Abstract
Background
Despite the relatively high prevalence of marijuana use among college students, little information exists regarding health outcomes associated with different use patterns or trajectories.
Methods
Seven annual personal interviews (Years 1–7) were administered to 1,253 individuals, beginning in their first year in college. Growth mixture modeling was used to identify trajectories of marijuana, alcohol, and tobacco use frequency during Years 1–6. Logistic regression was used to evaluate the relationship between marijuana use trajectories and several Year 7 health outcomes, holding constant Year 1 health, demographics, and alcohol and tobacco use trajectories.
Results
Six marijuana use trajectories were identified: Non-Use (71.5%wt of students), Low-Stable (10.0%wt), Late-Increase (4.7%wt), Early-Decline (4.3%wt), College-Peak (5.4%wt), and Chronic (4.2%wt). The six marijuana trajectory groups were not significantly different on Year 1 health-related variables, but differed on all ten Year 7 health outcomes tested, including functional impairment due to injury, illness, or emotional problems; general health rating; psychiatric symptoms; health-related quality of life; and service utilization for physical and mental health problems. Non-Users fared significantly better than most of the marijuana-using trajectory groups on every outcome tested. Chronic and Late-Increase users had the worst health outcomes.
Conclusions
Marijuana use patterns change considerably during college and the post-college period. Marijuana-using students appear to be at risk for adverse health outcomes, especially if they increase or sustain a frequent pattern of use.
Keywords: Cannabis, health outcomes, physical and mental health, health care utilization, longitudinal studies
1. Introduction
Marijuana remains the most commonly used illicit substance worldwide. In the U.S., marijuana use increased significantly among college-attending 18- to 22-year-olds from 17.9% to 20.2% between 2008 to 2009, but remained stable among their non-college-attending counterparts (Substance Abuse and Mental Health Services Administration, 2010). Our own data on a cohort of 1,253 first-year college students indicate that 24.6% of past-year marijuana users met DSM-IV criteria for marijuana abuse or dependence (Caldeira et al., 2008). While marijuana use prevalence is higher in the U.S. than in less affluent countries, young adulthood is typically the peak period of use internationally (Degenhardt and Hall, 2012).
Because marijuana use patterns can vary considerably over time, the need to account for intra-individual variability in the onset, duration, and frequency of marijuana use presents some challenges to researchers. Longitudinal growth mixture modeling is a useful tool for consolidating this variability into coherent trajectories, as has been demonstrated by several researchers in the past decade focusing mainly on adolescence (Brook et al., 2011a; Brook et al., 2011b; Brown et al., 2004; Ellickson et al., 2004; Flory et al., 2004; Juon et al., 2011; Lynne-Landsman et al., 2010; Windle and Wiesner, 2004). Two important studies have described marijuana use trajectories during the transition to young adulthood. Using data from Monitoring the Future, Schulenberg and colleagues (2005) identified five trajectories of marijuana use among 18-to-24 year-olds, namely chronic, decreased, increased, fling, and rare, in addition to a sixth group of abstainers. Their measure of “frequent” marijuana use was, by definition, insensitive to lower levels of marijuana use, which are more prevalent. Nevertheless, with the exception of the fling group, these trajectories were later confirmed in a similar study using the full range of marijuana use frequency (Jackson et al., 2008).
Considerable research has been devoted to understanding the health consequences of marijuana use (see reviews by Hall, 2009; Joy et al., 1999; Mehra et al., 2006; Moore et al., 2007). Acute marijuana intoxication contributes to increased risk for motor vehicle crashes and other accidental injuries. Over the long term, chronic marijuana users are at increased risk for marijuana dependence, psychiatric disorders, psychosis, cognitive deficits, and cancers and other diseases of the respiratory system. While most research has focused on the health effects of chronic, heavy marijuana use, the health consequences of less frequent marijuana use has received sparse attention. One large Australian study documented a dose-response relationship between marijuana use frequency and self-assessed health status, such that when use was categorized as past-year versus past-week, past-year use influenced health status about half as strongly as past-week use (Williams and Skeels, 2006). Even controlling for tobacco use, weekly marijuana use had about the same deleterious effect on health status as daily tobacco smoking.
Rather than focusing on marijuana involvement retrospectively or at a single time point, a more complete picture of marijuana’s health consequences can be obtained by investigating marijuana use trajectories. Several studies have linked marijuana use trajectory group membership in adolescence to adverse health outcomes in young or middle adulthood. In the largest of these studies (N=5,833), Ellickson et al. (2004) found that marijuana abstainers had better health ratings and life satisfaction at age 29, compared to all four of the marijuana-using trajectory groups they identified (i.e., early-high, stable-light, steady-increasers, occasional-light), and better mental health than two of the marijuana-using trajectory groups. In this and other studies, the worst health outcomes are generally associated with a trajectory characterized by early onset of frequent use. In smaller studies of ethnically diverse samples, marijuana trajectory group membership predicted significant differences in depressive and anxiety symptoms at age 29 (Brook et al., 2011a) and major depressive and substance use disorders at age 42 (Juon et al., 2011) and age 21 (Lynne-Landsman et al., 2010). On the other hand, some studies have failed to find a significant association between marijuana use trajectories and mental health outcomes in the earliest stages of young adulthood (i.e., ages 19 to 23) including psychopathology (Brown et al., 2004), depression, anxiety (Windle and Wiesner, 2004), and internalizing disorders (Flory et al., 2004).
Because marijuana use typically co-occurs with alcohol and tobacco use, its health effects are difficult to disentangle from use of the latter two substances. Jackson and colleagues (2008) demonstrated considerable overlap between the trajectories of alcohol, tobacco, and marijuana use in young adulthood, and emphasized the importance of common vulnerability to all three forms of substance use. Williams and Skeels (2006) demonstrated that failure to account for tobacco use resulted in a significantly inflated estimate of the effect of marijuana use on health status. For example, when cigarette smoking was not taken into account, weekly marijuana users were 46% less likely than non-users to report excellent or good health; however, after accounting for cigarette smoking, the effect of weekly marijuana use was considerably smaller (18%).
Several methodological limitations exist in prior studies of marijuana use trajectories. First, the timing between marijuana use observations has often been lengthy (i.e., several years); shorter intervals are needed to detect rapid changes in marijuana use patterns. Second, most studies have focused on marijuana use during adolescence, with few if any measures during the transition to young adulthood (i.e., ages 18 to 24), when changes in marijuana use are likely to continue occurring. Even fewer studies have focused on college students, an important segment of the young-adult population with high rates of drug involvement. Third, most studies have relied on categorical or ordinal measures of marijuana use, which have limited sensitivity to low levels of marijuana use. Finally, few studies have adequately controlled for the effects of alcohol and tobacco use, which are likely to contribute to health outcomes.
This study sought to overcome some of these limitations by taking advantage of an annual repeated-measures design spanning seven years, and using scale and count measures to capture the full range of variability in marijuana use frequency and health outcomes. We had three aims: (1) model the six-year trajectories of marijuana, alcohol, and tobacco use frequency; (2) compare the baseline (Y1) characteristics of individuals within each marijuana trajectory group; and (3) examine the prospective relationship between marijuana trajectory group membership and health-related outcomes six years later (Year 7: Y7), holding constant alcohol and tobacco use trajectories as well as Y1 health variables. A wide range of post-college health outcomes were examined, encompassing physical health, mental health, health service utilization, and quality of life.
2. Methods
2.1. Study design
Participants were recruited as part of the College Life Study at one large, public university in the mid-Atlantic region of the U.S. (Arria et al., 2008; Vincent et al., in press). After screening 82% of the entire incoming class of first-year, first-time students ages 17 to 19 during the summer prior to college entry in 2004 (N=3,401), we selected a sample for longitudinal study, oversampling students who used illicit drugs (including nonmedical prescription drug use) at least once prior to college. The two-hour baseline assessment (Y1) consisted of a personal interview and self-administered surveys on a variety of health-related behaviors and personal characteristics, and was administered on a rolling basis throughout the first year of college (N=1,253; response rate=86.5%). Six annual follow-up assessments (Y2–Y7) were similar in format and content. Annual follow-up rates ranged from 91.1% in Y2 (n=1,142) to 78.4% in Y7 (n=982). Eligibility remained open to all Y1 participants, regardless of continued college enrollment. Interviewers were trained extensively in human subject protections. Participants provided written informed consent and were paid for each assessment. The study was approved by the university’s IRB. A federal Certificate of Confidentiality was obtained.
2.2. Participants
Participants were 1,253 individuals (608 men, 915 white) who matriculated in the fall of 2004. They were ages 17 to 20, inclusive, at Y1 (Table 1). Analyses on Y7 health outcomes were restricted to the 973 individuals (77.7% of original sample) who participated in the Y7 assessment and had complete data on demographic covariates. Compared with the inclusion sample, the 280 excluded participants were more likely to be male (61.1% vs. 44.9%, p<0.001) and were slightly older (18.3 vs. 18.2 at Y1, p<0.001), but were similar with respect to race/ethnicity and neighborhood income. By Y7, 96% of the inclusion sample had graduated from college.
Table 1.
Comparison of baseline (Y1) sample characteristics, by marijuana trajectory group membership.
| All (N=1,253) | Non-Use (n=766) | Low-Stable (n=154) | Early-Decline (n=81) | Late-Increase (n=74) | College-Peak (n=100) | Chronic (n=78) | |
|---|---|---|---|---|---|---|---|
| % of sample | 100.0 | 61.1 | 12.3 | 6.5 | 5.9 | 8.0 | 6.2 |
| %wt of target populationa | 100.0 | 71.5 | 10.0 | 4.3 | 4.7 | 5.4 | 4.2 |
|
| |||||||
| % Male** | 48.5 | 41.9 | 48.1 | 58.0 | 68.9 | 62.0 | 67.9 |
| % White** | 73.1 | 68.9 | 75.3 | 85.2 | 77.0 | 80.8 | 83.3 |
| % Hispanic | 4.7 | 4.8 | 6.5 | 4.9 | 4.1 | 3.1 | 2.6 |
| Mean (SD) neighborhood incomeb, * | 7.3 (3.4) | 7.1 (3.3) | 7.4 (3.3) | 7.5 (3.4) | 7.5 (3.4) | 7.5 (3.7) | 8.5 (4.1) |
| Mean (SD) Age | 18.2 (.5) | 18.2 (.5) | 18.2 (.5) | 18.2 (.5) | 18.2 (.5) | 18.2 (.5) | 18.2 (.5) |
| Mean (SD) GHQ-12 score | 9.6 (4.2) | 9.7 (4.1) | 9.8 (4.3) | 9.8 (4.8) | 9.1 (3.4) | 9.3 (4.5) | 10.0 (4.9) |
| Mean (SD) BDI score | 5.3 (5.2) | 5.4 (5.3) | 5.2 (4.8) | 5.6 (5.4) | 4.3 (4.0) | 5.0 (5.1) | 6.2 (5.9) |
| Mean (SD) BAI score | 7.6 (7.1) | 7.7 (7.2) | 7.0 (5.6) | 8.9 (8.5) | 7.2 (8.0) | 6.1 (6.7) | 8.8 (7.2) |
| % Smoked cigarettes in the past month** | 24.0 | 14.0 | 24.7 | 32.1 | 35.1 | 57.0 | 59.7 |
| % Met DSM-IV criteria for alcohol dependence** | 14.7 | 9.8 | 19.6 | 25.9 | 16.2 | 24.2 | 26.9 |
| Age at onset of marijuana use** | |||||||
| % <15 | 18.5 | 9.1 | 29.2 | 40.8 | 20.0 | 40.4 | 58.8 |
| % 15–17 | 19.2 | 12.5 | 22.5 | 44.9 | 40.0 | 40.4 | 29.4 |
| % ≥ 18 | 62.3 | 78.4 | 48.3 | 14.3 | 40.0 | 19.2 | 11.8 |
Note: GHQ-12=General Health Questionnaire. BDI=Beck Depression Inventory. BAI=Beck Anxiety Inventory.
Weighted percent (%wt) of target population is statistically adjusted to correct for purposive sampling design.
The mean adjusted gross income for each participant’s home ZIP code during their last year in high school, measured in ten thousands.
p<.05;
p<.001
2.3. Measures
2.3.1. Alcohol, tobacco, and marijuana use
Past-month frequencies of using marijuana and smoking tobacco cigarettes were captured annually (range=0 to 30 days), as was past-year frequency of alcohol use (range=0 to 365 days). Age at onset of marijuana use was also measured. Alcohol dependence was assessed in Y1 using a series of standard interview questions (Substance Abuse and Mental Health Services Administration, 2003) that map to the DSM-IV criteria for alcohol abuse and dependence (American Psychiatric Association, 1994).
2.3.2. Psychiatric symptoms
Interviewers administered the 12-item General Health Questionnaire (GHQ-12) annually. Scoring was via the Likert (0 to 3) method, which sums the 12 items for a possible range of 0 to 36 (Goldberg and Williams, 1988). Also annually, participants self-administered the Beck Depression Inventory (BDI; Beck et al., 1979) and Beck Anxiety Inventory (BAI; Beck and Steer, 1990). Reliability was acceptable for all three measures (α≥0.78).
2.3.3. Health service utilization
In Y7 participants were asked two questions regarding how many times they visited a health professional during the past year for (1) problems with their physical health and (2) problems with their “emotions, nerves, or mental health.”
2.3.4. Functional impairment
In Y7 participants were asked three separate questions regarding how many days during the past year their usual activities were limited due to (1) “an illness or physical condition”, (2) “an emotional problem or trouble with your nerves”, and (3) “an accident or injury.”
2.3.5. Health-related quality of life
In Y7 participants completed the abbreviated version of the World Health Organization Quality of Life (WHOQOL-BREF) scale, yielding two subscale scores representing QOL-Physical (7 items) and QOL-Psychological (6 items). Raw scores were transformed to a 0 to 100 scale using standard methods (Murphy et al., 2000). Higher scores indicate better quality of life. Reliability was acceptable (α≥0.75).
2.3.6. Demographics
Gender was coded by the interviewer in Y1. Race and ethnicity were self-reported in Y3, and later dichotomized as white versus non-white and Hispanic versus non-Hispanic, respectively. As a proxy for socioeconomic status, we abstracted from publicly available data the mean adjusted gross income for each participant’s ZIP code during their last year of high school (MelissaDATA, 2003). Age at interview was computed from date of birth.
2.4. Analytic strategy
As noted above, we purposively oversampled students who used illicit or nonmedical prescription drugs at least once prior to college. We later computed sampling weights to correct for the sampling design, so that prevalence estimates would generalize to the original target population of incoming first-year students (%wt). Aside from prevalence estimates for trajectory group membership, all other analyses were performed on unweighted data.
For the first aim of identifying distinct trajectories of marijuana use, we used PROC TRAJ (Jones et al., 2001) in SAS (SAS Institute Inc., 2008) to estimate a multivariate mixture model based on the first six annual repeated measures of past-month marijuana use frequency, assuming a zero-inflated Poisson distribution for marijuana use frequency, because we expected a large proportion of zero values (i.e., non-users) in the population. Y7 data were excluded from trajectories to preserve the temporality between trajectories (Y1–Y6) and outcomes (Y7). We allowed for up to a third-degree polynomial to define rates of change over time and entered assessment year as the time variable (i.e., Y1–Y6). Similar procedures were used for tobacco and alcohol use frequency. Models were tested for one- to seven-group solutions. Selection of the best model for each substance was based on evaluation of both the Bayesian Information Criterion (BIC) and the size and interpretability of the resulting trajectory groups. Thus, models with a smaller BIC were not always preferred if they resulted in the addition of very small trajectory groups (<5% of sample).
For the second aim, Y1 differences between the marijuana trajectory groups were evaluated using χ2 tests of independence and oneway ANOVAs (α=0.05).
For the third aim, multiple regression was used to predict ten health-related outcomes in Y7 (i.e., GHQ-12, provider visits for physical and mental health, illness-related impairment days, emotional-related impairment days, injury-related impairment days, BDI, BAI, QOL-Physical, and QOL-Psychological) on the basis of marijuana trajectory group membership, holding constant demographics and alcohol and tobacco trajectory group membership. A normal distribution was assumed for scale scores (GHQ-12, BDI, BAI, QOL); the remaining outcomes were all count variables and therefore modeled assuming a Poisson distribution. To account for possible pre-existing differences in health, Y1 values of GHQ-12, BDI, and BAI were held constant in the respective models predicting Y7 GHQ-12, BDI, and BAI. For the remaining outcomes, comparable Y1 measures were not available; therefore, Y1 GHQ-12 was held constant for the models concerning provider visits, impairment days, and QOL.
3. Results
3.1. Marijuana use trajectories
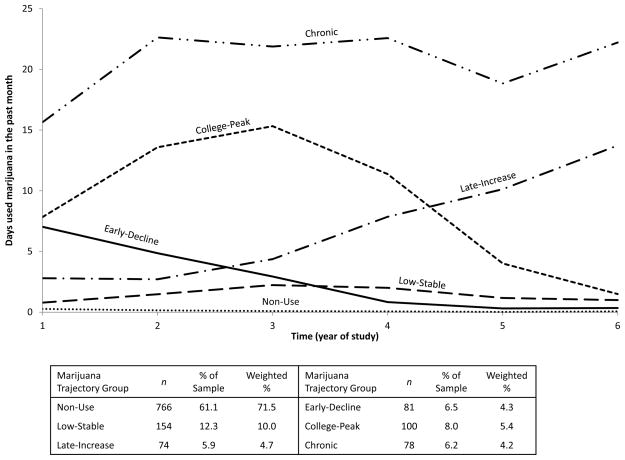
A six-group solution was selected as the best fit to the marijuana-use frequency data (Figure 1 and Table 2). The largest marijuana trajectory group reflected consistently negligible use (or non-use) with means at or near zero (Non-Use, n=766, 61.1% of sample). The Low-Stable group maintained low levels of marijuana use, below three days/month on average (n=154, 12.3%). A third group entered college with similarly low levels of marijuana use (three days/month) but then steadily increased starting in Y3 (Late-Increase, n=74, 5.9%). Two groups entered college with moderate levels of marijuana use (7–8 days/month), one of which declined steadily through Y6 (Early-Decline, n=81, 6.5%), whereas the other exhibited a more delayed decline after peaking in Y3 (College-Peak, n=100, 8.0%). The sixth group, deemed Chronic users, maintained means consistently greater than 15 days/month (n=78, 6.2%). Mean probabilities of respective group membership were high in all six groups (0.90 to 0.99). Evaluation of the linear, quadratic, and cubic parameters within each trajectory group revealed that marijuana use frequency changed significantly over time in all six trajectory groups. Nearly every parameter was statistically significant, with the exception of the linear effect for the Low-Stable trajectory, quadratic effect for the Early-Decline and Late-Increase trajectories, and cubic effect for the College-Peak trajectory. After statistically adjusting for the purposive sampling design, we estimate that the distribution of marijuana trajectory group membership among all first-year students was: 71.5%wt Non-Use, 10.0%wt Low-Stable, 4.7%wt Late-Increase, 4.3%wt Early-Decline, 5.4%wt College-Peak, and 4.2%wt Chronic. The seven-group solution had a smaller BIC than the six-group solution, but was not preferred because the seventh group was quite small (<5% of sample) and conceptually similar to the Early-Decline trajectory, albeit at a higher level of intensity.
Figure 1.
Marijuana use trajectories (N=1,253).
Table 2.
Bayesian Information Criteria (BIC) scores for trajectory models.
| Number of groups in model | Marijuana, past-month frequency | Alcohol, past-year frequency | Tobacco, past-month frequency |
|---|---|---|---|
| 1 | −33591.73 | −99093.88a | −39915.63 |
| 2 | −16139.45 | −99080.69a | −16697.66 |
| 3 | −13811.07 | −99129.07 | −14131.74 |
| 4 | −12962.22 | −91921.68 | −12996.56 |
| 5 | −12128.88 | −85891.85 | −12217.96 |
| 6 | −11879.60 | −80330.23 | −11842.44 |
| 7 | −11591.99 | −76589.78 | −11491.27 |
BIC is reported despite model convergence problems.
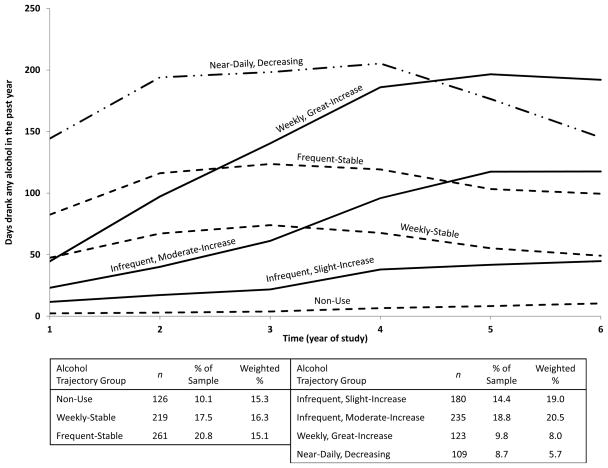
3.2. Alcohol use trajectories
A seven-group solution emerged as the best fit to the data on past-year drinking frequency (Figure 2 and Table 2), based on the BIC and the absence of any small groups. Three of the trajectory groups exhibited minimal change over the six years (Non-Use, Weekly-Stable, and Frequent-Stable), three exhibited substantial increases (Infrequent, Slight-Increase; Infrequent, Moderate-Increase; and Weekly, Great-Increase) and one significantly reduced its drinking frequency (Near-Daily, Decreasing). Unweighted and weighted distributions of alcohol use trajectories are presented in Figure 2. With the sole exception of the quadratic effect in the Non-Use group, all effects tested were significant (p<0.01). Mean probabilities of respective group membership were high (0.97 to 0.99).
Figure 2.
Alcohol use trajectories (N=1,253).
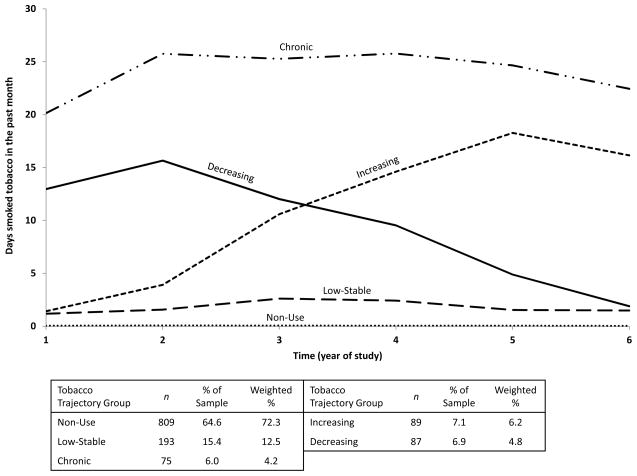
3.3. Tobacco use trajectories
A five-group solution provided the best fit to the tobacco use data (Figure 3 and Table 2). The six-group solution yielded a smaller BIC, but without introducing a new trajectory that was conceptually distinct (i.e., a second increasing trajectory with smaller slope and peak). The seven-group solution yielded an even smaller BIC, but with two very small trajectory groups (<5% of sample). The largest trajectory group had means consistently at or near 0 (Non-Use), two exhibited relatively stable patterns (Low-Stable and Chronic), and two were transitioning to higher and lower smoking levels (Increasing and Decreasing). See Figure 3 for unweighted and weighted distributions. Linear effects were significant in the Decreasing and Increasing groups only (p<0.001), quadratic effects were significant in all five groups (p<0.05), and a cubic effect was significant in the Chronic group only (p<0.05). Mean probabilities of respective group membership were high (0.95 to 0.99).
Figure 3.
Tobacco use trajectories (N=1,253).
3.4. Comparison of Y1 characteristics
Males and whites were generally overrepresented in the more frequent marijuana-using groups, compared with the Non-Use group (Table 1). On average, Chronic marijuana users came from significantly higher-income neighborhoods than did Non-Users. Tobacco smoking, alcohol dependence, and early onset of marijuana use (i.e., before age 15) were all significantly more prevalent among the marijuana-using groups relative to Non-Users, and highest among Chronic users. No significant differences existed with respect to ethnicity, age, or scores on GHQ-12, BDI, and BAI (all ps>0.05).
3.5. Multiple regression predicting Y7 health outcomes
Marijuana trajectory group membership significantly predicted all ten of the Y7 health outcomes tested (Table 3), holding constant demographics, Y1 characteristics, and alcohol and tobacco trajectory group membership. In general, the Chronic group fared the worst on all three of the psychiatric symptom measures (GHQ-12, BDI, and BAI) as well as both QOL-Physical and QOL-Psychological scores. However, the Late-Increase group had the highest levels of service utilization for both physical and mental health, and the greatest number of impairment days due to illness or emotions.
Table 3.
Results of multiple regression predicting Year 7 health outcomes on the basis of Years 1 through 6 marijuana use trajectory membership, holding constant alcohol and tobacco use trajectory membership (N=973).
| Trajectory Group | GHQ-12 Score† | Physical Health Visits† | Mental Health Visits† | Impairment Days: Illness† | Impairment Days: Emotions† | Impairment Days: Injury† | BDI Score†† | BAI Score‡ | Quality of Life: Physical† | Quality of Life: Psychological† |
|---|---|---|---|---|---|---|---|---|---|---|
| Non-Use | 8.83a | 1.44a,b | .75a | 1.83a | .50a | 2.40a | 2.97a | 4.05a | 84.08a | 74.09a |
| Low-Stable | 8.82a | 1.53a,b | 1.32b | 1.84a | .59a | 4.43b | 3.09a | 4.28a | 83.73b | 72.13b |
| Early-Decline | 8.88b | 1.16a,c | 2.04c | 2.02a | 1.17b | 3.99b | 2.70a,b | 5.10b | 83.06c | 72.48b |
| Late-Increase | 8.69a | 2.56d | 3.44d | 3.93b | 2.05c | 3.98b | 3.60c | 5.64b,d | 81.89d | 70.88c |
| College-Peak | 8.54a | .85c | .74a | 2.76c | 1.57b,c | 2.50a | 2.47b | 3.02c | 85.99e | 75.49d |
| Chronic | 10.21b | 1.86b,d | 1.97c | 2.96c | 1.28b | 3.87b | 4.56d | 5.96d | 79.11f | 67.98e |
Note: Results computed as estimated marginal means for each outcome variable. Variables for alcohol and tobacco use trajectory group membership were held constant in all models. GHQ-12=General Health Questionnaire. BDI=Beck Depression Inventory. BAI=Beck Anxiety Inventory.
Y1 GHQ-12 score, sex, race, ethnicity, and income were held constant.
Y1 BDI score, sex, race, ethnicity, and income were held constant.
Y1 BAI score, sex, race, ethnicity, and income were held constant.
Cells sharing the same superscripted letter within a column are not significantly different (p>.05).
3.6. Rationale for presentation of multiple comparisons
All possible between-group comparisons were evaluated for each health outcome (see Table 3); however, we focus herein on four specific sets of comparisons. Our approach was essentially exploratory, but was predicated on a hypothesized dose-response relationship between marijuana use frequency over time and severity of health outcomes. First, each marijuana-using trajectory group was compared with the Non-Use group, to evaluate which groups, if any, experienced adverse health outcomes. Second, we compared the Late-Increase and Chronic groups because both groups reached high levels of marijuana use in Y6, and therefore any differences in health outcomes might be attributable to differences in duration of frequent use. Third, we compared the College-Peak and Chronic groups because they both maintained relatively high levels of marijuana use in Y1–4, when most participants were still in college. Fourth, we compared the College-Peak and Early-Decline groups, because their trajectories began and ended at very similar marijuana use levels, although the College-Peak group temporarily attained much higher levels during Y2–4. The third and fourth sets of comparisons were thought to have relevance to understanding which health effects—if any—might be more enduring versus time-limited following a period of high-frequency marijuana use.
3.7. Comparisons with Non-Use group
Compared with the Non-Use group, the Chronic group fared significantly worse on nine of the ten outcomes tested (all but physical health visits), as did the Late-Increase group (all but GHQ-12). Despite having cut back on their marijuana use, the Early-Decline group fared significantly worse than the Non-Use group on seven outcomes (GHQ-12, mental health visits, emotion and injury-related impairment, BAI, and both QOL scores). The Low-Stable group had the fewest significant differences from the Non-Use group, faring worse on four outcomes (mental health visits, injury-related impairment, and both QOL measures). The College-Peak group was the only group that fared significantly better than Non-Users on any measure—namely, they had fewer physical health visits, lower scores on the BDI and BAI, and higher QOL-Physical and QOL-Psychological scores. On the other hand, they experienced significantly more illness- and emotion-related impairment than Non-Users.
3.8. Comparisons between Late-Increase and Chronic groups
Compared to Late-Increasers, Chronic users scored significantly worse on mean GHQ-12, BDI, and both QOL measures (Table 3). However, Chronic users experienced significantly fewer impairment days related to illness and emotional problems, and fewer visits for mental health problems. The two groups were not significantly different on mean BAI score, provider visits for physical health problems, or injury-related impairment days.
3.9. Comparisons between College-Peak and Chronic groups
Compared with the College-Peak group, the Chronic group scored significantly worse on the GHQ-12, BDI, BAI, and both QOL measures. They also accessed health providers more often for physical and mental health problems, and experienced more injuries. However, they were not significantly different on impairment days related to illness or emotions.
3.10. Comparisons between College-Peak and Early-Decline groups
Compared with the College-Peak group, the Early-Decline group scored significantly worse on the GHQ-12, BAI, and both QOL measures, and had more mental health visits and more injury-related impairment. Conversely, the College-Peak group experienced significantly more illness-related impairment days. The two groups were similar with respect to physical health visits, emotion-related impairment, and BDI score.
4. Discussion
In this longitudinal study of young adults originally recruited as college students, six distinct marijuana use trajectories were observed during a six-year period. A Low-Stable trajectory was the most prevalent (10.0%wt) after Non-Use (71.5%wt), while smaller proportions had moderately high use levels that were time-limited (5.4%wt College-Peak, 4.3%wt Early-Decline). Two groups exhibited high levels of use that were sustained in the post-college years: one in which a frequent pattern of use built up gradually during college (4.7%wt Late-Increase), and the other in which a frequent use pattern had already been well-established by college entry (4.2%wt Chronic). The trajectories we observed were consistent with other studies that spanned longer time frames (Brook et al., 2011b; Ellickson et al., 2004; Jackson et al., 2008), including the “fling” group identified in only one prior study (Schulenberg et al., 2005).
The six trajectory groups did not differ significantly on health-related variables in Y1, but did differ on all ten post-college health outcomes tested, including both mental and physical health problems. These differences persisted even after holding constant Y1 health measures and demographics, as well as the concurrent trajectories of alcohol and tobacco use. Individuals who consistently abstained from marijuana use fared significantly better than all five marijuana-using trajectories, including the Low-Stable group. Although the present findings are in need of confirmation, they add to a growing body of literature regarding the potential adverse effects of marijuana use on adolescent and young adult health.
By Y7, individuals in the Early-Decline group still had more psychiatric symptoms, mental health visits, emotion- and injury-related impairment, and poorer quality of life relative to Non-Users, despite having maintained low levels of marijuana use for three years. This is intriguing because, unlike the Late-Increase and Chronic groups, the period of frequent marijuana use was not proximal to the health outcomes measured. A similar finding was recently reported by Brook et al. (2011a), whereby “Maturing-Out” users were more likely to experience anxiety, but not depression, than the “Non/Low-Use” group. By contrast, Ellickson et al. (2004) found that “Early-High” users were indistinguishable from abstainers with respect to mental health by age 29. This discrepancy might be due to methodological differences in our assessment timing or statistical modeling approach, but we believe our use of scale variables for both marijuana use and health outcomes might have improved our ability to detect significant differences.
Individuals in the Late-Increase and Chronic groups both had significantly worse depressive and anxiety symptoms in Y7 in comparison to most of the other trajectory groups. Brook et al. (2011a) demonstrated a similar association in their “late onset” and “chronic” marijuana-using trajectory groups. The fact that this association held true even among the Late-Increase group—individuals for whom the onset of a frequent use pattern (i.e., more than four times/month) apparently occurred well into their college years—is intriguing and warrants further study. Our finding adds to prior evidence that late-onset marijuana use (i.e., after age 20)—and not just early-onset use in adolescence—is associated with increased risk for major depression in early and middle adulthood (Brook et al., 2011a; Juon et al., 2011). The emergence of a distinct trajectory of marijuana use that increased steadily beginning in Y3 of college underscores the importance of this developmental period for the onset of co-morbid problems with marijuana and depression. Epidemiologic evidence that the period of risk for initiating marijuana use appears to be extending longer into adulthood (Degenhardt et al., 2008) lends further urgency to the need for a research agenda focused on understanding the link between late-onset marijuana use and depression.
The fact that the Late-Increase group fared significantly worse than nearly all other groups on most of the outcomes we tested (i.e., more psychiatric symptoms, impairment days, and provider visits) suggests that their abrupt increase in marijuana use in mid-college might have coincided with the onset of a significant stressful life event or an emerging psychiatric disorder, although our research design cannot clarify the temporal or causal nature of this association. This finding contrasts with Windle and Weisner’s (2004) finding that adolescents who increased their marijuana use in high school had significantly more depressive symptoms at Y1 but, by young adulthood, were indistinguishable from other trajectory groups. This discrepancy might be attributable to methodological differences; for example, the five-year assessment intervals in Windle and Weisner’s study might not have been as sensitive to changes in marijuana use patterns as our annual assessments.
4.1. Limitations
Results must be interpreted in light of certain limitations. Many of the observed differences in health outcomes were modest, albeit significantly so. It is possible that young adults might underreport their symptoms in survey research, and clinical exams might have revealed more significant problems. However, in the absence of clinical health assessments, we cannot draw conclusions about the clinical severity of health effects observed, nor does this study inform about the longer-term effects of marijuana use trajectories. Whether or not the observed marijuana-related differences in health outcomes will attenuate, stabilize, or increase over time is unknown. Moreover, it is important to acknowledge that the observed associations between health outcomes and marijuana trajectory group membership do not necessarily point to a causal explanation. A number of unmeasured third variables could account for this association, such as an underlying propensity for behaviors and lifestyles that do not promote optimal health. One such example is the inverse association between marijuana use and physical activity (Delisle et al., 2010). Also, given prior evidence that adolescents with physical disabilities and chronic health problems are at increased risk for using marijuana (Jones and Lollar, 2008), it is plausible that in some cases, health problems preceded or even contributed to the development of increasing or chronic trajectories of use. Other evidence points to the importance of employment and life events as possible confounds that should be accounted for in subsequent analyses (Swain et al., in press).
Methodological limitations include the fact that participants were ascertained from one university; therefore, generalizability of results to other populations is unknown. Because our sample was predominantly White, we cannot say how the observed associations between trajectory group membership and health outcomes might have differed in other ethnic/racial groups. As in all self-report studies, data are subject to bias related to social desirability and recall. To minimize recall bias, we focused our analyses on past-month marijuana use, which might not be representative of marijuana use occurring at other times of the year, despite its strong correlation with past-year use in every assessment year (r≥0.83).
4.2. Strengths
The ability to control for concurrent trajectories of alcohol and tobacco use as possible confounds in the relationship between marijuana use and health outcomes is a major strength of the study. This is advantageous given that these trajectories tend to covary (Gray et al., 2011; Jackson et al., 2008). This study extends prior research on marijuana use trajectories by focusing on the transition from college to early adulthood (modal ages 18 to 24), a previously neglected developmental stage. Also, by using scale and count measures to take advantage of the full range of marijuana use frequency, psychiatric symptoms, and other health outcomes, this study advances prior research that has relied on categorical measures of disorder or “frequent” use. Moreover, whereas considerable research has focused on alcohol-related problems in college students (Wu et al., 2007), this study highlights the public health significance of their marijuana use, which has received little attention.
4.3. Implications
This study contributes greatly needed information about the potential consequences of marijuana use, which could be helpful in designing prevention initiatives. The finding that modest differences in health outcomes among marijuana-using groups were already apparent in young adulthood underscores the importance of identifying and intervening with marijuana-using students early in college. College settings might provide unique opportunities for confidential screening before problems escalate. Computerized and paper-and-pencil drug screening questionnaires have been shown to be highly acceptable to adolescents in primary care settings (Knight et al., 2007) and should be evaluated in college health centers. Further study is needed to evaluate the effectiveness of interventions aimed at reducing alcohol and other drug use among college students. Chronic, heavy marijuana use is thought to contribute to a number of more severe health outcomes over the long term, including lung and brain cancers as well as fatal traffic accidents (Calabria et al., 2010). Long-range follow-up studies are needed to confirm the present findings, and must account for other forms of substance use (Mehra et al., 2006). Further study is also needed to understand the interrelationships between age at onset of marijuana use and subsequent marijuana use trajectories in young adulthood. This study demonstrates one promising method for disentangling the effects of marijuana use from those of tobacco and alcohol.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. American Psychiatric Press; Washington, DC: 1994. [Google Scholar]
- Arria AM, Caldeira KM, O’Grady KE, Vincent KB, Fitzelle DB, Johnson EP, Wish ED. Drug exposure opportunities and use patterns among college students: Results of a longitudinal prospective cohort study. Subst Abus. 2008;29:19–38. doi: 10.1080/08897070802418451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. Australian And New Zealand Journal Of Psychiatry. 1979;36:272–275. doi: 10.1046/j.1440-1614.2002.t01-4-01015.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Beck Anxiety Inventory: Manual. The Psychological Corporation, Harcourt Brace Jovanovich, Inc; San Antonio, TX: 1990. [Google Scholar]
- Brook JS, Lee JY, Brown EN, Finch SJ, Brook DW. Developmental trajectories of marijuana use from adolescence to adulthood: Personality and social role outcomes. Psychol Rep. 2011a;108:339–357. doi: 10.2466/10.18.PR0.108.2.339-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook JS, Zhang C, Brook DW. Developmental trajectories of marijuana use from adolescence to adulthood: Personal predictors. Arch Pediatr Adolesc Med. 2011b;165:55–60. doi: 10.1001/archpediatrics.2010.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TL, Flory K, Lynam DR, Leukefeld C, Clayton RR. Comparing the developmental trajectories of marijuana use of African American and Caucasian adolescents: Patterns, antecedents, and consequences. Exp Clin Psychopharmacol. 2004;12:47–56. doi: 10.1037/1064-1297.12.1.47. [DOI] [PubMed] [Google Scholar]
- Calabria B, Degenhardt L, Hall W, Lynskey M. Does cannabis use increase the risk of death? Systematic review of epidemiological evidence on adverse effects of cannabis use. Drug Alcohol Rev. 2010;29:318–330. doi: 10.1111/j.1465-3362.2009.00149.x. [DOI] [PubMed] [Google Scholar]
- Caldeira KM, Arria AM, O’Grady KE, Vincent KB, Wish ED. The occurrence of cannabis use disorders and other cannabis-related problems among first-year college students. Addict Behav. 2008;33:397–411. doi: 10.1016/j.addbeh.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Chiu WT, Sampson N, Kessler RC, Anthony JC, Angermeyer M, Bruffaerts R, Girolamo Gd, Gureje O, Huang Y, Karam A, Kostyuchenko S, Lepine JP, Mora MEM, Neumark Y, Ormel JH, Pinto-Meza A, Posada-Villa J, Stein DJ, Takeshima T, Wells JE. Toward a global view of alcohol, tobacco, cannabis, and cocaine use: Findings from the WHO World Mental Health Surveys. PLoS Medicine. 2008;5:e141–e141. doi: 10.1371/journal.pmed.0050141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet. 2012;379:55–70. doi: 10.1016/S0140-6736(11)61138-0. [DOI] [PubMed] [Google Scholar]
- Delisle TT, Werch CE, Wong AH, Bian H, Weiler R. Relationship between frequency and intensity of physical activity and health behaviors of adolescents. J Sch Health. 2010;80:134–140. doi: 10.1111/j.1746-1561.2009.00477.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellickson PL, Martino SC, Collins RL. Marijuana use from adolescence to young adulthood: Multiple developmental trajectories and their associated outcomes. Health Psychol. 2004;23:299–307. doi: 10.1037/0278-6133.23.3.299. [DOI] [PubMed] [Google Scholar]
- Flory K, Lynam D, Milich R, Leukefeld C, Clayton R. Early adolescent through young adult alcohol and marijuana use trajectories: Early predictors, young adult outcomes, and predictive utility. Dev Psychopathol. 2004;16:193–213. doi: 10.1017/s0954579404044475. [DOI] [PubMed] [Google Scholar]
- Goldberg D, Williams P. A user’s guide to the General Health Questionnaire. NFER-NELSON; Windsor, Berkshire: 1988. [Google Scholar]
- Gray KM, Riggs PD, Min S-J, Mikulich-Gilbertson SK, Bandyopadhyay D, Winhusen T. Cigarette and cannabis use trajectories among adolescents in treatment for attentiondeficit/ hyperactivity disorder and substance use disorders. Drug Alcohol Depend. 2011;117:242–247. doi: 10.1016/j.drugalcdep.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W. The adverse health effects of cannabis use: What are they, and what are their implications for policy? Int J Drug Policy. 2009;20:458–466. doi: 10.1016/j.drugpo.2009.02.013. [DOI] [PubMed] [Google Scholar]
- Jackson KM, Sher KJ, Schulenberg JE. Conjoint developmental trajectories of young adult substance use. Alcohol Clin Exp Res. 2008;32:723–737. doi: 10.1111/j.1530-0277.2008.00643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating development trajectories. Sociol Methods Res. 2001;29:374–393. [Google Scholar]
- Jones SE, Lollar DJ. Relationship between physical disabilities or long-term health problems and health risk behaviors or conditions among US high school students. J Sch Health. 2008;78:252–257. doi: 10.1111/j.1746-1561.2008.00297.x. [DOI] [PubMed] [Google Scholar]
- Joy JE, Watson SJ, Benson JA. Marijuana and medicine: Assessing the science base. National Academy Press; Washington, DC: 1999. [PubMed] [Google Scholar]
- Juon H-S, Fothergill K, Green KM, Doherty EE, Ensminger M. Antecedents and consequences of marijuana use trajectories over the life course in an African American population. Drug Alcohol Depend. 2011;118:216–223. doi: 10.1016/j.drugalcdep.2011.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight JR, Harris SK, Sherritt L, Hook SV, Lawrence N, Brooks T, Carey P, Kossack R, Kulig J. Adolescents’ preferences for substance abuse screening in primary care practice. Subst Abus. 2007;28:107–117. doi: 10.1300/J465v28n04_03. [DOI] [PubMed] [Google Scholar]
- Lynne-Landsman SD, Bradshaw CP, Ialongo NS. Testing a developmental cascade model of adolescent substance use trajectories and young adult adjustment. Dev Psychopathol. 2010;22:933–948. doi: 10.1017/S0954579410000556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehra R, Moore BA, Crothers K, Tetrault J, Fiellin DA. The association between marijuana smoking and lung cancer: a systematic review. Arch Intern Med. 2006;166:1359–1367. doi: 10.1001/archinte.166.13.1359. [DOI] [PubMed] [Google Scholar]
- Melissa DATA. [Accessed on May 28, 2008];Income tax statistics lookup. 2003 http://www.melissadata.com/lookups/taxzip.asp.
- Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, Lewis G. Cannabis use and risk of psychotic or affective mental health outcomes: A systematic review. Lancet. 2007;370:319–328. doi: 10.1016/S0140-6736(07)61162-3. [DOI] [PubMed] [Google Scholar]
- Murphy B, Herman H, Hawthorne G, Pinzone T, Evert H. Australian WHOQOL instruments: User’s manual and interpretation guide. Australian WHOQOL Field Study Centre; Melbourne, Australia: 2000. [Google Scholar]
- SAS Institute Inc. SAS 9.2. SAS Institute Inc; Cary, NC: 2008. [Google Scholar]
- Schulenberg J, Merline A, Johnston LD, O’Malley PM, Bachman JG, Laetz VB. Trajectories of marijuana use during the transition to adulthood: The big picture based on national panel data. J Drug Issues. 2005;35:255–279. doi: 10.1177/002204260503500203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. 2002 National Survey on Drug Use and Health Questionnaire. Office of Applied Studies; Rockville, MD: 2003. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Summary of National Findings. NSDUH Series H-38A. I. Office of Applied Studies; Rockville, MD: 2010. Results from the 2009 National Survey on Drug Use and Health. [Google Scholar]
- Swain NR, Gibb SJ, Horwood LJ, Fergusson DM. Alcohol and cannabis abuse/dependence symptoms and life satisfaction in young adulthood. Drug Alcohol Rev. doi: 10.1111/j.1465-3362.2011.00339.x. in press. [DOI] [PubMed] [Google Scholar]
- Vincent KB, Kasperski SJ, Caldeira KM, Garnier-Dykstra LM, Pinchevsky GM, O’Grady KE, Arria AM. Maintaining superior follow-up rates in a longitudinal study: Experiences from the College Life Study. Int J Mult Res Approach. doi: 10.5172/mra.2012.6.1.56. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams J, Skeels CL. The impact of cannabis use on health. De Economist. 2006;154:517–546. [Google Scholar]
- Windle M, Wiesner M. Trajectories of marijuana use from adolescence to young adulthood: Predictors and outcomes. Dev Psychopathol. 2004;16:1007–1027. doi: 10.1017/s0954579404040118. [DOI] [PubMed] [Google Scholar]
- Wu L, Pilowsky DJ, Schlenger WE, Hasin D. Alcohol use disorders and the use of treatment services among college-age young adults. Psychiatr Serv. 2007;58:192–200. doi: 10.1176/appi.ps.58.2.192. [DOI] [PMC free article] [PubMed] [Google Scholar]