Abstract
Objective
To evaluate the effect of diet versus exercise intervention on weight reduction.
Methods
Participants were randomly divided by gender, age, and living area into four groups: group DE (diet and exercise, n = 16), group D (diet only, n = 15), group E (exercise only, n = 15), and group C (control, n = 16). This study ultimately aimed to help participants reduce their body mass index (BMI) by 7% of baseline value. Subjects were 62 residents (men and women ranging in age from 40 to 69 years) of two residential areas in Nara Prefecture, Japan, who participated in annual health checkups in 2006. BMI of the participants was ≥24 and <28 kg/m2 at baseline examination. All participants agreed to undergo a 6-month intervention between January 2007 and September 2007.
Results
In our intention-to-treat analysis, mean change in BMI from baseline to final examination was as follows: group DE mean BMI decreased 6.6%, group D mean BMI decreased 5.3%, group E mean BMI decreased 2.3%, and group C mean BMI decreased 2.2%. The reduction in BMI from baseline to final examination was significant in all groups (DE, p < 0.001; D, p < 0.001; E, p = 0.009; C, p = 0.019). Further, mean abdominal circumference was significantly reduced in all groups. Blood glucose levels were significantly reduced only in group DE (p = 0.047).
Conclusion
Combined intervention with diet and exercise proved to be effective in weight reduction, whereas exercise intervention alone was not found to be effective.
Keywords: Diet and exercise education, Diet only education, Exercise only education, Weight reduction, Japanese residents
Introduction
The 2006 National Health and Nutrition Survey conducted in Japan showed that 1 out of every 2 men and 5 women aged between 40 and 74 years were strongly suspected to be either experiencing or at the risk of developing metabolic syndrome [1]. Obesity is an important contributing factor of metabolic syndrome, and preventive measures are needed to counteract it. Studies conducted in China, Australia, Holland, Finland, and the USA have shown that incidence of diabetes may be lessened or prevented altogether by weight reduction through diet and exercise education [2–7], and meta-analysis was performed to confirm the weight-reducing effect [8], with results suggesting that significant weight reduction could be attained with combined education about diet and exercise.
Although body mass index (BMI) of Asians is lower compared with Europeans and Americans, Asians are more likely to develop abdominal obesity, type 2 diabetes mellitus, and high blood pressure [9]. However, to date, few reports in Japan have examined the effectiveness of diet and exercise education on weight reduction among neighborhood residents with an established control group [10–14].
In Japan, no research team has made comparative studies of effective weight loss intervention methods, such as with differing educational methods. These intervention procedures include combined education of diet and exercise, diet education alone, and exercise education alone.
Here, we investigated the effect of combined diet and exercise education on achieving weight loss among local Japanese residents with BMI between 24 and 28 kg/m2 with an established control group.
Materials and methods
Cases and samples
Our study was conducted among residents of Kashiba City and Kammaki Town in Nara Prefecture, two residential areas near major cities. The subjects were men and women aged from 40 to 69 years who had received an annual health checkup in 2006 and whose BMI was from 24 to 28 kg/m2. They confirmed during an oral consultation that they had no history of treatment, nor were they currently being treated for diabetes, heart disease, or stroke. A total of 896 residents satisfied the above conditions (701 city residents and 195 town residents). We sent them a letter requesting their participation in our intervention study targeted at weight loss. Details were explained at an explanatory meeting, after which 80 residents agreed to give their written informed consent to participate (62 city residents and 18 town residents). However, two residents subsequently declined participation, leaving 78 residents enrolled at baseline examination. A further 15 were excluded later for failing to meet the eligibility criteria at baseline examination, and a further 1 declined participation. This study ultimately enrolled 62 subjects (47 city residents and 15 town residents). The flow of participants through the trial is shown in Fig. 1.
Fig. 1.
Flow of participants through the trial
Study design
Study subjects were divided into four groups after stratified random allocation by area of residence, sex, and age. The combined diet and exercise education group (group DE) included 16 participants, the diet education-only group (group D) included 15 participants, the exercise education-only group (group E) included 15 participants, and the control group (group C) included 16 participants.
We set a 6-month intervention period. During this period, groups DE, D, and E received intervention after baseline examination, whereas participants in group C managed their weight on their own, with no intervention. Group C received health leaflets through the mail once a month (five times total). However, the leaflets were not related to weight loss, but rather concerned other health-related matters such as influenza, vegetable selection, ultraviolet (UV) radiation, and preventing food poisoning and heart attacks.
A final examination measuring the same parameters assessed at baseline was conducted 6 months after baseline examination. The effects of intervention were assessed by examining the difference in measurements taken at baseline and final examinations.
This study was conducted from January 2007 to July 2007 in Kashiba City and from March 2007 to September 2007 in Kammaki Town, Nara Prefecture, Japan.
Intervention procedure
The goal for participants assigned to receive intensive lifestyle intervention was to achieve and maintain weight reduction of at least 7% of initial BMI. The target weight reduction over 6 months was set at 7% of BMI at baseline examination, with target monthly weight reduction of 1–2 kg. Given these values, we approximated the energy which should be reduced per day to be 1046–2094 kJ. In group DE, we split this energy reduction into two parts: intake energy and expended energy. Specifically, we instructed the subjects to decrease their daily intake energy by 523–1046 kJ, and increase their daily energy expenditure by 523–1046 kJ through walking exercises. Group D was instructed to decrease their daily energy intake by 1046–2094 kJ, while group E was instructed to increase daily energy expenditure by 1046–2094 kJ through walking exercises. Registered dietitians (RDs) and health fitness programmers (HFPs) issued instructions seven times: four times in the first half of the 6-month intervention period, and once a month in the second half.
The duration of 2 h per contact session was set for each of group DE, group D, and group E; more specifically, group DE received 2 h of diet- and exercise-related education (1 h each), while group D received 2 h of diet education and group E received 2 h of exercise education.
Diet education
With regard to diet education, RDs initially spoke with each subject in groups DE and D individually, thereafter giving lectures to the groups as a whole. Meal improvement targets were set for each subject by the RD during the first contact session. These targets were determined by the RD after consulting with the subject and were aimed at resolving problems in dietary intake which the RDs informed them of based on the results of a food frequency questionnaire (FFQ). The FFQ was administered before the intervention, and the RDs described the subject’s dietary pattern using the Japanese Food Guide Spinning Top [15].
The subjects kept a weight diary which was used as a teaching material. During the individual session at the first meeting, the subject recorded meal targets; they were instructed to mark an “○” for any achieved targets and an “×” otherwise. Daily weight measurements were also recorded in the diary.
RDs conducted group education by giving lectures on “balanced diet,” “relationship between diet and obesity,” “how to include vegetables in the diet,” “how to eat between meals,” and “sugar and salt.”
Exercise education
With regard to the target of the exercise group, “the target number of walking steps to be increased” was set by the RDs. This number was meant to be the target which each subject deemed achievable, judging from the number of walking steps recorded at baseline examination. The HFPs were in charge of group exercise education and gave specific instructions regarding walking, stretching, and myodynamic resistance exercises. The subjects kept a weight and walking steps diary to be used as a teaching material. They entered in the diary their exercise targets set during their individual session and marked an “○” if the target was achieved and an “×” if it was not. They also recorded their daily weight measurements and the number of steps walked as measured by a pedometer (Digi-Walker; Yamasa Tokeikeiki Co. Ltd., Tokyo, Japan).
Baseline examination
Anthropometric measurements consisted of weight, height, and abdominal circumference. Weight was measured in 100-g units, and height in millimeters. BMI was calculated by the following formula: BMI = weight (kg)/height (m)2.
Measurements were taken by staff who had received sufficient training in measuring abdominal circumference based on the method used in the Physical Condition Assessment of the National Health and Nutrition Examination Survey (conducted by the National Institute of Health and Nutrition of Japan). They measured each subject’s abdominal circumference to the nearest 0.5 cm at the level of the navel with the subject in standing position.
Biochemical blood parameters used as evaluation indices were blood glucose, hemoglobin A1c (HbA1c), albumin/globulin (A/G) ratio, total cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides. Approximately 12 ml blood was collected from an antecubital vein at least 5 h after a meal.
Blood pressure was measured twice, with the subject in seated position, using a blood pressure monitor (HM-701; ELK Corporation, Osaka, Japan). The mean of the two values was used for analysis.
Habitual energy and nutrient intake were estimated using the self-administered FFQ developed by Date et al., which includes 76 food items. The subjects recorded their intake amount and frequency for each item over the previous 1-year period. To estimate the portion size for each item, we used a life-size color food photograph collection prepared specifically for use in the FFQ. Energy and nutrient intake per day were computed using original software based on the Standard Tables of Food Composition in Japan (5th revised and enlarged edition).
Biochemical blood analyses were conducted by Japan Medical Laboratory Co. Ltd., Osaka, Japan.
Sample size
The end point for this study was BMI value after 6-month intervention. Referring to the BMI distribution obtained in the National Health and Nutrition Examination Survey conducted in Japan [16], we estimated the mean baseline BMI to be 25.5 kg/m2. We assumed the drop in BMI after at least one type of intervention to be an average of 7% (BMI decrease of 1.8 kg/m2, standard deviation 1.5 kg/m2). We also assumed no change in the control group, which did not receive any education at all. The study was designed to have 80% power to detect a 1.8 kg/m2 difference in BMI over 6 months. Values were considered statistically significant for p < 0.05, and a 15% dropout rate was assumed. These assumptions necessitated enrollment of at least 15 subjects per group.
Statistical analyses
Stratified randomization was carried out at Nara Women’s University. The primary analysis was conducted by applying intention-to-treat methods, with baseline values carried forward for missing values. A paired t test was used to measure the effect of 6 months’ intervention on anthropometric measurements, physiological measurements, results of blood chemistry tests, dietary intake, and the number of steps walked per day within each group. One-way factorial analysis of variance (ANOVA) was performed to compare groups at baseline and after intervention for variables of interest. If significant differences were noted, intervention groups were compared with the control group (as a reference group) using Dunnett’s multiple comparison test. Differences between groups in baseline values were assessed by analysis of variance.
SPSS (17.0) statistical analysis software (SPSS Inc., Chicago, IL, USA) was used in the present study. Values were considered statistically significant at p < 0.05, and two-sided significance levels are quoted.
Ethical considerations
Our study plan was reviewed and approved by the Research Ethics Screening Committee of Nara Women’s University. All enrolled subjects gave their written informed consent.
The subjects were assured that they were free to discontinue participation at any point if they so wished, even if they had already consented to participate in the study. Data were made anonymous to protect subjects’ personal privacy.
During the 6 months following the final examination, group C received diet education to provide them with an opportunity to reduce their weight, but a new control group was not established, and thus we did not take into consideration the effect of intervention on group C.
Results
Table 1 presents the age, sex, BMI, height, and weight at baseline examination for the four randomly assigned groups. With regard to analysis of variance, no significant difference between the groups was observed. With regard to subject participation, 89% of the subjects who underwent the baseline examination participated in the final examination.
Table 1.
Baseline participant characteristics
| Characteristics | DE (n = 16) | D (n = 15) | E (n = 15) | C (n = 16) | p-Value* |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| Age (years) | 61 (8) | 62 (8) | 62 (5) | 62 (6) | 0.963 |
| Women (%) | 75 | 80 | 80 | 81 | 0.743 |
| Body mass index (kg/m2)a | 25.7 (1.1) | 25.4 (1.1) | 25.5 (0.8) | 25.4 (1.1) | 0.905 |
| Height (cm) | 154.7 (7.5) | 156.3 (8.0) | 156.4 (5.3) | 155.8 (8.4) | 0.912 |
| Weight (kg) | 61.5 (6.2) | 62.4 (7.3) | 62.4 (4.1) | 61.9 (8.4) | 0.977 |
DE diet + exercise, D diet, E exercise, C control, SD standard deviation
* One-way factorial ANOVA was performed to compare the four groups
aCalculated as weight in kilograms divided by the square of the height in meters
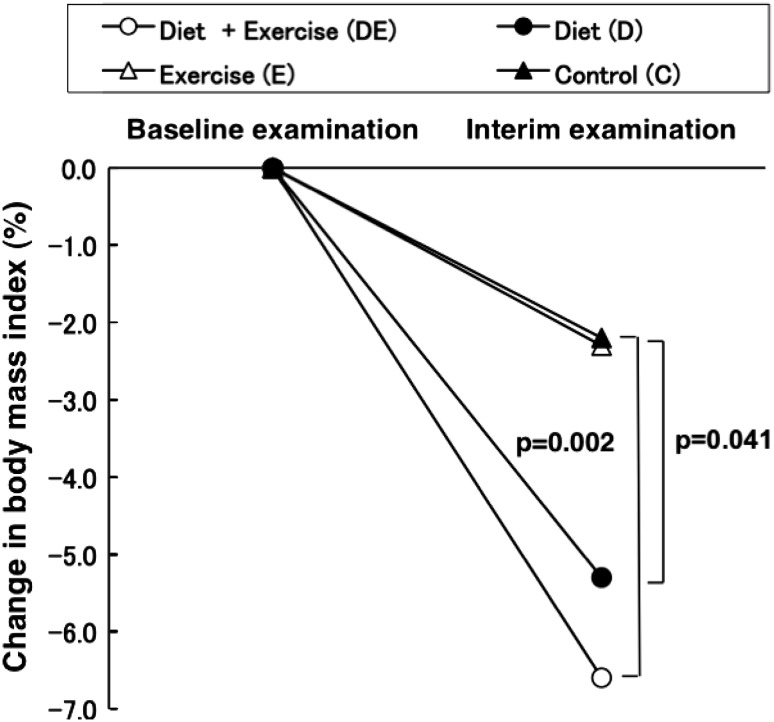
Changes in BMI at final examination compared with baseline are presented in Fig. 2 and Table 2. Mean change in BMI from baseline to final examination was as follows: group DE mean BMI decreased from 25.7 to 24.0 kg/m2 (−6.6%), group D mean BMI decreased from 25.4 to 24.1 kg/m2 (−5.3%), group E mean BMI decreased from 25.5 to 24.9 kg/m2 (−2.3%), and group C mean BMI decreased from 25.8 to 24.8 kg/m2 (−2.2%). In all groups, the reduction in BMI from baseline to final examination was significant (DE, p < 0.001; D, p < 0.001; E, p = 0.009; C, p = 0.019). Taking into account group C’s 2.2% reduction in BMI, the net weight loss effects of the intervention were 4.3% for group DE, 3.1% for group D, and 0.1% for group E. Comparing the decrease in BMI, the decreases observed in groups DE and D were significantly greater than that in group C (DE, p = 0.002; D, p = 0.041). However, the decrease in BMI observed in group E was not significant compared with that in group C (p = 1.000).
Fig. 2.
Change in body mass index from baseline to final examination (at 6 months) for each group was: group DE, −6.6%; group D, −5.3%; group E, −2.3%; group C, −2.2%. Significant reduction in body mass index between baseline and final examinations (at 6 months) was observed for all groups (DE, p < 0.001; D, p < 0.001; E, p = 0.009; C, p = 0.019; paired t test). Comparison of change in body mass index between baseline and final examinations (at 6 months) for groups DE, D, E, and C showed a significant change (DE, p = 0.002; D, p = 0.041; Dunnett’s multiple comparison test)
Table 2.
Comparison of baseline and final body weight, abdominal circumference, blood pressures, blood test, energy, nutritional intake, and number of walking steps for the four groups
| Characteristic | DE (n = 16) | D (n = 15) | E (n = 15) | C (n = 16) | p† | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | p* | Mean (SD) | p* | Mean (SD) | p* | Mean (SD) | p* | ||
| Anthropometric measurements | |||||||||
| Body mass index (kg/m2) | |||||||||
| Baseline | 25.7 (1.1) | 25.4 (1.1) | 25.5 (0.8) | 25.4 (1.1) | 0.905 | ||||
| Final | 24.0 (1.2) | <0.001 | 24.1 (1.0) | <0.001 | 24.9 (0.8) | <0.009 | 24.8 (1.2) | 0.019 | 0.032 |
| Abdominal circumference (cm) | |||||||||
| Baseline | 91.1 (4.2) | 93.6 (4.6) | 93.2 (3.4) | 93.1 (6.7) | 0.499 | ||||
| Final | 85.8 (3.8) | <0.001 | 89.3 (5.8) | <0.001 | 90.5 (3.8) | 0.008 | 90.0 (6.1) | 0.002 | 0.041 |
| Physiological measurements | |||||||||
| Systolic blood pressure (mmHg) | |||||||||
| Baseline | 131.0 (12.2) | 127.2 (15.6) | 126.4 (10.2) | 131.0 (9.7) | 0.596 | ||||
| Final | 125.4 (14.4) | 0.093 | 121.8 (12.9) | 0.025 | 127.2 (11.2) | 0.740 | 128.2 (17.2) | 0.472 | 0.612 |
| Diastolic blood pressure (mmHg) | |||||||||
| Baseline | 76.6 (7.1) | 75.7 (9.6) | 75.2 (7.1) | 75.4 (8.8) | 0.965 | ||||
| Final | 74.3 (7.5) | 0.187 | 71.9 (8.0) | 0.043 | 75.8 (8.2) | 0.701 | 73.4 (6.5) | 0.339 | 0.540 |
| Blood chemical tests | |||||||||
| Blood glucose (mmol/l) | |||||||||
| Baseline | 5.2 (0.4) | 5.0 (0.5) | 5.1 (0.3) | 5.2 (0.4) | 0.449 | ||||
| Final | 5.0 (0.4) | 0.047 | 4.9 (0.4) | 0.434 | 5.2 (0.4) | 0.285 | 5.3 (0.6) | 0.564 | 0.205 |
| HbA1c (%) | |||||||||
| Baseline | 5.1 (0.4) | 5.1 (0.4) | 5.2 (0.4) | 5.3 (0.4) | 0.517 | ||||
| Final | 5.1 (0.4) | 0.827 | 5.1 (0.4) | 0.595 | 5.3 (0.4) | 0.158 | 5.4 (0.4) | 0.008 | 0.081 |
| A/G ratio | |||||||||
| Baseline | 1.38 (0.13) | 1.32 (0.16) | 1.37 (0.10) | 1.41 (0.16) | 0.353 | ||||
| Final | 1.36 (0.12) | 0.386 | 1.35 (0.20) | 0.149 | 1.38 (0.14) | 0.585 | 1.37 (0.14) | 0.099 | 0.931 |
| Serum total cholesterol (mmol/l) | |||||||||
| Baseline | 5.9 (0.8) | 5.8 (0.6) | 5.8 (0.8) | 6.0 (0.9) | 0.353 | ||||
| Final | 5.8 (0.7) | 0.474 | 5.5 (0.8) | 0.017 | 5.7 (0.8) | 0.258 | 5.7 (1.1) | 0.134 | 0.865 |
| Serum HDL cholesterol (mmol/l) | |||||||||
| Baseline | 1.6 (0.5) | 1.7 (0.2) | 1.7 (0.3) | 1.6 (0.3) | 0.945 | ||||
| Final | 1.5 (0.4) | 0.062 | 1.6 (0.3) | 0.204 | 1.6 (0.3) | 0.730 | 1.5 (0.3) | 0.003 | 0.502 |
| Serum triglycerides (mmol/l) | |||||||||
| Baseline | 1.4 (0.9) | 1.4 (0.7) | 1.4 (0.7) | 1.3 (0.4) | 0.963 | ||||
| Final | 1.3 (0.7) | 0.580 | 1.2 (0.6) | 0.262 | 1.5 (1.0) | 0.476 | 1.5 (0.4) | 0.019 | 0.724 |
| Dietary intake | |||||||||
| Total energy (kJ/day) | |||||||||
| Baseline | 8782 (2766) | 8342 (1564) | 8702 (4012) | 10851 (2239) | 0.106 | ||||
| Final | 8434 (3004) | 0.347 | 7355 (1954)b | 0.009 | 9211 (3374) | 0.287 | 10447 (2488) | 0.615 | 0.039 |
| Protein (g/day) | |||||||||
| Baseline | 78.2 (26.9)a | 74.8 (20.3)b | 76.4 (28.3)c | 112.1 (34.2) | 0.002 | ||||
| Final | 80.7 (33.5) | 0.413 | 66.1 (23.7)b | 0.011 | 82.7 (30.6) | 0.113 | 100.7 (28.0) | 0.233 | 0.034 |
| Fat (g/day) | |||||||||
| Baseline | 64.9 (28.6) | 54.5 (9.6)b | 63.5 (33.5)c | 89.2 (28.4) | 0.009 | ||||
| Final | 66.3 (34.3) | 0.610 | 50.9 (15.7)b | 0.294 | 69.3 (34.6) | 0.115 | 84.1 (28.6) | 0.512 | 0.046 |
| Carbohydrate (g/day) | |||||||||
| Baseline | 276.1 (59.6) | 287.8 (52.2) | 290.0 (141.1) | 325.6 (52.9) | 0.510 | ||||
| Final | 262.9 (72.7) | 0.311 | 246.8 (63.7) | 0.003 | 297.0 (106.6) | 0.684 | 324.0 (71.2) | 0.944 | 0.065 |
| Number of walking steps (/day) | |||||||||
| Baseline | 8813 (2738) | – | 7300 (2604) | – | 0.126‡ | ||||
| Final | 10372 (1932) | 0.005 | – | 11014 (3185) | <0.001 | – | 0.500‡ | ||
DE diet + exercise, D diet, E exercise, C control, SD standard deviation
Baseline, baseline examination; Final, final examination (at 6 months); Blood glucose, 5-h glucose; A/G ratio, albumin/globulin
* Within-group changes from baseline, significance of paired t test
†One-way factorial ANOVA and Dunnett’s multiple comparison test were performed to compare the four groups
‡Significant difference between diet + exercise and exercise (unpaired t test)
aControl different from diet + exercise (p < 0.05)
bControl different from diet (p < 0.05)
cControl different from exercise (p < 0.05)
Mean values and standard deviations for anthropometric measurements physiological measurements, blood chemical tests, dietary intake, and number of steps walked per day at baseline and final examination for each group are presented in Table 2. Mean change in body weight from baseline to final examination was as follows: group DE mean body weight decreased from 61.5 to 57.4 kg (−4.1 kg), group D mean body weight decreased from 62.4 to 58.9 kg (−3.5 kg), group E mean body weight decreased from 62.4 to 61.0 kg (−1.4 kg), and group C mean body weight decreased from 61.9 to 60.4 kg (−1.5 kg). Reduction in body weight from baseline to final examination was significant in all groups (DE, p < 0.001; D, p < 0.001; E, p = 0.010; C, p = 0.027; data not shown in table). Significant decrease was observed in all groups for mean abdominal circumference value at final examination compared with that at baseline. Systolic blood pressure values fell significantly in groups DE and D, but diastolic blood pressure values were significantly decreased only in group D. With regard to blood chemical tests, blood glucose values were significantly reduced only in group DE (mean decrease 0.19 mmol/l). HbA1c increased significantly in group C. With regard to A/G ratio, no significant drop was observed in any group. Serum total cholesterol was significantly reduced only in group D (mean decrease 0.3 mmol/l), while HDL cholesterol fell significantly only in groups DE and C. Serum triglyceride levels were significantly increased in group C.
Comparing mean values for energy, protein, and carbohydrate intake at final examination with those at baseline in each group, a significant decrease was observed only in group D. However, no significant decrease in fat intake was observed in any group. Comparing mean values for number of walking steps at final examination with that at baseline for groups DE and E, both groups showed a significant increase (mean increase 1559 steps for group DE and 3714 steps for group E).
Discussion
In the present study, we examined the effect of lifestyle improvement on weight reduction among local residents of one city and one town in Nara Prefecture, Japan. After 6 months of intervention the mean BMI change was −6.6% among those receiving diet and exercise education, −5.3% in those receiving only diet education, −2.3% in those receiving only exercise education, and −2.2% in those in the control group. In comparison of the control group with the intervention groups, significant weight loss was observed in the diet and exercise education group (p = 0.002) and in the diet-only group (p = 0.041).
Multi-institutional research regarding whether diet or exercise education can better prevent occurrence of diabetes has been performed on glucose-tolerance-impaired patients or impaired glycemia patients in China [2], Australia [3], Holland [4], Finland [5, 6], and the USA [7]. Research conducted in the USA found that diabetes prevention was more effectively achieved by reduction of caloric intake and increase of energy expenditure than by drugs, highlighting the importance of lifestyle improvement in preventing onset of diabetes.
However, comparisons between Japan and the above-mentioned countries has shown stark differences with regard to eating habits, overall physique, and race make-up, among other such characteristics, and for this reason we cannot easily deliver the same diet and exercise education to Japanese people as to peoples of other countries. Lifestyle improvement techniques adapted specifically to Japan are necessary. Combined education on diet and exercise has been suggested to be effective in preventing obesity [17–22], and several randomized clinical trials (RCTs) have compared the effectiveness of combined education with education on diet or exercise alone [23–29]. However, most of these studies lacked a control group and therefore were unable to provide sufficient proof of effectiveness.
Few studies in Japan have scientifically demonstrated by comparison with a control group the effect of diet education and exercise education on weight reduction targeting local residents judged to have BMI slightly higher than normal or to be slightly obese. In 2007–2008, Tanaka et al. investigated the effectiveness of intervention in improving metabolic syndrome and visceral fat [13, 14]. However, they failed to establish control groups. We established control groups and investigated the effect of intervention by comparing the effects of combined education on diet and exercise with effects of diet or exercise education only, thereby offering new information.
Persons with BMI ≥24 but <28 kg/m2 were chosen as subjects in the present study. Given that persons with weights falling in the upper end of the normal range were anticipated to be at high risk of becoming obese, we chose those with BMI ≥24 kg/m2 as subjects. While the World Health Organization (WHO) criterion for obesity is BMI ≥30 kg/m2, the proportion of individuals with BMI ≥30 kg/m2 is lower in Japan than in Western countries. As no persons in the local area had BMI ≥28 kg/m2, we instead chose subjects with BMI <28 kg/m2 for the present study.
Given that a number of studies have reported a possible 6-month BMI of between 3% and 10%, we set a target BMI decrease of 7% by 6 months after baseline examination [19–22, 30–40]. In study by the Diabetes Prevention Program Research Group as well, weight loss of 7% was targeted [7]. In the present study, 44% (n = 7/16) of subjects in group DE, 27% (n = 4/15) in group D, 13% (n = 2/15) in group E, and 13% (n = 2/16) in group C experienced BMI decrease of 7% or more. The education given to the study participants also suggested that, in addition to body weight, abdominal circumference may be reduced.
With regard to blood test values such as blood glucose, no significant change was seen in comparison of the intervention groups with the control group. Given that the blood glucose level of those in the intervention group was already relatively low before the start of the study, their blood glucose levels may not have been able to fall any further.
Further, given that the evaluation criteria assessed in the present study were derived from pre-existing BMI, blood pressure, and hematological data, no new findings were feasible. However, given the present paucity of studies in Japan assessing diet and exercise depletion, we believe the results of this present study conducted in Japan to be of great value.
We need to look at the results of this study with a little reservation for the following reasons. First, this study was targeted at local residents living in the suburbs, mainly women. We therefore cannot be sure whether the same results may be obtained among urban residents. Second, although we invited 896 residents with BMI between 24 and 28 kg/m2 to participate in the study by posted mail, only 62 of them were ultimately enrolled. It is likely that they may have been particularly eager to receive education and improve their lifestyle. Third, exercise habits were evaluated by change in the number of walked steps. The reason we adopted walking in our exercise education is that this was a physical activity which subjects could accomplish every day with reasonable safety and without any special equipment or the aid of trainers. Only groups DE and E were fitted with pedometers, and therefore the change in the number of steps for groups D and C was not analyzed. If the level of physical activity had been analyzed using a structured questionnaire, results may have been easier to interpret. Fourth, to evaluate the quantity of energy intake, the FFQ was conducted in all subjects in this study, and their response to it might have raised their awareness of their poor dietary habits without diet education. After the intervention period, based on the results of the FFQ, we advised the subjects without diet education, though comments both oral and written, regarding how to change their diet contents.
The number of walked steps significantly increased among participants who received exercise education. However, because they did not receive any diet education, no significant change occurred in their diet intake. Overall, group E subjects had higher numbers of steps walked but a lower proportion of members achieving the target step numbers than in group DE. This seemed to be the reason why group E failed to burn the target calorie amount through walking. In addition, group E, which received no diet education, exhibited no beneficial effects from walking on weight reduction, in contrast to group DE, which did receive diet education.
Intervention with both diet and exercise education appears to be incorporated more easily and routinely among subjects and is believed to motivate the subjects more than intervention with either alone. We therefore believed that group E would show similar change in BMI to the control group.
Results from the present study showed that exercise-only education was not effective in achieving weight reduction, at least among a group of Japanese adults with BMI >24 and ≤28 kg/m2 whose average age was 62 years. Whether the same results may be found among the younger generation or those with higher BMIs, or among other racial groups, remains unclear.
Acknowledgments
This work was supported by a Research Fund for Health Science from the Ministry of Health, Labor, and Welfare in Japan. The authors express their thanks to the Public Health Bureaus of Kashiba City and Kammaki Town for their cooperation. The authors also thank Ms Hiromi Shinno (HFP), Ms Yuriko Kawaguchi (HFP), and Ms Hideko Shinohara (RD) for their cooperation.
Conflict of interest
The authors declare they have no conflict of interest.
References
- 1.Office for Life-Style Related Diseases Control General Affairs Division Health Service Bureau Ministry of Health, Labour and Welfare. The National Health and Nutrition Survey in Japan 2006. Tokyo: Dai-ichi Shuppan; 2009. p. 77–8 (in Japanese).
- 2.Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20:537–544. doi: 10.2337/diacare.20.4.537. [DOI] [PubMed] [Google Scholar]
- 3.Dunstan DW, Zimmet PZ, Welborn TA, Cameron AJ, Shaw J, Courten M, et al. The Australian Diabetes, Obesity and Lifestyle Study (AusDiab)—methods and response rates. Diabetes Res Clin Pract. 2002;57:119–129. doi: 10.1016/S0168-8227(02)00025-6. [DOI] [PubMed] [Google Scholar]
- 4.Mensink M, Corpeleijn E, Feskens EJ, Kruijshoop M, Saris WH, Bruin TW, et al. Study on lifestyle intervention and impaired glucose tolerance Maastricht (SLIM): design and screening results. Diabetes Res Clin Pract. 2003;61:49–58. doi: 10.1016/S0168-8227(03)00067-6. [DOI] [PubMed] [Google Scholar]
- 5.Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–1350. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- 6.Lindström J, Louheranta A, Mannelin M, Rastas M, Salminen V, Eriksson J, et al. The Finnish diabetes prevention study (DPS): lifestyle intervention and 3-year results on diet and physical activity. Diabetes Care. 2003;26:3230–3236. doi: 10.2337/diacare.26.12.3230. [DOI] [PubMed] [Google Scholar]
- 7.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Franz MJ, Wormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. JADA. 2007;107:1755–1767. doi: 10.1016/j.jada.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 9.James WP. The epidemiology of obesity: the size of the problem. J Intern Med. 2008;263:336–352. doi: 10.1111/j.1365-2796.2008.01922.x. [DOI] [PubMed] [Google Scholar]
- 10.Ishida S, Ito C, Murakami F, Horikawa C, Gennai N, Katayama M, et al. Prevention of type 2 diabetes mellitus by changing lifestyles among high risk persons: the diabetes prevention program of Hiroshima (DPPH). Design and one-year interim report on feasibility. J Jpn Diabetes Soc. 2004;47:707–13 (in Japanese).
- 11.Murakami F, Ito C, Ishida S. Prevention of type 2 diabetes mellitus by changing lifestyles among high risk persons. J Soc Met Clin Nutr. 2004;7:27–34 (in Japanese).
- 12.Sakane N, Sato J, Tsushita K, Tsujii S, Kotani K, Tsuzaki K, et al. Prevention of type 2 diabetes in a primary healthcare setting: three-year results of lifestyle intervention in Japanese subjects with impaired glucose tolerance. BMC Public Health. 2011;17:11–40. doi: 10.1186/1471-2458-11-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sasai H, Katayama Y, Numao S, Nakata Y, Tanaka K. Effects of exercise on visceral fat in obese middle-aged men: comparison to dietary modification. Jpn. J. Phys. Fitness Sports Med. 2008;57:89–100 (in Japanese).
- 14.Okura T, Nakata Y, Ohkawara K, Numao S, Katayama Y, Matsuo T, et al. Effects of aerobic exercise on metabolic syndrome improvement in response to weight reduction. Obesity. 2007;15:2478–2484. doi: 10.1038/oby.2007.294. [DOI] [PubMed] [Google Scholar]
- 15.Takemi Y, Yoshiike N, editors. The Japanese food guide spinning top “manual”. Tokyo: Dai-ichi Shuppan Publishers; 2005 (in Japanese).
- 16.Office for Life-Style Related Diseases Control General Affairs Division Health Service Bureau Ministry of Health, Labour and Welfare. The National Health and Nutrition Survey in Japan. Tokyo: Dai-ichi Shuppan Publishers; 2006. p. 147–8 (in Japanese).
- 17.Carels RA, Darby L, Cacciapaglia HM, Douglass OM, Harper J, Kaplar ME, et al. Applying a stepped-care approach to the treatment of obesity. J Psychosom Res. 2005;59:375–383. doi: 10.1016/j.jpsychores.2005.06.060. [DOI] [PubMed] [Google Scholar]
- 18.Koebnick C, Plank-Habibi S, Wirsam B, Gruendel S, Hahn A, Meyer-Kleine C, et al. Double-blind, randomized feedback control fails to improve the hypocholesterolemic effect of a plant-based low-fat diet in patients with moderately elevated total cholesterol levels. Eur J Clin Nutr. 2004;58:1402–1409. doi: 10.1038/sj.ejcn.1601984. [DOI] [PubMed] [Google Scholar]
- 19.Cox KL, Burke V, Morton AR, Beilin LJ, Puddey IB. The independent and combined effects of 16 weeks of vigorous exercise and energy restriction on body mass and composition in free-living overweight men—a randomized controlled trial. Metabolism. 2003;52:107–115. doi: 10.1053/meta.2003.50017. [DOI] [PubMed] [Google Scholar]
- 20.Mensink M, Feskens EJ, Saris WH, Bruin TW, Blaak EE. Study on lifestyle intervention and impaired glucose tolerance Maastricht (SLIM): preliminary results after one year. Int J Obes. 2003;27:377–384. doi: 10.1038/sj.ijo.0802249. [DOI] [PubMed] [Google Scholar]
- 21.Delahanty LM, Hayden D, Ammerman A, Nathan DM. Medical nutrition therapy for hypercholesterolemia positively affects patient satisfaction and quality of life outcomes. Ann Behav Med. 2002;24:269–278. doi: 10.1207/S15324796ABM2404_03. [DOI] [PubMed] [Google Scholar]
- 22.Liao D, Asberry PJ, Shofer JB, Callahan H, Matthys C, Boyko EJ, et al. Improvement of BMI, body composition, and body fat distribution with lifestyle modification in Japanese Americans with impaired glucose tolerance. Diabetes Care. 2002;25:1504–1510. doi: 10.2337/diacare.25.9.1504. [DOI] [PubMed] [Google Scholar]
- 23.Thomson RL, Buckley JD, Lim SS, Noakes M, Clifton PM, Norman RJ. Lifestyle management improves quality of life and depression in overweight and obese women with polycystic ovary syndrome. Fertil Steril. 2010;94:1812–1816. doi: 10.1016/j.fertnstert.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 24.Christiansen T, Paulsen SK, Bruun JM, Pedersen SB, Richelsen B. Exercise training versus diet-induced weight-loss on metabolic risk factors and inflammatory markers in obese subjects: a 12-week randomized intervention study. Am J Physiol Endocrinol Metab. 2010;298:E824–E831. doi: 10.1152/ajpendo.00574.2009. [DOI] [PubMed] [Google Scholar]
- 25.Molenaar EA, Ameijden EJ, Vergouwe Y, Grobbee DE, Numans ME. Effect of nutritional counselling and nutritional plus exercise counselling in overweight adults: a randomized trial in multidisciplinary primary care practice. Fam Pract. 2010;27:143–150. doi: 10.1093/fampra/cmp104. [DOI] [PubMed] [Google Scholar]
- 26.Coker RH, Williams RH, Yeo SE, Kortebein PM, Bodenner DL, Kern PA, et al. The impact of exercise training compared to caloric restriction on hepatic and peripheral insulin resistance in obesity. J Clin Endocrinol Metab. 2009;94:4258–4266. doi: 10.1210/jc.2008-2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Christiansen T, Paulsen SK, Bruun JM, Overgaard K, Ringgaard S, Pedersen SB, et al. Comparable reduction of the visceral adipose tissue depot after a diet-induced weight loss with or without aerobic exercise in obese subjects: a 12-week randomized intervention study. Eur J Endocrinol. 2009;160:759–767. doi: 10.1530/EJE-08-1009. [DOI] [PubMed] [Google Scholar]
- 28.Volpe SL, Kobusingye H, Bailur S, Stanek E. Effect of diet and exercise on body composition, energy intake and leptin levels in overweight women and men. J Am Coll Nutr. 2008;27:195–208. doi: 10.1080/07315724.2008.10719691. [DOI] [PubMed] [Google Scholar]
- 29.Anderssen SA, Carroll S, Urdal P, Holme I. Combined diet and exercise intervention reverses the metabolic syndrome in middle-aged males: results from the Oslo Diet and Exercise Study. Scand J Med Sci Sports. 2007;17:687–695. doi: 10.1111/j.1600-0838.2006.00631.x. [DOI] [PubMed] [Google Scholar]
- 30.Cook NR, Kumanyika SK, Cutler JA, Whelton PK. Dose–response of sodium excretion and blood pressure change among overweight, nonhypertensive adults in a 3-year diet intervention study. J Hum Hypertens. 2005;19:47–54. doi: 10.1038/sj.jhh.1001775. [DOI] [PubMed] [Google Scholar]
- 31.Kennedy BM, Paeratakul S, Champagne CM, Ryan DH, Harsha DW, McGee B, et al. A pilot church-based weight loss program for African-American adults using church members as health educators: a comparison of individual and group intervention. Ethn Dis. 2005;15:373–378. [PubMed] [Google Scholar]
- 32.Waller SM, Vander Wal JS, Klurfeld DM, McBurney MI, Cho S, Bijlani S, et al. Evening ready-to-eat cereal consumption contributes to weight management. J Am Coll Nutr. 2004;23:316–321. doi: 10.1080/07315724.2004.10719374. [DOI] [PubMed] [Google Scholar]
- 33.Burke V, Giangiulio N, Gillam HF, Beilin LJ, Houghton S. Physical activity and nutrition programs for couples: a randomized controlled trial. J Clin Epidemiol. 2003;56:421–432. doi: 10.1016/S0895-4356(02)00610-8. [DOI] [PubMed] [Google Scholar]
- 34.Xiao Y, Zhang ZT, Wang JB, Zhu WL, Zhao Y, Yan SF, et al. Effects of diet intervention on hyperlipidemia in eight communities of Beijing, China. Biomed Environ Sci. 2003;16:112–118. [PubMed] [Google Scholar]
- 35.James AP, Watts GF, Barrett PH, Smith D, Pal S, Chan DC, et al. Effect of weight loss on postprandial lipemia and low-density lipoprotein receptor binding in overweight men. Metabolism. 2003;52:136–141. doi: 10.1053/meta.2003.50032. [DOI] [PubMed] [Google Scholar]
- 36.Lantz H, Peltonen M, Torogerson LJ. A Diet and behavioral programme for the treatment of obesity. A 4-year clinical trial and a long-term post treatment follow-up. J Intern Med. 2003;254:272–279. doi: 10.1046/j.1365-2796.2003.01187.x. [DOI] [PubMed] [Google Scholar]
- 37.Lindstrom J, Eriksson JG, Valle TT, Aunola S, Cepaitis Z, Hakumaki M, et al. Prevention of diabetes mellitus in subjects with impaired glucose tolerance in the Finnish diabetes prevention study: results from a randomized clinical trial. J Am Soc Nephrol. 2003;14:S108–S113. doi: 10.1097/01.ASN.0000070157.96264.13. [DOI] [PubMed] [Google Scholar]
- 38.McManus K, Antinoro L, Sacks F. A randomized controlled trial of a moderate-fat, low-energy diet compared with a low fat, low-energy diet for weight loss in overweight adults. Int J Obes. 2001;25:1503–1511. doi: 10.1038/sj.ijo.0801796. [DOI] [PubMed] [Google Scholar]
- 39.Ramirez EM, Rosen JC. A comparison of weight control and weight control + body image therapy for obese men and women. J Consult Clin Psychol. 2001;69:440–446. doi: 10.1037/0022-006X.69.3.440. [DOI] [PubMed] [Google Scholar]
- 40.Dzator JA, Hendrie D, Burke V, Gianguilio N, Gillam HF, Beilin LJ, Houghton S. A randomized trial of interactive group sessions achieved greater improvements in nutrition and physical activity at a tiny increase in cost. J Clin Epidemiol. 2004;57:610–619. doi: 10.1016/j.jclinepi.2003.10.009. [DOI] [PubMed] [Google Scholar]