Abstract
Objective
Anxiety disorders are the most prevalent psychiatric disorders in the United States and result in substantial burden to the individual and society. While effective treatments for anxiety disorders have been developed, there has been substantially less focus on interventions aimed at the amelioration of anxiety related risk and maintenance factors. Anxiety sensitivity (AS) is a well-established, malleable risk and maintenance factor for panic disorder and other psychopathology. The aim of the current investigation was to enhance the efficacy of AS treatment through the refinement of a previously validated intervention.
Method
This one-session intervention utilized psychoeducation and interoceptive exposure to target AS and was compared to a health-focused control intervention among a non-treatment seeking sample (N = 104) of individuals with elevated AS.
Results
Study findings indicate that the active treatment group demonstrated significantly greater reductions in AS at posttreatment and across the one month study period than the control group. These treatment gains were seen across the ASI subscales. A month six follow-up assessment indicated that the treatment group retained the majority of their AS reduction while the control group retained their elevated AS scores. Participants meeting Axis I diagnostic criteria did not report a differential response to the intervention than those without a current diagnosis.
Conclusions
Despite the brevity of the treatment intervention, findings demonstrate that it resulted in substantial reductions in AS that were largely maintained six months post treatment. Anxiety treatment and prevention implications are discussed.
Keywords: Anxiety, Anxiety Sensitivity, Interoceptive Exposure, Treatment
Anxiety disorders are a highly prevalent and disabling form of psychopathology (Greenberg, et al., 1999; Kessler, et al., 2005). While there are many well-established cognitive behavioral treatments for anxiety (Chambless & Ollendick, 2001); research focused on the amelioration of anxiety risk and maintenance factors remains in a nascent stage (Feldner, Zvolensky, & Schmidt, 2004).
Research has consistently linked anxiety sensitivity (AS), a fear of anxiety-related symptoms, to the development and maintenance of anxiety problems. Individuals with preexisting anxiety and mood disorders report higher levels of AS than the general population (Olatunji & Wolitzky-Taylor, 2009). Prospective studies indicate that elevated AS predicts future occurrences of anxiety symptoms, panic attacks and anxiety disorders (Schmidt, Lerew, & Jackson, 1997; Schmidt, Zvolensky, & Maner, 2006). Within treatment investigations, AS has been shown to mediate symptom reduction in panic (Olatunji & Wolitzky-Taylor, 2009) and predict symptom reduction in PTSD (Fedoroff, Taylor, Asmundson, & Koch, 2000). A review of the relationship between AS and pain indicates that AS is associated with a number of pain-related outcomes including disability (Ocanez, McHugh, & Otto, 2010). Among daily smokers, AS predicts a decrease in perceived health and impairments in mental health and social functioning (McLeish, Zvolensky, Smits, Bonn-Miller, & Gregor, 2007).
To reduce the public health burden associated with anxiety psychopathology, several studies have focused specifically on the amelioration of AS. Gardenswartz and Craske (2001) compared a 1-day CBT-based workshop to a waitlist. Group differences were not reported in the reduction of AS but those in the workshop were less likely to develop panic disorder during follow-up. Schmidt et al. (2007) compared ASAT (Anxiety Sensitivity Amelioration Training) to a health and nutrition based control condition. The ASAT condition produced a significantly larger reduction in AS than the control condition (30% vs. 17%, respectively). While the two-year follow-up was limited by sample attrition, findings demonstrated that those in the ASAT condition had a lower incidence of Axis I diagnoses. Broman-Fulks and Storey (2008) evaluated the effect of an exercise regimen on AS amelioration. Those in the exercise condition reported a significant decrease in AS (38%), whereas the control group showed no reduction (4% increase). Feldner and colleagues’ (2008) investigation targeted AS and smoking. The AS-smoking group experienced a greater AS reduction than the control group (34% vs. 22% respectively).
Interoceptive exposure (IE) is thought to be an essential component of AS reduction and involves repeated exposure to feared bodily sensations with the aim of habituating to the fear of those sensations (Schmidt & Trakowski, 2004). While each of the previously mentioned AS amelioration investigations incorporated IE, there were a number of limitations in its utilization. Specifically, IE was not tailored to the participant and while some encouraged home practice, none assessed whether IE was completed independently. Therefore, the potency of IE may not have been fully maximized. Additionally, none of these investigations assessed the effect of current psychiatric status on AS amelioration. It stands to reason that those with an Axis I diagnosis would be less responsive to AS-focused interventions.
The current study extends this literature by focusing on an AS reduction paradigm that has increased potency in reducing this established risk factor. To this end, the current study refined the ASAT intervention and utilized a similar one-treatment session two-condition design among a sample of individuals with elevated AS. The intervention was modified to include in-session practice and homework (HW) of IE exercises tailored to the AS fears of each participant.
It was anticipated that the treatment group would show a greater reduction in AS than the control group and that those gains would be maintained at the six month follow-up. Second, it was expected that current psychopathology would result in a diminished treatment response. Third, we hypothesized that greater HW adherence would result in larger AS reduction among the intervention group.
Method
Participants
Participants were screened through an introductory psychology subject pool. In line with the criteria used by Schmidt et al. (2007), individuals with a score of 1.5 SD above the Anxiety Sensitivity Index (ASI) mean were invited to complete a screening appointment. To ensure the inclusion of only those with elevated scores, participants were reassessed at the screening appointment and randomized if their score remained at or above a 20. Participants were compensated for their time with course credit. If they completed the month six follow-up appointment, they received $10. Pre-intervention sample characteristics are presented in Table 1.
Table 1.
Pre-Intervention Characteristics of the Study Sample.
| ASERT (n = 52) | PHET (n = 52) | Total (N = 104) | |
|---|---|---|---|
| Female (%) | 84.6 | 82.7 | 83.7 |
| Age, M (SD) | 18.98 (1.34) | 18.73 (1.50) | 18.9 (1.42) |
| Race (%) | |||
| Caucasian | 84.6 | 78.8 | 81.7 |
| Black | 7.7 | 9.6 | 8.7 |
| Asian | 3.8 | 5.8 | 4.8 |
| Other | 3.8 | 5.7 | 4.8 |
| Hispanic/Latino | 7.7 | 15.4 | 11.5 |
| Primary Disorders (%) | |||
| Social Anxiety | 13.5 | 23.1 | 18.3 |
| Generalized Anxiety | 5.8 | 9.6 | 7.7 |
| Panic | 7.7 | 1.9 | 4.8 |
| Obsessive Compulsive | 3.8 | 1.9 | 2.9 |
| Major Depression | 1.9 | 3.8 | 2.9 |
| Substance Use | 1.9 | 3.8 | 2.9 |
| Other | 3.8 | 7.6 | 5.9 |
| BDI, M (SD) | 10.94 (9.14) | 12.00 (9.69) | 11.47 (9.39) |
| BAI, M (SD) | 15.65 (10.31) | 14.60 (9.11) | 15.12 (9.70) |
| ASI, M (SD) | |||
| Total | 29.40 (8.87) | 29.88 (9.90) | 29.64 (9.36) |
| Physical | 15.48 (6.13) | 16.17 (6.89) | 15.83 (6.50) |
| Social | 9.25 (2.72) | 9.50 (2.82) | 9.37 (2.76) |
| Cognitive | 4.67 (3.59) | 4.21 (3.43) | 4.44 (3.50) |
Note. BDI = Beck Depression Inventory; BAI = Beck Anxiety Inventory; ASI = Anxiety Sensitivity Index.
Therapists
Study therapists were doctoral students in a clinical psychology program. They were trained in the intervention protocol to ensure familiarity and adherence to the protocol. In addition, detailed manuals were provided to facilitate the presentation of the PowerPoint.
Assessments
Diagnostic Interview
Structured Clinical Interview for DSM-IV (SCID)
Axis I psychiatric diagnoses were determined using the SCID-NP (non-patient version; (First, Spitzer, Gibbon, & Williams, 1994)). The SCID was administered by doctoral student therapists who completed an extensive training in its administration and scoring. Interrater reliability estimates were calculated by comparing an additional random sample of approximately 5% of the SCID interviews conducted by the graduate therapists in the research clinic to a senior Ph.D-level clinical therapist. This large-scale analysis produced a kappa of .83.
Self-report Measures
Anxiety Sensitivity Index (ASI)
The ASI (Reiss, Peterson, Gursky, & McNally, 1986) is a 16-item measure of the fear of anxiety-related symptoms, AS. The measure has established strong psychometrics (Reiss, et al., 1986).
Beck Anxiety Inventory (BAI)
The BAI is a measure of general anxiety symptoms that has been shown to be both valid and reliable (Beck, Epstein, Brown, & Steer, 1988).
Beck Depression Inventory (BDI)
The BDI is a measure of general depression symptomatology that has been shown to be valid and reliable (Beck, Steer, & Garbin, 1988).
Homework Adherence
Homework Quantity Ratings
Three separate ratings of HW quantity were calculated based on the returned HW at week one and month one. The ratings included the number of days HW was completed, the number of online daily responses noting they had completed the HW, and the number of IE trials completed.
Homework Quality Rating
The overall quality of completed IE HW was assessed at both time points. Specifically, scores were calculated for the percentage of trials the participant identified 1) the IE exercises completed, 2) the sensations experienced, 3) the thoughts as well as 4) the percentage of days that initial fear reached a moderate level (five or greater on ten point scale) and 5) the fear reduced to a minimal level (one or lower on a ten point scale).
Procedure
Time Points
During the screening appointment, participants first consented to the study then completed the SCID and screening questionnaires. Those who met inclusionary criteria were randomly assigned to an experimental condition. At the intervention appointment, participants completed their assigned condition as well as pre- and post-treatment self-report measures. During both the mid-week and mid-month check-ins, participants logged in to the secure study website and completed the ASI. During the week one and month one follow-up appointments, their HW forms were collected and they completed the self-report questionnaires.
Description of Experimental Conditions
Anxiety Sensitivity Education and Reduction Training (ASERT)
This intervention was adapted from Schmidt et al. (2007). The therapist met with the participant for approximately 50 minutes to review a PowerPoint presentation and conduct IE. The presentation focused on the nature of stress and dispelling myths about the dangers of physiological arousal. After the presentation, the participant's fear of arousal sensations was assessed through completion of a number of IE exercises. The top fear producing exercise was repeated until distress ratings reached a minimal level (0-2). Monitoring forms were provided for daily IE HW over the month.
Physical Health Education Training (PHET)
This condition was designed to control for effects of general education and time spent with a therapist. The PHET PowerPoint presentation covered; diet, alcohol, water consumption, exercise and sleep. Monitoring of daily health habits was discussed and daily monitoring forms were provided for the subsequent month.
Results
Sample and Preliminary Analyses
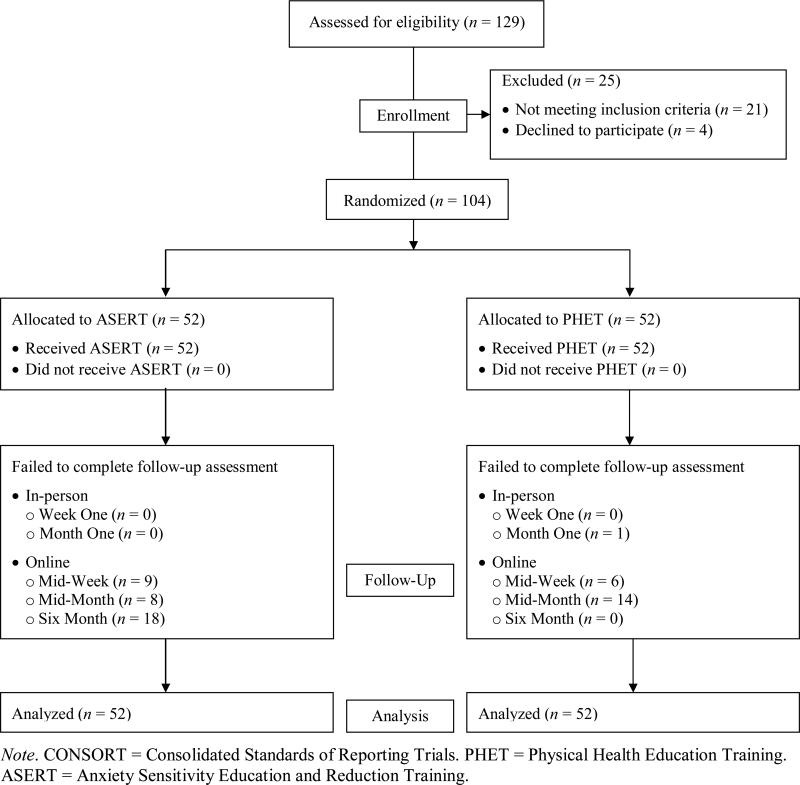
See Figure 1 for the CONSORT diagram. Pretreatment data indicate that there were no differences between conditions on the ASI (t (102) = .26, p = .80), BAI (t (102) = -.55, p = .58) or BDI (t (102) = .57, p = .57; see Table 1 for baseline scores). There were no differences between groups on current diagnoses (anxiety disorders (x2 (1) = .66, p = .42), mood disorders (x2 (1) = 2.83, p = .09), or any Axis I disorder (x2 (1) = 2.50, p = .11) nor were there any demographic differences between the groups: age (t (102) = -.89, p = .37), gender (x2 (1) = .07, p = .79), or race (x2 (4) = .75, p = .95).
Figure 1.
CONSORT Chart of Participants Detailing Patient Flow, Assignment and Drop-out.
Main Study Hypotheses
The effect of treatment condition on posttreatment AS was examined with four separate hierarchical linear regressions. In each equation, the ASI total, physical, social or cognitive scores served as the dependent variable while the pretreatment score for the dependent variables served as independent variable in Steps 1 and 2. Treatment condition (PHET coded 1; ASERT coded 2) was added as an independent variable at Step 2. The ASERT group evidenced a greater reduction in total and subscales ASI scores than the PHET group (see Table 2).
Table 2.
An examination of Treatment Condition on Posttreatment ASI.
| ASI |
||||||||
|---|---|---|---|---|---|---|---|---|
| Total |
Physical |
Social |
Cognitive |
|||||
| Predictor | ΔR2 | ß | ΔR2 | ß | ΔR2 | ß | ΔR2 | ß |
| Step 1 | .67 | .61 | .75 | .75 | ||||
| Pretreatment ASI | .82 | .78 | .86 | .86 | ||||
| Step 2 | .09 | .10 | .02** | .03 | ||||
| Pretreatment ASI | .81 | .76 | .85 | .88 | ||||
| Treatment Condition | -.29 | -.32 | -.14** | -.17 | ||||
Note. All values significant at p < .001 except where noted
p < .01.
ASI = Anxiety Sensitivity Index.
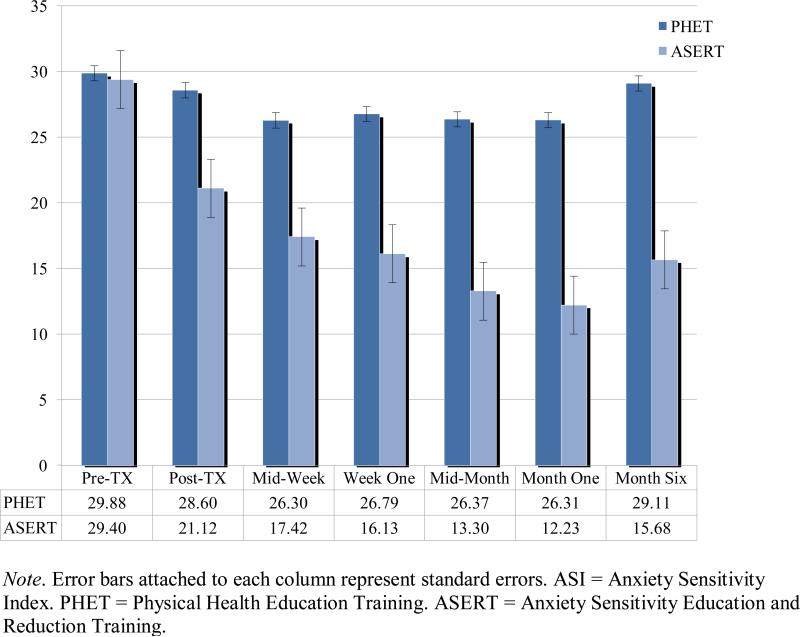
Following the same analytic strategy employed above, the change from baseline to each follow-up time point between the two conditions was examined. In line with study hypotheses, the ASERT group reported a greater reduction across the ASI total and subscale scores (see Table 1). ASI scores across the study period are presented in Figure 2.
Figure 2.
ASI Total Scores by Treatment Condition Across the Study Period.
To assess the maintenance effects of the interventions over the follow-up period, we repeated the analyses controlling for posttreatment scores. This allows for an examination of whether additional treatment gains were made between the two groups following the intervention appointment (see Table 3). These results indicated that there was a significant difference between groups across all ASI scores beginning at the mid-month check-in. All of the above analyses were rerun with psychiatric medication status as a covariate. These analyses indicated that medication status did not affect the pattern of results.
Table 3.
Beta Weights Examining Differences in ASI Scores Between the Two Participant Conditions Across the Follow-up Time Points.
| Time Points | |||||
|---|---|---|---|---|---|
| Mid-week | Week One | Mid-Month | Month One | Month Six | |
| Controlling for Baseline ASI | |||||
| ASI | |||||
| Total | -.37 (.67, .13)*** | -.42 (.68, .18)*** | -.47 (.70, .22)*** | -.54 (.62, .29)*** | -.51(41, .26)*** |
| Physical | -.36 (.66, .13)*** | -.41 (.65, .17)*** | -.51 (.66, .26)*** | -.54 (.58, .29)*** | -.54 (.42, .29)*** |
| Social | -.24 (.61, .06)*** | -.32 (.61, .10)*** | -.31 (.52, .09)*** | -.44 (.55, .19)*** | -.39 (.38, .15)*** |
| Cognitive | -.24 (.69, .06)*** | -.27 (.68, .07)*** | -.31 (.59, .09)*** | -.38 (.59, .15)*** | -.33 (.43, .11)** |
| Controlling for Posttreatment ASI | |||||
| ASI | |||||
| Total | -.10 (.80, .01) | -.16 (.81, .02)** | -.26 (.81, .06)*** | -.31 (.76, .09)*** | -.32 (.47, .09)** |
| Physical | -.08 (.80, .01) | -.15 (.80, .02)** | -.28 (.80, .07)*** | -.30 (.75, .08)*** | -.33 (.48, .09)** |
| Social | -.14 (.70, .02)* | -.21 (.71, .04)*** | -.21 (.67, .04)** | -.34 (.64, .11)*** | -.35 (.37, .12)** |
| Cognitive | -.05 (.81, .00) | -.09 (.77, .01) | -.18 (.78, .03)** | -.22 (.74, .05)*** | -.21 (.50, .04)* |
Note. R squared and R squared change are in parentheses. ASI = Anxiety Sensitivity Index.
p < .001
p < .01
p < .05
To examine whether diagnostic status resulted in differential treatment response, we completed moderator analyses. A hierarchical linear regression was constructed with the month one ASI score serving as the dependent variable. Treatment condition and diagnostic status were entered into the first step as independent variables as well as pretreatment ASI as a covariate. The treatment condition and diagnostic status interaction term were entered into the second step. Treatment condition and diagnostic status were centered in order to reduce multicollinearity. While condition was associated with month one ASI scores (β = - .54, p < .001), neither diagnostic status (β = .002, p = .98) nor the interaction term (β = -.03, p = .66) was. Total variance accounted for at Step 2 was 62% with .1% explained by the two independent variables. This suggests that diagnostic status did not affect treatment gains.
Several indices of HW adherence were collected among the ASERT condition to assess IE HW completion. We anticipated that the number of days IE was completed (quantity index) and the percentage of days IE trials were continued to the point of minimal distress (quality index) would be most predictive of posttreatment AS reduction. We focused our analyses on the month one time point as this timeframe allowed for a greater period of learning. Two linear regressions were constructed with either the quantity or quality index as the predictor, month one ASI as the dependent variable and pretreatment ASI as a covariate. Neither quantity (β = -.02, p = .91, R2 = .28, ΔR2 = .001) nor quality (β = .01, p = .92, R2 = .28, ΔR2 = .001) was associated with month one AS. Given that these results ran counter to our hypotheses, we ran analyses examining the other HW indices. Using the above analytic strategy, the same pattern of results emerged with neither HW quality nor quantity associated with AS scores at week one or month one.
Discussion
Despite the PHET condition being a somewhat active control group, the ASERT group demonstrated greater reductions in AS immediately following treatment and additional gains across the follow-up period. The current results demonstrate that this brief intervention had a broad effect on AS as evidenced by reductions across all subscales. Moreover, both groups largely maintained their scores with the ASERT group retaining the majority of their AS reduction while the PHET group continued to report substantially elevated AS scores.
Direct comparisons across AS intervention trials are complicated by a host of factors including different follow-up time points, AS measures, levels of baseline AS, and length of treatment. Remaining cognizant of the imperfect nature of such a comparison, it is still useful to evaluate the efficacy of the current trial in light of previous trials. The reduction in total AS scores in the current study at the month one follow-up (58%) is greater in magnitude than the reductions reported by Gardenswartz and Craske (2001) (43%), Feldner et al. (2008) (34%), Broman-Fulks et al. (2008) (41%) and Schmidt et al. (2007) (30%). The current results suggest that the ASERT intervention resulted in greater treatment effects than the previous interventions.
As would be expected based on the elevated AS in the current sample, there was a high rate of current Axis I psychopathology. While it could be hypothesized that current psychopathology would result in reduced responsiveness to ASERT, those with and without an Axis I diagnosis showed the same pattern of AS treatment results. This speaks to ASERT's potential applications both in terms of prevention, as was seen in the Schmidt et al. (2007) investigation, and as a possible adjunct to assist therapists working with anxiety patients.
Counter to our hypotheses, HW indices were not associated with AS treatment gains. However, the pattern of AS scores across the study (see Figure 2) indicate that the reduction in AS scores was not limited to the intervention appointment but continued across the HW period with the lowest scores recorded at the end of this period. The only additional intervention during this time was the assigned IE HW, which is consistent with the idea that IE HW may be partially responsible for these gains. Future research should continue to explore IE HW to examine whether it is necessary for treatment gains and if so how much is necessary to maximize gains.
This study should be considered in light of its limitations and opportunities for subsequent research. Beyond the limitations and future research noted above, the current sample had limited age and racial heterogeneity. While the sample was composed of a substantial proportion of individuals with current psychopathology and others at increased risk for psychopathology based both on age and elevated AS, future investigations should employ a more diverse sample to ensure the intervention's generalizability. As noted, this investigation was not designed to assess the prevention of psychopathology. Future investigations with this aim especially in young samples would add to our understanding of anxiety prevention.
Despite these limitations, this investigation provides important information regarding the amelioration of a well-established anxiety risk and maintenance factor. Many individuals receive anxiety treatment after years of impairment or receive no treatment at all due largely to barriers in access and cost (Schmidt & Keough, 2010; Wang, et al., 2005). Weekly therapy sessions with a highly trained therapist remain the therapeutic gold standard but this model is not sufficiently meeting society's profound need. Interventions such as the current one that produce a sizable treatment effect in AS through a one hour computer assisted intervention have the potential to help address this void by addressing access and cost. While this type of intervention does not fully address these problems, they have the potential to fill a need in a stepped care process that offers the potential to more fully address the current inadequacies in our mental health system.
Acknowledgments
This investigation was supported in part by a National Institutes of Mental Health Award (1F31 MH086174-01).
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/CCP
Contributor Information
Meghan E. Keough, Florida State University Department of Psychiatry and Behavioral Sciences, University of Washington School of Medicine..
Norman B. Schmidt, Florida State University
References
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Broman-Fulks JJ, Storey KM. Evaluation of a brief aerobic exercise intervention for high anxiety sensitivity. Anxiety Stress Coping. 2008;21:117–128. doi: 10.1080/10615800701762675. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Ollendick TH. Empirically supported psychological interventions: controversies and evidence. Annual Review of Psychology. 2001;52:685–716. doi: 10.1146/annurev.psych.52.1.685. [DOI] [PubMed] [Google Scholar]
- Fedoroff IC, Taylor S, Asmundson GJG, Koch WJ. Cognitive factors in traumatic stress reactions: Predicting PTSD symptoms from anxiety sensitivity and beliefs about harmful events. Behavioural and Cognitive Psychotherapy. 2000;28:5–15. [Google Scholar]
- Feldner MT, Zvolensky MJ, Babson K, Leen-Feldner EW, Schmidt NB. An integrated approach to panic prevention targeting the empirically supported risk factors of smoking and anxiety sensitivity: Theoretical basis and evidence from a pilot project evaluating feasibility and short-term efficacy. Journal of Anxiety Disorders. 2008;22:1227–1243. doi: 10.1016/j.janxdis.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldner MT, Zvolensky MJ, Schmidt NB. Prevention of anxiety psychopathology: A critical review of the empirical literature. Clinical Psychology: Science and Practice. 2004;11:405–424. [Google Scholar]
- First MB, Spitzer RL, Gibbon J, Williams JB. Structured Clinical interview for DSM-IV nonpatient edition (SCID-N/P, Version 2.0) Biometrics Research Department; New York: 1994. [Google Scholar]
- Gardenswartz CA, Craske MG. Prevention of panic disorder. Behavior Therapy. 2001;32:725–737. [Google Scholar]
- Greenberg PE, Sisitsky T, Kessler RC, Finkelstein SN, Berndt ER, Davidson JR, Fyer AJ. The economic burden of anxiety disorders in the 1990s. Journal of Clinical Psychology. 1999;60:427–435. doi: 10.4088/jcp.v60n0702. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–603. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- McLeish AC, Zvolensky M, Smits JA, Bonn-Miller MO, Gregor K. Concurrent associations between anxiety sensitity and perceived health and health disability among young adult daily smokers. Cognitive Behaviour Therapy. 2007;36:1–11. doi: 10.1080/16506070600794653. [DOI] [PubMed] [Google Scholar]
- Ocanez KLS, McHugh RK, Otto M. A meta-analytic review of the association between anxiety sensitivity and pain. Depression and Anxiety. 2010;27:760–767. doi: 10.1002/da.20681. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Wolitzky-Taylor KB. Anxiety sensitivity and the anxiety disorders: a meta-analytic review and synthesis. Psychology Bulletin. 2009;135:974–999. doi: 10.1037/a0017428. [DOI] [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety Sensitivity, Anxiety Frequency and the Prediction of Fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Eggleston AM, Woolaway-Bickel K, Fitzpatrick KK, Vasey MW, Richey JA. Anxiety sensitivity amelioration training (ASAT): A longitudinal primary prevention program targeting cognitive vulnerability. Journal of Anxiety Disorders. 2007;21:302–319. doi: 10.1016/j.janxdis.2006.06.002. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Keough ME. Treatment of panic. Annual Review of Clinical Psychology. 2010;6:241–256. doi: 10.1146/annurev.clinpsy.121208.131317. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Lerew DR, Jackson RJ. The role of anxiety sensitivity in the pathogenesis of panic: Prospective evaluation of spontaneous panic attacks during acute stress. Journal of Abnormal Psychology. 1997;106:355–364. doi: 10.1037//0021-843x.106.3.355. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Trakowski J. Interoceptive assessment and exposure in panic disorder: A descriptive study. Cognitive and Behavioral Practice. 2004;11:81–92. [Google Scholar]
- Schmidt NB, Zvolensky MJ, Maner JK. Anxiety sensitivity: Prospective prediction of panic attacks and axis I pathology. Journal of Psychiatric Research. 2006;40:691–699. doi: 10.1016/j.jpsychires.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:603–613. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]