Abstract
A 74-year-old immunocompetent man admitted for severe retro-orbital headache was diagnosed with isolated sphenoiditis. At the time of scheduled surgery, the patient was mildly obtunded, and a head CT revealed a temporal lobe abscess. The patient underwent a left temporal craniectomy and a bilateral endoscopic sphenoid sinusotomy, which revealed gross fungal debris. The patient made a full recovery with resolution of abscess and sinus findings. Suspicion for intracranial infection should be raised in any sinus patient with neurological changes. Early diagnosis with imaging studies is extremely important for surgical drainage before permanent neurological sequelae.
Keywords: Abcess, allergic sinusitis, fungal infection, headache, sinonasal, sphenoiditis, temporal lobe
Isolated sphenoid sinusitis accounts for 2–3% of all sinus infections evaluated by radiological imaging. Fungal sphenoiditis is present in ∼5% of isolated sphenoiditis. Noninvasive fungal sphenoid sinusitis rarely presents with serious complications. However, diplopia and/or transient vision loss have been reported in up to 3% of cases. Intracranial extension and cerebral abscess is another serious complication of isolated sphenoiditis and although similar cases have been previously reported, intracranial complications from fungal sinusitis are exceedingly rare. Intracranial extension from sinusitis is a rare but potentially fatal disease characterized by bony erosion of the skull base and extension into the adjacent cavities, such as the orbit or cranial vault. It is usually associated with acute fulminant invasive fungal sinusitis in the immunocompromised population, such as patients who have undergone hematopoietic stem cell transplantation or solid organ transplant, those with human immunodeficiency virus/acquired immunodeficiency syndrome or diabetes mellitus, or those who are undergoing treatment with chemotherapy or immunosuppressants.1 However, this complication has now been shown to very rarely occur in immunocompetent individuals as well and seems to be increasing in frequency in this population.1–4
Of the approximately 20 pathogenic fungi, the three most common fungal infections in the nasal sinuses are the opportunistic genera of Aspergillus, Mucor, and Candida, of which Aspergillus is the most prevalent organism.5 Although rare, each of these can invade the adjacent structures, with Mucor being the most invasive and requiring the most aggressive surgical treatments. Intracranial extension and abscess formation most commonly occurs from the frontal sinus to the frontal and frontoparietal areas of the brain.1 The rarest occurrence of invasive fungal sinusitis is seen in the sphenoid sinus, because of only 2.7% of all sinus infections occurring there.6 The rarity of this infection in comparison with other sinuses is because of both the anatomic orientation of the sphenoid sinus receiving little directed airflow and because the sinus mucosa is lined by relatively few glands, producing less mucus to serve as a reservoir for infection.7 When invasion does occur from the sphenoid sinus, it can occur through one of two mechanisms: retrograde thrombophlebitis through diploic veins of the skull or by direct extension through normal anatomic pathways or wall erosion.8 The infection can either enter the frontoparietal areas of the brain similar to extension from the frontal and ethmoid sinuses, or it can extend into the cavernous sinus, causing visual defects secondary to destruction of cranial nerves III, IV, V, and VI. Another potential site of invasion is the temporal lobe, which has rarely been documented.7,8
CASE REPORT
A 74-year-old immunocompetent man with history of chronic hypertension and chronic obstructive pulmonary disease was admitted with severe retro-orbital headache. A routine brain window CT scan revealed incindental isolated sphenoiditis (Fig. 1). After appropriate workup there was no other finding or comorbidity attributable to the patient's headache. The patient was subsequently scheduled for sinus surgery as an outpatient. At the time of surgery, the patient presented with mild obtundation, confusion, and receptive aphasia (Fig. 2). The patient was subsequently transferred to the university hospital for further workup. A head CT (Fig. 3) with contrast and an MRI with contrast both revealed two lobulated, rim-enhancing lesions with surrounding edema and local mass effect in the left temporal lobe, suggestive of brain abscesses (Figs. 4 and 5).
Figure 1.

Brain window head CT showing incidental sphenoiditis with no intracranial pathology.
Figure 2.

Preoperative maxillofacial high-resolution computed tomography showing bilateral isolated sphenoiditis with osteosclerotic changes.
Figure 3.

Head CT showing multiple brain abscesses within the left posterior parietal and temporal lobes, prominent vasogenic edema causing regional sulcal effacement.
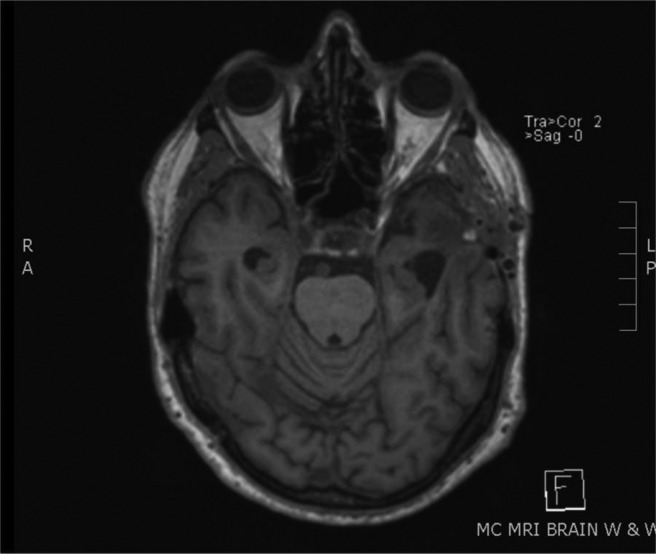
Figure 4.
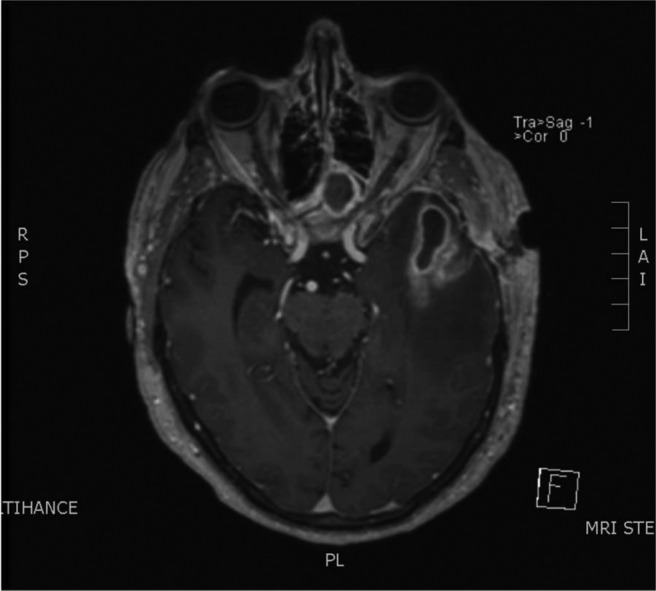
MRI with contrast; sphenoid sinusitis; rim enhancing lesions with surrounding edema and local mass effect in the left temporal lobe.
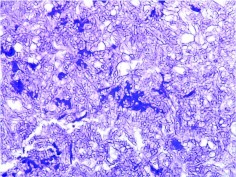
Figure 5.
Periodic acid schiff 100×. Branching pseudohyphae consistent with Candida spp., taken from a fungus ball removed from the sphenoid sinus.
The patient underwent a left temporal craniectomy using image-guided stereotaxy for drainage of the abscess and resection of necrotic tissue. Concurrently, the patient underwent a bilateral endoscopic sphenoid sinusotomy using endoscopic transnasal approach with image-guided navigation. The sphenoid sinus was widened with a microdebrider and was found to be impacted with gross fungal debris. Tissue from the sinus was removed along with the gross fungal debris, which was sent for culture. Sphenoid irrigation with saline and a posterior ethmoidectomy were then performed, creating a wide opening for the sphenoid sinus to drain. The pathology report confirmed Candida infection (Fig. 5). The patient was also started on i.v. antifungal therapy and continued on nasal saline irrigations for the remainder of the hospitalization. The patient made a full recovery postoperatively, with resolution of abscess and sinus findings on subsequent imaging (Fig. 6). One year postoperatively the patient had no residual neurological sequelae.
Figure 6.
Follow-up MRI 4 months postoperatively. Surgical changes consistent with left temporal craniotomy and underlying left temporal encephalomalacia. Otherwise resolved sphenoiditis and fluid collections.
DISCUSSION
Although intracranial extension of sphenoid sinusitis is rare, an index of suspicion should be maintained because of its severe morbidities and up to 30% mortality rate. This is compounded by the fact that the most common early presentation of isolated sphenoiditis is nonspecific headache, often misdiagnosed as a more benign process as the disease process continues untreated, which could increase the eventual progression into an intracranial complication.7 Careful attention should be paid to the course of symptoms in the patient, as the initial cerebritis causes a headache followed by an asymptomatic phase due to coalescence of the abscess.8 This is often followed directly by seizures or focal neurological deficits, both directly correlating with long-term morbidities.1 With subsequent rupture of the abscess, death commonly results. Diagnosis is made by CT or MRI showing cystic lesions.
Final bacterial cultures from the brain abscess and the sphenoid sinus revealed Streptococcus anginosus. We are suggesting direct extension of bacterial superinfection by one of two mechanisms: retrograde thrombophlebitis through diploic veins of the skull or by direct extension through normal anatomic pathways or wall erosion.
The treatment of choice for isolated fungal sinusitis with bacterial superinfection leading to intracranial abscess is surgical drainage of the affected sinus with concurrent broad-spectrum antifungal agents and the appropriate antibacterial agents, along with neurosurgical consultation for stereotactic aspiration or craniotomy.1 Although early intracerebral abscesses may resolve with medical therapy, a low threshold for aggressive intervention must be maintained because most cases will eventually require a neurosurgical procedure.8
CONCLUSION
Temporal lobe abscess secondary to bacterial superinfection of a noninvasive isolated fungal sphenoiditis is a rare and potentially life-threatening occurrence. This is particularly unusual in this case of an immunocompetent patient. The case presented is unique in regard to the location of intracranial invasion, as well as the diagnosis of bacterial superinfection of chonic fungal sinusitis leading to direct intracranial extension, a phenomenon much more highly associated with Aspergillus and Mucor. With early diagnosis and immediate surgical drainage, survival with a low chance of long-term morbidities significantly increases.
Footnotes
Presented at the Triological Society Combined Sections Meeting, Orlando, Florida, February 2010
Funded by the Loma Linda Department of Otolaryngology; this sponsorship did not influence the study design, collection, analysis, or interpretation of data; in the writing of the article; or the decision to submit the article to publication
The authors have no conflicts to declare pertaining to this article
REFERENCES
- 1. Epstein VA, Kern RC. Invasive fungal sinusitis and complications of rhinosinusitis. Otolaryngol Clin North Am 41:497–524, viii, 2008 [DOI] [PubMed] [Google Scholar]
- 2. Lin JJ, Wu CT, Hsia SH, et al. Pneumocephalus: A rare presentation of Candida sphenoid sinusitis. Pediatr Neurol 40:398–400, 2009 [DOI] [PubMed] [Google Scholar]
- 3. Chopra H, Dua K, Malhotra V, et al. Invasive fungal sinusitis of isolated sphenoid sinus in immunocompetent subjects. Mycoses 49:30–36, 2006 [DOI] [PubMed] [Google Scholar]
- 4. Sridhara SR, Paragache G, Panda NK, Chakrabarti A. Mucormycosis in immunocompetent individuals: An increasing trend. J Otolaryngol 34:402–406, 2005 [DOI] [PubMed] [Google Scholar]
- 5. Anselmo-Lima WT, Lopes RP, Valera FC, Demarco RC. Invasive fungal rhinosinusitis in immunocompromised patients. Rhinology 42:141–144, 2004 [PubMed] [Google Scholar]
- 6. Lew D, Southwick FS, Montgomery WW, et al. Sphenoid sinusitis. A review of 30 cases. N Engl J Med 309:1149–1154, 1983 [DOI] [PubMed] [Google Scholar]
- 7. Lawson W, Reino AJ. Isolated sphenoid sinus disease: An analysis of 132 cases. Laryngoscope 107:1590–1595, 1997 [DOI] [PubMed] [Google Scholar]
- 8. Giannoni CM, Stewart MG, Alford EL. Intracranial complications of sinusitis. Laryngoscope 107:863–867, 1997 [DOI] [PubMed] [Google Scholar]