Abstract
Introduction
The aim of this study was to determine the incidence of intra-abdominal hypertension (IAH) in patients with two or more categorized risk factors (CRF) for IAH, and their morbidity and mortality during their intensive care unit (ICU) stay.
Methods
Prospective cohort study carried out at a medical ICU. A total of 151 medical patients were enrolled during a period of 3 months. After ICU whole staff training, we conducted daily screening of the four CRF for IAH based on the World Society of Abdominal Compartment Syndrome (WSACS) guidelines (namely, diminished abdominal wall compliance, increased intraluminal content, increased abdominal content, and capillary leak syndrome or fluid resuscitation). In those patients with risk factors of at least two different categories (≥2 CRF), intra-abdominal pressure (IAP) was measured every 8 h during ICU stay. Data included demographics, main diagnosis on admission, severity scores, cumulative fluid balance, daily mean IAP, resolution of IAH, days of ICU and hospital stay, and mortality.
Results
Eighty-seven patients (57.6%) had ≥2 CRF for IAH, 59 (67.8%) out of whom developed IAH. Patients with ≥2 CRF had a significantly higher mortality rate (41.4 vs. 14.3%, p < 0.001). Patients with IAH had higher body mass index, severity scores, organ dysfunctions/failures, number of CRF for IAH, days of ICU/hospital stay and hospital mortality rate (45.8 vs. 32.1%, p = 0.22). Non-resolution of IAH was associated with a higher mortality rate (64.7 vs. 35.3%, p = 0.001). None of the cohort patients developed abdominal compartment syndrome. The multivariate analysis showed that IAH development (odds ratio (OR) 4.09; 95% confidence interval (CI) 0.83-20.12) was a non-independent risk factor for mortality, and its non-resolution (OR 13.15; 95% CI 22.13-81.92) was an independent risk factor for mortality.
Conclusions
Critically ill medical patients admitted to ICU with ≥2 CRF have high morbidity, mortality rate, and incidence of IAH, so IAP should be measured and monitored as recommended by the WSACS. Our study highlights the importance of implementing screening and assessment protocols for an early diagnosis of IAH.
Keywords: intra-abdominal hypertension, abdominal compartment syndrome, intra-abdominal pressure, multiple organ failure, critically ill patients, intensive care.
Introduction
Intra-abdominal hypertension (IAH) is associated with adverse outcomes in critically ill patients [1,2]. Elevated intra-abdominal pressure (IAP) above physiologic limits has deleterious effects on end-organ function due to pathophysiologic changes such as a drop in cardiac output, diminished chest wall compliance, decreased renal and visceral blood flow, and increased intracranial pressure [3-11].
IAH has traditionally been associated with patients undergoing abdominal surgery and trauma patients who require aggressive volume resuscitation [12-16]. Several studies have demonstrated that IAH is also frequently present in critically ill nonsurgical patients, and is now considered to be associated with the general process of inflammation and resuscitation [17-22]. However, establishing comparisons for incidence, morbidity and mortality rates in medical patients from data of published clinical trials is difficult, mainly due to three reasons: firstly, the absence of uniform definitions before consensus guidelines, which allow us to reproduce and interpret the results; secondly, the different methods used for IAP measurement; and lastly, the fact that most clinical studies have been performed on mixed populations (both medical and surgical).
The World Society of Abdominal Compartment Syndrome (WSACS) has published a consensus statement including definitions and recommendations for the screening and management of IAH and abdominal compartment syndrome (ACS) [23,24]. Following this consensus, the aim of this study was to determine the incidence of IAH in exclusively critically ill medical patients with high risk of IAH development, and their morbidity and mortality during their intensive care unit (ICU) stay.
Materials and methods
This study was conducted in a university hospital medical ICU in accordance with a protocol that was approved by the local ethics committee. The study fulfilled the requirements of the Declaration of Helsinki, and included an informed consent from the patients on admission (or their family if necessary) to participate and publish the results.
All medical patients admitted to the ICU during a three-month period and expected to stay > 24 h were prospectively enrolled, provided they needed a bladder catheter. Exclusion criteria were ICU stay < 24 h, age < 18 years, pregnancy, contraindication for intravesical pressure measurement (pelvic fracture, hematuria, or neurogenic bladder), and bladder surgery. WSACS consensus for assessment of IAH was implemented as a new protocol [23,24].
Data collection
Demographic data
Age, gender, body mass index (BMI) expressed as kg/m2 [25], main diagnosis on admission, cumulative fluid balance, length of ICU and hospital stay, and hospital mortality were considered in collecting the patients' data. Patients were followed until death or hospital discharge, whatever came first.
Organ dysfunction
On admission, APACHE II (Acute Physiology and Chronic Health Evaluation) and SOFA (Sequential Organ Failure Assessment) scores were recorded using the worst values of the day [26,27]. Organ dysfunction/failure was evaluated using the SOFA score (dysfunction = subscore ≤2, failure = subscore ≥3). The SOFA maximum score was based on the worst value of each organ system during the ICU stay.
Risk factors for IAH
All patients were prospectively screened for risk factors (RF) of IAH on admission and daily during their ICU stay until death or discharge, based on four categories from the WSACS algorithm (Table 1). Those patients who presented any RF of at least two different categories (≥2 categorized risk factors (CRF)), at any time on admission or during the ICU stay, were considered to have a high risk of developing IAH, and IAP was monitored (starting the day they were found to have ≥2 CRF). Those patients with < 2 CRF on admission and daily during the ICU stay were considered to have a low risk of developing IAH according to WSACS recommendations and their IAP measurement was not recorded. For the main analysis, we calculated the number of RF as categories (one minimum, four maximum) on admission (first 24 h) and during the ICU stay (mean RF categories present per day).
Table 1.
Categorized risk factors for intra-abdominal hypertension
| Diminished abdominal wall compliance |
| • Mechanical ventilation |
| • Abdominal surgery with primary fascial or tight closure |
| • Major trauma |
| • Major burns |
| • Prone positioning |
| • Head of bed > 30 degrees |
| • Body mass index ≥ 30 kg/m2 or morbid obesity |
| Increased intra-luminal contents |
| • Gastroparesis (gastric dilation or gastric residual > 500 mL). |
| • Ileus, paralytic or mechanical (abdominal distention or absence of bowel sounds) |
| • Colonic pseudo-obstruction |
| Increased abdominal contents |
| • Hemoperitoneum or pneumoperitoneum |
| • Ascites secondary to liver dysfunction |
| • Ascites secondary to liver dysfunction |
| • Other intra-abdominal injuries (peritonitis, abscess) |
| Capillary leak syndrome or fluid resuscitation |
| • Acidosis (arterial pH < 7.2) |
| • Hypotension (systolic blood pressure < 90 mmHg or mean arterial pressure < 70 mmHg or a systolic blood pressure decrease > 40 mmHg or > 2 standard deviation below normal for age in the absence of other causes of hypotension) |
| • Hypothermia (core temperature < 33°C). |
| • Multiple transfusions (> 10 units of blood) |
| • Coagulopathy (platelets < 55,000/mm3 or prothrombin time < 15 s or partial thromboplastin time > 2 times normal or international standardized ratio > 1.5) |
| • Massive fluid resuscitation (> 5 L of colloid or crystalloid) |
| • Acute pancreatitis |
| • Oliguria (urine output < 500 mL). |
| • Sepsis (American-European Consensus Conference definitions) |
| • Major trauma |
| • Major burns |
| • Damage control laparotomy |
IAP measurement
IAP was measured intravesically using a closed-system Foley bladder catheter according to the modified Kron technique [28,29] with an instillation volume of 25 ml of saline. Abdominal perfusion pressure (APP) was calculated as mean arterial pressure minus IAP [30,31]. Measurements of IAP and APP were recorded every 8 h in patients with ≥2 CRF until resolution of IAH (in case it developed), death, or discharge from the ICU. IAH was defined as a repeated (at least three consecutive values separated by 8 h) elevation of IAPmin (the lowest value of each of the three IAP measures) ≥12 mmHg [23]. For the main analysis, IAPmean and APPmean (mean of the three daily values) were calculated per day.
IAH characteristics
We recorded the day of onset, days of sustained IAH, surgical abdominal decompression, and resolution. Resolution of IAH was defined as a sustained IAPmin < 12 mmHg in all measurements recorded every 8 h for a minimum of 48 h; and non-resolution was defined as a sustained IAPmin ≥ 12 mmHg in all measurements until death or discharge from the ICU. IAH was classified according to the time of onset (on admission or during ICU stay) and the development of symptoms (acute, over a period of hours; subacute, over a period of days; or chronic, over a period of months/years). We also recorded the grade of maximal IAP reached during the ICU stay (I, 12-15; II, 16-20; III, 21-25; IV, ≥25 mmHg) [23].
Statistical analysis
Univariate analysis
Continuous non-normally distributed variables were expressed as the median and interquartile range and compared using the nonparametric Mann-Whitney test. Continuous normally distributed variables were expressed as mean ± standard deviation, and compared using the student's t test. Categorical variables were expressed as numbers and percentages and compared using the chi-square test or Fisher exact test. All p values were two-tailed, and p < .05 was considered as statistically significant.
Multivariate analysis
The prognostic relevance of two different parameters was analyzed: variables associated with development of IAH and the prognostic value of IAH and its non-resolution. Backward multiple logistic models were used, including all the variables yielding p < .2 by univariate analysis and those considered clinically relevant. Possible interactions were tested. The results were summarized as odds ratios their respective 95% confidence intervals. The area under the receiver operating characteristic (ROC) curve was used to assess discrimination; an area under the ROC curve of 1.0 denotes perfect discrimination, whereas a value close to 0.50 indicates no apparent accuracy. The Hosmer-Lemeshow goodness-of-fit test was used to evaluate agreement between the observed and expected results across all the probability strata of the outcome of interest (calibration); p > .05 indicates a good fit for the model. Kaplan-Meier curves for survival at 28-day hospital stay were constructed for subgroups with IAH.
Results
Criteria for IAP monitoring and incidence of IAH (Figures 1 and 2)
Figure 1.
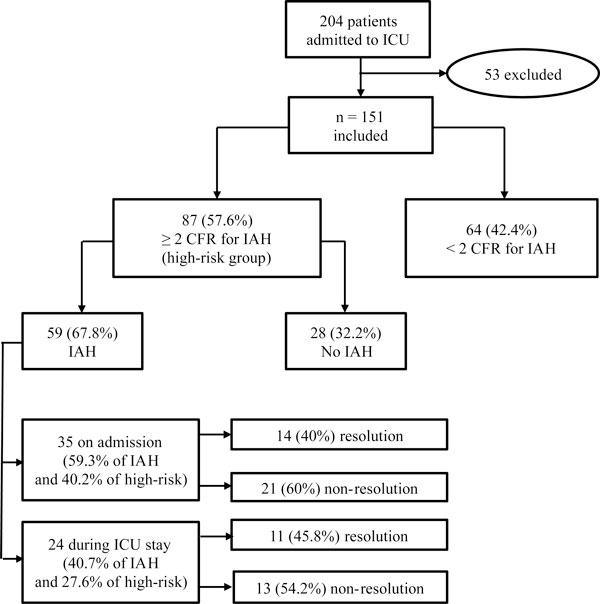
Algorithm and general results of the study cohort. IAH, intra-abdominal hypertension; ICU, intensive care unit; CRF, categorized risk factors.
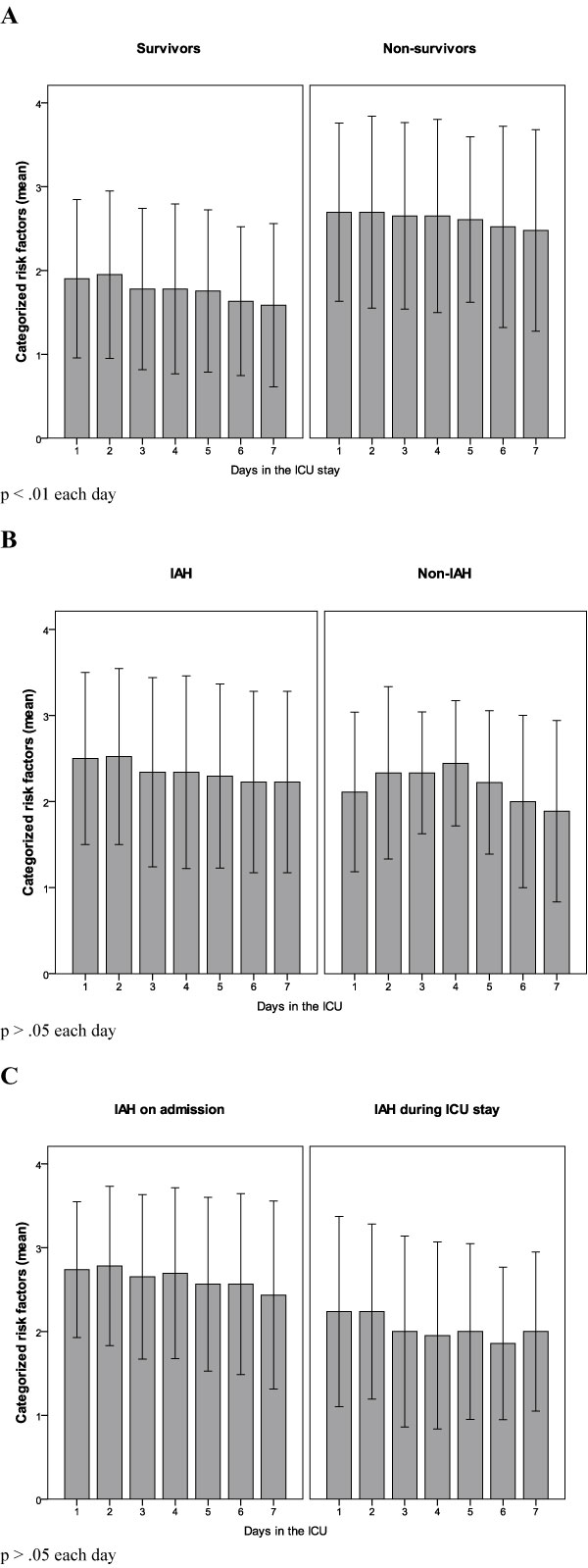
Figure 2.
Differences in the evolution of the number of categorized risk factors during the ICU stay. Differences in the evolution of the number of categorized risk factors during the ICU stay across survivors and non-survivors in the study cohort (A), patients with and without IAH (B), and patients with IAH on admission or during the ICU stay (C). ICU, intensive care unit; IAH, intra-abdominal hypertension.
During the study period, 204 patients were admitted. Fifty-three were excluded: 5 refused to participate, 22 had ICU stay < 24 hours, 12 had contraindications for intravesical pressure measurement or bladder surgery, 11 did not require urinary catheterization, 2 were < 18 years and 1 was pregnant. We finally enrolled 151 medical patients, and the entire protocol was completed in all of them. Main diagnosis on admission was cardiopulmonary disease (Table 2). Sixty-four patients presented < 2 CRF (42.4%) on admission and during all the ICU stay, and IAP was not measured; the remaining 87 (57.6%) patients presented ≥2 CRF (high risk group) for IAH (88.5% on admission and 11.5% during ICU stay), and IAP was monitored following the study protocol. In the high risk group, 59 of the 87 patients developed IAH (67.8%): 35 on admission (59.3%) and 24 during the ICU stay (40.7%). Overall 67.8% of the high risk group subjects developed IAH, 40.2% on admission, and another 27.6% during the ICU stay. Figure 2 shows the differences in the evolution of the number of CRF during the ICU stay across different subgroups of patients. Comparisons between survivors and non-survivors in the study cohort and high risk group are shown in Tables 3 and 4. There were no statistical differences in IAP levels between survivors and non-survivors (11.8 vs. 12.0 mmHg, p = 0.78).
Table 2.
Main diagnosis of the study cohort on admission
| Study cohort (n = 151) | |
|---|---|
| Cardiopulmonary diagnosis | 67 (44.4) |
| Acute/chronic liver failure | 7 (4.6) |
| Acute pancreatitis | 5 (3.3) |
| Gastrointestinal disease | 8 (5.3) |
| Other intra-abdominal processes | 4 (2.6) |
| Acute renal failure | 13 (8.6) |
| Cardiac arrest | 5 (3.3) |
| Neurologic disease | 30 (19.9) |
| Other | 12 (8) |
Values are n (percent).
Table 3.
Categorized risk factors between survivors and non-survivors in the study cohort
| Survivors (n = 109) | Non-survivors (n = 42) | p value | |
|---|---|---|---|
| Number of categorized risk factors | |||
| On admission | 1.5 ± 0.9 | 2.4 ± 1.1 | < .001 |
| During ICU stay | 1.6 ± 1 | 2.8 ± 1.1 | < .001 |
| Risk factors during ICU stay | |||
| (n, percent) | |||
| Diminished abdominal wall compliance | 75 (68.8) | 39 (92.8) | = .002 |
| Increased intraluminal contents | 20 (18.3) | 24 (57.1) | < .001 |
| Increased abdominal contents | 10 (9.2) | 16 (38.1) | < .001 |
| Capillary leak syndrome/fluid resuscitation | 61 (55.9) | 36 (85.7) | = .001 |
ICU, intensive care unit. Data are presented as mean ± standard deviation, unless otherwise indicated.
Table 4.
Categorized risk factors between survivors and non-survivors in the high risk group
| Survivors (n = 51) | Non-survivors (n = 36) | p value | |
|---|---|---|---|
| Number of categorized risk factors | |||
| On admission | 2.2 ± 0.8 | 2.7 ± 0.9 | < .001 |
| During ICU stay | 2.6 ± 0.7 | 3.1 ± 0.8 | < .001 |
| Risk factors during ICU stay (n, percent) | |||
| Diminished abdominal wall compliance | 48 (94.1) | 35 (97.2) | < .001 |
| Increased intraluminal contents | 20 (39.2) | 24 (67.6) | < .001 |
| Increased abdominal contents | 10 (19.6) | 16 (44.4) | < .001 |
| Capillary leak syndrome/fluid resuscitation | 45 (88.2) | 34 (94.4) | < .001 |
Categorized risk factors between survivors and non-survivors in the high risk group (87 patients with ≥2 categorized risk factors). ICU, intensive care unit. Data are presented as mean ± standard deviation, unless otherwise indicated.
General characteristics for the comparison between high risk and low risk groups (Table 5)
Table 5.
General characteristics of the study cohort, and comparisons between patients
| Study cohort | ≥2 categorized risk factors | <2 categorized risk factors | p value | |
|---|---|---|---|---|
| Patients (n, percent) | 151 (100) | 87 (57.6) | 64 (42.4) | - |
| Age (years) | 56.7 ± 17.5 | 55.8 ± 17.2 | 58 ± 17.9 | NS |
| Male gender (n, percent) | 106 (70.2) | 66 (75.9) | 40 (62.5) | NS |
| Body mass index (kilograms per square meter) | 25.9 ± 5.3 | 26.3 ± 5.6 | 25.3 ± 4.9 | NS |
| Acute Physiology and Chronic Health Evaluation score, points | 20.1 ± 8.4 | 22.8 ± 7.9 | 16.5 ± 7.8 | < .001 |
| Sequential Organ Failure Assessment score on day 1, points | 6.4 ± 3.9 | 7.9 ± 3.9 | 4.4 ± 2.7 | < .001 |
| Number of organ failures on day 1, points | 3 ± 1.3 | 3.2 ± 1.3 | 2.2 ± 1.1 | < .001 |
| Sequential Organ Failure Assessment score maximum, points | 8.1 ± 5.2 | 10.5 ± 5.1 | 4.8 ± 3.1 | < .001 |
| Number of organ failures maximum, points | 3 ± 1.5 | 3.8 ± 1.5 | 2.3 ± 1.1 | < .001 |
| Positive cumulative fluid balance during ICU stay | 59 (39.1) | 34 (39) | 25 (39) | NS |
| ICU stay (days)a | 5 (3-12) | 9 (4-25) | 3 (2-4) | < .001 |
| Hospital stay (days)a | 16 (9-37) | 24 (4-55) | 13 (8-21) | = .001 |
| Hospital mortality (n, percent) | 42 (27.8) | 36 (41.4) | 6 (14.3) | < .001 |
| Number of categorized risk factors | ||||
| On admission | 1.7 ± 1.0 | 2.4 ± 0.9 | 0.8 ± 0.4 | < .001 |
| During ICU stay | 2.0 ± 1.1 | 2.8 ± 0.8 | 0.8 ± 0.3 | < .001 |
| Risk factors during ICU stayb (n, percent) | ||||
| Diminished abdominal wall compliance | 114 (75.5) | 83 (95.4) | 31 (48.4) | < .001 |
| Mechanical ventilation | 104 (68.9) | 77 (88.5) | 27 (42.2) | < .001 |
| Head of bed > 30° | 135 (89.4) | 83 (95.4) | 52 (81.3) | = .005 |
| Body mass index ≥30 kg/m2 | 36 (23.8) | 26 (29.9) | 10 (15.6) | = .04 |
| Increased intraluminal contents | 44 (29.1) | 44 (50.6) | 0 (0) | < .001 |
| Gastroparesis | 37 (24.5) | 37 (42.5) | 0 (0) | < .001 |
| Ileus | 21 (13.9) | 21 (24.1) | 0 (0) | < .001 |
| Increased abdominal contents | 26 (17.2) | 26 (29.9) | 0 (0) | < .001 |
| Ascites/liver dysfunction | 14 (9.3) | 14 (16.1) | 0 (0) | = .001 |
| Ascites of other causes | 4 (2.6) | 4 (4.6) | 0 (0) | NS |
| Capillary leak syndrome/fluid resuscitation | 97 (64.2) | 79 (90.8) | 18 (28.1) | < .001 |
| Acidosis | 32 (21.2) | 28 (32.2) | 4 (6.3) | < .001 |
| Hypotension | 68 (45) | 61 (70.1) | 7 (10.9) | < .001 |
| Hypothermia | 7 (4.6) | 7 (8) | 0 (0) | = .01 |
| Multiple transfusions | 3 (2) | 3 (3.4) | 0 (0) | NS |
| Coagulopathy | 48 (31.8) | 40 (46) | 8 (12.5) | < .001 |
| Massive fluid resuscitation | 49 (32.5) | 40 (46) | 9 (14.1) | < .001 |
| Acute pancreatitis | 5 (3.3) | 5 (5.7) | 0 (0) | NS |
| Oliguria | 43 (28.5) | 35 (40.2) | 8 (12.5) | < .001 |
| Sepsis | 68 (45) | 56 (64.4) | 12 (18.8) | < .001 |
General characteristics of the study cohort, and comparisons between patients with ≥2 vs. <2 categorized risk factors for intra-abdominal hypertension. aData are presented as median and interquartile range. bAbdominal surgery with primary fascial or tight closure, major trauma, major burns, prone positioning, colonic pseudo-obstruction, hemoperitoneum or pneumoperitoneum; other intra-abdominal injuries and damage control laparotomy are not included due to the very low number of patients with these risk factors. APACHE II, Acute Physiology and Chronic Health Evaluation; CRF, categorized risk factors; IAH, intra-abdominal hypertension; ICU, intensive care unit; NS, not significant; SOFA, Sequential Organ Failure Assessment. Data are presented as mean ± standard deviation, unless otherwise indicated.
We compared patients with ≥2 CRF (n = 87) with those with < 2 CRF for IAH (n = 64). Severity of illness, ICU and hospital length of stay, and mortality rate (41.4 vs. 14.3%, p < 0.001) were significantly higher in the high risk group.
General characteristics for the comparison between IAH and non-IAH groups (Tables 6 and 7)
Table 6.
General characteristics of the patients with ≥2 categorized risk factors and comparisons between patients
| ≥2 Categorized risk factors | Intra-abdominal hypertension | No intra-abdominal hypertension | p value | |
|---|---|---|---|---|
| Patients (n, percent) | 87 (100) | 59 (67.8) | 28 (32.2) | |
| Age (years) | 55.8 ± 17.2 | 59.3 ± 16.4 | 48.5 ± 16.6 | .006 |
| Male gender (n, percent) | 66 (75.9) | 44 (74.6) | 22 (78.6) | NS |
| Body mass index (kilograms per square meter) | 26.3 ± 5.6 | 27.7 ± 5.6 | 23.4 ± 4.2 | < .001 |
| APACHE II score, points | 22.8 ± 7.9 | 24.4 ± 7.8 | 19.5 ± 7.2 | .007 |
| SOFA score on day 1, points | 7.9 ± 3.9 | 8.8 ± 4.0 | 6.2 ± 3.3 | .004 |
| Number of organ failures on day 1, points | 3.2 ± 1.3 | 3.5 ± 1.3 | 2.5 ± 1.2 | .002 |
| SOFA score maximum, points | 10.5 ± 5.1 | 11.7 ± 4.7 | 7.9 ± 4.9 | .001 |
| Number of organ failures maximum, points | 3.8 ± 1.5 | 4.2 ± 1.4 | 3.0 ± 1.4 | < .001 |
| Positive cumulative fluid balance during ICU stay | 34 (39) | 25 (42.4) | 9 (32.1) | NS |
| ICU stay (days)a | 9 (4-25) | 11 (7-29) | 4 (3-9) | < .001 |
| Hospital stay (days)a | 24 (4-55) | 29 (13-61) | 15 (6-34) | .005 |
| Hospital mortality (n, percent) | 36 (41.4) | 27 (45.8) | 9 (32.1) | NS |
| Number of categorized risk factors | ||||
| On admission | 2.4 ± 0.9 | 2.5 ± 0.9 | 2.1 ± 0.8 | .05 |
| During ICU stay | 2.8 ± 0.8 | 2.9 ± 0.8 | 2.4 ± 0.6 | .006 |
| Risk factors during ICU stayb (n, percent) | ||||
| Diminished abdominal wall compliance | 83 (95.4) | 57 (96.6) | 26 (92.9) | NS |
| Mechanical ventilation | 77 (88.5) | 51 (86.4) | 26 (92.9) | NS |
| Head of bed > 30° | 83 (95.4) | 57 (96.6) | 26 (92.9) | NS |
| Body mass index ≥30 kg/m2 | 26 (29.9) | 24 (40.7) | 2 (7.1) | .001 |
| Increased intraluminal contents | 44 (50.6) | 33 (55.9) | 11 (39.3) | NS |
| Gastroparesis | 37 (42.5) | 28 (47.5) | 9 (32.1) | NS |
| Ileus | 21 (24.1) | 16 (27.1) | 5 (17.9) | NS |
| Increased abdominal contents | 26 (29.9) | 23 (39) | 3 (10.7) | .007 |
| Ascites/liver dysfunction | 14 (16.1) | 12 (20.3) | 2 (7.1) | NS |
| Ascites of other causes | 4 (4.6) | 4 (6.8) | 0 (0) | NS |
| Capillary leak syndrome/fluid resuscitation | 79 (90.8) | 55 (93.2) | 24 (85.7) | NS |
| Acidosis | 28 (32.2) | 22 (37.3) | 6 (21.4) | NS |
| Hypotension | 61 (70.1) | 46 (78) | 15 (53.6) | .02 |
| Hypothermia | 7 (8) | 5 (8.5) | 2 (7.1) | NS |
| Multiple transfusions | 3 (3.4) | 2 (3.4) | 1 (3.6) | NS |
| Coagulopathy | 40 (45.9) | 30 (50.8) | 10 (35.7) | NS |
| Massive fluid resuscitation | 40 (46) | 30 (50.8) | 10 (35.7) | NS |
| Acute pancreatitis | 5 (5.7) | 5 (8.5) | 0 (0) | .005 |
| Oliguria | 35 (40.2) | 27 (45.8) | 8 (28.6) | NS |
| Sepsis | 56 (64.4) | 40 (67.8) | 16 (57.1) | NS |
| IAP during ICU stay | 12 ± 3 | 13 ± 1 | 8 ± 1 | < .001 |
| APP mean during ICU stay | 74 ± 13 | 73 ± 12 | 74 ± 15 | NS |
General characteristics of the patients with ≥2 categorized risk factors, and comparisons between patients with and without intra-abdominal hypertension. aData are presented as median and interquartile range. bAbdominal surgery with primary fascial or tight closure, major trauma, major burns, prone positioning, colonic pseudo-obstruction, hemoperitoneum or pneumoperitoneum; other intra-abdominal injuries and damage control laparotomy are not included due to the very low number of patients with these risk factors. APACHE II, APP, abdominal perfusion pressure; Acute Physiology and Chronic Health Evaluation; CRF, categorized risk factors; IAH, intra-abdominal hypertension; IAP, intra-abdominal pressure (mmHg); ICU, intensive care unit; NS, not significant; SOFA, Sequential Organ Failure Assessment. Data are presented as mean ± standard deviation, unless otherwise indicated.
Table 7.
Comparison of organ failure according to SOFA score between IAH and non-IAH patients
| Intra-abdominal hypertension(n = 59) | No intra-abdominal hypertension (n = 28) | p value | |
|---|---|---|---|
| Organ failures on day 1 | |||
| Respiratory | 56 (94.9) | 27 (96.5) | NS |
| Circulatory | 43 (72.8) | 11 (39.2) | < .003 |
| Renal | 32 (54.2) | 4 (14.6) | < .001 |
| Hepatic | 21 (35.6) | 6 (21.4) | NS |
| Neurological | 28 (47.5) | 16 (67.1) | NS |
| Coagulation | 28 (47.5) | 7 (25) | = .04 |
| Organ failures during ICU stay | |||
| Respiratory | 58 (98.4) | 26 (92.8%) | NS |
| Circulatory | 47 (79.7) | 16 (57.1%) | = .02 |
| Renal | 38 (64.4) | 6 (21.5%) | < .001 |
| Hepatic | 32 (54.3) | 8 (28.5%) | = .02 |
| Neurologic | 37 (62.7) | 18 (6.3%) | NS |
| Coagulation | 37 (62.7) | 11 (3.3%) | = .04 |
Comparison of organ failure according to SOFA score (Sequential Organ Failure Assessment Score) between IAH and non-IAH patients on admission and during the entire ICU stay. IAH, intra-abdominal hypertension; ICU, intensive care unit; NS, not significant. Values are n (percent).
We compared patients who developed IAH with ≥2 CRF (n = 59) with those who did not despite having ≥2 CRF (n = 28). Mortality rate was higher in patients with IAH, although this did not reach statistical (45.8 vs. 32.1%, p < 0.22) significance. Patients with IAH were older, had a higher BMI, higher severity scores and proportion of organ failure, and had a longer ICU and hospital stay. Increased abdominal content (39 vs. 10.7%, p = 0.007) and IAPmean (13 + 1 vs. 8 + 1 mmHg, p < 0.001) were also significantly higher.
General characteristics of patients with IAH (Table 8, Figure 3)
Table 8.
Characteristics of patients with intra-abdominal hypertension and comparisons between survivors and non-survivors
| Intra-abdominal hypertension | Survivors | Non-survivors | p value | |
|---|---|---|---|---|
| Patients (n, percent) | 59 (100) | 32 (54.2) | 27 (45.8) | - |
| Age (years) | 59.3 ± 16.4 | 55.7 ± 16.6 | 63.5 ± 15.5 | NS |
| Male gender (n, percent) | 44 (74.6) | 23 (71.8%) | 21 (77.8) | NS |
| Body mass index (kilogram per square meter) | 27.7 ± 5.6 | 27.8 ± 6.8 | 27.6 ± 3.9 | NS |
| APACHE II score, points | 24.4 ± 7.8 | 22.5 ± 8.8 | 26.6 ± 5.7 | .03 |
| SOFA score on day 1, points | 8.8 ± 4 | 7.5 ± 3.7 | 10.2 ± 3.9 | .009 |
| Number of organ failures on day 1, points | 1.7 ± 1.1 | 1.3 ± 1 | 2.2 ± 0.9 | < .001 |
| SOFA score maximum, points | 11.7 ± 4.7 | 10.2 ± 4.2 | 13.5 ± 4.8 | .006 |
| Number of organ failures maximum | 2.6 ± 1.3 | 2.3 ± 1.2 | 3.1 ± 1.3 | .02 |
| Number of categorized risk factors | 2.5 ± 0.9 | 2.3 ± 0.8 | 2.8 ± 0.9 | 03 |
| At admission | 2.9 ± 0.8 | 2.7 ± 0.8 | 3.3 ± 0.7 | .003 |
| During ICU stay | 5 (8.5) | 3 (9.4) | 2 (7.4) | - |
| Classification of IAH according to | ||||
| Presentation or development of symptoms (n, percent) | ||||
| Acute | 51 (86.4) | 26 (81.2) | 25 (92.6) | - |
| Subacute | 3 (5.1) | 3 (9.4) | 0 (0) | NS |
| Chronic | 6 (10.2) | 3 (9.4) | 3 (11.1) | NS |
| Grade of IAP reached during ICU | ||||
| stay (n, percent) | ||||
| I (12-15 mmHg) | 34 (57.6) | 19 (59.4) | 15 (55.5) | NS |
| II (16-20 mmHg) | 14 (23.7) | 8 (25) | 6 (22.2) | NS |
| III (21-25 mmHg) | 5 (8.5) | 2 (6.2) | 3 (11.1) | NS |
| IV (> 25 mmHg) | 13 ± 1 | 14 ± 2 | 13 ± 1 | NS |
| IAP mean during ICU stay | 73 ± 12 | 74 ± 12 | 71 ± 12 | .001 |
| APP mean during ICU stay | 35 (59.3) | 21 (65.6) | 14 (51.8) | NS |
| Time of IAH development (n, percent) | ||||
| On admission | 24 (40.7) | 11 (34.4) | 13 (48.1) | NS |
| During ICU stay | 1 (1-3) | 1 (1-3) | 1 (1-4) | NS |
| Day of IAH development during ICU staya | 8 (4-16) | 7 (4-16) | 9 (6-16) | NS |
| Days with maintained IAH during ICU staya | 34 (57.6) | 12 (37.5) | 22 (81.5) | |
| Non-resolved IAH (n, percent) | ||||
| Positive cumulative fluid balance at IAH diagnosis | 49 (83) | 27 (84.4) | 22 (81.5) | |
| Positive cumulative fluid balance during ICU stay | 25 (42.4) | 10 (31.2) | 15 (55.5) | |
| ICU stay (days)a | 1 (7-29) | 12 (7-26) | 12 (6-33) | |
| Hospital stay after ICU (days)a | 29 (13-61) | 34 (23-58) | 16 (8-65) |
aData are presented as median and interquartile range. APACHE II, Acute Physiology and Chronic Health Evaluation; APP, abdominal perfusion pressure; IAH, intra-abdominal hypertension; IAP, intra-abdominal pressure (mmHg); ICU, intensive care unit; NS, not significant; SOFA, Sequential Organ Failure Assessment. Data are presented as mean ± standard deviation, unless specified.
Figure 3.
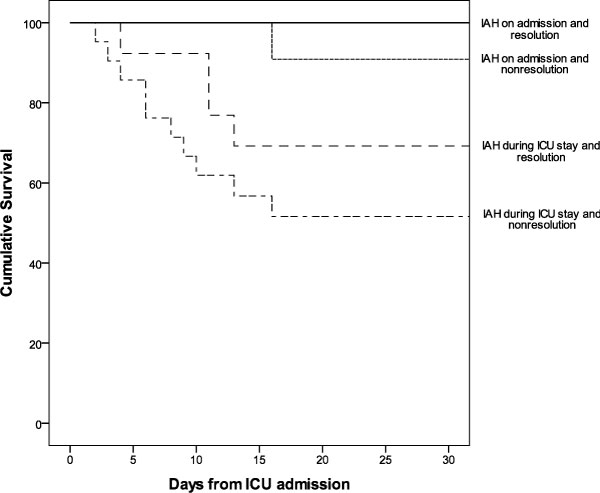
Kaplan-Meier cumulative survival curve for different subgroups of patients with IAH. Kaplan-Meier cumulative survival curve for different subgroups of patients with IAH: IAH on admission or during the ICU stay depending on resolution or non-resolution of IAH. IAH, intra-abdominal hypertension; ICU, intensive care unit.
Non-survivors had significantly higher severity scores, number of organ failures, and CRF for IAH, both on admission and during the ICU stay. The more commonly found subtypes of IAH were subacute (51 patients, 86.4%) and grade II (34 patients, 57.6%). IAH was resolved in a high proportion of patients (42.4%) and none presented ACS or required surgical abdominal decompression. Patients in whom IAH was not resolved (57.6%) had a significantly higher mortality rate than patients whose condition was resolved (64.7 vs. 35.2%, p = 0.001). Kaplan-Meier survival analysis for patients with IAH on admission or during the ICU stay depending on resolution is shown in Figure 3.
Multivariate analysis: predictive and prognostic models (Tables 9, 10 and 11)
Table 9.
Logistic regression model for predictors of development of IAH in the high risk group
| Coefficients | Odds ratio | 95% confidence interval | p value | |
|---|---|---|---|---|
| Age ≥65 years | 0.780 | 2.18 | 0.66-7.15 | .19 |
| Body mass index ≥30, kg/m2 | 2.312 | 10.09 | 1.97-51.58 | .005 |
| SOFA score at admission | 0.153 | 1.16 | 1.00-1.35 | .04 |
| Number of categorized risk factors for IAH during ICU stay | 0.840 | 2.31 | 1.09-4.88 | .02 |
| Constant | -3.408 |
Predictors of development of IAH in the group with ≥2 categorized risk factors for IAH (87 patients). CI, confidence interval; SOFA, Sequential Organ Failure Assessment; IAH, intra-abdominal hypertension; ICU, intensive care unit. Area under receiver operating characteristic curve = 0.80; Hosmer-Lemeshow goodness-of-fit (x2 = 4.22; p = 0.835).
Table 10.
Logistic regression model for predictors of mortality in the high risk group
| Coefficients | Odds ratio | 95% Confidence interval | p value | |
|---|---|---|---|---|
| Age ≥65 yrs | 2.057 | 3.82 | 2.08-29.28 | .002 |
| APACHE II score ≥20 | 1.614 | 5.02 | 1.11-22.70 | .03 |
| SOFA score maximum during ICU stay | 0.224 | 1.25 | 1.03-1.51 | .01 |
| Positive cumulative fluid balance during ICU stay | 1.730 | 5.64 | 1.50-21.14 | .06 |
| No. of categorized risk factors for IAH during ICU stay | 1.200 | 3.32 | 0.94-11.72 | .34 |
| Increased abdominal content during ICU stay | 1.007 | 2.73 | 0.34-21.78 | .08 |
| IAH | 1.409 | 4.09 | 0.83-20.12 | |
| Constant | -9.908 |
Predictors of mortality in the group with ≥2 categorized risk factors for IAH (87 patients). APACHE II, Acute Physiology and Chronic Health Evaluation; CI, confidence interval; IAH, intra-abdominal hypertension; ICU, intensive care unit; SOFA, Sequential Organ Failure Assessment. Area under receiver operating characteristic curve = 0.78; Hosmer-Lemeshow goodness-of-fit (x2 = 3.78; p = 0.870).
Table 11.
Logistic regression model for predictors of mortality in the IAH group
| Coefficients | Odds ratio | 95% confidence interval | p value | |
|---|---|---|---|---|
| Age ≥65 yrs | 2.811 | 16.63 | 2.46-112.30 | .004 |
| SOFA score maximum during ICU stay | 0.196 | 1.22 | 0.97-1.53 | .09 |
| No. of categorized risk factors for IAH during ICU stay | 2.297 | 9.94 | 1.59-62.00 | .01 |
| Increased abdominal content during ICU stay | 1.847 | 6.34 | 0.43-93.31 | .17 |
| Non-resolution of IAH | 2.577 | 13.15 | 22.13-81.92 | .006 |
| Constant | -13.953 |
Predictors of mortality in the patients with IAH (59 patients). CI, confidence interval; IAH, intra-abdominal hypertension; ICU, intensive care unit; SOFA, Sequential Organ Failure Assessment. Area under receiver operating characteristic curve = 0.80
Predictive model for IAH development in the high risk group (87 patients with ≥2 CRF)
SOFA on admission, obesity, and number of CRF during ICU stay (odds ratio (OR), 2.31; 95% confidence interval (CI), 1.09 - 4.88) were independent predictors of IAH development.
Predictive model of mortality in the high risk group (87 patients with ≥2 CRF)
IAH development was a non-independent predictor of mortality (OR, 4.09; 95% CI, 0.83 - 20.12).
Predictive model of mortality in the IAH group (59 patients)
Non-resolution of IAH (OR, 13.15; 95% CI, 22.13 - 81.92), number of CRF during ICU stay (OR, 9.94; 95% CI, 1.59-62.00), and age ≥65 years were independent predictors of mortality. Even though the ROC curve showed good discrimination, the Hosmer-Lemeshow test indicated inadequate calibration across all the probability strata for mortality in the model.
Discussion
This is a prospective epidemiologic study performed in a population of exclusive critically ill medical patients following the WSACS guidelines for the assessment of IAH (screening, IAP measurement, definitions, and classification recommendations). Other published studies had been performed in mixed populations (medical and surgical), before the WSACS consensus statement, based on different definitions of IAH or limited by incomplete assessment in terms of screening or classification of the IAH [17-21].
Our study revealed several interesting findings. Firstly, there was a large number of patients with high risk (≥2 CRF) for IAH development, and the incidence of IAH in this group was high; in addition, the mortality in this subgroup was significantly higher as compared with the low risk subgroup. Secondly, there was an association of IAH with illness severity and the number/type of RF reported in the literature. Thirdly, IAH was a predictor of mortality in association with other clinical factors. And finally, non-resolution of IAH was an independent predictive factor of mortality. Our results support the importance of implementing screening and assessment protocols, according to WSACS recommendation, in order to identify a subgroup of high risk patients with high mortality and high incidence of IAH whom should be monitored for IAP.
Screening, risk factors and incidence of IAH
A large number of patients presented ≥2 CRF for IAH development, and the incidence of IAH in this group was high (67.8%) on admission or during the ICU stay. In addition, several high risk patients without IAH might have shown underestimated IAP levels because of the different factors usually present in the critically ill population, such as sedation or gastric/colonic decompression. A high incidence of IAH had also been reported in the literature [17-21]; however, when trying to combine our results with previously described findings, three main methodology issues should be accounted for: a) incidence is recorded on admission or during the first week; b) most reports refer to mixed populations (both medical and surgical); c) definitions of IAH differed across the studies (incidence rates can vary depending on the threshold IAP level used as a diagnostic criterion). Unlike previous studies, our study analyzes the incidence of IAH in a high risk population on admission and throughout the entire ICU stay, following WSACS consensus guidelines, and exclusively in critically ill medical patients. Reintam et al. [17] and Vidal et al. [18] have also used WSACS definitions for IAH, and they report incidence rates of 37% in a mixed population, and 43% in the medical subgroup of a mixed population, respectively.
Numerous conditions predispose to IAH development, and our results are consistent with those from other studies [20,21]. In the high risk group, we found an association between IAH and the CRF proposed by the WSACS, specially the increased abdominal content. Obesity and the number of CRF for IAH during ICU stay were independent predictors of IAH development. Data on fluid balance were only qualitative (positive or negative), and the association between IAH and massive fluid loading in the presence of sepsis and/or capillary leak described in the literature could not be studied.
Severity scores and organ failure in patients with IAH
Increases in IAP have deleterious effects on end-organ system function by compromising perfusion, thus leading to multiorganic dysfunction (MOD) and poor outcome. In our population, IAH was significantly associated with higher severity of illness scores and incidence of organ failure. In addition, the study design allowed us to compare organ impairment during ICU stay between patients with and without IAH (Table 5). Previous studies analyzed organ impairment only during the first days of ICU stay, thus making it difficult to study the association between MOD and IAH throughout the entire ICU stay.
Characteristics of IAH
WSACS gives special attention to the IAH classification; this correlates with the patient's profile, namely, whether the patient is medical or surgical [17-21,32-34]. Classification of IAH as acute and with high IAP grades (III-IV) is typical for surgical patients, whereas classification of IAH as subacute and with low-moderate IAP grades (I-II) is characteristic for medical patients [17-21,35]. Our results in medical patients are consistent with this observation. The IAH classification varies depending on the study; however, no studies include all the classification types currently recommended by WSACS. In summary, a complete classification is important for planning future studies and comparing results, and the differentiation between medical or surgical patients is, in our opinion, necessary for a correct analysis based on the differences with regard to the causes and evolution of IAH in those two types of patient's profile.
Fourteen patients reached grade III of IAH, and five grade IV, but none of them developed ACS because a sustained elevation of IAP > 20 mmHg associated with organ deterioration was not detected. In concordance with this, no patient required surgical abdominal decompression.
Prognostic implications of IAH
Development of IAH has been described as an independent predictor of mortality in mixed populations [20]. In our study IAH was a non-independent predictor of mortality, and this supports the fact that IAH was a marker of mortality in association with other clinical factors. In accordance with this, patients with IAH had higher severity scores and number of CRF for IAH that can independently increase mortality risk. In fact, the number of CRF during ICU stay was an independent predictor of mortality in the group with IAH.
We found a high rate of resolution of IAH in our medical patients, but non-resolution was an independent predictor of mortality, resulting in a considerably high OR (non-resolution meant that death was 13 times more likely). Treatment of IAH was nonsurgical in all cases and none developed ACS, although no conclusions can be drawn in the absence of clinical intervention data. Management guidelines for IAH have been proposed by the WSACS [24] although they are based on studies that analyze therapeutic strategies in isolation and in different patient profiles [36-40].
Limitations of the study
IAP was not measured in all cases (only in those with ≥2 CRF), and patients with < 2 CRF and no IAP recorded might have developed IAH during their ICU stay (e.g., patients with mechanical ventilation and therefore, diminished abdominal wall compliance but with no RF in other categories and no IAP measured). Therefore, the study followed the WSACS screening recommendations but was not designed to validate them in order to identify a subgroup of high risk patients for IAH development, as compared with a low risk subgroup. The study was underpowered to analyze each RF of the four categories as predictors of IAH (small sample size) or the IAP level as a predictor of mortality (the IAPmean in the patients with IAH were relatively low to perform comparisons in the outcome). Not all patients who had their IAP measured were sedated, which could have caused a falsely elevated IAP. Although resolution of IAH was a prognostic factor, our study was not designed to focus on therapeutic management of IAH, and no conclusions can be drawn or ascertainments can be made about the strategies that were effective.
Conclusions
Critically ill medical patients admitted to the ICU with high risk of IAH development (≥2 CRF) have high morbidity, mortality, and incidence of IAH, so IAP should be measured as recommended by the WSACS. In this subgroup of patients, the presence of IAH is associated with mortality as a non-independent risk factor, and non-resolution of this process is an independent predictor of mortality. Our study supports the implementation of protocols based on WSACS guidelines for IAH screening and assessment to allow an early approach to this syndrome. Large, multicenter randomized controlled clinical trials are needed to confirm our results and to further promote the WSACS recommendations regarding IAH screening and management.
Abbreviations
APACHE II: Acute Physiology and Chronic Health Evaluation; APP: abdominal perfusion pressure; BMI: body mass index; CRF: categorized risk factors; IAH: intra-abdominal hypertension; IAP: intra-abdominal pressure; ICU: intensive care unit; MOD: multiple organ dysfunction; RF: risk factors; SOFA: Sequential Organ Failure Assessment; WSACS: World Society of Abdominal Compartment Syndrome.
Consent
Written informed consent was obtained from the patients or their relatives for publication of this case report. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
All authors read and approved the final manuscript. PS conceived the study and participated in its design and coordination. PS and JM performed the statistical analysis. LA and PG participated in analysis and interpretation of data. IM, MZ and MT collected data. All authors contributed to the writing and preparation of the manuscript.
Authors' information
PS, MD, PhD; JM, MD, Associate Professor of Medicine, Universidad Complutense de Madrid (UCM), Spain; MT, RN, Chief of Critical Care Nurse Department; IM, MD; MZ, MD; LA, MD, PhD, Chief of Internal Medicine Department, Professor of Medicine, UCM, Spain; PG, MD.
Contributor Information
Patricia Santa-Teresa, Email: patriciasantateresa@hotmail.com.
Javier Muñoz, Email: jmunoz.hgugm@salud.madrid.org.
Ignacio Montero, Email: juanignaciomonteroroblas@gmail.com.
María Zurita, Email: correomariazurita@yahoo.es.
María Tomey, Email: 914395521@telefonica.net.
Luis Álvarez-Sala, Email: lalvarezsalaw@medynet.com.
Pablo García, Email: pitiusas@terra.es.
Acknowledgements
This article has been published as part of Annals of Intensive Care Volume 2 Supplement 1, 2012: Diagnosis and management of intra-abdominal hypertension and abdominal compartment syndrome. The full contents of the supplement are available online at http://www.annalsofintensivecare.com/supplements/2/S1
We are indebted to the study coordinators, clinical research associates, and intensive care residents. We are especially grateful to all the nurses and nursing assistants in our ICU for IAP measurements. We are indebted to the Fundación para la Investigación Biomédica del Hospital Gregorio Marañón, especially Mr Thomas O'Boyle and Dr Jose María de Miguel, for advice in the preparation of this manuscript, and to the faculty members of the WSACS for raising concern about intra-abdominal hypertension in intensive care patients.
References
- Balogh Z, McKinley BA, Cox CS Jr, Allen SJ, Cocanour CS, Kozar RA, Moore EE, Miller CC III, Weisbrodt NW, Moore FA. Abdominal compartment syndrome: the cause of effect of postinjury multiple organ failure. Shock. 2003;20(6):483–492. doi: 10.1097/01.shk.0000093346.68755.43. [DOI] [PubMed] [Google Scholar]
- Balogh Z, McKinley BA, Holcomb JB, Miller CC, Cocanour CS, Kozar RA, Valdivia A, Ware DN, Moore FA. Both primary and secondary abdominal compartment syndrome can be predicted early and are harbingers of multiple organ failure. J Trauma. 2003;54(5):848–859. doi: 10.1097/01.TA.0000070166.29649.F3. [DOI] [PubMed] [Google Scholar]
- Cullen DJ, Coyle JP, Teplick R, Long MC. Cardiovascular, pulmonary, and renal effects of massively increased intra-abdominal pressure in critically ill patients. Crit Care Med. 1989;17(2):118–121. doi: 10.1097/00003246-198902000-00002. [DOI] [PubMed] [Google Scholar]
- Kashtan J, Green JF, Parsons EQ, Holcroft JW. Hemodynamic effects of increased abdominal pressure. J Surg Res. 1981;30(3):249–255. doi: 10.1016/0022-4804(81)90156-6. [DOI] [PubMed] [Google Scholar]
- Barnes GE, Laine GA, Giam PY, Smith EE, Granger HJ. Cardiovascular responses to elevation of intra-abdominal pressure. Am J Physiol. 1985;248(2 Pt 2):R208–13. doi: 10.1152/ajpregu.1985.248.2.R208. [DOI] [PubMed] [Google Scholar]
- Obeid F, Saba A, Fath J, Guslits B, Chung R, Sorensen V, Buck J, Horst M. Increases in intra-abdominal pressure affect pulmonary compliance. Arch Surg. 1995;130(5):544–547. doi: 10.1001/archsurg.1995.01430050094016. [DOI] [PubMed] [Google Scholar]
- Doty JM, Saggi BH, Blocher CR, Fakhry I, Gehr T, Sica D, Sugerman HJ. Effects of increased renal parenchymal pressure on renal function. J Trauma. 2000;48(5):874–877. doi: 10.1097/00005373-200005000-00010. [DOI] [PubMed] [Google Scholar]
- Sugrue M, Balogh Z, Malbrain M. Intra-abdominal hypertension and renal failure. ANZ J Surg. 2004;74(1-2):78. doi: 10.1046/j.1445-1433.2003.02896.x. [DOI] [PubMed] [Google Scholar]
- Diebel LN, Wilson RF, Dulchavsky SA, Saxe J. Effect of increased intra-abdominal pressure on hepatic arterial, portal venous and hepatic microcirculatory blood flow. J Trauma. 1992;33(2):279–282. doi: 10.1097/00005373-199208000-00019. [DOI] [PubMed] [Google Scholar]
- Bloomfield GL, Ridings PC, Blocher CR, Marmarou A, Sugerman HJ. A proposed relationship between increased intra-abdominal, intrathoracic, and intracranial pressure. Crit Care Med. 1997;25(3):496–503. doi: 10.1097/00003246-199703000-00020. [DOI] [PubMed] [Google Scholar]
- Citerio G, Vascotto E, Villa F, Celotti S, Pesenti A. Induced abdominal compartment syndrome increases intracranial pressure in neurotrauma patients: a prospective study. Crit Care Med. 2001;29(7):1466–1471. doi: 10.1097/00003246-200107000-00027. [DOI] [PubMed] [Google Scholar]
- Raeburn CD, Moore EE, Biffl WL, Johnson JL, Meldrum DR, Offner PJ, Franciose RJ, Burch JM. The abdominal compartment syndrome is a morbid complication of postinjury damage control surgery. Am J Surg. 2001;182(6):542–546. doi: 10.1016/s0002-9610(01)00821-2. [DOI] [PubMed] [Google Scholar]
- Mcnelis J, Soffer S, Marini CP, Jurkiewicz A, Ritter G, Simms HH, Nathan I. Abdominal compartment syndrome in the surgical intensive care unit. Am Surg. 2002;68(1):18–23. [PubMed] [Google Scholar]
- Maxwell RA, Fabian TC, Croce MA, Davis KA. Secondary abdominal compartment syndrome: an underappreciated manifestation of severe hemorrhagic shock. J Trauma. 1999;47(6):995–999. doi: 10.1097/00005373-199912000-00001. [DOI] [PubMed] [Google Scholar]
- Mayberry JC, Welker KJ, Goldman RK, Mullins RJ. Mechanism of acute ascites formation after trauma resuscitation. Arch Surg. 2003;138(7):773–776. doi: 10.1001/archsurg.138.7.773. [DOI] [PubMed] [Google Scholar]
- Balogh Z, McKinley BA, Cocanour CS, Kozar RA, Valdivia A, Sailors RM, Moore FA. Supranormal trauma resuscitation causes more cases of abdominal compartment syndrome. Arch Surg. 2003;138(6):637–642. doi: 10.1001/archsurg.138.6.637. [DOI] [PubMed] [Google Scholar]
- Reintman A, Parm P, Kitus R, Kern H, Starkopf J. Primary and secondary intra-abdominal hypertension-different impact on ICU outcome. Crit Care Med. 2008;34(9):1624–1631. doi: 10.1007/s00134-008-1134-4. [DOI] [PubMed] [Google Scholar]
- Vidal MG, Ruiz Weisser J, Gonzalez F, Toro MA, Loudet C, Balasini C, Canales H, Reina R, Estenssoro E. Incidence and clinical effects of intra-abdominal hypertension in critically ill patients. Crit Care Med. 2008;36(6):1823–1831. doi: 10.1097/CCM.0b013e31817c7a4d. [DOI] [PubMed] [Google Scholar]
- Lonardo M, Piazza O, Marco G, De Robertis E, Servillo G, Tufano R. Intra-abdominal hypertension is not reliable as an early predictor of mortality in the intensive care unit. Minerva Anestesiol. 2007;73(9):447–450. [PubMed] [Google Scholar]
- Malbrain ML, Chiumello D, Pelosi P, Bihari D, Innes R, Ranieri VM, Del Turco M, Wilmer A, Brienza N, Malcangi V, Cohen J, Japiassu A, De Keulenaer BL, Daelemans R, Jacquet L, Laterre PF, Frank G, de Souza P, Cesana B, Gattinoni L. Incidence and prognosis of intraabdominal hypertension in a mixed population of critically ill patients: a multiple-center epidemiological study. Crit Care Med. 2005;33(2):315–322. doi: 10.1097/01.ccm.0000153408.09806.1b. [DOI] [PubMed] [Google Scholar]
- Malbrain ML, Chiumello D, Pelosi P, Wilmer A, Brienza N, Malcangi V, Bihari D, Innes R, Cohen J, Singer P, Japiassu A, Kurtop E, De Keulenaer BL, Daelemans R, Del Turco M, Cosimini P, Ranieri M, Jacquet L, Laterre PF, Gattinoni L. Prevalence of intra-abdominal hypertension in critically ill patients: a multicentre epidemiological study. Intensive Care Med. 2004;30(5):822–829. doi: 10.1007/s00134-004-2169-9. [DOI] [PubMed] [Google Scholar]
- Malbrain ML, De Laet I. AIDS is coming to your ICU: be prepared for acute bowel injury and acute intestinal distress syndrome. Intensive Care Med. 2008;34(9):1565–1569. doi: 10.1007/s00134-008-1135-3. [DOI] [PubMed] [Google Scholar]
- Malbrain ML, Cheatham ML, Kirkpatrick A, Sugrue M, Parr M, De Waele J, Balogh Z, Leppäniemi A, Olvera C, Ivatury R, D'Amours S, Wendon J, Hillman K, Johansson K, Kolkman K, Wilmer A. Results from the International Conference of Experts on Intra-abdominal Hypertension and Abdominal Compartment Syndrome. I. Definitions. Intensive Care Med. 2006;32(11):1722–1732. doi: 10.1007/s00134-006-0349-5. [DOI] [PubMed] [Google Scholar]
- Cheatham ML, Malbrain ML, Kirkpatrick A, Sugrue M, Parr M, De Waele J, Balogh Z, Leppäniemi A, Olvera C, Ivatury R, D'Amours S, Wendon J, Hillman K, Wilmer A. Results from the international Conference of Experts on Intra-abdominal Hypertension and Abdominal Compartment Syndrome. II. Recommendations. Intensive Care Med. 2007;33(6):951–962. doi: 10.1007/s00134-007-0592-4. [DOI] [PubMed] [Google Scholar]
- Garrow JS. Quetelet index as indicator of obesity. Lancet. 1986;24;1(8491):1219. doi: 10.1016/s0140-6736(86)91207-9. [DOI] [PubMed] [Google Scholar]
- Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: A severity of disease classification system. Crit Care Med. 1985;13(10):818–829. [PubMed] [Google Scholar]
- Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–710. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- Cheatham ML, Safcsak K. Intraabdominal pressure: A revised method for measurement. J Am Coll Surg. 1998;186(5):594–595. doi: 10.1016/s1072-7515(98)00122-7. [DOI] [PubMed] [Google Scholar]
- Malbrain ML. Different techniques to measure intra-abdominal pressure (IAP): Time for a critical reappraisal. Intensive Care Med. 2004;30(3):357–371. doi: 10.1007/s00134-003-2107-2. [DOI] [PubMed] [Google Scholar]
- Cheatham ML, Vhite MW, Sagraves SG, Johnson JL, Block EF. Abdominal perfusion pressure: A superior parameter in the assessment of intra-abdominal hypertension. J Trauma. 2000;49(4):621–627. doi: 10.1097/00005373-200010000-00008. [DOI] [PubMed] [Google Scholar]
- Malbrain ML. In: Yearbook of Intensive Care and Emergency Medicine. Vincent JL, editor. Springer, Berlin Heidelberg New York; 2002. Abdominal perfusion pressure as prognostic marker in intra-abdominal hypertension; pp. 792–814. [Google Scholar]
- Sugrue M, Buist MD, Hourihan F, Deane S, Bauman A, Hillman K. Prospective study of intra-abdominal hypertension and renal function after laparotomy. Br J Surg. 1995;82(2):235–238. doi: 10.1002/bjs.1800820234. [DOI] [PubMed] [Google Scholar]
- Ivatury RR, Porter JM, Simon RJ, Islam S, John R, Stahl WM. Intra-abdominal hypertension after life-threatening penetrating abdominal trauma: prophylaxis, incidence, and clinical relevance to gastric mucosal pH and abdominal compartment syndrome. J Trauma. 1998;44(6):1016–1021. doi: 10.1097/00005373-199806000-00014. [DOI] [PubMed] [Google Scholar]
- De Waele JJ, Hoste EA, Malbrain M. Decompressive laparotomy for abdominal compartment syndrome - a critical analysis. Crit Care Med. 2006;10(2):R51. doi: 10.1186/cc4870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malbrain ML. Abdominal pressure in the critically ill: measurement and clinical relevance. Intensive Care Med. 1999;25(12):1453–1458. doi: 10.1007/s001340051098. [DOI] [PubMed] [Google Scholar]
- Balogh Z, Moore FA, Goettler CE, Rotondo MF, Schwab CW, Kaplan MJ. In: Abdominal compartment syndrome. Ivatury RR, Cheatham ML, Malbrain MLNG, Sugrue M, editor. Landes Biomedical: Georgetown; 2006. Surgical management of abdominal compartment syndrome; pp. 266–296. [Google Scholar]
- De Waele J, Delaet I, Hoste E. The effect of neuromuscular blockers on intraabdominal pressure. Abstracts of the 36th Critical Care Congress, Orlando, Florida, USA, February 17-21, 2007. Crit Care Med. 2006;34(12 Abstr Suppl):A70. [PubMed] [Google Scholar]
- Van der Spoel JI, Oudemans-van Straaten HM, Stoutenbeek CP, Bosman RJ, Zandstra DF. Neostigmine resolves critical illness-related colonic ileus in intensive care patients with multiple organ failure. A prospective, double-blind, placebo-controlled trial. Intensive Care Med. 2001;27(5):822–827. doi: 10.1007/s001340100926. [DOI] [PubMed] [Google Scholar]
- Reckard JM, Chung MH, Varma MK, Zagorski SM. Management of intraabdominal hypertension by percutaneous catheter drainage. J Vasc Interv Radiol. 2005;16(7):1019–1021. doi: 10.1097/01.RVI.0000157781.67279.72. [DOI] [PubMed] [Google Scholar]
- Parra MW, Al-Khayat H, Smith HG, Cheatham ML. Paracentesis for resuscitation-induced abdominal compartment syndrome: an alternative to decompressive laparotomy in the burn patient. J Trauma. 2006;60(5):1119–1121. doi: 10.1097/01.ta.0000217274.48792.4d. [DOI] [PubMed] [Google Scholar]