Abstract
Background
The safety benefits of bar-coded medication dispensing and administration technology (BCMA) depend on its intended users favorably perceiving, accepting, and ultimately using the technology.
Objectives
(1) To describe pharmacy workers’ perceptions and acceptance of a recently implemented BCMA system and (2) to model the relationship between perceptions and acceptance of BCMA.
Methods
Pharmacists and pharmacy technicians at a Midwest US pediatric hospital were surveyed following the hospital’s implementation of a BCMA system. Twenty-nine pharmacists and ten technicians’ self-reported perceptions and acceptance of the BCMA system were analyzed, supplemented by qualitative observational and free-response survey data. Perception-acceptance associations were analyzed using structural models.
Results
The BCMA system’s perceived ease of use was rated low by pharmacists and moderate by pharmacy technicians. Both pharmacists and technicians perceived that the BCMA system was not useful for improving either personal job performance or patient care. Pharmacy workers perceived that individuals important to them encouraged BMCA use. Pharmacy workers generally intended to use BCMA but reported low satisfaction with the system. Perceptions explained 72% of the variance in intention to use BCMA and 79% of variance in satisfaction with BCMA.
Conclusions
To promote their acceptance and use, BCMA and other technologies must be better designed and integrated into the clinical work system. Key steps to achieving better design and integration include measuring clinicians’ acceptance and elucidating perceptions and other factors that shape acceptance.
Keywords: bar coded medication dispensing and administration systems, BCMA, technology acceptance, pediatric hospital
Medication errors may be as prevalent as one per day for the average hospitalized patient.1 Administration errors are especially common and, compared to errors occurring at other medication management stages, have a low probability of being intercepted.2 Bar-coded medication dispensing and administration (BCMA) technology is recommended as one way to prevent inpatient medication administration errors and to detect errors before they cause harm.3,4 Recent studies by Poon and colleagues offer evidence that BCMA improves medication dispensing and administration safety.5,6 However, there was also evidence that pharmacy workers perceived the BCMA system to worsen work performance, leading to staff resistance.7 Research on nurses shows that nurses employ numerous workarounds and often override BCMA systems.8,9 Workarounds, overrides, and similar behaviors partially result from clinicians’ low acceptance of the health information technology (HIT) in question and low acceptance, in turn, may be caused by unfavorable perceptions concerning the HIT.10 It is therefore important to assess clinicians’ perceptions and acceptance of new HIT and to identify those perceptions associated with HIT acceptance.11 However, nurses’ perceptions and acceptance of BCMA are seldom studied, 12,13 and studies of pharmacy workers’ perceptions and acceptance are entirely absent. Thus, this study’s two objectives were: (1) to describe hospital pharmacists’ and pharmacy technicians’ perceptions and acceptance of a recently implemented BCMA system and (2) to model the relationship between perceptions and acceptance of BCMA. Although it is important to measure a variety of BCMA-related perceptions following BCMA implementation (Objective 1), it is equally as important to find out which of these perceptions is driving workers’ acceptance of BCMA (Objective 2). The latter allows a more focused approach to generating solutions to improve BCMA acceptance and use.
Conceptual framework
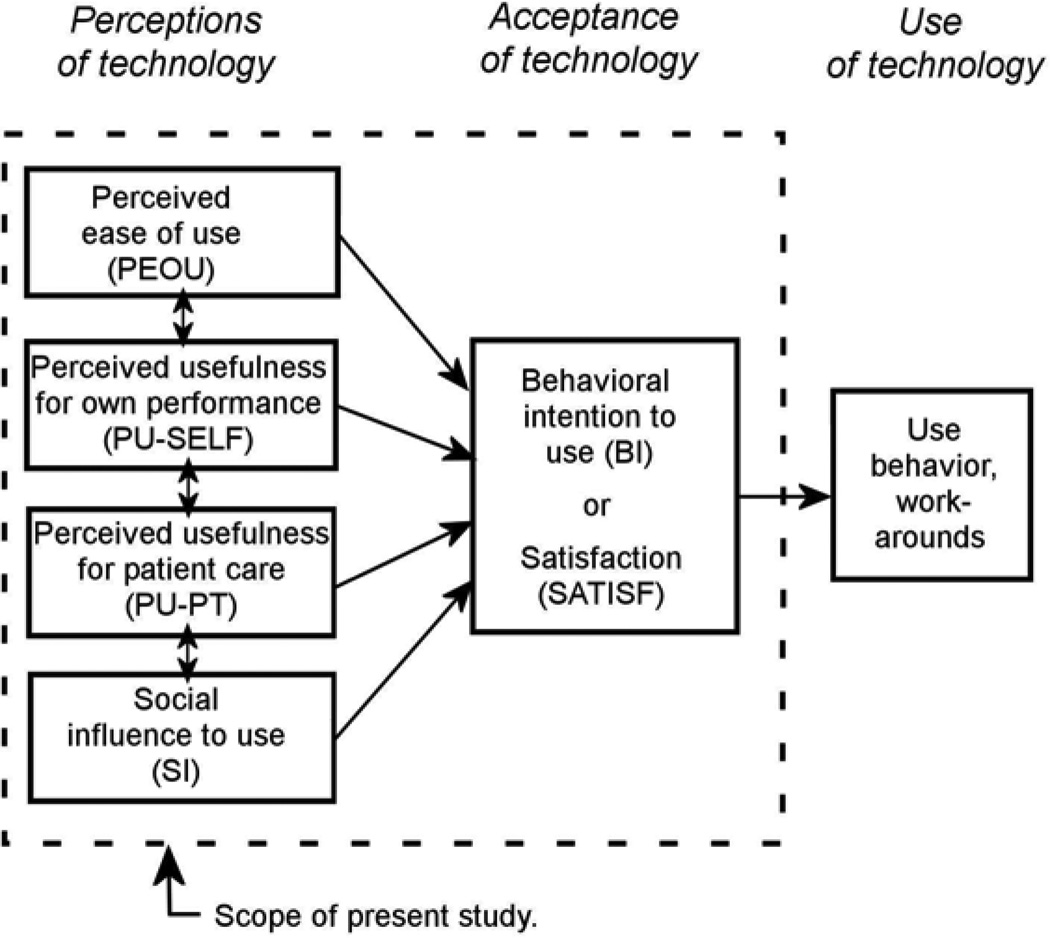
The study’s conceptual framework (Figure 1) is adapted from the Technology Acceptance Model (TAM), a family of theories—TAM,14 TAM2,15 and TAM316—that posit a causal relationship (a) between user perceptions of technology and user acceptance and (b) between acceptance and actual use.* TAM is the most widely used theoretical framework in the health IT acceptance and use literature, though no previous work has used TAM to study BCMA or pharmacy workers.11 Following TAM, this study assessed three categories of BCMA perceptions:
Perceived ease of use (PEOU), or “the degree to which a person believes that using a particular system would be free of effort.”14, p.320
Perceived usefulness (PU), or “the degree to which a person believes that using a particular system would enhance his or her job performance.”14, p.320 Holden and Karsh note that PU is often defined in terms of usefulness for the user’s productivity on the job (PU-SELF) but that in healthcare settings, PU can also be thought of in terms of usefulness for improving patient care (PU-PT).11 PU-SELF and PU-PT were both measured in this study.
Perceived social influence (SI), or “the degree to which an individual perceives that important others believe he or she should use the new system.”17, p.451
Figure 1.
The study’s conceptual model, depicting a relationship between several perceptions of technology and technology acceptance, conceptualize as behavioral intention to use and/or satisfaction with technology. A relationship between acceptance and use behavior is posited but not within the scope of the present study.
This study also assessed two categories of pharmacy workers’ acceptance of BCMA:
Behavioral intention (BI) to use BCMA.
Satisfaction (SATISF) with BCMA.
BI and SATISF are the two classic conceptualizations of technology acceptance, and both are believed to predict actual use.18,19 BI is conceptually similar to an individual’s motivation to use BCMA and is the measure of acceptance specified in TAM.14 SATISF is an overall evaluation or attitude toward BCMA and is the measure of acceptance recommended when technology use is mandatory. 20 Although perceived ease of use, perceived usefulness, and social influence are typically hypothesized to predict acceptance, behavioral theory and evidence from TAM research in healthcare suggests that in different contexts, different predictors will be salient.11,21 Thus, for example, it can be hypothesized that perceived usefulness for patient care will be a salient predictor of acceptance of a safety-promoting technology in a clinical setting and may be a stronger predictor of acceptance than a more generic measure of usefulness for one’s job performance.
METHODS
Design and setting
The study was a cross-sectional, paper survey administered to pharmacists and pharmacy technicians at a 236-bed free-standing pediatric academic community hospital in the Midwest US. The survey was administered August-November 2007, about 8 months after a phased roll- out of a BCMA system (GE Healthcare’s Centricity Pharmacy). The hospital additionally used computerized provider order entry (CPOE) and automated medication-dispensing cabinets. The study was approved by Institutional Review Boards at the University of Wisconsin-Madison and the study hospital. Details on survey administration procedures are available elsewhere.22
Survey instrument
Standard multi-item scales validated in prior TAM studies were used for PEOU,23 PU-SELF,23 and SI.24 BI was measured with two items from Venkatesh and Morris25 and two items created for the study. PU-PT and SATISF scales were newly created for the study. All survey items were based on strong theory and underwent extensive pre-testing by the research team, survey experts, and clinicians. Frequent prompts in the survey asked respondents to think of “the past 30 days.” Responses were on a numbered seven-point scale ranging from 0 to 6, with the response category labels “not at all,” “a little,” “some,” “a moderate amount,” “pretty much,” “quite a lot,” and “a great deal,” as well as an option to mark “don’t know.” Table 2 shows individual scale items and reports each scale’s internal consistency.
Table 2.
Sample demographics.
| All pharmacy workers |
Pharmacists | Pharmacy technicians |
|
|---|---|---|---|
| Analyzed N | N = 39 | N = 29 | N = 10 |
| % Female | 51% | 41% | 80% |
| % White, non-Hispanic | 97% | 96% | 100% |
| Age | |||
| 18–29 | 10% | 11% | 10% |
| 30–39 | 10% | 7% | 20% |
| 40–49 | 50% | 46% | 60% |
| 50–59 | 26% | 32% | 10% |
| 60+ | 3% | 4% | 0% |
| Education | |||
| % completing college | 31% | 100% | 50% |
| % completing graduate/professional school | 56% | 72% | 10% |
| Years in occupation | 18.0 | 21.0 | 9.8 |
| Years with hospital | 13.5 | 16.2 | 5.9 |
| Shift worked | |||
| Day | 56% | 65% | 30% |
| Evening | 23% | 21% | 30% |
| Night | 8% | 7% | 10% |
| Floating | 10% | 7% | 20% |
| Weekend only | 3% | 0% | 10% |
| Hours worked in average week (SD) | 38.8(14.7) | 40.7(12.4) | 33.4(19.8) |
Analysis
Descriptive statistics for perceptions and acceptance scales and individual items were calculated in SPSS. Scores one each scale were calculated for respondents by taking the mean of all valid individual item responses from that scale (using a floating denominator). Scale means and standard deviations were then calculated for all pharmacy workers, pharmacists only, and pharmacy technicians only. Pharmacists’ and technicians’ mean scores were compared with independent samples t-tests with unequal variances assumed. Response frequencies were calculated for individual scale items. Because there was some missing data, response frequencies were calculated using the total number of valid responses (i.e., not counting item non-responses) as the denominator.
To test the perception-acceptance relationship, two Composite Indicator Structural Equation (CISE)-alpha models26 were analyzed in MPlus, using maximum likelihood estimation with pair-wise deletion. In this approach, composite indicators (scales) are modeled and adjusted for measurement error. Measurement error for the composite indicators can either be fixed based on a priori knowledge of the reliability of the composites, or from sampled measures of Cronbach’s alpha or split-half reliability. In this study’s models, the measurement error was fixed and based on an estimate of reliability of composite variables, (1 - Cronbach's alpha)*σ2.27
In one model, the outcome was BI (behavioral intention to use BCMA); in the other, SATISF (satisfaction with BCMA). In both models, PEOU, PU-SELF, PU-PT, and SI served as the predictors. The participant’s role (ROLE: pharmacist vs. pharmacy technician) was entered as a covariate to adjust all estimated relationships for differences in role and to test whether BCMA acceptance differed by role. An a priori alpha criterion of .05 was used. 95% confidence intervals and model R2 were calculated.
CISE-alpha modeling is a variant of regression and therefore should meet sample size requirements for conducting regression. The current analyzed sample size met the common rule of thumb criterion that there should be at least a five-to-one ratio between the number of subjects (N = 39) and the number of estimated parameters (five in the present models: four predictors and one covariate).28 CISE-alpha was selected because, for small sample sizes, it is a superior approach compared to structural equation modeling, which involves a large number of parameters, or path analysis, which does not adjust for measurement error and results in less reliable estimates.29, 30
Qualitative data for interpreting survey findings
Qualitative observation and open-ended survey data were collected and analyzed to help interpret pharmacy workers’ BCMA perceptions. Observations of 16 pharmacy workers (7 pharmacists, 9 pharmacy technicians) were conducted February – March 2008, a little over one year after BCMA implementation. Open-ended responses about BCMA were analyzed from a follow-up survey administered to pharmacy workers February – May 2008. Qualitative data were analyzed for themes and specific examples that might explain pharmacy workers’ quantitative survey responses.
RESULTS
Forty-one of 73 (56.2%) pharmacy workers completed the survey. Two respondents were removed from analyses because they had no direct clinical duties or did not report their work role. This resulted in an analyzed sample of 39 respondents: 29 pharmacists and 10 pharmacy technicians. Sample demographics are reported in Table 2.
Perceptions of BCMA system
Table 3a reports pharmacy workers’ mean scores on the four perception scales (response frequencies for individual items are reported in the Appendix). Pharmacists rated the BCMA system as not easy to use. Twenty-four percent of pharmacists perceived that BCMA was “not at all” easy to use and 41% that using BCMA required “quite a lot” of mental effort or more. In contrast, technicians had moderate or higher ratings of BCMA ease of use, with 50% of technicians responding that BCMA was “quite a lot” or “a great deal” clear and understandable.
Table 3.
Mean scores on perception and acceptance scales for all pharmacy workers, pharmacists, and pharmacy technicians.*
| Mean (SD) | |||
|---|---|---|---|
| All pharmacy workers |
Pharmacists | Pharmacy techgtcians |
|
| (a) Perceptions | |||
| Perceived ease of use (PEOU)** | 2.56(1.35) | 2.17(1.10) | 3.68(1.42) |
| Perceived usefulness for self (PU-SELF) | 1.57(1.38) | 1.38(1.17) | 2.17(1.86) |
| Perceived usefulness for patient (PU-PT) | 2.04(1.68) | 1.88(1.71) | 2.61 (1.54) |
| Perceived social influence (SI) | 4.20(1.76) | 4.29(1.75) | 3.95(1.86) |
| (b) Acceptance | |||
| Behavioral intention to use system (BI) | 3.12(1.66) | 3.14(1.57) | 3.06(2.03) |
| Satisfaction with system (SATISF) | 2.23(1.64) | 2.03(1.58) | 2.78(1.76) |
Scale range from 0 to 6.
p ≤ .05 for independent samples t-test comparing pharmacists and technicians.
Pharmacy workers did not perceive that BCMA was useful for improving either personal job performance or patient care. Thirty-seven percent of all respondents (37% of pharmacists, 37% of technicians) believed that BCMA did “not at all” improve job performance and 52% (56% of pharmacists, 25% of technicians) perceived that BCMA did “not at all” make patient care easier. However, 47% of respondents (48% of pharmacists, 43% of technicians) believed that BCMA reduced the likelihood of medication error “a moderate amount” or more.
Pharmacy workers reported high social influence to use BCMA. In response to the question, “To what extent do people who influence your behavior think that you should use the bar-coding system,” 69% (77% of pharmacists, 44% of technicians) responded “quite a lot” or more. Statistically significant correlations were found between PEOU and PU-SELF (r = .57), PEOU and PU-PT (r = .59), and PU-SELF and PU-PT (r = .65).
Acceptance of BCMA system
Table 3b reports mean scores on the two acceptance scales. Intention to use BCMA was moderate and although pharmacy workers predicted that they would use the system, 28% (32% of pharmacists, 12% of technicians) reported that if it were up to them, they would not use it at all. Twenty-nine percent of pharmacy workers (30% of pharmacists, 25% of technicians) responded “not at all” to the question “How much do you want to use the bar-coding system?” Satisfaction with BCMA was low. Forty-six percent of all respondents (46% of pharmacists, 43% of technicians) reported that they would not recommend the BCMA system to a friend at another hospital and 63% (68% of pharmacists, 43% of technicians) reported “a moderate amount” or more dissatisfaction with BCMA. (Ninety-one percent of pharmacy workers, and 100% of pharmacy technicians, reported a non-zero level of dissatisfaction with BCMA.) A statistically significant correlation was found between BI and SATISF (r = .61).
Perceptions associated with BCMA acceptance
In CISE-alpha models, the combination of perceptions explained 72% (± 32%) of variance in behavioral intention (BI) to use BCMA and 79% (± 9%) in satisfaction (SATISF) with BCMA. Significant predictors of BI were, in order of magnitude, perceived usefulness of BCMA for patient care (PU-PT) and perceived social influence to use BCMA (SI). Significant predictors of SATISF with BCMA were, in order of magnitude, perceived ease of use of BCMA (PEOU), perceived usefulness of BCMA for patient care (PU-PT), and perceived usefulness of BCMA for one’s job (PU-SELF). In neither of the models was the covariate ROLE statistically significant. Table 4 reports unstandardized and standardized parameter estimates for the two CISE-alpha models.
Table 4.
Results of Composite Indicator Structural Equation (CISE)-alpha modeling analysis with (A) behavioral intention to use BCMA and (B) satisfaction with BCMA as the outcomes.*
| Unstandardized parameter estimate (95% confidence interval) |
Standardized parameter estimate (95% confidence interval) |
||
|---|---|---|---|
| (A) |
Behavioral intention to use system (BI) (R2 = .72; 95% CI [.40, 1.04]) |
||
| Perceived ease of use (PEOU) | .01 (−.47, .49) | .01 (−.44, .46) | |
| Perceived usefulness for self (PU-SELF) | .36 (−.02, .74) | .37 (−.03, .78) | |
| Perceived usefulness for patient (PU-PT)*** | .49 (.17, .82) | .62 (.26, .98) | |
| Perceived social influence (SI)** | .34 (.05, .62) | .41 (.07, .74) | |
| Covariate: Pharmacist vs. technician (ROLE) | .52 (−.45, 1.50) | .18 (−.16, .52) | |
| (B) |
Satisfaction with system (SATISF) (R2 = .79; 95% CI [.70, .88]) |
||
| Perceived ease of use (PEOU)*** | .63 (.28, .98) | .60 (.33, .88) | |
| Perceived usefulness for self (PU-SELF)*** | .40 (.09, .70) | .41 (.08, .75) | |
| Perceived usefulness for patient (PU-PT)*** | .38 (.12, .63) | .48 (.15, .81) | |
| Perceived social influence (SI) | −.03 (−.24,. 19) | −.03 (−.29, .23) | |
| Covariate: Pharmacist vs. technician (ROLE) | .43 (−.33, 1.19) | .15 (−.10, .40) |
BCMA = Bar coded medication administration and dispensing system; CI = confidence interval.
Parameter estimates refer to the predictor-outcome or covariate-outcome association.
p ≤.05,
p ≤.01
DISCUSSION
Pediatric hospital pharmacists did not find their recently implemented BCMA easy to use. and neither pharmacists nor technicians found BCMA useful to themselves. Pharmacy workers were not satisfied with BCMA, despite social pressure from others to use BCMA and a moderate level of intention to do so. While surveys did not quantitatively assess the specific reasons behind these perceptions, qualitative data from observations and open-ended responses to a follow-up survey provide some insight. Findings of low perceived ease of use and usefulness should alert those who design, procure, and implement BCMA that, from the pharmacy employee’s perspective, a BCMA system may not be usable or beneficial and may need to be modified.7,31 The next two sections use the results of qualitative data to illustrate some of the specific ways in which the studied BCMA often did not meet usability and usefulness requirements, possibly explaining the survey findings. Recommendations are available for addressing these and other usability and usefulness concerns.32–34
Ease of use
Observations revealed that BCMA imposed new steps and added time in the medication management process, particularly for pharmacists. As one pharmacist wrote on the follow-up survey, “I would not recommend the bar-code system to any other hospital. It is a very inconsistent system and takes much more time to use than not.”
Bar-codes had to be printed on unit-dosed medication labels and because bar-codes were dose-specific, labels could not be reused when dosing changes were made, requiring new labels to be printed. Sometimes this feature of BCMA created extra work for pharmacists, who had to “play games” with BCMA, as one pharmacist said,35 to allow nurses to administer a full dose: for example, to administer up to 100mg of fentanyl PRN (as needed), as ordered, using 2 × 50mg doses of fentanyl as dispensed from the automatic dispensing cabinet (accompanied by 50mg bar-code labels).
Pharmacists also found themselves paying more careful attention to the timing of medications. In one observation, at 8:40am, a pharmacist in the pediatric intensive care unit’s satellite pharmacy received an order to change the timing on a medication from once every 48h to once every 36h. Thirty-six hours from the most recently documented administration of the dose would be at 8:00 that morning (40 minutes ago). Furthermore, the hourly delivery run from central pharmacy had just left (at 8:30) and the next one would not be until 9:30. The pharmacist selected 10:00 as the scheduled administration time. The pharmacist explained that prior to BCMA, there would not have been as much concern in selecting a “realistic” timing and the expectation would be that the medication would be administered as soon as possible, with the nurse documenting the actual time and the reason for any lateness. With BCMA, any late medication would automatically be marked as a “missed dose,” an outcome that the observed pharmacist preferred to avoid. When pharmacists did schedule medications that could not be realistically administered on time, nurses would request that the pharmacists change the timing in the BCMA system, something that would happen several times in a typical day.
There were other examples of “extra” work. An institutional policy was in place allowing clinicians to use a blank paper medication administration record (MAR) for quickly documenting the administration of lifesaving medications during (non-code) emergency situations. However, BCMA was being used to retroactively charge these administered medications, which would require the pharmacist to enter a new order for those medications into BCMA, charge them, and then discontinue them immediately. As another example"one-time” doses that nurses could previously administer (and document) a second time if necessary “disappeared” from the electronic MAR after the first administration. This resulted in pharmacists having to add an additional PRN order. Referring to an observed case of this type, a pharmacist remarked, “See all the monkey business we do? That’s where things used to be a lot faster.” Importantly, new steps and work processes introduced following BCMA implementation may in fact have helped to improve quality and safety; indeed, the new processes and roles around a new technology may be as important to quality and safety as the technology itself.36 However, when new processes and expectations are experienced by pharmacy workers as “extra work,” this may be because accommodations such as freeing up work time were not made; this may lead to rushing or skipping steps, which may in turn negatively affect safety and quality.37
Pharmacy technicians seemed to perceive less additional BCMA-related work than pharmacists, consistent with their ratings of ease of use being higher than pharmacists’ ratings. Technicians who repackaged pills from bulk bottles to individual blister packs had to print and affix bar-code labels to each new package. One pharmacy technician commented during observations that the new packaging process was less problematic as it became easier over time.
Usefulness
In a follow-up survey response, a pharmacy technician commented, “The pharmacy has incurred a great deal more work, and I would consider it worth the time and effort if it improved patient safety. This is not the case.” Indeed, neither pharmacists nor technicians believed that BCMA was useful for their job in general or for patient care. One frequently cited barrier to BCMA improving patient care was that “nurses have been overriding the system a lot. Some have even admitted to pharmacy [that] they wait until the end of their shift to scan the bar-codes of the meds they have already administered. This defeats the purpose of having bar-coding systems” (from a follow-up survey, pharmacy technician). Such behavior would be consistent with findings from other hospitals around the country.3,8,37,38 Two pharmacists described one reason why nurses might override BCMA: bugs in the BCMA system sometimes resulted in correct medications either not scanning or, upon being scanned, generating an error message identical to the message generated to alert nurses of an incorrect medication.
Pharmacy workers also may have reported low perceived usefulness of BCMA because of the limits of the BCMA in supporting the entirety of medication management. At the time of the survey on perceptions and acceptance, BCMA was not being used to manage pharmacy inventory (though there were plans to, e.g., add automated prompts to restock PRN medications based on the number of doses documented in BCMA as administered) or to keep track of drip rates in “real time.” Additionally, BCMA could not verify important information such as whether a technician had accurately prepared a medication, whether a prepared medication was expired, or the true contents of a temporary medication container (e.g., the BCMA might scan and verify the bar-code affixed to a prepared syringe but could not determine the syringe’s true contents or compare the accuracy of the label relative to those contents). Indeed, pharmacy workers and nurses continued to make major contributions to medication safety, with BCMA providing perhaps only marginal added usefulness in that regard. One pharmacist wrote on the follow-up survey, “As much as technology has helped improve the dispensing process, the human element remains the most important.… We need to be masters of the technology not slaves to it.”
However, some pharmacy workers recognized that BCMA could be useful. One pharmacist wrote, “We are still better off with it then without it…” and several pharmacists and technicians commented during observations how much they valued BCMA’s “Timeline” feature, which gave pharmacy workers quick and easy access to an electronic history of when each medication was documented as administered. The Timeline feature was deemed useful for scheduling administration times and for pharmacokinetics processes. This finding in particular summarizes the current state of health IT in general – that aspects of health IT that support clinician cognitive work are valued, but aspects that increase workload or complicate work, are deemed failures.39
It should be noted that the self-reported low ratings of ease of use and usefulness of BCMA, and the comments and observations that may explain those ratings, do not provide evidence about BCMA’s actual impact on quality and safety. These ratings do, however, provide evidence that pharmacists and pharmacy technicians do not believe BCMA is easy to use or useful. Although it is possible and perhaps even likely that the BCMA design features or policies for BCMA use that contributed to users’ low ratings of ease of use and usefulness did also reduce safety and quality, it is not known what the overall net effect of BCMA was.
Predictors of BCMA acceptance
Pharmacy workers’ perceptions of BCMA explained 72% of variation in their intentions to use it and 79% of their satisfaction, indicating the importance of perceptions. BCMA’s perceived ease of use was strongly associated with pharmacy workers’ satisfaction with BCMA, but not with their intentions to use BCMA. This suggests that pharmacy workers may put up with a difficult-to-use system if they must, but that they may not be satisfied with it. Consequently, the usability of a BCMA or other health IT used by pharmacy workers should be a central concern.39
The perceived usefulness of BCMA for personal job performance was associated with satisfaction but not intention to use BCMA, whereas the perceived usefulness of BCMA for patient care was a strong and significant predictors of both acceptance outcomes. Clearly, pharmacy workers make decisions about and evaluate technological systems based on their potential benefit for patient care, and less so on generic job performance. The perceived impact on patient care of BCMA and other health IT should therefore be measured and should be included in models along with (or instead of) measures of generic perceived usefulness.11, 40
Social influence—or the perception that others wanted pharmacy workers to use BCMA—was positively associated with intention to use BCMA, but not with satisfaction, highlighting the role of social forces in shaping BCMA use behavior, and the need to better understand those forces.41 Although pharmacy workers did not offer comments about the social influence on them to use BCMA, observations and analysis of organizational policies showed that BCMA use was mandatory in most parts of the hospital and that hospital administration expected that BCMA would be used. Indeed, pharmacy workers gave a mean response of 5.6 on the 0–6 scale in answer to the question, “To what extent is the decision to use the bar-coding system beyond your control?” Clinical and management processes (e.g., compliance monitoring) had been newly designed or redesigned around the new BCMA system, lending BCMA a ubiquitous presence; joked one pharmacy technician, “Even our food is bar-coded.”
Limitations
This study was conducted in only one site, whose characteristics and pre-BCMA work patterns likely influenced how pharmacy workers responded to BCMA. As an example, the number of older pharmacists at the research site may have contributed to lower ratings of BCMA’s perceived ease of use. However, in unreported analyses, there was no correlation between age category and any of the perceptions or acceptance scales. In any case, it is important to replicate these findings in other settings and with different BCMA systems.
Although pharmacy workers’ perceptions and acceptance were measured and modeled, this study did not include measures of pharmacy workers’ actual BCMA use. Nevertheless, prior empirical and theoretical work contends that acceptance does in fact predict the volume and nature of actual IT use as well as performance with IT.17–19,42 In fact, there is more evidence for the relationship between acceptance and IT use than there is for the relationship between IT system quality and use.43 The health IT literature abounds with case studies of unfavorable perceptions of health IT linked to non-use (overrides, workarounds, feature non-use), resistance, and even abandonment.44–51 There is also emerging quantitative evidence linking perceptions to health IT use.11 Even when clinicians report intending to use a system, dissatisfaction with the system may lead them to use it minimally or perhaps to work around it when possible. For example, Holden and colleagues suggested that nurses’ negative perceptions of the process for documenting medication administration post-BCMA may have resulted in nurses working around the BCMA system studied here.12 It bears investigating whether similar workaround behaviors would be found in the pharmacy context. It could be hypothesized that even in mandatory use environments, certain use behaviors including workarounds and the selective use of BCMA features would result from unfavorable perceptions of BCMA and low satisfaction, even if self-reported intention to use BCMA is high. Further, it might be opined that even if BCMA is used as mandated in the course of pharmacy work, pharmacy workers dissatisfied with BCMA would be less likely to volunteer additional effort to, for example, help nurses to use BCMA more effectively and efficiently.
A small sample size (N = 39) was analyzed, although the response rate was reasonable and over half of the study hospital’s pharmacy workers were surveyed. With pharmacists and technicians combined, the sample size met the rule of thumb criteria for conducting regression-based modeling analyses. This required the combination of two dissimilar work roles. However, all model parameters were adjusted by including ROLE as a covariate and, additionally, there were no differences in acceptance between pharmacists and technicians. Separate pharmacist-only models, not reported here, produced essentially the same pattern of results. This is consistent with the fact that the conceptual models tested here have been validated across a very large variety of worker types within as well as outside of healthcare.11,52–57 Nevertheless, it is worth pursuing further research into whether there are profession- or role-related differences in the acceptance of BCMA or other health IT.58
Some of the survey scales and individual items were either newly created or modified for this study. While their validity requires further testing, the new items were developed based on strong theory; all items were subjected to rigorous pre-testing; all scales had very high internal consistencies (all Cronbach’s alphas ≥ .80); and factor structure was validated using confirmatory factor analysis (not reported). The predictive validity of the survey measures was confirmed by study results.
CONCLUSION
User perceptions and acceptance of health IT are important, especially when the (safety) benefits of the IT depend on the nature of its use. Present findings raise concerns about how well commercially available BCMA systems are designed and implemented for pharmacists and pharmacy technicians. It is suggested that more attention be paid to the IT-related perceptions, acceptance, and use behavior of healthcare professionals. Users’ perceptions of a health IT system are “expert opinions” because, after all, they are the ones using it daily. That does not mean only asking users their preferences for design but also systematically learning about their experiences and involving users as participants in IT usability testing. Additionally, users’ interactions with a health IT ultimately decide its value: even a well-designed IT fails to achieve its outcomes if it is not used, worked around, or used in a limited way or inappropriately. Improved IT design must be accompanied by workable policies for its use and better integration of IT into the structures and processes of work.
Table 1.
Measurement scales, item wording, and Cronbach's alphas for scales.
| Scales | Items | Chronbach’s alpha* |
|---|---|---|
| Perceived ease of use (PEOU) |
|
.80 |
| Perceived usefulness for self (PU-SELF) |
|
.93 |
| Perceived usefulness for patient (PU-PT) |
|
.93 |
| Perceived social influence (SI) |
|
.84 |
| Behavioral intention to use system (BI) |
|
.81 |
| Satisfaction with system (SATISF) |
|
.88 |
Based on the full sample analysis (N=39).
ACKNOWLEDGMENTS
The authors wish to thank the study participants and colleagues involved in the Bar-coding study. This work was supported by a grant from the Agency for Healthcare Research and Quality (AHRQ) (1 R01 HS013610) and National Library of Medicine (1 R01 LM008923) to author BK. The funding agencies had no role in the study or publication except for providing funding for the study. The authors thank two anonymous reviewers for their helpful feedback.
Appendix
Appendix A.
Pharmacists' response frequencies for individual scale items.
| Resiponse frequencies (%) on 0–6 scale | |||||||
|---|---|---|---|---|---|---|---|
| 0 not at all |
1 a little |
2 some |
3 moderate amount |
4 pretty much |
5 quite a lot |
6 a great deal |
|
| Perceived ease of use (PEOU) | |||||||
| … clear and understandable | 0% | 11% | 21% | 29% | 25% | 14% | 0% |
| … easy to use | 24% | 31% | 14% | 14% | 10% | 7% | 0% |
| … requires a lot of mental effort | 0% | 0% | 14% | 28% | 17% | 7% | 34% |
| … easy to get it to do what I want | 21% | 29% | 29% | 4% | 14% | 4% | 0% |
| Perceived usefulness for self (PU-SELF) | |||||||
| … improves job performance | 37% | 19% | 19% | 19% | 7% | 0% | 0% |
| … increases productivity | 64% | 14% | 14% | 7% | 0% | 0% | 0% |
| … enhances effectiveness in job | 39% | 18% | 29% | 11% | 4% | 0% | 0% |
| …useful in job | 18% | 32% | 7% | 21% | 11% | 11% | 0% |
| Perceived usefulness for patient (PU-PT) | |||||||
| … improves patient care | 22% | 26% | 17% | 9% | 13% | 13% | 0% |
| … reduces likelihood of medication error | 24% | 12% | 16% | 16% | 8% | 16% | 8% |
| … facilitates better patient care decision making | 50% | 18% | 5% | 14% | 5% | 5% | 5% |
| … makes caring for patients easier | 56% | 20% | 12% | 8% | 0% | 0% | 4% |
| Perceived social influence (SI) | |||||||
| … people who influence my behavior want me to use system | 7% | 0% | 4% | 4% | 7% | 52% | 26% |
| … people who are important to me want me to use system | 8% | 8% | 8% | 12% | 12% | 24% | 28% |
| Behavioral intention to use system (BI) | |||||||
| … intend to use system, if I have access i | 7% | 15% | 19% | 15% | 7% | 15% | 22% |
| ... predict I will use system, if I have access | 0% | 8% | 19% | 4% | 4% | 23% | 42% |
| … would want to use system, if it were up to me | 32% | 0% | 11% | 21% | 7% | 21% | 7% |
| … want to use the system | 30% | 11% | 15% | 26% | 4% | 11% | 4% |
| Satisfaction with system (SATISF) | |||||||
| … satisfied with system | 21% | 21% | 21% | 11% | 11% | 14% | 0% |
| … prefer system to prior process | 33% | 21% | 17% | 8% | 4% | 13% | 4% |
| … dissatisfied with system | 11% | 14% | 7% | 14% | 11% | 25% | 18% |
| … would recommend to a friend at another hospital | 46% | 14% | 11% | 11% | 7% | 11% | 0% |
Appendix B.
Pharmacy technicians' response frequencies for individual scale items.
| Response frequencies (%) on 0–6 scale | |||||||
|---|---|---|---|---|---|---|---|
| 0 not at all |
1 a little |
2 some |
3 moderate amount |
4 pretty much |
5 quite a lot |
6 a great deal |
|
| Perceived ease of use (PEOU) | |||||||
| … clear and understandable | 0% | 0% | 20% | 0% | 30% | 20% | 30% |
| … easy to use | 0% | 22% | 0% | 11% | 44% | 0% | 22% |
| … requires a lot of mental effort | 11% | 0% | 44% | 22% | 11% | 0% | 11% |
| … easy to get it to do what I want | 25% | 0% | 13% | 13% | 25% | 13% | 13% |
| Perceived usefulness for self (PU-SELF) | |||||||
| … improves job performance | 38% | 0% | 25% | 13% | 0% | 25% | 0% |
| … increases productivity | 50% | 13% | 13% | 13% | 0% | 0% | 13% |
| … enhances effectiveness in job | 25% | 13% | 25% | 0% | 25% | 0% | 13% |
| …useful in job | 22% | 11% | 11% | 22% | 22% | 0% | 11% |
| Perceived usefulness for patient (PU-PT) | |||||||
| … improves patient care | 20% | 0% | 0% | 0% | 60% | 20% | 0% |
| … reduces likelihood of medication error | 14% | 0% | 43% | 14% | 0% | 14% | 14% |
| … facilitates better patient care decision making | 67% | 0% | 0% | 0% | 0% | 33% | 0% |
| … makes caring for patients easier | 25% | 25% | 0% | 25% | 25% | 0% | 0% |
| Perceived social influence (SI) | |||||||
| … people who influence my behavior want me to use system | 0% | 11% | 11% | 33% | 0% | 0% | 44% |
| … people who are important to me want me to use system | 0% | 11% | 11% | 22% | 11% | 0% | 44% |
| Behavioral intention to use system (BI) | |||||||
| … intend to use system, if I have access | 0% | 13% | 50% | 0% | 0% | 25% | 13% |
| … predict I will use system, if I have access | 0% | 0% | 33% | 17% | 0% | 17% | 33% |
| … would want to use system, if it were up to me | 13% | 13% | 0% | 13% | 13% | 25% | 25% |
| … want to use the system | 25% | 13% | 25% | 0% | 0% | 13% | 25% |
| Satisfaction with system (SATISF) | |||||||
| … satisfied with system | 0% | 13% | 13% | 13% | 25% | 38% | 0% |
| … prefer system to prior process | 33% | 0% | 17% | 0% | 17% | 33% | 0% |
| … dissatisfied with system | 0% | 14% | 43% | 14% | 0% | 14% | 14% |
| … would recommend to a friend at another hospital | 43% | 0% | 14% | 0% | 0% | 43% | 0% |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The Technology Acceptance Model (TAM) was originally developed in the mid-1980s to explain variation in technology use behavior. It was adapted from the Theory of Reasoned Action, a social-psychological theory applicable to a wide range of behaviors. As TRA was updated and evolved into the Theory of Planned Behavior (TPB), similar updates were made to subsequent versions of TAM. Some, though not all, of those updates are reflected in the models tested in this study.
REFERENCES
- 1.Institute of Medicine. Preventing Medication Errors. Washington, DC: National Academies Press; 2007. [Google Scholar]
- 2.Bates DW, Cullen DJ, Laird N, Petersen LA, Small SD, Servi D, et al. Incidence of adverse drug events and potential adverse drug events - implications for prevention. JAMA-Journal of the American Medical Association. 1995;274:29–34. [PubMed] [Google Scholar]
- 3.Karsh B, Wetterneck T, Holden RJ, Rivera-Rodriguez AJ, Faye H, Scanlon MC, et al. Bar-coding in medication administration. In: Yih Y, editor. Handbook of Healthcare Delivery Systems. Boca Raton, FL: CRC Press; 2011. pp. 47-1–47-17. [Google Scholar]
- 4.Oren E, Shaffer ER, Guglielmo BJ. Impact of emerging technologies on medication errors and adverse drug events. Am J Health Syst Pharm. 2003;60:1447–1458. doi: 10.1093/ajhp/60.14.1447. [DOI] [PubMed] [Google Scholar]
- 5.Poon EG, Keohane CA, Yoon CS, Ditmore M, Bane A, Levtzion-Korach O, et al. Effect of bar-code technology on the safety of medication administration. N. Engl. J. Med. 2010;362:1698–1707. doi: 10.1056/NEJMsa0907115. [DOI] [PubMed] [Google Scholar]
- 6.Poon EG, Cina JL, Churchill W, Patel N, Featherstone E, Rothschild JM, et al. Medication dispensing errors and potential adverse drug events before and after implementing bar-code technology in the pharmacy. Annals of Internal Medicine. 2006;145:426–434. doi: 10.7326/0003-4819-145-6-200609190-00006. [DOI] [PubMed] [Google Scholar]
- 7.Nanji KC, Cina J, Patel N, Churchill W, Gandhi TK, Poon EG. Overcoming barriers to the implementation of a pharmacy bar-code scanning system for medication dispensing: A case study. J Am Med Inform Assoc. 2009;16:645–650. doi: 10.1197/jamia.M3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koppel R, Wetterneck TB, Telles JL, Karsh B. Workarounds to barcode medication administration systems: Their occurrences, causes, and threats to patient safety. J Am Med Inform Assoc. 2008;15:408–423. doi: 10.1197/jamia.M2616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miller DF, Fortier CR, Garrison KL. Bar-code medication administration technology: Characterization of high-alert medication triggers and clinician workarounds. Annals of Pharmacotherapy. 2010;45:162–168. doi: 10.1345/aph.1P262. [DOI] [PubMed] [Google Scholar]
- 10.Holden RJ, Karsh B. A theoretical model of health information technology usage behaviour with implications for patient safety. Behav Inf Technol. 2009;28:21–38. [Google Scholar]
- 11.Holden RJ, Karsh B. The Technology Acceptance Model: Its past and its future in health care. J Biomed Inform. 2010;43:159–172. doi: 10.1016/j.jbi.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holden RJ, Brown RL, Alper SJ, Scanlon MC, Patel NR, Karsh B. That's nice, but what does IT do? Evaluating the impact of bar-coded medication administration by measuring changes in the process of care. International Journal of Industrial Ergonomics. 2011;41:370–379. doi: 10.1016/j.ergon.2011.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hurley AC, Bane A, Fotakis S, Duffy ME, Sevigny A, Poon EG, et al. Nurses’ satisfaction with medication administration point-of-care technology. Journal of Nursing Administration. 2007;37:343–349. doi: 10.1097/01.nna.0000285114.60689.02. [DOI] [PubMed] [Google Scholar]
- 14.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quart. 1989;13:319–339. [Google Scholar]
- 15.Venkatesh V, Davis FD. A theoretical extension of the Technology Acceptance Model: Four longitudinal field studies. Manage Sci. 2000;46:186–204. [Google Scholar]
- 16.Venkatesh V, Bala H. Technology acceptance model 3 and a research agenda on interventions. Decision Sciences. 2008;39:273–315. [Google Scholar]
- 17.Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information 438 technology: Toward a unified view. MIS Quart. 2003;27:425–478. [Google Scholar]
- 18.DeLone WH, McLean ER. The DeLone and McLean model of information systems success: A ten-year update. J MIS. 2003;19(4):9–30. [Google Scholar]
- 19.Wixom BH, Todd PA. A theoretical integration of user satisfaction and technology acceptance. Information Systems Research. 2005;16:85–102. [Google Scholar]
- 20.Brown SA, Massey AP, Montoya-Weiss MM, Burkman JR. Do I really have to? User acceptance of mandated technology. European Journal of Information Systems. 2002;11:283–295. [Google Scholar]
- 21.Ajzen I. The Theory of Planned Behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- 22.Holden RJ, Patel NR, Scanlon MC, Shalaby TM, Arnold JM, Karsh B. Effects of mental demands during dispensing on perceived medication safety and employee well being: A study of workload in pediatric hospital pharmacies. Res Soc Admin Pharm. 2010;6:293–306. doi: 10.1016/j.sapharm.2009.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Venkatesh V, Speier C, Morris MG. User acceptance enablers in individual decision making about technology: Toward an integrated model. Decision Sciences. 2002;33(2):297–316. [Google Scholar]
- 24.Venkatesh V, Morris MG, Ackerman PL. A longitudinal field investigation of gender differences in individual technology adoption decision-making processes. Organ Behav Hum Decis Process. 2000;83:33–60. doi: 10.1006/obhd.2000.2896. [DOI] [PubMed] [Google Scholar]
- 25.Venkatesh V, Morris MG. Why don't men ever stop to ask for directions? Gender, social influence, and their role in technology acceptance and usage behavior. MIS Quart. 2000;24:115–139. [Google Scholar]
- 26.McDonald RA, Behson SJ, Seifert CF. Strategies for dealing with measurement error in multiple regression. Journal of the Academy of Business and Economics. 2005;5:80–97. [Google Scholar]
- 27.Hayduk LA. Structural Equations Modeling with LISREL. Baltimore, MD: Johns Hopkins University Press; 1987. [Google Scholar]
- 28.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 2nd ed. Cambridge, MA: Harper & Row; 1989. [Google Scholar]
- 29.Bandalos DL. The effects of item parceling on goodness-of-fit and parameter estimate bias in structural equation modeling. Structural Equation Modeling. 2002;9:78–102. [Google Scholar]
- 30.Bandalos DL, Finney SJ. Item parceling issues in structural equation modeling. In: Marcoulides GA, Schumacker RE, editors. New Developments and Techniques in Structural Equation. Mahawah, NJ: Lawrence Erlbaum; 2001. pp. 269–296. [Google Scholar]
- 31.Patterson ES, Rogers ML, Render ML. Fifteen best practice recommendations for bar-code medication administration in the veterans health administration. Joint Commission Journal on Quality and Safety. 2004;30:355–365. doi: 10.1016/s1549-3741(04)30041-9. [DOI] [PubMed] [Google Scholar]
- 32.American Society of Health-System Pharmacists Foundation. Implementing a Bar-coded Medication Safety Program. 2004 [Google Scholar]
- 33.Hook J, Pearlstein J, Samarth A, Cusack C. Using Barcode Medication Administration to Improve Quality and Safety: Findings from the AHRQ Health IT Portfolio. Rockville, MD: Agency for Healthcare Research and Quality; 2008. AHRQ Publication No. 09-0023-EF. [Google Scholar]
- 34.Patchett JA. Bar-coding: A practical approach to improving medication safety. Bethesda, MD: ASHP Advantage; 2004. [Google Scholar]
- 35.Holden RJ, Alper SJ, Scanlon MC, Murkowski K, Rivera AJ, Karsh B. Challenges and problem-solving strategies during medication management: A study of a pediatric hospital before and after bar-coding; Proceedings of the 2nd International Conference on Healthcare Systems Ergonomics and Patient Safety; Strasbourg, France. 2008. [Google Scholar]
- 36.Stead WW. Rethinking electronic health records to better achieve quality and safety goals. Annual Review of Medicine. 2007;58:35–47. doi: 10.1146/annurev.med.58.061705.144942. [DOI] [PubMed] [Google Scholar]
- 37.Carayon P, Wetterneck TB, Hundt AS, Ozkaynak M, DeSilvey J, Ludwig B, et al. Evaluation of nurse interaction with bar-code medication administration technology in the work environment. J Patient Saf. 2007;3:34–42. [Google Scholar]
- 38.Patterson ES, Cook RI, Render ML. Improving patient safety by identifying side effects from introducing bar-coding in medication administration. J Am Med Inform Assoc. 2002;9:540–553. doi: 10.1197/jamia.M1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Karsh B, Weinger MB, Abbott PA, Wears RL. Health information technology: Fallacies and sober realities. J Am Med Inform Assoc. 2010;17:617–623. doi: 10.1136/jamia.2010.005637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Holden RJ. Physicians’ beliefs about using EMR and CPOE: In pursuit of a contextualized understanding of health IT use behavior. Int J Med Inform. 2010;79:71–80. doi: 10.1016/j.ijmedinf.2009.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Holden RJ. Social and personal normative influences on healthcare professionals to use information technology: Towards a more robust social ergonomics. Theor Issues Ergon Sci. 2011 doi: 10.1080/1463922X.2010.549249. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Goodhue DL, Thompson RL. Task-technology fit and individual performance. MIS Quart. 1995;19:213–236. [Google Scholar]
- 43.Petter S, DeLone WH, McLean ER. Measuring information systems success: Models, dimensions, measures, and interrelationships. European Journal of Information Systems. 2008;17:236–263. [Google Scholar]
- 44.Lapointe L, Rivard S. A multilevel model of resistance to information technology implementation. MIS Quart. 2005;29:461–491. [Google Scholar]
- 45.Lapointe L, Rivard S. Getting physicians to accept new information technology: Insights from case studies. CMAJ. 2006;174:1573–1578. doi: 10.1503/cmaj.050281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Simon SR, Soran CS, Kaushal R, Jenter CA, Volk LA, Burdick E, et al. Physicians' use of key functions in electronic health records from 2005 to 2007: A statewide survey. J Am Med Inform Assoc. 2009;16:465–470. doi: 10.1197/jamia.M3081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Timmons S. Nurses resisting information technology. Nursing Inquiry. 2003;10:257–269. doi: 10.1046/j.1440-1800.2003.00177.x. [DOI] [PubMed] [Google Scholar]
- 48.Spil TAM, Schuring RW, Michel-Verkerke MB. Electronic prescription system: Do the professionals use it? International Journal of Healthcare Technology and Management. 2004;6:32–55. [Google Scholar]
- 49.Sittig DF, Wright A, Osheroff JA, Middleton B, Teich JM, Ash JS, et al. Grand challenges in clinical decision support. J Biomed Inform. 2008;41:387–392. doi: 10.1016/j.jbi.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Aarts J, Doorewaard H, Berg M. Understanding implementation: The case of a computerized physician order entry system in a large Dutch university medical center. J Am Med Inform Assoc. 2004;11:207–216. doi: 10.1197/jamia.M1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Leviss J. H.I.T. or Miss: Lessons Learned from Health Information Technology Implementations. Chicago, IL: AHIMA Press; 2010. [Google Scholar]
- 52.King WR, He J. A meta-analysis of the technology acceptance model. Inf Manag. 2006;43:740–755. [Google Scholar]
- 53.Legris P, Ingham J, Collerette P. Why do people use information technology? A critical review of the technology acceptance model. Inf Manag. 2003;40:191–204. [Google Scholar]
- 54.Yousafzai SY, Foxall GR, Pallister JG. Technology acceptance: a meta-analysis of the TAM: Part 2. Journal of Modelling in Management. 2007;2:281–304. [Google Scholar]
- 55.Yousafzai SY, Foxall GR, Pallister JG. Technology acceptance: a meta-analysis of the TAM: Part 1. Journal of Modelling in Management. 2007;2:251–280. [Google Scholar]
- 56.Lee Y, Kozar KA, Larsen KRT. The technology acceptance model: past, present, and future. Communications of the American Informatics Society. 2003;12:752–780. [Google Scholar]
- 57.Ma Q, Liu L. The technology acceptance model: A meta-analysis of empirical findings. Journal of Organizational and End User Computing. 2004;16:59–72. [Google Scholar]
- 58.Hu PJH, Chau PYK. Physician acceptance of telemedicine technology: An empirical investigation. Topics in Health Information Management. 1999;19:20–35. [PubMed] [Google Scholar]