the circulation that is reproducible when exertion is repeated.[12] One of the most significant benefits of formal CRET within all participating age groups is the improvement of aerobic exercise capacity and CRF. Following participation in CRET, the patient improvement in aerobic exercise capacity validated in a higher level of fitness, irrespective of patient characteristics, afforded such a high priority which equates to improved prognosis, it is secondary to the wealth of other data.[13] In this context, elderly patients were found to have greater improvements in exercise capacity compared to younger patients after CRET (Table 1).[14]
Table 1. Benefit of CRET programs in elderly CHD patients.
| Improvements in Exercise Capacity | Changes |
| Estimated METs | +34% |
| Maximal oxygen consumption (peak VO2) | +13% |
| Anabolic threshold | +11% |
| Improvements in Lipids | |
| Total cholesterol | −1% |
| HDL-C | +3% |
| LDL-C | 0% |
| Triglycerides | −5% |
| Total cholesterol/HDL-C | −4% |
| LDL-C/HDL-C | −3% |
| Reduction in Obesity Indices | |
| Weight | −1% |
| % Body fat | −6% |
| Body mass index | −1% |
| Improvements in Blood Rheology | |
| Reduction in homocysteine levels | * |
| Improvement in viscosity | * |
| Major Morbidity and Mortality | |
| Reduction in overall mortality | * |
| Reduction in congestive heart failure | * |
| Reduction in hospital costs | * |
| Reduction in non-fatal MI | * |
| Improvement in Psychological Factors | |
| Depression score | −12.6% |
| Anxiety score | −4.3% |
| Hostility score | −2.3% |
One of the earliest studies on exercise training in an elderly CHD cohort was published in 1985 by Williams et al.[15] The goal was to study any potential benefits that early exercise programs may have on elderly CHD patients. All patients participated in a 12-week exercise program within six weeks of acute MI or coronary artery bypass grafting (CABG). The study showed that elderly patients exhibited significant changes in maximal heart rate (126 to 138 beats/min), maximal metabolic equivalents (METs) (5.3 to 8.1), as well as other parameters. Furthermore, among the 25 elderly patients receiving a beta-blocking agent, peak METs increased from 5.1 to 7.8 (P < 0.05). In the remaining 51 elderly patients not receiving a beta-blocking agent, peak METs increased from 5.4 to 8.2 (P < 0.05). It should be noted that the magnitude of increase in peak METs was not significantly different according to beta-blocker use.
A 1993 study[16] documenting CRET benefits was comprised of 92 patients > 65 years and 182 patients < 65 years who were enrolled in phase II CRET after a major CHD event. At baseline, estimated peak METs (5.6 ± 1.6 vs. 7.7 ± 3.0, P < 0.0001) was lower in elderly patients. After CRET, the older patients showed significant improvements in peak METs (5.6 ± 1.6 vs. 7.5 ± 2.3, P < 0.0001). Moreover, improvements in functional capacity, percent body fat and body mass index, as well as lipids, were statistically similar in the older and younger patients. These results highlight the importance of referring all eligible patients to CRET irrespective of age.
In an age related study, Lavie and Milani[17] evaluated 125 younger ( < 55 years) and 57 elderly CHD patients ( > 70 years) in an effort to determine the impact of formal Phase II CRET programs (supervised ambulatory outpatient programs spanning 3–6 months) on cardiopulmonary variables and QoL. Before initiation of CRET, elderly patients were found to have a lower estimated aerobic exercise capacity (≥ 27%; P < 0.001), peak oxygen consumption (VO2) (≥ 19%; P < 0.01), and anaerobic threshold (−10%; P < 0.05), as well as total function scores (≥ 11%; P < 0.01) and a trend toward total QoL scores (≥ 5%; P = 0.06). Following CRET, the elderly patients were found to have significant improvements in estimated aerobic exercise capacity (+32%; P < 0.0001), peak VO2 (+13%; P < 0.0001), anaerobic threshold (+11%; P = 0.03), total function scores (+27%; P < 0.0001), and total QoL scores (+20%; P < 0.0001). Although younger patients showed greater improvements in estimated aerobic exercise capacity (+44% vs. +32%; P = 0.08) and peak VO2 (+18% vs. +13%; P < 0.01), the elderly had statistically greater improvements in both function scores (+27% vs. +20%; P = 0.02), as well as total QoL scores (+20% vs. +14%; P = 0.03).
Another study by McConnell et al.[18] evaluated 581 CRET patients of various age groups (40s, 50s, 60s, and 70s) and gender (125 females; 456 males) and examined trends with regards to peak exercise capacity, body composition, and lipids. Although peak exercise capacity decreased with increasing age, the percentage improvement attributed to CRET was similar across all the age groups. Women were found to have lower peak exercise capacities when compared to men, but showed similar relative improvements (26.6% and 28.8%, respectively) after CRET. The study concluded CRET showed favorable outcomes with respect to peak exercise capacity and CRF, body composition, and lipids, across each age group regardless of gender.
Over the last decade, it has been shown that there is a discrepancy and overestimation of CRF when assessing exercise capacity using estimated METs when compared to precise measurement of functional capacity using peak VO2.[19] However, despite this discrepancy between estimated METs and measured peak VO2, studies have shown that both measurements of CRF robustly predict prognosis among patients.[20],[21]
2.3. Psychological risk factors
It is becoming increasingly evident that psychological risk factors and CHD are intertwined more closely than initially suspected five decades ago.[22] Depression has been shown to be independently associated with CV morbidity and mortality.[23] Although the roles of anxiety and hostility on CHD are less clear, there is substantial evidence to suggest these risk factors negatively impact CV health.[24]
Ariyo et al.[25] showed a significant association between depression and CHD in the elderly. The authors of the study examined 4493 Americans ≥ 65 years of age over a six year period for the development of CHD and mortality. The effect of depression was assessed by a modified version of the Depression Scale of the Center for Epidemiological Studies. This 10-item scale recorded participants' depression scores as a continuous measure from 0 to 30. It determined the unadjusted HR for the development of CHD was 1.2 (P = 0.006) for every 5-unit increase in mean depression score; the HR for all-cause mortality was 1.3 (P < 0.0001).
A study published in 2004 by Lavie et al.[26] examined the prevalence of high hostility symptoms in elderly patients compared to younger patients, as well as the effect of formal CRET programs among these individuals. The study included 500 consecutive patients following CHD events to determine the impact of aging on hostility scores, prevalence of hostility symptoms, and the impact of CRET on elderly patients with hostility. It was found that higher hostility scores and the prevalence of hostility symptoms were inversely related to age (P < 0.01). Elderly person with hostility symptoms had a greater body weight (P = 0.02), four times higher anxiety and depression scores (P < 0.0001), two times higher scores for somatization (P < 0.0001), and 17% lower scores for QoL (P < 0.001) compared with elderly persons without hostility symptoms. The study demonstrated marked reduction in hostility following CR. Furthermore, the authors showed that although hostility symptoms are relatively uncommon in elderly persons with CHD, these patients have a worse CHD risk profiles and have marked improvements following CRET programs.
Lavie and Milani[27] evaluated 104 younger CHD patients (age < 55 years) and compared this group with a group of 260 older CHD patients (age > 70 years). After formal CRET, the prevalence of anxiety fell by 61% in the younger patients and by 32% in the older patients, suggesting CRET has a significant effect on anxiety reduction.
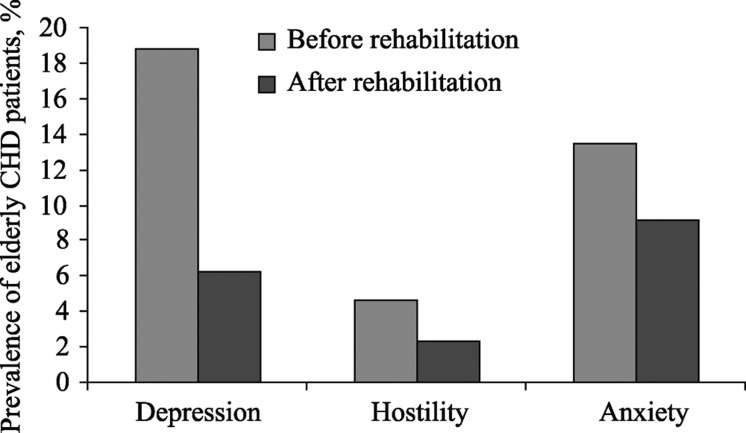
In addition to the benefits on CV health, CRET has been shown to have positive effects on psychological stress, including a significant reduction in mortality related to depression, as well as other psychological risk factors,[28],[29] (Figure 1).
Figure 1. Prevalence of psychological risk factors in elderly coronary heart disease (CHD) patients before and after cardiac rehabilitation and exercise therapy (CRET). (n = 260, mean age 75 ± 3 years). Adapted from Lavie CJ & Milani RV.[27].
2.4. Inflammation
There is strong evidence linking inflammation, particularly elevated levels of C-reactive protein (CRP), to atherosclerotic vascular events and CHD.[30] Although other inflammation markers, such as myeloperoxidase, pentraxin-3, interleukin-6, and metalloproteinase-9, may also have a role in the development of CHD events, CRP is the most clinically applicable indicator, due to its chemical stability, relatively long half-life, lack of significant precautions required for sampling, lack of diurnal variation, and substantial clinical evidence.[31]
In addition to the role of CRP as a marker of CV risk, studies have shown that high CRP levels may be a focus (signal) for intervention. In the Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis in Myocardial Infarction 22 trial (PROVE-IT 22),[32] the study demonstrated that regardless of low-density lipoprotein cholesterol (LDL-C) levels, patients who have low CRP levels after statin therapy have better clinical outcomes than those with higher CRP levels.
In 2008, the Justification for Use of Statins in Prevention: An Intervention Trial Evaluating Rosuvastatin (JUPITER)[33] demonstrated that individuals with normal LDL-C levels, but elevated CRP levels, have a increased incidence of CV events.
In addition to pharmacologic management of elevated CRP levels, non-pharmacologic approaches, such as weight loss[34] and CRET, have also been shown to be therapeutic. A study by Milani et al.[35] assessed the effects of three months of CRET programs on high-sensitivity CRP levels in CHD patients. Among the 277 patients assessed, 235 (mean age 67 ± 11) completed CRET while 42 control patients who did not attend CRET. After CRET, the mean (5.9 ± 7.7 mg/L to 3.8 ± 5.8 mg/L; −36%; P < 0.0001) and median levels of high sensitivity CRP (−41%; P = 0.002) decreased significantly among patients in the CRET group. This improvement was not seen in the control population. Rehabilitation patients experienced similar significant reductions in high sensitivity CRP regardless of whether they received statin therapy or experienced weight loss.
Another study examined CRP levels in 172 patients with CHD who participated in a CRET program.[36] Patients who participated in CRET demonstrated significant improvements in CRP (−3.1, P = 0.003). These improvements in CRP did not differ significantly based on age, or the presence of metabolic syndrome (MS).
In conclusion, increased inflammation, typically depicted by CRP, appears to be a strong indicator of CV health and the risk for adverse events. Pharmacologic approaches have convincingly demonstrated the value of reducing inflammation on prognosis. CRET has also been shown to significantly improve inflammation and may be one of several key mechanisms through which a significant risk reduction is realized following participation in this lifestyle intervention.
2.5. Obesity
Obesity and a metabolic syndrome (MS) currently represent an epidemic in the US.[37] Over time, numerous studies have demonstrated that these individuals are more likely to be predisposed to hypertension (HTN), insulin resistance, dyslipidemia, heart failure (HF), obstructive sleep apnea, in addition to other medical conditions.
Before discussing the beneficial effects of formal CRET on obesity indices as well as MS among the elderly, the “obesity paradox” should be mentioned. The obesity paradox is the counterintuitive observation in which obese patients with CHD or HF have better prognosis than leaner patients.[38],[39] Others have demonstrated the relative safety and efficacy of intentional weight loss among obese patients with CHD.[40] Among elderly patients, this paradoxical effect has been observed even among those without CV disease,[41] with certain exceptions, such as elderly patients with abnormal left ventricular geometry and preserved systolic function.[42] At present, there is currently a lack of evidence regarding the beneficial effects of weight loss programs among the elderly. Nonetheless, studies have shown that formal CRET programs have significant benefits on obesity indices among the general population,[43] as well as elderly.[44]–[46] It should be noted there is little evidence pertaining to safety and efficacy of weight loss programs among the elderly. Regardless, it is very probable that intentional weight loss in a controlled setting with proper diet control and ET is beneficial among elderly obese patients, despite the obesity paradox. Further studies are needed to clarify this issue.
3. Under-utilization of CRET in the elderly
Despite the beneficial effects of formal CRET programs as described above, there is considerable evidence to suggest that the participation rates among many eligible patients is far less than ideal. The reasons behind this are many and can be appreciated on multiple levels beginning with the patient and involving other factors, such as poor referral and encouragement by physicians, inconvenience, and a lack of importance placed on preventative medicine.
Suaya et al.[45] evaluated outpatient CRET usage after post-hospitalization for acute MI or CABG surgery on a total of 267,427 patients aged ≥ 65 year old who survived for a minimum of 30 days after discharge. They found CRET was utilized in 13.9% of the patients who were hospitalized for acute MI and 31.0% of the patients after CABG surgery. They found that the older individuals, women, nonwhites, and patients with co-morbidities (including HF, previous stroke, diabetes mellitus, or cancer) were significantly less likely to receive CRET. In general, women were less likely to attend CRET than men,[46] a finding consistent among older women as well. This is almost certainly due to the fact that older female coronary patients were less likely to be referred for CRET, despite an overall clinical profile similar to other patients with higher referral rates.[47] In addition to poor participation by women, persons over the age of 65,[48] minorities,[49] lower socio- economic status,[50] and the unemployed[51] have all been associated with lower CRET participation rates.
Another factor that affects participation in CRET programs involves physician referral and encouragement. A study of 226 patients with a mean age of 70.4 ± 6 years showed the overall CRET enrollment rate in this cohort was only 21%.[52] More importantly, multivariate analysis showed the strength of the endorsement of the primary physician was the most powerful predictor of CRET participation.
It has also been demonstrated that the type of provider that refers the patient to CRET also plays a strong role in participation and attendance. Patients cared for by a cardiologist or cardiac surgeon are more likely to participate in CRET compared to those under the care of a primary care physician.[53]
Finally, the patient must be willing to participate in CRET programs. It is very likely that in our society, patients may not place as much value on preventative measures. Over the last few decades, there has been a decrease in physical activity[54] with a concomitant rise in overweight and obese[55] patients. This culture of physical inactivity, particularly with reference to CRET participation, has been attributed to such factors as inconvenience,[56] lack of understanding of the disease process,[57] lack of transportation,[58] responsibilities at home,[59] as well as numerous other factors.
4. Safety of CRET in the elderly
One of the potential concerns that adversely impact referral is the perceived safety of CRET, especially among elderly patients. Van Camp et al.[60] sought to determine the incidence of major CV complications in outpatient CRET settings. They obtained data from 167 randomly selected CRET programs that included 51,303 patients who had exercised 2,351,916 hours from January 1980 through December 1984. Over the four-year period, they observed 21 cardiac arrests (18 in which the patient was successfully resuscitated and three fatal) and 8 non-fatal MI's and incidence rates per 1,000,000 patient hours of exercise were 8.9 for cardiac arrests, 3.4 for MI's, and 1.3 for fatalities. These data showed the risk of CV complications, although present, was extremely low. Studies completed by co- authors of this paper have also shown no occurrence of significant CV events among elderly patients during CRET.[17],[19],[20],[29],[47] Unfortunately, there are no large studies that have evaluated the overall safety of CRET programs among the elderly. Even so, there is no reason or rationale to suspect an increased risk of adverse events in properly screened and supervised elderly patients participating in CRET.
5. Clinical implications
(1) Elderly CHD patients should be referred for CRET with proper explanation of their disease process and achievable benefits from formal CRET programs.
(2) Elderly CHD patients should be repeatedly encouraged to participate in CRET programs due to the demonstrated benefit and relatively low risk.
(3) Elderly CHD patients who do not participate in CRET programs should still be encouraged to exercise for at least 30 min on most days, preferably at least 45 min 4∼5 times weekly.[7]
(4) The patient should be referred to CRET programs with a proper prescription that describes the mode of ET, duration, intensity and frequency.[5],[8]
6. Conclusion
CHD is a major cause of morbidity and mortality among elderly patients. Over the last few decades, there has been increased interest in the role CRET programs, among patients of all ages. The beneficial effects of these programs on mortality, exercise capacity, psychological risk factors, inflammation, and obesity documented in younger cohorts is also consistent among elderly patients. However, elderly patients are universally underrepresented in CRET programs for various reasons. Due to the evidence-based benefits obtained from CRET, physicians should place more attention on referring and encouraging elderly patients to participate and attend these programs. One of the major limitations of this review arises from the fact that a large amount of the available information comes from observational studies of attendees versus non-attendees. The fact that these studies lack randomization creates a selection bias with regards to those are able to attend versus those that are unable to do so. It would be unethical to randomize patients into either group since CRET is currently considered standard of care.
References
- 1.Heron M, Hoyert DL, Murphy SL, et al. Deaths: Final Data for 2006. Natl Vital Stat Rep. 2009;57:1–134. [PubMed] [Google Scholar]
- 2.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suaya JA, Stason WB, Ades PA, et al. Cardiac rehabilitation and survival in older coronary patients. J Am Coll Cardiol. 2009;54:25–33. doi: 10.1016/j.jacc.2009.01.078. [DOI] [PubMed] [Google Scholar]
- 4.Wenger NK. Current status of cardiac rehabilitation. J Am Coll Cardiol. 2008;51:1619–1631. doi: 10.1016/j.jacc.2008.01.030. [DOI] [PubMed] [Google Scholar]
- 5.Lavie CJ, Thomas RJ, Squires RW, et al. Exercise training and cardiac rehabilitation in primary and secondary prevention of coronary heart disease. Mayo Clin Proc. 2009;84:373–383. doi: 10.1016/S0025-6196(11)60548-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leon AS, Franklin BA, Costa F, et al. Cardiac rehabilitation and secondary prevention of coronary heart disease: an American Heart Association scientific statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity), in collaboration with the American association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2005;111:369–376. doi: 10.1161/01.CIR.0000151788.08740.5C. [DOI] [PubMed] [Google Scholar]
- 7.Lavie CJ, Milani RV, Arena RA. Particular utility of cardiac rehabilitation in relation to age. Curr Cardiovasc Risk Rep. 2011;5:432–439. [Google Scholar]
- 8.Balducci S, Zanuso S, Nicolucci A, et al. Effect of an intensive exercise intervention strategy on modifiable cardiovascular risk factors in subjects with type 2 diabetes mellitus: a randomized controlled trial: the Italian Diabetes and Exercise Study (IDES) Arch Intern Med. 2010;170:1794–1803. doi: 10.1001/archinternmed.2010.380. [DOI] [PubMed] [Google Scholar]
- 9.O'Connor GT, Buring JE, Yusuf S, et al. An overview of randomized trials of rehabilitation with exercise after myocardial infarction. Circulation. 1989;80:234–244. doi: 10.1161/01.cir.80.2.234. [DOI] [PubMed] [Google Scholar]
- 10.Hammill BG, Curtis LH, Schulman KA, et al. Relationship between cardiac rehabilitation and long-term risks of death and myocardial infarction among elderly Medicare beneficiaries. Circulation. 2010;121:63–70. doi: 10.1161/CIRCULATIONAHA.109.876383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Suaya JA, Stason WB, Ades PA, et al. Cardiac rehabilitation and survival in older coronary patients. J Am Coll Cardiol. 2009;54:25–33. doi: 10.1016/j.jacc.2009.01.078. [DOI] [PubMed] [Google Scholar]
- 12.Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd Edition. Butterworth Publishers; 1990. [PubMed] [Google Scholar]
- 13.Arena R, Myers J, Guazzi M. The future of aerobic exercise testing in clinical practice: is it the ultimate vital sign? Future Cardiol. 2010;6:325–342. doi: 10.2217/fca.10.21. [DOI] [PubMed] [Google Scholar]
- 14.Lavie CJ, Milani RV. Effects of cardiac rehabilitation programs on exercise capacity, coronary risk factors, behavioral characteristics, and quality of life in a large elderly cohort. Am J Cardiol. 1995;76:177–179. doi: 10.1016/s0002-9149(99)80054-x. [DOI] [PubMed] [Google Scholar]
- 15.Williams MA, Maresh CM, Esterbrooks DJ, et al. Early exercise training in patients older than age 65 years compared with that in younger patients after acute myocardial infarction or coronary artery bypass grafting. Am J Cardiol. 1985;55:263–266. doi: 10.1016/0002-9149(85)90357-1. [DOI] [PubMed] [Google Scholar]
- 16.Lavie CJ, Milani RV, Littman AB. Benefits of cardiac rehabilitation and exercise training in secondary coronary prevention in the elderly. J Am Coll Cardiol. 1993;22:678–683. doi: 10.1016/0735-1097(93)90176-2. [DOI] [PubMed] [Google Scholar]
- 17.Lavie CJ, Milani RV. Disparate effects of improving aerobic exercise capacity and quality of life after cardiac rehabilitation in young and elderly coronary patients. J Cardiopulm Rehabil. 2000;20:235–240. doi: 10.1097/00008483-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 18.McConnell TR, Laubach CA, 3rd, Szmedra L. Age and gender related trends in body composition, lipids, and exercise capacity during cardiac rehabilitation. Am J Geriatr Cardiol. 1997;6:37–45. [PubMed] [Google Scholar]
- 19.Milani RV, Lavie CJ, Spiva H. Limitations of estimating metabolic equivalents in exercise assessment in patients with coronary artery disease. Am J Cardiol. 1995;75:940–942. doi: 10.1016/s0002-9149(99)80693-6. [DOI] [PubMed] [Google Scholar]
- 20.Kavanagh T, Mertens DJ, Hamm LF, et al. Prediction of long-term prognosis in 12169 men referred for cardiac rehabilitation. Circulation. 2002;106:666–671. doi: 10.1161/01.cir.0000024413.15949.ed. [DOI] [PubMed] [Google Scholar]
- 21.Kavanagh T, Mertens DJ, Hamm LF, et al. Peak oxygen intake and cardiac mortality in women referred for cardiac rehabilitation. J Am Coll Cardiol. 2003;42:2139–2143. doi: 10.1016/j.jacc.2003.07.028. [DOI] [PubMed] [Google Scholar]
- 22.Menezes AR, Lavie CJ, Milani RV, et al. Psychological risk factors and cardiovascular disease: is it all in your head? Postgrad Med. 2011;123:165–176. doi: 10.3810/pgm.2011.09.2472. [DOI] [PubMed] [Google Scholar]
- 23.Lichtman JH, Bigger JT, Jr, Blumenthal JA, et al. AHA science advisory. Depression and coronary heart disease. Recommendations for screening, referral, and treatment. A science advisory from the American Heart Association Prevention Committee to the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care Outcomes Research. Prog Cardiovasc Nurs. 2009;24:19–26. doi: 10.1111/j.1751-7117.2009.00028.x. [DOI] [PubMed] [Google Scholar]
- 24.Janszky I, Ahnve S, Lundberg I, et al. Early-onset depression, anxiety, and risk of subsequent coronary heart disease: 37-year follow-up of 49,321 young Swedish men. J Am Coll Cardiol. 2010;56:31–37. doi: 10.1016/j.jacc.2010.03.033. [DOI] [PubMed] [Google Scholar]
- 25.Ariyo AA, Haan M, Tangen CM, et al. Depressive symptoms and risks of coronary heart disease and mortality in elderly Americans. Circulation. 2000;102:1773–1779. doi: 10.1161/01.cir.102.15.1773. [DOI] [PubMed] [Google Scholar]
- 26.Lavie CJ, Milani RV. Impact of aging on hostility in coronary patients and effects of cardiac rehabilitation and exercise training in elderly persons. Am J Geriatr Cardiol. 2004;13:125–130. doi: 10.1111/j.1076-7460.2004.03285.x. [DOI] [PubMed] [Google Scholar]
- 27.Lavie CJ, Milani RV. Adverse psychological and coronary risk profiles in young patients with coronary artery disease and benefits of formal cardiac rehabilitation. Arch Intern Med. 2006;166:1878–1883. doi: 10.1001/archinte.166.17.1878. [DOI] [PubMed] [Google Scholar]
- 28.Milani RV, Lavie CJ. Reducing psychosocial stress: a novel mechanism of improving survival from exercise training. Am J Med. 2009;122:931–938. doi: 10.1016/j.amjmed.2009.03.028. [DOI] [PubMed] [Google Scholar]
- 29.Milani RV, Lavie CJ, Mehra MR, et al. Impact of exercise training and depression on survival in heart failure due to coronary heart disease. Am J Cardiol. 2011;107:64–68. doi: 10.1016/j.amjcard.2010.08.047. [DOI] [PubMed] [Google Scholar]
- 30.Danesh J, Wheeler JG, Hirschfield GM, et al. C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. N Engl J Med. 2004;350:1387–1397. doi: 10.1056/NEJMoa032804. [DOI] [PubMed] [Google Scholar]
- 31.Lavie CJ, Church TS, Milani RV, et al. Impact of physical activity, cardiorespiratory fitness, and exercise training on markers of inflammation. J Cardiopulm Rehabil Prev. 2011;31:137–145. doi: 10.1097/HCR.0b013e3182122827. [DOI] [PubMed] [Google Scholar]
- 32.Ridker PM, Cannon CP, Morrow D, et al. C-reactive protein levels and outcomes after statin therapy. N Engl J Med. 2005;352:20–28. doi: 10.1056/NEJMoa042378. [DOI] [PubMed] [Google Scholar]
- 33.Ridker PM, Danielson E, Fonseca FA, et al. Rosuvastatin to Prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359:2195–2207. doi: 10.1056/NEJMoa0807646. [DOI] [PubMed] [Google Scholar]
- 34.Lavie CJ, Milani RV, Verma A, et al. C-reactive protein and cardiovascular diseases—is it ready for primetime? Am J Med Sci. 2009;338:486–492. doi: 10.1097/MAJ.0b013e3181c61b66. [DOI] [PubMed] [Google Scholar]
- 35.Milani RV, Lavie CJ, Mehra MR. Reduction in C-reactive protein through cardiac rehabilitation and exercise training. J Am Coll Cardiol. 2004;43:1056–1061. doi: 10.1016/j.jacc.2003.10.041. [DOI] [PubMed] [Google Scholar]
- 36.Caulin-Glaser T, Falko J, Hindman L, et al. Cardiac rehabilitation is associated with an improvement in C-reactive protein levels in both men and women with cardiovascular disease. J Cardiopulm Rehabil. 2005;25:332–336. doi: 10.1097/00008483-200511000-00003. [DOI] [PubMed] [Google Scholar]
- 37.Artham SM, Lavie CJ, Milani RV. Value of weight reduction in patients with cardiovascular disease. Curr Treat Options Cardiovasc Med. 2010;12:21–35. doi: 10.1007/s11936-009-0056-y. [DOI] [PubMed] [Google Scholar]
- 38.Artham SM, Lavie CJ, Patel HM, et al. Impact of obesity on the risk of heart failure and its prognosis. J Cardiometab Syndr. 2008;3:155–161. doi: 10.1111/j.1559-4572.2008.00001.x. [DOI] [PubMed] [Google Scholar]
- 39.Lavie CJ, Milani RV, Ventura HO. Obesity, heart disease, and favorable prognosis—truth or paradox? Am J Med. 2007;120:825–826. doi: 10.1016/j.amjmed.2007.06.023. [DOI] [PubMed] [Google Scholar]
- 40.Lavie CJ, Milani RV. Cardiac rehabilitation and exercise training programs in metabolic syndrome and diabetes. J Cardiopulm Rehabil. 2005;25:59–66. doi: 10.1097/00008483-200503000-00001. [DOI] [PubMed] [Google Scholar]
- 41.Artham SM, Lavie CJ, Patel DA, et al. Obesity paradox in the elderly: is fatter really fitter? Aging Health. 2009;5:177–184. [Google Scholar]
- 42.Lavie CJ, Milani RV, Ventura HO, et al. Left ventricular geometry and mortality in patients > 70 years of age with normal ejection fraction. Am J Cardiol. 2006;98:1396–1399. doi: 10.1016/j.amjcard.2006.06.037. [DOI] [PubMed] [Google Scholar]
- 43.Milani RV, Lavie CJ. The effects of body composition changes to observed improvements in cardiopulmonary parameters after exercise training with cardiac rehabilitation. Chest. 1998;113:599–601. doi: 10.1378/chest.113.3.599. [DOI] [PubMed] [Google Scholar]
- 44.Lavie CJ, Milani RV. Effects of cardiac rehabilitation programs in very elderly patients ≥ 75 years of age. Am J Cardiol. 1995;76:177–179. doi: 10.1016/s0002-9149(99)80054-x. [DOI] [PubMed] [Google Scholar]
- 45.Suaya JA, Shepard DS, Normand SL, et al. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116:1653–1662. doi: 10.1161/CIRCULATIONAHA.107.701466. [DOI] [PubMed] [Google Scholar]
- 46.Thomas RJ, Miller NH, Lamendola C, et al. National survey on gender differences in cardiac rehabilitation programs. Patient characteristics and enrollment patterns. J Cardiopulm Rehabil. 1996;16:402–412. doi: 10.1097/00008483-199611000-00010. [DOI] [PubMed] [Google Scholar]
- 47.Ades PA, Waldmann ML, Polk DM, et al. Referral patterns and exercise response in the rehabilitation of female coronary patients aged greater than or equal to 62 years. Am J Cardiol. 1992;69:1422–1425. doi: 10.1016/0002-9149(92)90894-5. [DOI] [PubMed] [Google Scholar]
- 48.Centers for Disease Control and Prevention (CDC) receipt of outpatient cardiac rehabilitation among heart attack survivors—United States, 2005. MMWR Morb Mortal Wkly Rep. 2008;57:89–94. [PubMed] [Google Scholar]
- 49.Witt BJ, Thomas RJ, Roger VL. Cardiac rehabilitation after myocardial infarction: a review to understand barriers to participation and potential solutions. Eura Medicophys. 2005;41:27–34. [PubMed] [Google Scholar]
- 50.Hiatt AM, Hoenshell-Nelson N, Zimmerman L. Factors influencing patient entrance into a cardiac rehabilitation program. Cardiovasc Nurs. 1990;26:25–29. [PubMed] [Google Scholar]
- 51.Lane D, Carroll D, Ring C, et al. Predictors of attendance at cardiac rehabilitation after myocardial infarction. J Psychosom Res. 2001;51:497–501. doi: 10.1016/s0022-3999(01)00225-2. [DOI] [PubMed] [Google Scholar]
- 52.Ades PA, Waldmann ML, McCann WJ, et al. Predictors of cardiac rehabilitation participation in older coronary patients. Arch Intern Med. 1992;152:1033–1035. [PubMed] [Google Scholar]
- 53.Barber K, Stommel M, Kroll J, et al. Cardiac rehabilitation for community-based patients with myocardial infarction: factors predicting discharge recommendation and participation. J Clin Epidemiol. 2001;54:1025–1030. doi: 10.1016/s0895-4356(01)00375-4. [DOI] [PubMed] [Google Scholar]
- 54.Caban-Martinez AJ, Lee DJ, Fleming LE, et al. Leisure-time physical activity levels of the US workforce. Prev Med. 2007;44:432–436. doi: 10.1016/j.ypmed.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 55.Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol. 2009;53:1925–1932. doi: 10.1016/j.jacc.2008.12.068. [DOI] [PubMed] [Google Scholar]
- 56.Ramm C, Robinson S, Sharpe N. Factors determining non-attendance at a cardiac rehabilitation programme following myocardial infarction. N Z Med J. 2001;114:227–229. [PubMed] [Google Scholar]
- 57.Whitmarsh A, Koutantji M, Sidell K. Illness perceptions, mood and coping in predicting attendance at cardiac rehabilitation. Br J Health Psychol. 2003;8(Pt 2):209–221. doi: 10.1348/135910703321649178. [DOI] [PubMed] [Google Scholar]
- 58.King KM, Humen DP, Smith HL, et al. Predicting and explaining cardiac rehabilitation attendance. Can J Cardiol. 2001;17:291–296. [PubMed] [Google Scholar]
- 59.Gallagher R, McKinley S, Dracup K. Predictors of women's attendance at cardiac rehabilitation programs. Prog Cardiovasc Nurs. 2003;18:121–126. doi: 10.1111/j.0889-7204.2003.02129.x. [DOI] [PubMed] [Google Scholar]
- 60.Van Camp SP, Peterson RA. Cardiovascular complications of outpatient cardiac rehabilitation programs. JAMA. 1986;256:1160–1163. doi: 10.1001/jama.256.9.1160. [DOI] [PubMed] [Google Scholar]