Abstract
The early developments of brain positron emission tomography (PET), including the methodological advances that have driven progress, are outlined. The considerable past achievements of brain PET have been summarized in collaboration with contributing experts in specific clinical applications including cerebrovascular disease, movement disorders, dementia, epilepsy, schizophrenia, addiction, depression and anxiety, brain tumors, drug development, and the normal healthy brain. Despite a history of improving methodology and considerable achievements, brain PET research activity is not growing and appears to have diminished. Assessments of the reasons for decline are presented and strategies proposed for reinvigorating brain PET research. Central to this is widening the access to advanced PET procedures through the introduction of lower cost cyclotron and radiochemistry technologies. The support and expertize of the existing major PET centers, and the recruitment of new biologists, bio-mathematicians and chemists to the field would be important for such a revival. New future applications need to be identified, the scope of targets imaged broadened, and the developed expertize exploited in other areas of medical research. Such reinvigoration of the field would enable PET to continue making significant contributions to advance the understanding of the normal and diseased brain and support the development of advanced treatments.
Keywords: advances, brain, disorders, drug development, physiology, PET
Introduction
A projection of the future applications of brain positron emission tomography (PET) requires us to address the growing concern that the field is currently not realizing its full potential in the quest to derive new information on the human brain in health and disease. To consider this objectively, we have reviewed the development and achievements of brain PET to date, to identify the impact the speciality has had in changing previous consensus and generating new understanding. Based on the foundation of this assessment the future direction of brain PET is projected.
The Development of Brain Positron Emission Tomography
Pre-Positron Emission Tomography Applications of Positron Emitting Radionuclides to Study Regional Brain Function
One of the first positron emitting radionuclides used for brain imaging was Arsenic-74 (74As), which has a long radioactive half-life of 17.8 days. Its leakage across the disrupted blood–brain barrier (BBB) was used for brain tumor delineation by Brownell and Sweet (1953) in Boston, USA, who detected the emitted positrons using a pair of coincident radiation detectors. Ter-Pogossian and Powers (1957) in St Louis, Missouri, reported the first biological application of oxygen-15 involving the administration of molecular oxygen-15 (15O2) by inhalation to a tumor bearing rat. After this, the animal was killed and autoradiographs of the tumor were recorded. The first application of oxygen-15 for measuring the regional oxygen extraction and perfusion of the human brain was also pioneered by the St Louis group. Initially in 1967, Ter-Pogossian and others administered the tracer as a single breath and followed the head time course with a pair of detectors (Ter-Pogossian et al, 1969). Their first attempt using a noninvasive approach produced time course data that was difficult to interpret (Ter-Pogossian and Herscovitch, 1985). As a result, they resorted to intracarotid artery injections of bolus 15O2-labeled red blood cells and oxygen-15-labeled water (H215O), to record the first pass extraction of oxygen and perfusion, respectively. From these data, they were able to derive absolute values of regional cerebral oxygen utilization, in milliliters of oxygen per 100 mL of tissue per minute (mL/100 mL per minute), and perfusion, in milliliters of blood per 100 mL of tissue per minute (mL/100 mL per minute) (Ter-Pogossian et al, 1970). A less invasive method based on the continuous inhalation of 15O2, designed to make imaging more practical, was subsequently developed by Jones et al (1976). This method created a ‘steady-state' distribution of radioactivity in the brain, dependent on perfusion and oxygen extraction as well as the radioactive decay of the radionuclide. When complemented by the continuous inhalation of carbon dioxide labeled with oxygen-15 ([15O]CO2), which results in a continuous arterial supply of [15O]H2O, it was possible to distinguish between the regional cerebral oxygen extraction and perfusion. The oxygen-15 steady-state method was demonstrated using the newly developed Boston positron camera (Burnham and Brownell, 1972) to record the first images of human brain metabolism in 1973 (Figure 1; Jones et al, 1976). In the mid 1970s, the steady-state method was used for qualitative imaging with the Anger gamma camera, to study various clinical conditions including stroke (Lenzi et al, 1978), brain tumors (McKenzie et al, 1978), cerebral lupus erythematosus (Pinching et al, 1978), and Parkinson's disease (PD) (Lenzi et al, 1979). The Anger camera was also used as a novel pharmacokinetic tool, pioneered by French researchers Comar, Maziere, Raynaud, and others in Orsay, who imaged the distribution of three 11C-labeled psychotropic drugs in the human brain (Raynaud et al, 1974). For this, they used the methyl iodide method for labeling with carbon-11, a method first developed in their institute (Marazano et al, 1977). These early imaging studies produced intense excitement, as it became apparent that molecular processes could be imaged relatively noninvasively in the living human brain.
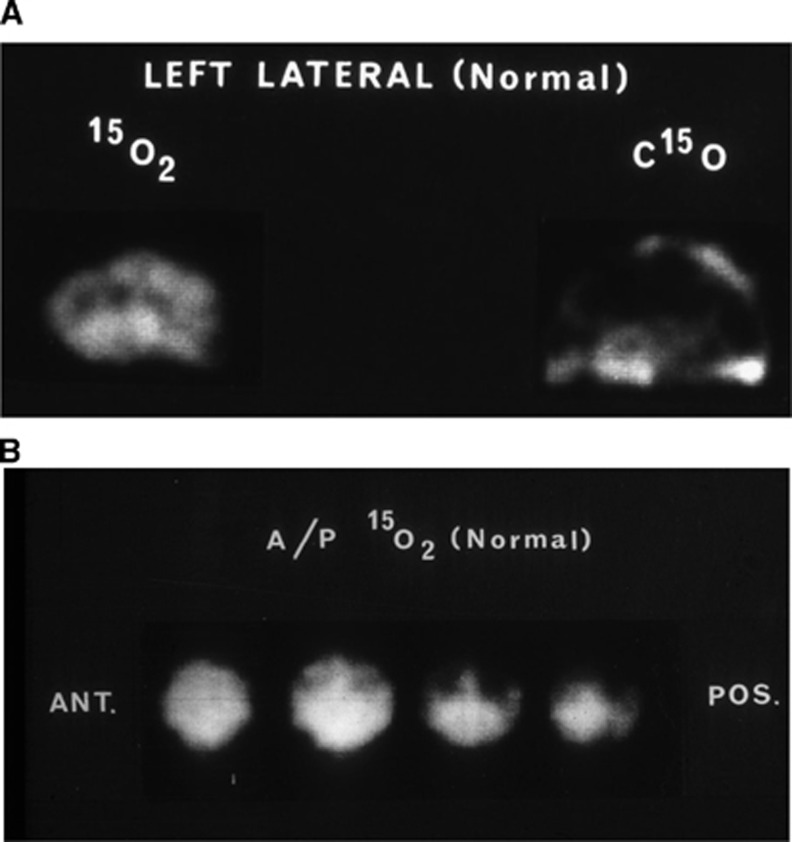
Figure 1.
(A) The first reported image of regional human brain metabolism in 1973 (Jones et al, 1976). This was recorded as a lateral view using the Massachusetts General Hospital positron camera (Burnham and Brownell, 1972) to image the steady-state distribution of radioactivity while continuously inhaling 15O2 as a tracer of oxygen utilization. Also shown is the steady-state distribution of radioactivity while continuously inhaling C15O to label red cells and hence delineate the cerebral vascular volume. (B) Anterior-posterior view of the steady distribution of radioactivity while continuously inhaling 15O2. The camera data have been focused on four equally spaced vertical planes.
The Introduction of Brain Positron Emission Tomography
The development of PET instrumentation in the 1970s, particularly through work in Boston (Burnham and Brownell, 1972; Chesler, 1973) and in St Louis (Phelps et al, 1975; Ter-Pogossian et al, 1975), has enabled the three-dimensional quantification of tissue radioactivity (Hoffman et al, 1979). A major stimulus to advance brain PET was the adaptation of the ex-vivo 2-deoxy-glucose technique pioneered by Sokoloff et al (1977) by labeling fluorodeoxyglucose with fluorine-18 ([18F]FDG) (Ido et al, 1978). [18F]FDG was first used in 1976 to image regional cerebral glucose metabolism in humans using single photon emission computerized tomography (SPECT; Alavi and Reivich, 2002; Kuhl et al, 1976). Soon after, Phelps et al (1979) used the quantitative capability of one of the first commercial positron emission tomographs to show both the quality of the brain metabolic images that could be produced and the opportunity to measure absolute regional cerebral glucose utilization rate (in mg/g per minute). Quantitative application of the steady-state oxygen-15 method to PET cameras quickly followed, allowing the determination of the regional cerebral metabolic rate for oxygen metabolism (CMRO2) in milliliters of oxygen per gram of tissue per minute (mL/g per minute) and cerebral blood flow (CBF) in milliliters of blood per gram of tissue per minute (mL/g per minute) (Baron et al, 1979; Frackowiak et al, 1980). Quantitative imaging of regional cerebral metabolism and perfusion that involved a further correction for intravascular oxygen-15 (Lammertsma and Jones, 1983) produced a wide range of novel, stimulating information on the human brain in health and disease. The introduction of more sensitive and longer axial surveying tomographs also allowed the use of dynamic methods to measure CMRO2 and CBF (Mintun et al, 1984).
Imaging Molecular Markers with Brain Positron Emission Tomography
The late 1970s and early 1980s saw a rapid increase in the development of tracers for brain PET. Key brain PET radiotracers and ligands that have been used for human studies are given in chronological order in Table 1. Imaging of regional amino-acid metabolism in brain tumors was performed using [11C]methionine (Bergstrom et al, 1983) as well as 11C-labeled unnatural amino acids (Hubner et al, 1981). The uptake and retention kinetics of bischloroethylnitrosourea (BCNU/carmustine), a drug targeting brain tumors, was assessed using a [11C]-radiolabeled version (Diksic et al, 1984). In 1983, major methodological advances were made in imaging neurotransmitter function. First, a group at McMaster University, Canada showed the ability to measure the kinetics of [18F]-labeled-6-fluoro-L-DOPA ([18F]F-DOPA), a dopamine synthesis pathway analog (Garnett et al, 1983). In the same year, researchers at The Johns Hopkins Hospital showed the ability to image neuronal receptors using [11C]-labeled methyl-spiperone, a ligand for the dopamine type-2/serotonin type-2 (D2/5-HT2) receptors (Wagner et al, 1983). This study represented a major methodological advance, as previously there was concern that the specific activity of the tracer, i.e., the ratio of labeled-to-unlabeled drug, would not be sufficient to provide an adequate signal-to-noise ratio to quantify targets with low tissue concentration, such as neuroreceptors, while satisfying tracer conditions (ensuring tracer concentrations in tissue result in <5% occupancy of the target). This demonstration provided important confidence for further neuroreceptor ligand development during the mid to late 1980s. [11C]raclopride, a more selective D2 receptor ligand with more favorable kinetics than methyl-spiperone, was developed by workers at the Karolinska Institute in Sweden, allowing for superior quantification of the D2 receptor. Soon after, ligands were introduced for a range of neuroreceptors, including [11C]Schering-23390 for the dopamine type-1 (D1) receptor; [11C]nomifensine for the dopamine transporter (DAT); [11C]flumazenil (FMZ) for the central benzodiazepine receptor; [11C]deprenyl for monoamine oxidase type-B (MAO-B) enzyme; [11C]PK-11195 for the peripheral benzodiazepine receptor (now known as the 18-kDa translocator protein—TSPO); [11C]diprenorphine, a nonselective opiate receptor antagonist; and [11C]carfentanil, a selective μ-opioid receptor agonist. This explosion was enabled by the development of a wide repertoire of techniques for rapidly labeling molecules with carbon-11 with high specific activity. In parallel, applications of PET for imaging the heart and tumors were being developed. Progressing into the 1990s, higher affinity and more selective PET imaging agents were introduced for novel targets in the serotonin system: [11C]WAY 100635 for 5-HT1A; [11C]MDL 100907 for the 5-HT2A; [11C]McNeil 5652 and [11C]DASB for the serotonin transporter (SERT/5-HTT). For the dopamine system, high-affinity ligands for D1 ([11C]NNC112) and D2 ([11C]FBL 457 and [18F]fallypride) have enabled the imaging of extrastriatal receptors; and [11C]β-CIT was developed for the dopamine transporter. Other high-affinity imaging agents introduced include [11C]MP4A and [11C]PMP for the acetylcholinesterase enzyme; 6-[18F]FA and 2-[18F]F-A-85380 for the α4β2 nicotinic receptor; [18F]SPA-RQ for the neurokinin-1 receptors; [11C]DTBZ for the vesicular monoamine transporter type 2; and [18F]MK-9470 for the cannabinoid-1 receptor. From 2000 onwards, the range of ligands for the monoamine systems has expanded further and tracers for novel targets such as 11C-labeled Pittsburgh compound-B ([11C]PiB) for β-amyloid, [11C]methyl reboxetine (MRB) for the norepinephrine transporter (NET), [11C]PBR28 a second generation TSPO ligand, and [11C]verapamil, a P-glycoprotein (P-gp) substrate were developed. More recently, advances have also been made in the measurement of regional cerebral protein syntheses using tracers such as [11C]leucine (Barrio et al, 1983; Tomasi et al, 2009). In addition, PET evaluation of biodistribution, brain penetration, and tissue pharmacokinetics of radiolabeled novel drugs have become valuable tools in drug development. Although not comprehensive, the PET radiotracers summarized here and in Table 1 illustrate the considerable and expanding range of imaging molecules that have been established for biochemical and physiological systems within the brain.
Table 1. Principal radiotracers used for human brain PET studies to date.
| Radiotracer | Targets | Reference |
|---|---|---|
| [11C]psychotropic drugs | Drug pharmacokinetics | Raynaud et al (1974) |
| [18F]FDG | Glucose utilization | Kuhl et al (1976) |
| [11C]methionine | Amino-acid transport | Comar et al (1976) Eur J Nucl Med 1:11–14 |
| [11C]unnatural amino acids | Amino-acid transport | Hubner et al (1979) J Nucl Med 20:507–513 |
| [15O]oxygen | Oxygen utilization | Frackowiak et al (1980) |
| [15O]water | Blood flow | Frackowiak et al (1980) |
| [11C]leucine | Protein synthesis | Barrio et al (1983) |
| [18F]F-DOPA | Dopamine synthesis | Garnett et al (1983) |
| [11C]methyl-spiperone | Dopamine and serotonin receptors | Wagner et al (1983) |
| [11C]PK-11195 | Peripheral benzodiazepine receptors | Camsonne et al (1984) J Labelled Comp Radiopharm 21:985–991 |
| [11C]BCNU/carmustine | Drug pharmacokinetics | Diksic et al (1984) |
| [11C]diprenorphine | Nonselective opiate receptors | Jones et al (1985) Lancet 326:665–666 |
| [11C]carfentanil | μ-Opioid receptor | Frost et al (1985) J Comput Assist Tomogr 9(2):231–236 |
| [11C]flumazenil (FMZ) | Central benzodiazepine receptors | Samson et al (1985) Eur J Pharmacol 110:247–251 |
| [11C]raclopride | Dopamine type 2 (D2) receptor | Ehrin et al (1985) Int J Appl Radiat Isot 36:269–273 |
| [11C]Schering-23390 | Dopamine type 1 (D1) receptor | Halldin et al (1986) Int J Rad Appl Instrum 37:1039–1043 |
| [11C]nomifensine | Dopamine transporter (DAT) | Aquilonius et al (1987) Acta Neurol Scand 76:283–287 |
| [11C]deprenyl | Monoamine oxidase type-B (MAO-B) | Fowler et al (1987) Science 235(4787):481–485 |
| [11C]McNeil 5652 | Serotonin transporter (SERT/5-HTT) | Suchiro et al (1993) Life Sci 53:883–892 |
| [11C]WAY 100635 | Serotonin 5-HT1A receptor | Pike et al (1994) Med Chem Res 5:208–227 |
| [11C]FBL 457 | Dopamine (D2/3) receptors | Halldin et al (1995) J Nucl Med 36:1275–1282 |
| [11C]MTBZ | Vesicular monoamine transporter (VMAT2) | Kilbourn et al (1995) Eur J Pharmacol 278:249–252 |
| L-1-[11C]tyrosine | Brain tumor protein synthesis | Willemsen et al (1995) |
| [11C]MDL 100907 | Serotonin 5-HT2A receptor | Lundkvist et al (1996) Life Sci 58:187–192 |
| [11C]β-CIT-FE | Dopamine transporter (DAT) | Halldin et al (1996) Synapse 22:386–390 |
| [11C]PMP | Acetylcholinesterase (ACE) | Kilbourn et al (1996) Synapse 22:123–131 |
| [11C]verapamil | P-glycoprotein (P-gp) substrate | Elsinga et al (1996) J Nucl Med 37:1571–1575 |
| [11C]MP4A | Acetylcholinesterase (ACE) | Iyo et al (1997) Lancet 349:1805–1809 |
| [11C]NNC112 | Dopamine (D1) receptor | Halldin et al (1998) J Nucl Med 37:2061–2068 |
| [18F]A-85380 | Nicotinic acetylcholine receptors | Horti et al (1998) Nucl Med Biol 25:599–603 |
| [18F]fallypride | Dopamine (D2) receptor | Mukherjee et al (1999) Nucl Med Biol 26:519–527 |
| [11C]α-methyl-l-tryptophan | Tryptophan activity | Shoaf et al (2000) J Cereb Blood Flow Metab 20:244–252 |
| [11C]DASB | Serotonin transporter (SERT/5-HTT) | Ginovart et al (2001) J Cereb Blood Flow Metab 21:1342–1353 |
| [11C]Ro15-4513 | GABA-benzodiazepine receptors | Lingford-Hughes et al (2002) J Cereb Blood Flow Metab 22:878–889 |
| [11C]temazolomide | Temazolomide pharmacokinetics | Saleem et al (2003) |
| [18F]SPA-RQ | Neurokinin-1 receptor | Solin et al (2004) Mol Imaging Biol 6:373–384 |
| [11C]PIB | β-Amyloid | Klunk et al (2004) |
| [18 F]fluoroethyl-L-tyrosine | Brain tumor protein synthesis | Pauleit et al (2005) |
| [18F]fluorothymidine | Brain tumor proliferation | Chen et al (2005) |
| [11C]harmine | Monoamine oxidase type-A (MAO-A) | Ginovart et al (2006) |
| [18F]MK-9470 | Cannabinoid receptor type 1 (CBR-1) | Burns et al (2007) PNAS 104:9800–9805 |
| [11C]methylreboxetine (MRB) | Norepinephrine transporter (NET) | Logan et al (2007) Nucl Med Biol 34:667–679 |
| [11C]ABP688 | Glutamate receptor 5 (mGluR5) | Ametamey et al (2007) J Nucl Med 48:247–252 |
| [11C]PBR28a | Translocator protein (TSPO) | Imaizumi et al (2008) Neuroimage 39:1289–98 |
| [18F]fluoromisonidazole | Brain tumor hypoxia | Spence et al (2008) |
| [11C]AZ10419369a | Serotonin 5-HT1B receptor | Pierson et al (2008) Neuroimage 41:1075–1085 |
| [18F]SP-203a | Glutamate receptor 5 (mGluR5) | Brown et al (2008) J Nucl Med 49:2042–2048 |
| [18F]galacto-RGD | Brain tumor angiogenesis | Schnell et al (2009) |
| [11C]SB-207145 | Serotonin 5-HT4 receptor | Marner et al (2009) J Nucl Med 50:900–908 |
| [11C]GSK189254a | Histamine-3 receptor | Ashworth et al (2010) J Nucl Med 51:1021–1029 |
| [11C]P943a | Serotonin 5-HT1B receptor | Gallezot et al (2010) J Cereb Blood Flow Metab 30:196–210 |
| [11C]GSK931145a | Glycine transporter 1 (GlyT1) | Passchier et al (2010) Synapse 64:261–270 |
| [11C]GSK215083a | Serotonin 5-HT6 receptor | Parker et al (2012) J Nucl Med (E-pub ahead of print) |
PET, positron emission tomography.
Recently tested in humans but pending further clinical investigation.
Positron Emission Tomography Camera Technology
Improvements in axial and transaxial spatial resolutions were achieved by using smaller detector elements and extending the detector array axially thereby increasing the range of axial survey. The development of the block detector array, which shared the light emitted from groups of scintillating crystals between just four photomultipliers, allowed for practical readout from individual small sensors to advance transaxial and axial spatial resolution and for recording multiple transaxial planes (Casey and Nutt, 1986). Together, these developments improved the ability to record kinetic data, as well as enhancing sensitivity and allowing data to be collected in 3D (The theory and practice of 3D PET, 1998). A reduction of dead time, the registration of random and scattered coincidences, and realization of higher spatial resolution were achieved by using scintillation detectors with improved light output characteristics. Lutetium oxy orthosilicate (Melcher and Schweitzer, 1992) became the principal detector material of choice, used today in high performance PET cameras for the brain (Wienhard et al, 2002), body (Kadrmas et al, 2009), and small animals (Cherry et al, 1996).
Positron Emission Tomography Data Processing and Analysis
Significant advances have been made in PET data processing by reducing the noise in the reconstructed image through iterative (Lange and Carson, 1984), 3D (The theory and practice of 3D PET, 1998), and 4D reconstructions (Reader et al, 2006), and by incorporating the tomograph's spatial resolution response (Sureau et al, 2008). While providing improved contrast for small objects and regions with low counting statistics, such reconstructions result in bias compared with the ‘gold-standard' filtered back projection method. Hence, the balance between bias and variability has to be carefully considered in relation to the study aims when choosing a reconstruction method. Quantification of tracer concentrations within small structures that are subject to partial volume effects (Hoffman et al, 1979) has been improved by corrective procedures, which use accurate anatomical information from coregistered magnetic resonance imaging (MRI) scans (Muller-Gartner et al, 1992).
The quantitative and specific nature of PET-derived data enables its principal utility to derive meaningful biological parameters, such as the density or affinity of a molecular target, or the rate of transport through a molecular pathway. The method most trusted to derive such parameters is an appropriate compartmental model, incorporating a combination of PET camera-derived dynamic tissue data with an input function derived from metabolite corrected arterial plasma data (Carson, 2003; Cunningham et al, 2005). Data-driven methods, such as spectral analysis (Cunningham and Jones, 1993) and methods to reduce noise like signal averaging and cluster analysis (Ashburner et al, 1996) along with the use of basis functions (Gunn et al, 1997) and wavelet analysis (Turkheimer et al, 2000) and other denoising processing (Christian et al, 2010), have complemented classical compartmental models. They have provided increased utility in the analysis of data from ligands and tissues with complex kinetics. Analysis of regional differences in outcome parameters has been powerfully enhanced by voxel-based statistical parametric mapping, which was introduced to analyze PET-derived CBF images (Friston et al, 1994) and extended to ligand binding studies and functional MRI (fMRI) activation data.
Implementing optimal quantification is resource intensive and requires the infrastructure and necessary skills to collect and analyze arterial blood samples during the course of the PET scan, restricting its use to relatively few centers. This has led to the development of alternative, simplified quantification methods, which can have valuable use in some cases. For example, the simplified reference tissue model that uses radioactivity measured in a reference region as a substitute input function, overcoming the need for arterial blood samples (Lammertsma and Hume, 1996). However, simplified quantification methods contain inherent assumptions, and for each new PET tracer an explicit demonstration of the validity of these assumptions must be performed by a comparison against ‘gold-standard' measures based on metabolite corrected arterial input models.
The Achievements of Brain Positron Emission Tomography
The unique information produced by brain PET research is substantial and includes important findings that led to changes of standard concepts. Initial reports focused on quantitative measurements of brain metabolism and blood flow. As new methodologies have developed, the focus shifted to the measurement of specific targets, especially receptors and enzymes. Applications developed to study normal and pathological brain processes have been extended to support drug development and more recently to clinical health care. In association with leading exponents of brain PET (see acknowledgements), the key achievements of brain PET in major clinical areas are outlined, focusing on the new information derived, the impact the information has made, and the changes that have been brought about in concepts of neuroscience.
Cerebrovascular Disease
The historical perspective and impact of brain oxygen-15 PET studies have recently been reviewed (Baron and Jones, 2011). Quantitative mapping of the supply and utilization of oxygen within the brain, and hence the balance between the two, the oxygen extraction fraction (OEF), has been studied in patients with recurrent cerebral ischemic attacks. A state of focally reduced CBF and raised OEF was coined ‘misery perfusion' by Baron and interpreted as reflecting exhausted vasodilatory reserve (Baron et al, 1981b). This provided a marker of potentially reversible cerebral ischemia and the rationale for surgical brain revascularization. Subsequently, postsurgery follow-up PET showed this pattern to be reversed, in association with a cessation of clinical attacks (Baron et al, 1981b; Leblanc et al, 1987a; Muraishi et al, 1993; Powers et al, 1984; Samson et al, 1985). Also of interest was the finding that the ratio of cerebral blood volume to perfusion was increased in the chronic ischemic areas, reflecting vasodilation compensating for the reduced perfusion pressure, which reverts to normal postvascular surgery (Gibbs et al, 1984; Leblanc et al, 1987b; Sette et al, 1989). These studies contributed to reversing the widespread belief that in stenosis or chronic occlusion of major cerebral arteries the clinical events are exclusively embolic, as opposed to hemodynamic—with major implications for clinical management. Severe misery perfusion was also found in acute stroke patients (Figure 2), documenting in humans the concept of a ‘penumbra' of viable tissue poststroke (Ackerman et al, 1981; Baron et al, 1981a; Wise et al, 1983), as previously shown in animal models. Observation of this phenomenon up to 16 hours after stroke onset has countered the earlier belief that after acute occlusion, cerebral tissue was viable for only minutes. These findings supported the case for randomized controlled trials and specialized stroke units which focus on administering, where appropriate, thrombolytic therapy hours after stroke onset. Importantly, however, larger clinical PET studies showed that penumbra was present in only a fraction of patients, while others showed either an extensive area of near-zero CMRO2—a marker of established tissue necrosis—or a pattern of focal hyperperfusion with preserved oxygen metabolism, indicating prior reperfusion with spontaneous salvage of the penumbra (Marchal et al, 1993). The notion that penumbra imaging could help to select the appropriate candidates for acute thrombolysis has since been guided using magnetic resonance-based diffusion and perfusion imaging, validated against PET though with some caveats (Sobesky et al, 2005b; Takasawa et al, 2008; Zaro-Weber et al, 2009, 2010) and more recently computed tomography-based perfusion imaging. Tissue viability in the acute stage has also been assessed using the neuronal marker [11C]FMZ (Heiss et al, 2001; Sette et al, 1989). Positron emission tomography has showed the elevation of TSPO signal, indicative of microglial activation, as well as selective neuronal loss in the salvaged penumbra, indicating that this tissue is affected by cellular processes that may impact long-term clinical recovery (Gerhard et al, 2005; Guadagno et al, 2008; Price et al, 2006; Ramsay et al, 1992). Several days after stroke, oxygen-15 imaging showed a delayed luxury-type of flow-metabolism mismatch, a pattern of high or normal perfusion but very low CMRO2, documenting reperfusion of metabolically dead cerebral tissue (Ackerman et al, 1981; Baron et al, 1981b; Lenzi et al, 1982; Wise et al, 1983). Thus, after stroke, conclusions reached on the basis of cerebral perfusion-based methods only should be treated with caution. An interesting and novel observation after stroke was the demonstration of a matched reduction of oxygen metabolism and blood flow to cerebral tissues remote from, and disconnected as a result of, the infarct or hemorrhage. The most striking example of these effects, shown with both oxygen-15 and [18F]FDG, involves the cerebellar hemisphere contralateral to the stroke—so-called crossed cerebellar diaschisis (Baron et al, 1980, 1984; Pantano et al, 1986; Serrati et al, 1994; Sobesky et al, 2005a). The presence of such a remote functional deficit with potential for metabolic recovery has implications for poststroke rehabilitation of recuperable functional tissue. [15O]H2O-based activation methods showed neuroplastic processing after adult-onset stroke that first showed the reorganization of large-scale networks underlying clinical recovery (Calautti et al, 2001; Chollet et al, 1991; Weiller et al, 1995). The methodology developed for studying regional oxygen utilization in cerebral vascular disease has been used to research head trauma patients. Here, the use of hyperoxia showed a universal increase in the CMRO2 with the at-risk tissue which was not evident from the microdialysis measures of lactate and pyruvate (Nortje et al, 2008). The use of [18F]FDG or TSPO ligands such as [11C]PK11195 (which reflects macrophage activity) offers the possibility of detecting unstable carotid atheromatous plaques, potentially enabling the detection of patients at risk of impending stroke and for monitoring therapy (Lamare et al, 2011; Moustafa et al, 2010; Rudd et al, 2002).
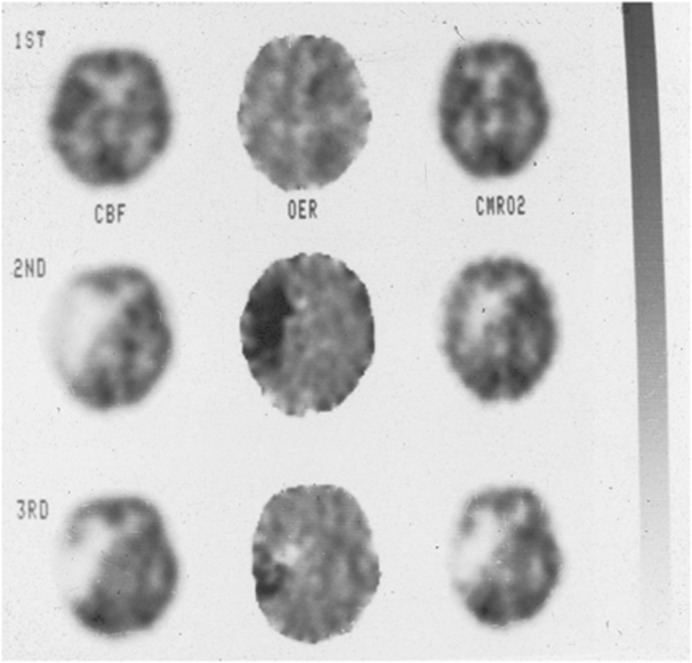
Figure 2.
Positron emission tomography (PET) images depicting cerebral blood flow (CBF), oxygen extraction ratio (OER), and cerebral metabolic rate of oxygen (CMRO2) of a patient after a left hemisphere transient ischemic attack (1ST), 7 hours after a major stroke (2ND), and 4 days after the stroke (3RD). The high oxygen extraction ratio seen within hours after the stroke fell in association with a decline in cortical oxygen metabolism (Wise et al, 1983).
Movement Disorders
Stoessl et al (2011) have recently reviewed the milestones in the imaging of movement disorders. In Parkinson's Disease (PD), PET studies have been instrumental in allowing the dissection of dopaminergic dysfunction. The use of [18F]-labeled F-DOPA as an index of presynaptic dopaminergic function has enabled the assessment of striatal nerve terminal function (Garnett et al, 1983). Striatal uptake of F-DOPA has been shown to correlate with the dopaminergic cell counts in the substantia nigra, as well as with striatal dopamine levels (Snow et al, 1993). [18F]F-DOPA PET showed that dopamine deficiency in PD selectively affects the posterior more than the anterior striatum, and the increased F-DOPA turnover in early PD reflects a reduced capacity for the synaptic vesicles to store dopamine (Sossi et al, 2002). Interestingly, brain PET has been used to show that the placebo effect in PD is mediated by release of endogenous dopamine (de la Fuente-Fernandez et al, 2001).
Positron emission tomography has also been valuable in monitoring the results of neuronal transplantation trials. While both F-DOPA uptake (Freeman et al, 1995; Kordower et al, 1995; Ma et al, 2010; Nakamura et al, 2001; Olanow et al, 2003; Wenning et al, 1997) and amphetamine-induced dopamine release, as measured with [11C]raclopride (Piccini et al, 1999), have been shown to consistently improve after neuronal transplantation, the clinical response has been limited (Freed et al, 2001; Olanow et al, 2003). This suggests that functional reinnervations of cortico-striatal-thalamocortical loops, as demonstrated by movement-related activation of the prefrontal and supplementary motor cortex imaged with [15O]H2O PET, are delayed (Piccini et al, 2000), and presumably may not occur in some cases. Brain PET has also been key to promoting the view of PD as a disease which is not confined to the dopamine system, as studies using cholinergic and serotonergic ligands have showed multisystem involvement. Reductions of cholinergic function are more widespread than that seen in patients with Alzheimer's disease (AD) (Bohnen et al, 2003; Hilker et al, 2005) and global reductions in 5-HT1A receptor density have been shown (Doder et al, 2003). Widespread brain dysfunction has been shown by imaging metabolic activity using [18F]FDG and CBF using [15O]H2O (Eidelberg et al, 1994). Metabolic network activity was found to be abnormal in the clinically unaffected hemisphere in unilateral PD patients (Tang et al, 2010), while CBF activation during motor learning is more widespread in early-stage PD patients, indicating potential compensatory mechanisms (Mentis et al, 2003).
The differences detected by PET in movement disorders have made it useful for investigating underlying pathology and for differential diagnosis. For example, preservation of striatal D2 receptors was found to differentiate PD patients from those with multiple systems atrophy. In dopamine responsive dystonia patients, a distinct disease-related metabolic network that is significantly different from that associated with PD and primary dystonia suggests a unique mechanism for this disorder. Network analysis has also revealed a consistent metabolic pattern characteristic of early or presymptomatic Huntingdon's disease (Feigin et al, 2001, 2007).
Dementia
A goal in dementia imaging has been to provide accurate neurochemical phenotyping of the variants of clinical dementia, such as Alzheimer's Disease (AD), frontotemporal dementia, dementia with Lewy bodies (DLB), and PD with dementia. The initial report using PET was based on the measurements of CMRO2, CBF, and OEF, which showed hypometabolism in the parietal and temporal regions in the less severe AD patients with more profound reductions in the frontal regions of patients with more severe degenerative dementia. There was no evidence of ischemia in either AD or multiinfarct dementia (Frackowiak et al, 1981). [18F]FDG has proven to be a sensitive metabolic marker to detect minimal changes in the function of terminal projections of excitatory pathways before structural changes (Benson et al, 1983; Friedland et al, 1983). Multiple patterns of altered metabolism have been identified in distinct dementia syndromes. These include occipital hypometabolism in DLB (Albin et al, 1996) and predominantly frontal hypometabolism in frontotemporal dementia and variant AD (Ishii et al, 1998). Focal cerebral hypometabolism appears to be predictive of patients who have neurodegenerative problems at a time when they are not able to be diagnosed clinically (Minoshima et al, 2004). In patients with mild cognitive impairment, characteristic [18F]FDG PET patterns of hypometabolism have been shown to predict AD diagnosis within 1 to 3 years (Herholz, 2010).
Differentiation of AD from DLB is readily shown by PET imaging of presynaptic nigrostraital dopamine terminal integrity with [18F]F-DOPA or the striatal vesicular monoamine transporter marker [11C]DTBZ (Koeppe et al, 2008). This has important impact on clinical care, as the treatment of DLB patients with antipsychotics precipitates profound rigidity and sometimes autonomic instability that may even be fatal. Similarly, DLB patients with symptomatic parkinsonism should not be treated aggressively with dopamine replacement therapy, as this precipitates psychosis.
In-vivo imaging of acetylcholinesterase with N-[11C]methylpiperidyl propionate as a marker of the presynaptic cholinergic system (Figure 3) has confirmed cholinergic projection defects in early-stage AD, but these were not as pronounced as may be expected from postmortem data (Bohnen et al, 2003; Kuhl et al, 1999). The cortical cholinergic defects have been found to be more pronounced in DLB compared with AD, which explains why DLB patients may respond more dramatically to cholinergic therapy than AD patients.
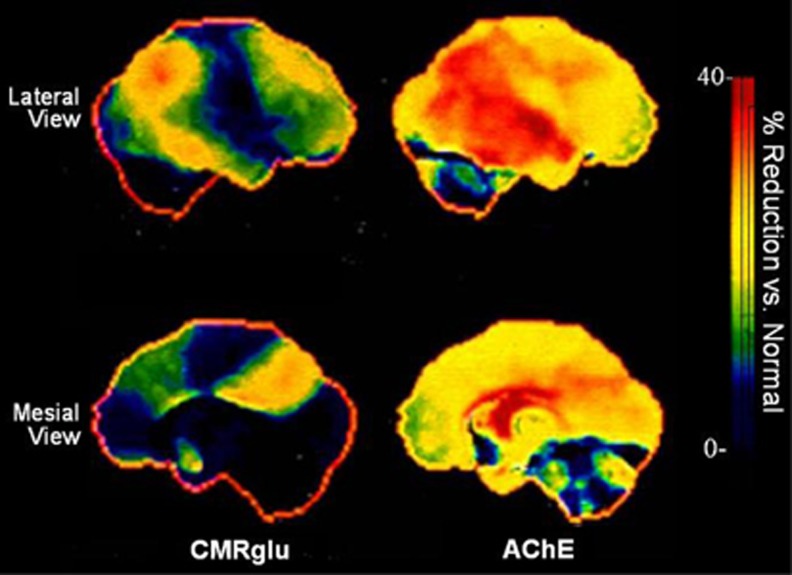
Figure 3.
Positron emission tomography (PET) images showing percentage reductions in regional glucose utilization and acetylcholinesterase (AChE) activity in Alzheimer's disease (AD) patients compared with controls, using [18F]-FDG and N-[11C] methylpiperidyl propionate, respectively. Glucose focal hypometabolism was focally prominent in posterior cingular gyrus and parietal cortex. Loss of AChE activity was even more diffuse and involved the entire neocortex, as well as the hippocampus (Kuhl et al, 1999). CMRglu, cerebral metabolic rate of glucose.
The introduction of ligands that target amyloid deposits, such as the [11C]PiB that binds selectively to fibrillary amyloid, has enabled AD patients to be distinguished from age-matched controls (Klunk et al, 2004). Combined amyloid and striatal vesicular monoamine transporter imaging revealed very significant discordant molecular imaging classifications compared with consensus clinical diagnostic classifications (Burke et al, 2011). Prospective and ongoing studies are revealing that PiB-positive patients with mild cognitive impairment have a much greater rate of progress and conversion to AD than PiB-negative mild cognitive impairment patients (Jack et al, 2010; Koivunen et al, 2011; Okello et al, 2009; Wolk et al, 2009). Using [11C]verapamil, PET imaging has shown that P-gp function is decreased in AD. This is the first direct evidence that the P-gp transporter at the BBB is compromised in sporadic AD, suggesting that it may be involved in AD pathogenesis (van Assema et al, 2012). Further, the first-generation TSPO ligand [11C]PK11195 has been used as a marker of activated microglia to show increased neuroinflammatory activity in AD patients (Cagnin et al, 2001), opening additional avenues for identifying the underlying pathological process leading to the pathogenic protein deposits characteristic of AD.
Epilepsy
Imaging with [18F]FDG PET has shown that patients with temporal lobe epilepsy who were seizure free after temporal lobe resection had a greater proportion of hypometabolic area surgically removed than individuals who continued to have seizures (Willmann et al, 2007). This finding raises the possibility of tailoring, especially in anatomically complex cases, the extent of resection according to the area of hypometabolism. [18F]FDG PET has been long integrated in presurgical neuroimaging in many centers and proved to be clinically useful in identifying focal glucose metabolic abnormalities—in particular, patients with normal MRI—in both temporal and neocortical epilepsies (Kumar et al, 2010) and subtle focal cortical dysplasia (Kim et al, 2011).
[11C]FMZ delineation of γ-aminobutyric acid receptor A (GABA-A) availability may provide a biochemical marker of epileptogenicity and strengthens the hypothesis that inhibitory mechanisms are disturbed in the epileptic focus (Bouvard et al, 2005). In the context of identifying epileptogenic tissue, binding of [11C]FMZ was significantly lower in the epileptic focus than in the contralateral homotopic reference region and the remaining neocortex (Savic et al, 1988). However, although [11C]FMZ showed great potential in selected patient subgroups, it has not yet reached the stage of routine clinical application. [11C]FMZ PET identified occult but surgically relevant abnormalities of benzodiazepine receptors (Ryvlin et al, 1998) and in malformations of cortical development detected abnormalities sensitively and objectively, which were more extensive than subtle structural abnormality revealed with MRI (Hammers et al, 2001; Richardson et al, 1998). Further, the use of interictal [11C]FMZ PET in patients with idiopathic generalized epilepsy, together with voxel-based morphometry MRI studies, has truly challenged the concept of generalized epilepsies, as it has revealed predominantly frontal increases in [11C]FMZ binding suggestive of focal microdysgenesis (Koepp et al, 1997; Savic et al, 1994). In a similar vein, the prevailing concept of focal epilepsies with epileptogenic zones, which after complete resection would lead to seizure freedom, has been challenged in a recent meta-analysis of [11C]FMZ PET studies (Laufs et al, 2011). The authors identified an area in the human piriform (primary olfactory) cortex that was active in association with interictal electroencephalography spikes and where benzodiazepine and GABA-A receptor complex expression were reduced as seizure frequency increased.
The endocannabinoid system is also implicated in epileptogenicity. A recent PET study using the radioligand [18F]FMK-9 to assess type 1 cannabinoid receptor showed potential for its use as a supplementary tool for enhanced definition of the preseizure onset zone for presurgical evaluation (Goffin et al, 2011). The results suggested a role for cannabinoid-1 receptor in the pathophysiology of seizures, although timing of the PET scans in relation to seizures was important to maximize sensitivity of the tracer.
One major drawback in clinical PET imaging is that of specificity: both FDG and FMZ PET show cause and consequence of seizure activity in the focus and projection area of the seizure onset. This can make treatment decisions for respective surgery difficult. But 11C-α-methyl-l-tryptophan PET may help to identify epileptic lesions in situations where changes identified with other modalities such as FDG PET or electroencephalography are unclear, for example, as shown in children with tuberous sclerosis (Chugani et al, 2011).
Positron emission tomography studies using opioid receptor ligands have supported findings from animal experiments suggesting a predominantly anticonvulsant effect of opioid peptides. With the μ-selective ligand [11C]carfentanil, increased μ-opioid receptor availability in the areas of the epileptogenic temporal lobe exhibiting interictal hypometabolism was shown (Frost et al, 1988). Studies with the nonselective opioid ligand [11C]diprenorphine showed the generalized displacement of opioid receptor ligands during absence seizures (Bartenstein et al, 1993) and a focal displacement during seizures of reading epilepsy (Koepp et al, 1998b). A role for the opioid system in the postictal rise in seizure threshold has also been suggested (Hammers et al, 2007). These brain PET studies provide strong support for the prevailing opinion that endogenous opioids are released after generalized and partial seizures, having a role in the tonic anticonvulsive mechanism that limits the spread of seizure activity from the epileptogenic focus.
The challenge in treating most central nervous system (CNS) diseases such as epilepsy is overcoming drug resistance due to poor delivery and retention of pharmaceuticals across the BBB. In patients with temporal lobe epilepsy, the K1 (influx rate constant) values of [11C]verapamil (a permeability-glycoprotein P-gp substrate) in drug-sensitive patients were higher than those in healthy volunteers, while those from the drug-resistant patients fell in between these two groups. This suggests BBB permeability differences and a less efficient P-gp function in drug-sensitive patients resulting in higher drug concentrations in the brain. After the administration of tariquidar, an inhibitor of P-gp, smaller K1 increases are observed in the drug-resistant patients (+27%) compared with healthy volunteers (+40%), supporting overexpression of P-gp function in drug-resistant epilepsy patients (Koepp, personal communication).
Schizophrenia
There is a good argument to be made that compared with all other psychiatric disorders, brain PET has made the biggest impact on the understanding and treatment of schizophrenia—the disease with the greatest hospitalization costs. Brain PET has been particularly influential in documenting enhanced dopaminergic activity in schizophrenia and the importance of addressing it in treatment. Quantitative imaging of the D2 receptor in the basal ganglia using [11C]raclopride showed that the magnitude of its blockade by a range of antipsychotic drugs correlated with symptom relief (Farde et al, 1988), thereby supporting the dopamine hypotheses of antipsychotic action (Figure 4). Receptor occupancy titrated against dose of antipsychotic drug (or plasma concentration) showed distinct thresholds for antipsychotic effects and extrapyramidal syndromes as induced by classical antipsychotic drugs (Figure 4). This work has had important clinical consequences in reducing the doses of antipsychotics used in clinical treatment of acute schizophrenic episodes, without impairing efficacy and improving tolerability (Farde et al, 1988; Farde, 1996; Kapur et al, 1996; Nord and Farde, 2011; Tauscher and Kapur, 2001). Using methylphenidate and amphetamine challenges, brain PET confirmed the earlier SPECT finding of heightened release of dopamine in schizophrenic patients compared with controls (Breier et al, 1997; Kegeles et al, 2010; Laruelle et al, 1999, 2003). Further evidence of elevated dopaminergic function was provided by the finding of increased [18F]F-DOPA signal in nonmedicated schizophrenic patients (Hietala et al, 1995) and in subjects with prodromal signs of schizophrenia (Howes et al, 2009; Figure 5). The combination of these findings suggests that schizophrenia is associated with elevated dopaminergic function in the associative regions of the striatum, which may also have an adverse effect on the dorsolateral prefrontal cortex where information is processed from. [15O]H2O PET imaging of schizophrenic patients during auditory and visual hallucinations has shown focal activations in the inner speech and auditory/linguistic association cortices of the brain, providing a biological basis for the subjective reports of schizophrenic patients' experience (Silbersweig et al, 1995). This used a method developed to capture transient changes in regional CBF with PET (Silbersweig et al, 1993). Imaging with [11C]PK11195 has showed an elevated TSPO availability, implying the presence of neuroinflammation within the first 5 years of schizophrenia onset. This suggests that neuronal damage may be involved in the loss of gray matter associated with this disease and indicates microglia as a potential novel target for neuroprotective therapies in schizophrenia (van Berckel et al, 2008).
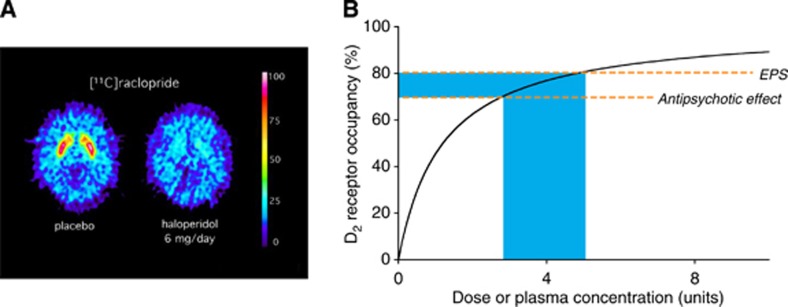
Figure 4.
(A) [11C]raclopride positron emission tomography (PET) images through the caudate/putamen level of a schizophrenic patient treated with placebo (left) and haloperidol (right) as described in Farde et al (1992). (B) The suggested distinct thresholds for antipsychotic effects and extrapyramidal syndromes (EPSs) as induced by classical antipsychotic drugs. Owing to the hyperbolic relationship between occupancy of the D2 receptor and dose of antipsychotic drug (or plasma concentration) there is a rather narrow interval for optimal therapeutic treatment. Figure modified from Farde (1996).
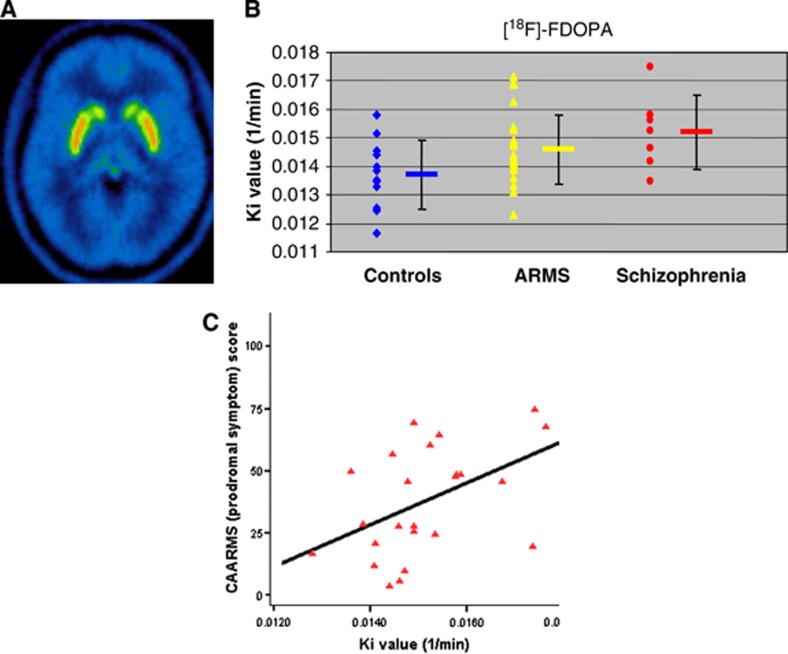
Figure 5.
(A) Straital [18F]16-fluoro-L-DOPA ([18F]F-DOPA) summation image. (B) Individual and group striatal [18F]F-DOPA Ki values (influx rate constants) for normal controls, subjects with At-Risk Mental Status (ARMS) and those with schizophrenia, showing significantly higher (P<0.05) Ki values in schizophrenia patients compared with controls. (C) Positive correlation between total Comprehensive Assessment of At-Risk Mental States (CAARMS) score (higher score indicates greater severity of prodromal symptoms) and Ki values (Howes et al, 2009).
Addiction
Neuroimaging has had a key role in defining the neurobiology of addiction and helped establish addiction as a ‘brain disease', with PET leading the characterization of neurotransmitter systems in intoxication, withdrawal, and abstinence. A key discovery has been the blunted striatal dopaminergic activity, at presynaptic and postsynaptic levels, in a range of addictions. Since sensitization was first proposed, i.e., that dopaminergic neurotransmission was potentiated after repeated drug exposure, the measurement of dopamine release in addiction has been pursued vigorously. An early study using [11C]raclopride found the opposite, with a blunting of methylphenidate-induced striatal dopamine in chronic cocaine abusers compared with controls (Volkow et al, 1997). This finding was replicated using amphetamine and [11C]raclopride PET imaging (Martinez et al, 2007) in a study which compared the effects of amphetamine between functional subdivisions of the striatum (limbic, associative, and sensorimotor) and found that the dopamine response was significantly blunted in all three regions. Subsequently, blunting of amphetamine-induced dopamine release in the limbic region of the striatum was shown to be associated with drug-seeking behavior. Baseline levels of striatal dopamine, as measured with the α-methyl paratyrosine paradigm and [11C]raclopride PET, are also depleted in cocaine abusers (Martinez et al, 2009). The blunting of elicited dopamine release has also been reported in alcoholism, though restricted to the ventral striatum (Martinez et al, 2005; Volkow et al, 1997). There has been a limited number of studies using [18F]F-DOPA, but reduced levels in alcohol and cocaine addiction have been reported (Heinz et al, 2005b). Availability of dopamine receptors 2 and 3 (D2/3) have been measured in many PET and SPECT studies with tracers such as [11C]raclopride or [123I]IBZM. The majority of studies in abstinent alcohol or cocaine addicts report lower D2/3 receptor levels in the striatum, particularly in the ventral region (Martinez and Narendran, 2010).
The dopaminergic system is modulated by opioid neurotransmission. Availability of μ-opioid receptors, as measured with [11C]carfentanil and [11C]diprenorphine PET, is increased in early abstinence from cocaine, alcohol, or opioids and the increases are related to craving (Heinz et al, 2005a; Williams et al, 2007, 2009; Zubieta et al, 1996). Positron emission tomography has also been used to characterize dose–occupancy relationship for opioid substitute medications, methadone, and buprenorphine. While buprenorphine can be shown to occupy μ-opioid receptors using [11C]carfentanil PET (Greenwald et al, 2003), even high levels of methadone show limited or no occupancy of opioid receptors when using the nonsubtype-selective ligand [11C]diprenorphine (Kling et al, 2000; Melichar et al, 2005), which questions the mode of action of methadone treatment.
Many of the effects of alcohol in the brain are mediated by stimulating the GABA-benzodiazepine receptor. Reduced GABA-benzodiazepine receptor levels have been shown with [123I]iomazenil SPECT in alcohol dependence after weeks of abstinence, and [11C]Ro15 4513 PET showed this to occur in the nucleus accumbens and hippocampus (Lingford-Hughes et al, 2012).
Depression and Anxiety
Imaging with PET has provided an important contribution toward understanding the pathophysiology of major depressive disorders (MDDs), identifying endophenotypes and vulnerability traits, as well as assessing therapeutics and identifying new opportunities for prevention. Facilitated by the development of suitable radioligands for monoaminergic receptors (such as the 5-HT1A, 5-HT2A, and D2), reuptake transporters (such as the serotonin transporter (SERT/5-HTT), dopamine transporter (DAT) and norepinephrine transporter (NET)), and the catabolic enzymes (MAO-A and -B), PET imaging has had a considerable impact on the monoamine theory of MDD. Given that MAO-A is an enzyme that metabolizes monoamines, such as serotonin, norepinephrine, and dopamine, elevated MAO-A density is proposed as the primary mechanism of the multiple monoamine reduction observed in MDD.
Imaging studies have investigated differences in the availability of 5-HT1A and 5-HT2A receptors between healthy volunteers and patients with MDD (Drevets et al, 1999; Meyer, 2008; Sargent et al, 2000; Savitz and Drevets, 2009; Smith and Jakobsen, 2009). Patients with major depressive episode show a reduction in 5-HT1A receptor availability (Drevets et al, 1999; Sargent et al, 2000), while MDD patients who show high levels of pessimism show an elevation in 5-HT2A receptor availability (Bhagwagar et al, 2006; Meyer et al, 2003). The availability of MAO-A activity, as measured with [11C]harmine PET (Ginovart et al, 2006), was found to be elevated in patients with MDD (Meyer et al, 2006, 2009), consistent with postmortem data (Johnson et al, 2011).
The development of novel therapeutics for mood disorders has benefited from the assessment of target occupancy with PET and has been used in the development of 5-HT1A antagonists, dopamine reuptake inhibitors, and MAO-A inhibitors (Meyer et al, 2002; Rabiner et al, 2000, 2001; Sacher et al, 2011). An 80% occupancy of the 5-HTT by serotonin reuptake inhibitors distinguishes medications from placebo in the treatment of major depressive episode in clinical trials (Meyer et al, 2004). Lower occupancies were observed with doses that lacked clinical efficacy and the affinity of medications tested were found to differ by two orders of magnitude compared with in-vitro results, emphasizing the value of an in-vivo evaluation of target occupancy with PET. This has led to the recognition of an 80% occupancy being a requirement for the development of novel antidepressants targeting 5-HTT.
An intriguing question raised by the PET findings in patients with MDD is whether these are trait or state markers. The PET studies in individuals at risk due to genetic predisposition, stressful life events, or personality traits, have provided a key contribution to the investigation of vulnerability to mood disorders. Alterations in several monoamine system markers support the notion of a disordered serotonergic neurotransmitter system being associated with a vulnerability to MDD. For example, the finding of elevated MAO-A availability in the prefrontal and anterior cingulate cortex in states of high risk for MDD recurrence associated with depressed mood, such as during early postpartum and in early withdrawal from heavy cigarette smoking, is exciting (Bacher et al, 2011; Meyer et al, 2009; Sacher et al, 2010). Greater MAO-A availability may lower brain monoamine concentration, which is associated with subsequent major depressive episode (Freis, 1954). Low 5-HTT binding activity was found in the dorsolateral prefrontal cortex of healthy co-twins of patients with mood disorders (Frokjaer et al, 2009), indicating a genetic vulnerability that may contribute to the pathophysiology of depression. Elevated 5-HTT levels in affect-modulating brain regions have been shown during the winter relative to the summer months (Kalbitzer et al, 2010; Praschak-Rieder et al, 2008; Ruhe et al, 2009), a finding of relevance to seasonal affective disorder pathology. Persistent reductions in 5-HT1A receptors have been shown in patients fully recovered from a major depressive episode (Bhagwagar et al, 2004), implying that reduced 5-HT1A availability may predispose to MDD, or be a result of the illness. Interestingly, an initial report has shown that psychotherapy increases brain serotonin 5HT1A receptors in patients with MDD (Karlsson et al, 2010). In healthy subjects, neuroticism, vulnerability, and familial risk have all been positively associated with increased frontolimbic 5-HT2A receptor levels and binding activity (Frokjaer et al, 2008, 2010).
Positron emission tomography and SPECT have been widely used in the investigation of anxiety disorders. Reductions in 5-HT1A availability have also been observed in anxiety disorders (Lanzenberger et al, 2007; Nash et al, 2008; Neumeister et al, 2004). Interestingly, 5-HTT reductions observed in patients with MDD correlated in magnitude with the severity of cooccuring anxiety, rather than depressive symptoms (Reimold et al, 2008). A recent meta-analysis found decreased striatal D2 receptor and mesencephalic 5-HTT binding in obsessive compulsive disorder, and reductions in GABA-A receptors in frontocortical regions in panic disorder and temporocortical areas in generalized anxiety disorder (Nikolaus et al, 2010). When all anxiety disorders were pooled, reductions in midbrain 5-HTT and 5-HT1A receptors, striatal D2 and GABA-A receptors were observed, indicating a major role for dopamine, 5-HT, and GABA neurotransmission in anxiety disorders.
Cerebral Tumors
Using oxygen-15 and [18F]FDG PET studies, brain gliomas showed a low OEF compared with the normal brain, whereas their glucose extraction fraction was similar (Rhodes et al, 1983). This clear in-vivo demonstration of the preferential aerobic glycolysis of human tumors, known as the Warburg effect, paved the way for the current widespread use of [18F]FDG for tumor localization throughout the body, principally for disease staging and also as a marker of treatment response. It was shown early in the application of PET that it enabled the differentiation of therapy induced tissue changes from recurrent brain tumor (Di Chiro et al, 1988). However, because of the high background of glucose utilization in normal brain tissue, labeled amino acids such as [11C]methionine (Bergstrom et al, 1983) and [11C]tyrosine (Willemsen et al, 1995), as well as labeled unnatural amino acids such as [11C]amino cyclopentane carboxylic (Hubner et al, 1981), have subsequently showed greater sensitivity for defining cerebral tumors by exploiting their increased protein synthesis compared with normal brain tissue. Evaluation of tumor [11C]methionine PET data compared with normal brain tissue uptake data suggests a means to improve the sensitivity of detecting tumor infiltration of white matter (Coope et al, 2007). The current tracer of choice for imaging amino-acid transport/protein synthesis appears to be [18F]-(fluoroethyl)-L-tyrosine (FET), which when combined with MRI has shown to improve the diagnostic assessment of cerebral gliomas (Pauleit et al, 2005). Using the labeled analog of thymidine [18F]FLT, it has been possible to image brain tumor proliferation (Chen et al, 2005). Using [18F]fluoromisonidazole to image tumor hypoxia, it was shown that the volume and intensity of hypoxia before radiotherapy is strongly associated with worse survival and time to progression (Spence et al, 2008) and as a marker of integrin α(v)β(3) expression, [18F]galacto-RGD peptide has been used to image angiogenesis in brain tumors (Schnell et al, 2009).
Temazolomide is an anticancer drug currently used in the treatment of brain tumors, which has shown improved survival when combined with radiotherapy and is now standard therapy after surgery for high grade gliomas (Stupp et al, 2005). When undergoing early clinical testing, [11C]temazolomide PET studies were used to show adequate delivery and dosimetry of the drug within the cancerous tissue of the brain, which helped to support the development of what has become a billion dollar per year therapeutic agent (Saleem et al, 2003).
Studies of the Healthy Human Brain
Using [18F]FDG, patterns of regional cerebral glucose metabolism have been reported for the maturational changes in infants (Chugani and Phelps, 1986). These were shown to be in agreement with neurophysiological and anatomical alterations known to occur during infant development. Using the brain PET [15O]H2O activation method (Fox et al, 1987a) and analytical methodology such as statistical parametric mapping (Friston et al, 1994), a range of exciting results were reported covering, for example, visual (Fox et al, 1987b; Lueck et al, 1989), cognition (Petersen et al, 1988; Posner et al, 1988), working memory (Paulesu et al, 1993), and face perception (Dolan et al, 1997). As a result, more neuroscientists became attracted to using imaging of regional cerebral function for researching the normal brain. The increased scientific output drew the attention of exponents of MRI, which led to the introduction of the blood oxygen level-dependent functional MRI (fMRI) technique. fMRI relies on the fact that during transient cerebral activation the brain undergoes the uncoupling of flow from oxygen utilization through aerobic glycolysis, i.e., the glucose-lactate switch. As a result, the OEF is reduced and the local venous oxygen content rises. Since blood hemoglobin is diamagnetic when oxygenated (and paramagnetic when not) this provides a local increase in the MRI signal indicating regions of brain activity. Proof of this underlying mechanism of uncoupling came from brain PET studies which showed that regional CBF and glucose utilization were increased during activation but not oxygen utilization (Fox and Raichle, 1986).
Interestingly, it has been reported that by quantitatively imaging glucose and oxygen utilization with [18F]FDG and oxygen-15, regions of physiological aerobic glycolysis are present in the resting state and differentially distributed (Figure 6; Vaishnavi et al, 2010). The use of aerobic glycolysis as a brain energy source is less efficient at producing adenosine triphosphate compared with oxidative phosphorylation (by a factor of 30), but its facility for faster rate changes makes it uniquely suited to accommodate small, rapidly changing requirements in energy. This observation suggests that one of the factors contributing to the regional variation may be the percentage of nonneuronal cells, such as astrocytes, which use aerobic glycolysis for glutamate cycling.
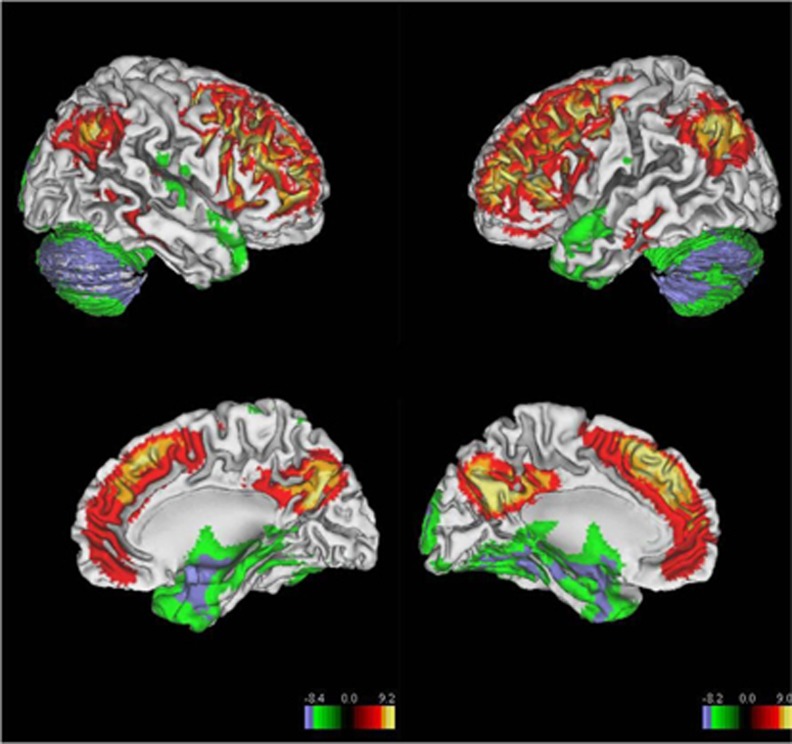
Figure 6.
Distribution of aerobic glycolysis in resting human brain using a glycolytic index (n=33, groupwise t test, ∣Z∣>4.4, P<0.0001, cluster>99, corrected for multiple comparisons). Specifically, regions with significantly high glycolysis include bilateral prefrontal cortex, bilateral lateral parietal lobe, posterior cingulate/precuneus, gyrus rectus, bilateral lateral temporal gyrus, and bilateral caudate nuclei. In contrast, cerebellum and bilateral inferior temporal gyrus have significantly low levels of aerobic glycolysis (Vaishnavi et al, 2010).
The PET investigations have been instrumental in advancing the understanding of the neurochemical and physiological systems in normal brain function. The demonstration of the feasibility of PET techniques to detect the increased blockade of D2 receptors when normal subjects experienced reward (Koepp et al, 1998a) and dopamine release during the performance of motor tasks (Goerendt et al, 2003) has enabled subsequent dissection of the role of dopaminergic circuits in normal human learning and executive function (Badgaiyan et al, 2007; Cervenka et al, 2008; Garraux et al, 2007; Karabanov et al, 2010; MacDonald et al, 2009). In turn, this has led to the evaluation of individual differences in brain neurochemistry and physiology within a healthy population. Numerous PET studies have linked personality traits related to novelty seeking, impulsivity, and adventurousness to measures of dopamine release (Leyton et al, 2002; Oswald et al, 2007) and D2/D3 availability in the midbrain (Zald et al, 2008) and cortical regions (Bernow et al, 2011). These findings are considered significant, as disturbances in dopaminergic neurotransmission have been implicated in the pathophysiology of addiction, as have the personality traits of impulsivity, novelty seeking, and high reward dependence. The finding of a link between striatal D2 receptor availability and the personality trait of detachment (Breier et al, 1998; Farde et al, 1997) has indicated a potential disruption of D2-mediated neurotransmission underlying negative symptoms in schizophrenia. Likewise, such studies may provide a mechanistic link between personality factors and brain neurochemistry. The role of opioidergic neurotransmission in the pathophysiology of addictive behavior is supported by the finding of a relationship between reward dependence and opioid receptor availability (Schreckenberger et al, 2008). Similar investigations of various facets of serotonergic neurotransmission in healthy volunteers have provided numerous links to levels of anxiety and aggression, as well as the personality traits of harm avoidance and openness to experience (Kalbitzer et al, 2009; Moresco et al, 2002; Soliman et al, 2011; Soloff et al, 2010; Tauscher et al, 2001; Witte et al, 2009). Investigation of individual differences has benefited from the acquisition of large data sets, which was made possible by the standardization of acquisition and quantitative analysis so that data can be combined across numerous studies (Rabiner et al, 2002).
Drug Development
Pharmacology in general and drug development in particular has been an unqualified success area for brain PET imaging. Information derived from PET studies is easily interpreted in pharmacological terms and can be readily incorporated into the drug development process. The PET-derived information can be used to make go/no-go decisions, and has therefore become a routine investigational technique considered by Pharma and Biotech in developing central nervous system (CNS) therapeutics. This has led to considerable investment of ‘Big Pharma' in imaging expertize: the top 12 Pharma companies have internal imaging units and their own preclinical imaging facilities used for ligand development and derisking novel compounds before first-in-human studies. Reciprocally, the greatest impacts the field of drug development has had on brain PET has been in optimizing the quantification of drug interaction with their targets and making use of Pharma compound libraries to develop novel PET radioligands, thus increasing the number of targets that can be examined with PET.
The application of brain PET in industry has focused on the determination of brain penetration and target occupancy of novel compounds in phase I. Such information, though expensive to acquire, produces a significant impact on the overall cost of drug development by eliminating unsuitable molecules at an early stage and refining the dose range tested in late-phase clinical studies. This has been particularly useful for targets such as the D2 receptor and the SERT/5-HTT, where levels of occupancy necessary for clinical efficacy have been established by investigating the occupancy of existing compounds at clinically useful doses (Farde et al, 1988; Meyer et al, 2004).
For targets where a PET radioligand is available, or can be developed, target occupancy studies can be used to quantify drug engagement with its target (Bench et al, 1993). In addition to confirming CNS penetration, measurement of target occupancy at different doses allows the characterization of the plasma target occupancy relationship and can derisk the design of larger phase II and III trials by ensuring dose selection is optimized (Bergström et al, 2004; Searle et al, 2010). Methodological developments derived from kinetic analysis of the drug-target interaction after single dose occupancy studies have enabled prediction of the occupancy that would be observed after repeat dosing (Abanades et al, 2011). Such drug-target occupancy studies have benefited from the development of efficient experimental designs that use sequential adaptive optimal designs to minimize the number of PET scans required (Zamuner et al, 2002).
Direct radiolabeling of novel CNS drugs with 11C and 18F has facilitated ‘microdose' studies. These use tracer amounts of labeled drug to evaluate drug brain penetration and biodistribution in early development phases (Bergstrom et al, 2003, 2006; Kiesewetter et al, 2002) and can prove very useful for investigating the pharmacokinetics of novel drugs designed for targets which have no suitable PET radioligand available. A significant advance in this methodology has been achieved by incorporating in-vitro equilibrium dialysis information from blood and tissue homogenate. In this way free, rather than just total, brain concentration of the drug can be quantified to provide further confidence about whether pharmacological activity will be reached (Gunn et al, 2007).
The lack of appropriate radioligands for many brain targets is a major challenge for PET molecular imaging, both for academic research into understanding disease and for application to drug development. The growing interest in the use of molecular imaging in support of drug development and the accompanying establishment of dedicated molecular imaging groups in companies such as Merck, Pfizer, Novartis, Astra-Zeneca, Roche, Johnson and Johnson, and GlaxoSmithKline have improved the overall rate of ligand discovery. As a result, over the past 10 years, a significant growth has occurred in targets that can be studied with PET, including 5-HT1B receptors, 5-HT4 receptors, H3 receptors, CB-1 receptors, type 1 glycine transporters NPY-Y1, and mGluR1 receptors (Andersson et al, 2011; Ashworth et al, 2010; Gallezot et al, 2010; Hamill et al, 2009; Hostetler et al, 2011a, 2011b; Marner et al, 2009; Passchier et al, 2010; Sanabria-Bohorquez et al, 2012). In addition, encouraging advances have been made recently in design-based biomathematical modeling (Guo et al, 2009), better understanding of factors predicting nonspecific binding (Baciu et al, 2006; Jiang et al, 2011), and new approaches to medicinal and PET chemistry, providing a new set of tools to optimize future radioligand development.
Reflections on the Current Status of Brain Positron Emission Tomography
As documented here, brain PET has made a considerable impact, by providing new information on human brain disorders and normal human brain function over the past 30 years. The unique information that has been produced is substantial, and includes important concept changes. Given the reports from the first decade of its applications, and the increasing biological and medical focus on molecular imaging, translational research, experimental medicine, biomarker discovery and support for drug development, brain PET may be expected to be at the center stage of biomedical research. Layered on this has been the anticipation that the pharmaceutical industry would exploit PET to support drug development, and that new imaging biomarkers would stem from the libraries of compounds residing in pharmaceutical companies. The development of neurotransmitter and enzyme ligands has provided an invaluable experience and a practical blueprint for the development of ligands for other targets. Yet from these premises, brain PET research does not appear to have evolved as extensively as expected. From the overall developments and accumulated experience, it is perceived that brain PET has not been fully exploited. We plotted the studies referenced in this review by year of publication to obtain a visual representation of the progress of both the development of PET methodology and the achievements of the field (Figure 7). Only one reference for a given outcome is scored despite there being, in some cases, a number of publications reporting/reinforcing a given outcome. We stress this analysis has not been based on a systematic review of the literature but on the items and references contained in this review. Nevertheless, we believe this analysis to be of interest, as we consider that we have obtained a representative sample of the perceived highlights of brain PET from a selection of experts in the field. The scoring of the key methodological developments has been done from the perspective of the more immediate applications, based on our own experiences and the feedback received from the 13 nonauthor expert collaborators. While the scoring of some events has been clear, for others it is more subjective and no weight is given to those outcomes, which are more impactful than others. Also, the more recent developments may be underrepresented, as time is needed to fully assess their impact. The reader could create his or her own trend data from the accompanying bibliography. We are fully aware that a large and important area of methodological development is not represented in this data set, namely those that have occurred in radio synthetic chemistry, cyclotrons, and their production targets. For this, we ask forgiveness from our respected colleagues and associates who are and have been active in these areas. However, the ligand and tracer development that have been itemized do reflect to some extent the advances made in these areas. Despite these shortcomings, our analysis does give insight into the trends in the field. Waves of methodological development, as expected, precede waves of the achievements of new information on the human brain. The waves of development in the 1980s and 1990s are largely due to the introduction of new ligands and tracers for brain PET. The data clearly show that the annual achievements produced by brain PET studies are not increasing. The ratio between achievements during a given year and the accumulated methodological developments up to that year has been steady. It rose to a peak in the periods 2000 to 2005 but fell back to a low during the later part of the decade. Despite the accumulation of methodological advances on a number of fronts, radiochemistry, ligand/tracer developments, tomographs, reconstructions, quantification, kinetic modeling, noise reductions, etc, the resulting achievement outcomes have been somewhat constant relative to the methodology developments. Surprisingly, there does not appear to have been an amplification or synergy of the effects of these developments of improved sensitivity and specificity for enhancing the output of new information on the human brain in health and disease. These data reinforce our perception of a lack of initiative and momentum in the field at this time, with a reduction in its interest and application. This is further evidenced by the fact that there has been no new commercial design of a brain dedicated PET camera since 1995. At the 2011 American Academy of Neurology meeting, of the 1,400 oral and 1,900 poster presentations, only ∼1% involved PET, with many of these being [18F]FDG-based studies (Feldmann, 2011). Of the over 500 presentations at the 19th International Symposium on Radiopharmaceutical Science in 2011, only a few percent reported new methodologies for labeling with carbon-11 which is the key label for the small molecules needed as brain PET tracers and ligands (see Table 1). At the 2011 biannual Conference of the International Society of Cerebral Blood Flow and Metabolism (ISCBFM), there were few reports of new impacting information on the human brain based on PET studies. The fact that brain PET procedures have not translated significantly into routine clinical care may be an important contributor to this state of affairs.
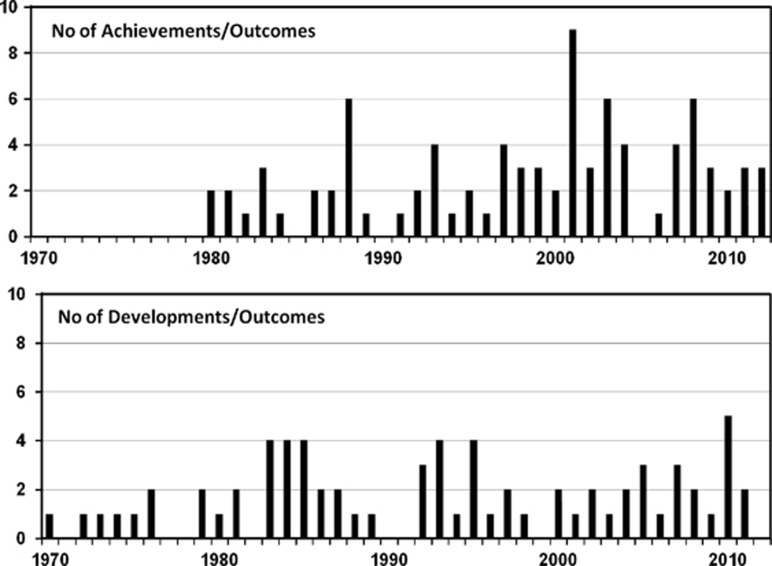
Figure 7.
Chronology plots showing the significant ‘developmental and methodological' outcomes in brain PET and the reporting of ‘achievement' outcomes of new or consensus changing information on the human brain. Only one reference for a given outcome is scored. This analysis has not been based on a systematic review of the literature but on the references contained in this review. A large and important area of methodological developments is not directly represented, namely those that have occurred in radio synthetic chemistry, cyclotrons, and their production targetry.
From the position of those who oversaw the beginning of brain PET as an exciting technique, with massive potential for obtaining unique information on the human brain in both health and disease, its current applications and the lack of excitement in anticipated future expectations are disappointing. This is especially the case given the accumulated methodological advances and the unique information that brain PET can provide for studying the human brain—the most complex biological structure known to humans, the most investigated and the least understood. It needs to be noted that the costs of brain disorders in Europe are near 800 Billion Euros per year (Gustavsson et al, 2011). Brain PET is a unique tool for researching those brain disorders that represent major clinical/economical burdens and for the challenges of understanding the ageing brain in the era of increasing human longevity. Thus, there are compelling factors for increased application of brain PET, a technique with a proven track record for gaining useful and impactful information.
Reasons for Diminished Brain Positron Emission Tomography Research Activity
One reason for reduced interest in brain PET was the introduction of fMRI in 1991. This was stimulated in part by the seminal work of PET-based studies of regional brain activation, and has led to a number of clinical neuroscientists, who were previously leading exponents of brain PET, to move their experimental base to fMRI—a cheaper, simpler, quicker, and more user-friendly method. Although this represented a lost intellectual force from the field of brain PET, brain PET remains unrivaled for the quantification of specific molecular targets. An encouraging development is the growing field of multimodal imaging, whereby the specific molecular approach of PET with the flexibility and superior temporal and spatial resolution of MRI is integrated, and it is hoped that this complementary approach will reinvigorate interactions between these two areas of neuroscience (Rabiner et al, 2011).
The major factors which have hindered widespread application of PET are that it is expensive and has practical implementation difficulties. Positron emission tomography is time consuming, often invasive, and involves exposure to ionizing radiation. Importantly, undertaking meaningful, top of the range PET studies is also a multidisciplinary ‘big science' activity that requires a significant financial investment in technology and highly trained personnel. Worldwide access to such a ‘big science' PET-based institute is very limited: hence, the number of worldwide investigators is currently very restricted. The cost–benefit ratio for top of the range PET is not obviously clear, especially when a short-term analysis is conducted. With this uncertainty, recent history has shown PET institutes to be highly politically vulnerable to takeovers by inexperienced administrative bodies, resulting in the demise of a number of former world-class centers. In recent years, the heightened regulations concerning the administration of material to human subjects and the associated introduction of Good Manufacturing Practice has hindered wider application of PET, with compliance proving difficult, costly, and distracting. From the scientific development and applications points of view, not enough clinical neuroscientists, chemists, and biologists are engaged in brain PET. In summary, despite the considerable number of developments in the methodologies underlying brain PET, they are not translating into applications. It is concluded that this must be due to lack of access to this sophisticated methodology.
Future of Brain Positron Emission Tomography
Areas of Development
Brain PET has made its greatest advances in quantifying metabolism and G-protein coupled receptors in various disease states and after treatment. Similar, though lesser, success has been achieved in the imaging of enzymes, e.g., monoamine oxidase A and B (MAO-A and -B), hexokinase, phosphodiesterase 4 and 10 (PDE4 and 10), fatty acid amide hydrolase (FAAH), and transporters, e.g., dopamine transporter (DAT), serotonin transporter (SERT/5-HTT), norepinephrine transporter (NET), vesicular monoamine transporter type 2 (VMAT2), and vesicular acetylcholine transporter (VAChT). However, it has been singularly unsuccessful in the quantification of ion channels (other than GABA-A), or the intracellular second messenger systems. The quantification of kinase and phosphatase activity and immune processes remains in its infancy, as does the quantification of pathological deposits found in neurodegenerative diseases (e.g., τ-protein and α-synuclein). These targets are of increasing importance in the investigation of brain pathophysiology as well as in the assessment of novel treatments for CNS disorders.
An area of great excitement is the detection of neurotransmitter fluctuations in the living human brain. While this has been well established for the dopamine system (Laruelle, 2000), and has generated valuable new data in understanding its role, extension to other systems has been hampered by the lack of suitable tools. Within the past 10 years, and in particular in the last few, promising tools have been made available for imaging fluctuations in 5-HT (Ridler et al, 2011), endogenous opioids (Zubieta et al, 2001), GABA (Frankle et al, 2009), and glutamate (Miyake et al, 2011). The combination of tissue pharmacokinetic data acquired with PET, with pharmacodynamic data acquired by other functional techniques such as blood oxygen level-dependent fMRI (Rabiner et al, 2011), [18F]FDG PET, and electroencephalography promises to provide added value.
Further suggestions of relevant biological processes that require robust imaging agents to enable their study in the living human brain include:
Downstream effector pathways coupled to neuroreceptors;
Neuroimmunity/inflammation as a factor in brain disease and the role of astrocytes and their associated chemokines;
Transient opening of the BBB as a factor in brain inflammation;
Enhancing the delivery of drugs across the BBB;
Specific imaging markers of neuronal and glial subtypes;
Progenitor stem cell activity and their chemokines for repairing brain damage;
Glioma stem cell activity;
Brain viral and bacterial infections (e.g., herpes encephalitis and tuberculosis);
Brain plasticity, e.g., in stroke recovery;
The neurochemical components underlying memory, learning, maturation, ageing cognitive decline/enhancement, and personality.
The choice of specific targets in the areas proposed above will rest on collaborative interactions between molecular imaging professionals and the wider neuroscience and clinical community. The development of imaging in these novel areas will require a profound understanding of the underlying biology and so the involvement of new researchers with specialized knowledge in these areas is critical. Target interaction studies demand the availability of a radioligand that has good affinity for the target, and binds with high specificity and selectivity (Cunningham et al, 2005). Such ligands exist for many targets in the CNS, however, the discovery of novel biological targets requires the development of novel PET radioligands: a complex and resource-intensive undertaking, which requires highly specialized and skilled staff and complex infrastructure. While the contributions of the pharmaceutical industry to developing specific imaging biomarkers are impressive, there is a case for industries contributing to the development of generic tracers that would enable in-vivo screening of a whole class of drugs. Proactive involvement of professional organizations, such as ISCBFM, will be valuable in engaging clinical neuroscientists to identify areas of need for brain PET application, and to enable a clear definition of the clinical research questions and the biomarkers required to focus future development. Importantly, here the ISCBFM could be instrumental in making the funding agencies aware of the true costs and above all the cost to benefit of undertaking high quality PET studies.
Proposed Strategies to Advance the Future Applications of Brain Positron Emission Tomography
It is of note that PET data collection, reconstruction, presentation, and analysis are somewhat more advanced than the applications. However, going forward, there is still scope for methodological improvements. For example, the manufacturers of PET scanners could be encouraged to implement software for accepted applications so that studies become less cumbersome and time consuming. Increasing the availability of brain-specific tomographs that implement recent technical developments would enhance brain pharmacokinetic measures in microdose studies. The establishment of centralized ‘photo-shops' at international expert centers for specialized quantitative analysis of electronically transferred kinetic PET data could also encourage wider beneficial use of this methodology.
Optimization of Radioligand Development
The development and characterization of radioligands for a novel target is a time and resource-intensive exercise, where success is not guaranteed. The development of comprehensive in-silico and in-vitro assays, which are able to assess a potential molecule's suitability, will go a long way toward improving radioligand development. Traditionally, the assessment of a molecule's suitability focused on a molecule's affinity and specificity for the target, plus its lipophilicity as a predictor of brain penetration and nonspecific binding. The use of in-vitro data in an appropriate biomathematical model to predict the in-vivo performance of a candidate molecule promises to improve the success rate of ligand development activities (Guo et al, 2009). Furthermore, to tighten the results from patient groups and hence reduce the numbers required per study, multitracer studies in the same patient may help to normalize the data.
The pharmaceutical industry is in position to be a major partner in this discovery and development process, both as a user of brain PET to support drug development and as the holder of libraries of candidate radioligands. An encouraging development is the increasing recognition within Pharma and Biotech companies that the development of novel radioligands represents a precompetitive activity, with information sharing within industry and academia promising to advance the field by preventing duplication of effort. Multipartner cooperative initiatives are under way, e.g., the European Innovative Medicine Initiative, which focuses on the development and validation of these tools. The commitment of international biologists and chemists to engage in radioligand development is essential in discovering and converting promising candidate molecules. Such commitment should be possible, given the exciting potential for researching the human brain. But key to mobilizing these scientists is improving the accessibility to short-lived positron emitting radionuclides and the development of easier tracer radiolabeling.
Cyclotron and Radiochemistry Developments
An encouraging approach to improving access to short-lived positron emitting radionuclides is the introduction of low powered microcyclotrons. These emit significantly reduced levels of radiation and promise to be cheaper, quicker to install, and easier to operate in a biology/chemistry laboratory or clinical environment, without the need for a qualified engineer (Nutt et al, 2007). But with the prospect of easier access comes the challenge of using the relatively low radionuclide yields associated with such machines. Research and development will be necessary to refine the hot atom chemistry within the target being bombarded to produce usable yields of the radionuclides, with acceptable specific activity for the radiolabeling of tracer molecules. The small volumes of reagents produced by the microcyclotrons will also need to be handled efficiently and used rapidly. Microfluidics-based chemical reactors offer solutions for these challenges, including the means for rapid online assays and quality control of the radiolabeled products. Assemblies of low cost, integrated systems that are prepackaged and sterilized for ‘single use' will address the Good Manufacturing Practice need for providing material for administering to humans. These methodologies will require a shift from current practises, but it is encouraging to note that at the 2011 19th International Symposium on Radiopharmaceuticals a number of presentations were devoted to microfluidics chemistry. The development of this strategy and resolution of the challenges it encounters will require the attention of world's best chemists. Further, the practical application of microcyclotron and microfluidics to research will need the strategic integration of biology and chemistry input.
Expanding Positron Emission Tomography Applications and Encouraging New Expertize
A greater synergy between brain and out-of-brain imaging is required. Tools developed for one therapeutic area often have applications in another. For example, dopaminergic tracers such as [18F]F-DOPA and [11C]DTBZ are under investigation as tools to detect insulin producing cells in the pancreas (Kapoor et al, 2009; Souza et al, 2006), while oncology targets such as Akt have been found to be of interest in the transduction of G-protein coupled receptor neurotransmission in the brain (Beaulieu et al, 2005). This methodological cross-fertilization can only benefit the PET field as a whole.
An education and training strategy to increase the critical mass of informed practitioners and hence the ‘culture' would be to develop the application of PET across internal medicine. The case for this was revealed in a recent survey across a major Academic Health Science Centre in the UK, which focused on identifying potential future clinical research applications. The results showed that there is an unmet need to address major clinical research questions that could be approached with PET. These were found to cluster around the topics of inflammation, infection, peptides, and stem cell therapy. Diseases identified that could be gainfully researched with PET included: chronic obstructive pulmonary disease, asthma, rheumatoid arthritis, atheroma, diabetes, renal disease, tuberculosis, hepatitis, and HIV (Jones and Long, personal communication). The ‘wish list' of imaging biomarkers proposed to meet these needs focused on ‘biological' macromolecules especially those involving antibody scaffolds. Although such biomarkers have limited interest for the brain, they may be of interest to delineate brain endothelial function and intravascular pathology, such as atheroma. Conversely, there is a case for developing macromolecule-based tracer methods to quantify transient opening of the BBB given the hypothesized role this has in neuroinflamation. Generic radiolabeling of macromolecules with carbon-11, fluorine-18, or gallium-68 may enable a wide repertoire of biomarkers to be developed simultaneously and rapidly. Were the applications of PET to be broadened across internal medicine, PET centers would become more cost effective by extending their scientific collaborative and user base. This would benefit brain PET by increasing the pool of PET active chemists and biologists and the expertize in quantitative data analysis and interpretation. Neuroscientists also need to be encouraged to the brain PET field. Given the relative maturity of the field and its wider application, such a revival would be reinforced by the pharmaceutical and the health care industries as they seek evidence-based data on the efficacy of new therapeutics.
Discussion
The journey of brain PET over the past 35 years shows significant advances in methodology, including tomographs, cyclotron technologies, the discovery of tracers and ligands, radiolabeling of imaging biomarkers, and PET data processing and analysis. An overview of the achievements of brain PET studies shows that there have been a significant number of impacting and concept changing results across a range of important human brain disorders. However, current brain PET research activity is not commensurate with its full potential in translational experimental medicine or health care. The reasons for this have been outlined, but high on the list is the lack of access to this specialized methodology. To invigorate the field, it would be appropriate that bodies like the ISCBFM derive a consensus on areas of clinical neuroscience that could benefit from future brain PET-based research and development. The opportunity for greatly improving access to cyclotron and radiolabeling facilities has been identified and novel developments in low cost, low powered microcyclotrons and microfluidics chemistry may provide such opportunities. Improved access to the field for the international community of chemists and biologists will aid the development of future biomarkers. The possibilities for locating microcyclotron and microfluidics facilities in neurology or psychiatric departments as well as in the pharmaceutical industry could become a reality and with it enhanced exploitation and impact of brain PET research.
The importance of the traditional ‘big science' multidisciplinary PET centers cannot be overestimated. These remain the custodians of the cross-disciplinary approach, which is essential for future PET developments. Such centers, encompassing physics, chemistry, biology, biomathematics, and clinical aspects of PET, offer multidisciplinary cross-fertilization and the ability to undertake complex paradigms and protocols, and could provide the necessary expertize to support the development of new applications of PET. Such facilities are expensive to maintain, but are needed to ensure that developments in individual disciplines are undertaken in the context of producing advances in the field as a whole. We would like to propose that a limited number of national and international centers of excellence are established and maintained to have a coordinating role for smaller satellite centers. An ongoing dialog is envisaged between the ‘big science' centers and the operationally minimalistic brain PET facilities. Novel and complex protocols could be undertaken in the larger groups, with the aim of providing validated simplified procedures that could be translated to the satellite centers. Such ‘big science'/satellite center relationships could traverse international boundaries. This would maximize both ends of the brain PET spectrum and help to justify the funding of the expensive to maintain ‘big science' facilities. Importantly, it would realize the full potential of the expertize that has been developed over the past 35 years, which is primarily confined to the relatively few and alarmingly declining ‘big science' PET centers. If these developments were to happen, the remaining challenge will be to attract the next generation of neurologists, psychiatrists, neurobiologists, and drug developers to commit themselves to this reinvigorated, reemerging speciality, stimulated by the current inertia for more translation from bench to bedside and evidence-based studies on therapeutic efficacies. Finally, the widespread application of oncology PET and MRI is due to their clinical utility. Hence, such a clinical translation for brain PET would certainly help reinvigorate the speciality. Here, the introduction of amyloid plaque imaging may be such an example of a future routine daily clinical use.
Conclusion
Significant advances have been made in brain PET methodologies and its application has gained impacting results in a range of brain disorders, normal brain physiology, and drug development. However, despite its unique strengths and in view of the present needs in translational experimental medicine, PET is currently not achieving its full potential in brain research. Reinvigoration of the field based on major clinical research and health-care questions, along with projected advances in radionuclide production, radiochemistry, and radioligand development would enable brain PET to fully contribute toward beneficial research of the human brain.
Acknowledgments
The authors thank the following contributors to the section on ‘Achievements of Brain PET': Overview of earlier studies, Richard Frackowiak (University of Lausanne, Switzerland); Schizophrenia, Marc Laruelle (Yale University, USA) and Shitij Kapur (Kings College London, UK); Dementia, Kirk Frey (University of Michigan, USA); Epilepsy, Matthias Koepp (University College London, UK); Movement Disorders, David Brooks (Imperial College London, UK); Cerebral Vascular Disease, Jean-Claude Baron (Cambridge University, UK); Addiction, Anne Lingford-Hughes (Imperial College London, UK) and Marc Laruelle (Yale University, USA); Depression and Anxiety, Jeffery Meyer (University of Toronto, Canada) and Gitte Moos Knudsen (University of Copenhagen); Drug Development and Pharmacology, Roger Gunn and Jan Passchier (Imanova Limited, UK, formerly the GSK Clinical Imaging Centre). Also acknowledged is the kind provision of figures from Kirk Frey (University of Michigan, USA), Lars Farde (Karolinka Institute, Sweden), Marcus Raichle (Washington University, USA), and Oliver Howes (Kings College London, UK); and contributory analysis by Maria Feldmann. Manuscript writing assistance was provided by Melanie Green.
The authors declare no conflict of interest.
References
- Abanades S, Van Der Aart J, Barletta JAR, Marzano C, Searle GE, Salinas CA, Ahmad JJ, Reiley RR, Pampols-Maso S, Zamuner S, Cunningham VJ, Rabiner EA, Laruelle MA, Gunn RN. Prediction of repeat-dose occupancy from single-dose data: characterisation of the relationship between plasma pharmacokinetics and brain target occupancy. J Cereb Blood Flow Metab. 2011;31:944–952. doi: 10.1038/jcbfm.2010.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ackerman RH, Correia JA, Alpert NM, Baron JC, Gouliamos A, Grotta JC, Brownell GL, Taveras JM. Positron imaging in ischemic stroke disease using compounds labeled with oxygen 15. Initial results of clinicophysiologic correlations. Arch Neurol. 1981;38:537–543. doi: 10.1001/archneur.1981.00510090031002. [DOI] [PubMed] [Google Scholar]
- Alavi A, Reivich M. Guest editorial: the conception of FDG-PET imaging. Semin Nucl Med. 2002;32:2–5. doi: 10.1053/snuc.2002.29269. [DOI] [PubMed] [Google Scholar]
- Albin RL, Minoshima S, D'Amato CJ, Frey KA, Kuhl DA, Sima AA. Fluoro-deoxyglucose positron emission tomography in diffuse Lewy body disease. Neurology. 1996;47:462–466. doi: 10.1212/wnl.47.2.462. [DOI] [PubMed] [Google Scholar]
- Andersson JD, Pierson ME, Finnema SJ, Gulyas B, Heys R, Elmore CS, Farde L, Halldin C. Development of a PET radioligand for the central 5-HT1B receptor: radiosynthesis and characterization in cynomolgus monkeys of eight radiolabeled compounds. Nucl Med Biol. 2011;38:261–272. doi: 10.1016/j.nucmedbio.2010.08.006. [DOI] [PubMed] [Google Scholar]
- Ashburner J, Haslam J, Taylor C, Cunningham VJ, Jones T.1996A cluster analysis approach for the characterization of dynamic PET data Quantification of brain function using PET(Myers R, Cunningham VJ, Bailey D, Jones T, eds),San Diego: Academic Press; 301–306. [Google Scholar]
- Ashworth S, Rabiner EA, Gunn RN, Plisson C, Wilson AA, Comley RA, Lai RYK, Gee AD, Laruelle M, Cunningham VJ. Evaluation of 11C-GSK189254 as a novel radioligand for the H 3 receptor in humans using PET. J Nucl Med. 2010;51:1021–1029. doi: 10.2967/jnumed.109.071753. [DOI] [PubMed] [Google Scholar]
- Bacher I, Houle S, Xu X, Zawertailo L, Soliman A, Wilson AA, Selby P, George TP, Sacher J, Miler L, Kish SJ, Rusjan P, Meyer JH. Monoamine oxidase A binding in the prefrontal and anterior cingulate cortices during acute withdrawal from heavy cigarette smoking. Arch Gen Psychiatry. 2011;68:817–826. doi: 10.1001/archgenpsychiatry.2011.82. [DOI] [PubMed] [Google Scholar]
- Baciu M, Sebai SC, Ces O, Mulet X, Clarke JA, Shearman GC, Law RV, Templer RH, Plisson C, Parker CA, Gee A. Degradative transport of cationic amphiphilic drugs across phospholipid bilayers. Philos Transact A Math Phys Eng Sci. 2006;364:2597–2614. doi: 10.1098/rsta.2006.1842. [DOI] [PubMed] [Google Scholar]
- Badgaiyan RD, Fischman AJ, Alpert NM. Striatal dopamine release in sequential learning. Neuroimage. 2007;38:549–556. doi: 10.1016/j.neuroimage.2007.07.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron JC, Bousser MG, Comar D, Castaigne P. Crossed cerebellar diaschisis” in human supratentorial brain infarction. Trans Am Neurol Assoc. 1980;105:459–461. [PubMed] [Google Scholar]
- Baron JC, Bousser MG, Comar D, Soussaline F, Castaigne P. Noninvasive tomographic study of cerebral blood flow and oxygen metabolism in vivo. Potentials, limitations, and clinical applications in cerebral ischemic disorders. Eur Neurol. 1981a;20:273–284. doi: 10.1159/000115247. [DOI] [PubMed] [Google Scholar]
- Baron JC, Bousser MG, Rey A, Guillard A, Comar D, Castaigne P. Reversal of focal ‘misery-perfusion syndrome' by extra-intracranial arterial bypass in hemodynamic cerebral ischemia. A case study with 15O positron emission tomography. Stroke. 1981b;12:454–459. doi: 10.1161/01.str.12.4.454. [DOI] [PubMed] [Google Scholar]
- Baron JC, Comar D, Soussaline F, Todd-Pokropek AE, Bousser MG, Castaigne P, Kellersholhn C. Continuous 15O inhalation technique: an attempt to quantify CBF, EO2 and CMRO2. Acta Neurol Scand. 1979;60:194–195. [Google Scholar]
- Baron JC, Jones T.2011Oxygen metabolism, oxygen extraction and positron emission tomography: historical perspective and impact on basic and clinical neuroscience Neuroimagee-pub ahead of print) [DOI] [PubMed]
- Baron JC, Rougemont D, Soussaline F, Bustany P, Crouzel C, Bousser MG, Comar D. Local interrelationships of cerebral oxygen consumption and glucose utilization in normal subjects and in ischemic stroke patients: a positron tomography study. J Cereb Blood Flow Metab. 1984;4:140–149. doi: 10.1038/jcbfm.1984.22. [DOI] [PubMed] [Google Scholar]
- Barrio JR, Keen RE, Ropchan JR, MacDonald NS, Baumgartner FJ, Padgett HC, Phelps ME. L-[1-11C]leucine: routine synthesis by enzymatic resolution. J Nucl Med. 1983;24:515–521. [PubMed] [Google Scholar]
- Bartenstein PA, Duncan JS, Prevett MC, Cunningham VJ, Fish DR, Jones AK, Luthra SK, Sawle GV, Brooks DJ. Investigation of the opioid system in absence seizures with positron emission tomography. J Neurol Neurosurg Psychiatry. 1993;56:1295–1302. doi: 10.1136/jnnp.56.12.1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaulieu JM, Sotnikova TD, Marion S, Lefkowitz RJ, Gainetdinov RR, Caron MG. An Akt/beta-arrestin 2/PP2A signaling complex mediates dopaminergic neurotransmission and behavior. Cell. 2005;122:261–273. doi: 10.1016/j.cell.2005.05.012. [DOI] [PubMed] [Google Scholar]
- Bench CJ, Lammertsma AA, Dolan RJ, Grasby PM, Warrington SJ, Gunn K, Cuddigan M, Turton DJ, Osman S, Frackowiak RSJ. Dose dependent occupancy of central dopamine D2 receptors by the novel neuroleptic CP-88,059-01: a study using positron emission tomography and 11C-raclopride. Psychopharmacology. 1993;112:308–314. doi: 10.1007/BF02244926. [DOI] [PubMed] [Google Scholar]
- Benson DF, Kuhl DE, Hawkins RA, Phelps ME, Cummings JL, Tsai SY. The fluorodeoxyglucose 18F scan in Alzheimer's disease and multi-infarct dementia. Arch Neurol. 1983;40:711–714. doi: 10.1001/archneur.1983.04050110029003. [DOI] [PubMed] [Google Scholar]
- Bergstrom M, Collins VP, Ehrin E, Ericson K, Eriksson L, Greitz T, Halldin C, von Holst H, Langstrom B, Lilja A, Lundqvist H, Nagren K. Discrepancies in brain tumor extent as shown by computed tomography and positron emission tomography using [68Ga]EDTA, [11C]glucose, and [11C]methionine. J Comput Assist Tomogr. 1983;7:1062–1066. doi: 10.1097/00004728-198312000-00022. [DOI] [PubMed] [Google Scholar]
- Bergstrom M, Grahnen A, Langstrom B. Positron emission tomography microdosing: a new concept with application in tracer and early clinical drug development. Eur J Clin Pharmacol. 2003;59:357–366. doi: 10.1007/s00228-003-0643-x. [DOI] [PubMed] [Google Scholar]
- Bergström M, Hargreaves RJ, Burns HD, Goldberg MR, Sciberras D, Reines SA, Petty KJ, Ögren M, Antoni G, Långström B, Eskola O, Scheinin M, Solin O, Majumdar AK, Constanzer ML, Battisti WP, Bradstreet TE, Gargano C, Hietala J. Human positron emission tomography studies of brain neurokinin 1 receptor occupancy by aprepitant. Biol Psychiatry. 2004;55:1007–1012. doi: 10.1016/j.biopsych.2004.02.007. [DOI] [PubMed] [Google Scholar]
- Bergstrom M, Yates R, Wall A, Kagedal M, Syvanen S, Langstrom B. Blood-brain barrier penetration of zolmitriptan—Modelling of positron emission tomography data. J Pharmacokinet Pharmacodyn. 2006;33:75–91. doi: 10.1007/s10928-005-9001-1. [DOI] [PubMed] [Google Scholar]
- Bernow N, Yakushev I, Landvogt C, Buchholz HG, Smolka MN, Bartenstein P, Lieb K, Grunder G, Vernaleken I, Schreckenberger M, Fehr C. Dopamine D2/D3 receptor availability and venturesomeness. Psychiatry Res. 2011;193:80–84. doi: 10.1016/j.pscychresns.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Bhagwagar Z, Hinz R, Taylor M, Fancy S, Cowen P, Grasby P. Increased 5-HT(2A) receptor binding in euthymic, medication-free patients recovered from depression: a positron emission study with [(11)C]MDL 100,907. Am J Psychiatry. 2006;163:1580–1587. doi: 10.1176/ajp.2006.163.9.1580. [DOI] [PubMed] [Google Scholar]
- Bhagwagar Z, Rabiner EA, Sargent PA, Grasby PM, Cowen PJ. Persistent reductions in brain serotonin1A receptor binding in recovered depressed men measured by positron emission tomography with [11C]WAY-100635. Mol Psychiatry. 2004;9:386–392. doi: 10.1038/sj.mp.4001401. [DOI] [PubMed] [Google Scholar]
- Bohnen NI, Kaufer DI, Ivanco LS, Lopresti B, Koeppe RA, Davis JG, Mathis CA, Moore RY, DeKosky ST. Cortical cholinergic function is more severely affected in parkinsonian dementia than in Alzheimer disease: an in vivo positron emission tomographic study. Arch Neurol. 2003;60:1745–1748. doi: 10.1001/archneur.60.12.1745. [DOI] [PubMed] [Google Scholar]
- Bouvard S, Costes N, Bonnefoi F, Lavenne F, Mauguiere F, Delforge J, Ryvlin P. Seizure-related short-term plasticity of benzodiazepine receptors in partial epilepsy: a [11C]flumazenil-PET study. Brain. 2005;128:1330–1343. doi: 10.1093/brain/awh470. [DOI] [PubMed] [Google Scholar]
- Breier A, Kestler L, Adler C, Elman I, Wiesenfeld N, Malhotra A, Pickar D. Dopamine D2 receptor density and personal detachment in healthy subjects. Am J Psychiatry. 1998;155:1440–1442. doi: 10.1176/ajp.155.10.1440. [DOI] [PubMed] [Google Scholar]
- Breier A, Su TP, Saunders R, Carson RE, Kolachana BS, de Bartolomeis A, Weinberger DR, Weisenfeld N, Malhotra AK, Eckelman WC, Pickar D. Schizophrenia is associated with elevated amphetamine-induced synaptic dopamine concentrations: evidence from a novel positron emission tomography method. Proc Natl Acad Sci USA. 1997;94:2569–2574. doi: 10.1073/pnas.94.6.2569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownell GL, Sweet WH. Localization of brain tumours with positron emitters. Nucleonics. 1953;11:40–45. [Google Scholar]
- Burke JF, Albin RL, Koeppe RA, Giordani B, Kilbourn MR, Gilman S, Frey KA. Assessment of mild dementia with amyloid and dopamine terminal positron emission tomography. Brain. 2011;134:1647–1657. doi: 10.1093/brain/awr089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnham CA, Brownell GL. A multi-crystal positron camera. IEEE Trans Nucl Sci. 1972;19:201–205. [Google Scholar]
- Cagnin A, Brooks DJ, Kennedy AM, Gunn RN, Myers R, Turkheimer FE, Jones T, Banati RB. In-vivo measurement of activated microglia in dementia. Lancet. 2001;358:461–467. doi: 10.1016/S0140-6736(01)05625-2. [DOI] [PubMed] [Google Scholar]
- Calautti C, Leroy F, Guincestre JY, Baron JC. Dynamics of motor network overactivation after striatocapsular stroke: a longitudinal PET study using a fixed-performance paradigm. Stroke. 2001;32:2534–2542. doi: 10.1161/hs1101.097401. [DOI] [PubMed] [Google Scholar]
- Carson RE.2003Tracer kinetic modeling in PET Positron emission tomography: basic science and clinical practice(Valk PE, Bailey D, Townsend DW, Maisey MN, eds). London: Springer-Verlag [Google Scholar]
- Casey ME, Nutt R. A multicrystal two dimensional BGO detector system for positron emission tomography. IEEE Trans Nucl Sci. 1986;33:460–463. [Google Scholar]
- Cervenka S, Backman L, Cselenyi Z, Halldin C, Farde L. Associations between dopamine D2-receptor binding and cognitive performance indicate functional compartmentalization of the human striatum. Neuroimage. 2008;40:1287–1295. doi: 10.1016/j.neuroimage.2007.12.063. [DOI] [PubMed] [Google Scholar]
- Chen W, Cloughesy T, Kamdar N, Satyamurthy N, Bergsneider M, Liau L, Mischel P, Czernin J, Phelps ME, Silverman DH. Imaging proliferation in brain tumors with 18F-FLT PET: comparison with 18F-FDG. J Nucl Med. 2005;46:945–952. [PubMed] [Google Scholar]
- Cherry SR, Shao Y, Siegel S, Silverman RW, Meadors K, Young J, Jones WF, Newport D, Mooyers C, Mumcuoglu EU, Chatziioannou A, Farquhar T, Andreaco M, Paulus M, Binkley D, Nutt R, Phelps ME. MicroPET: a high resolution PET scanner for imaging small animals. IEEE Nuclear Science Symposium (Conference Record) 1996;2:1120–4. [Google Scholar]
- Chesler DA.1973Positron tomography and three-dimensional reconstruction Tomographic imaging in nuclear medicine(Freedman GS, ed).New York: Society of Nuclear Medicine [Google Scholar]
- Chollet F, DiPiero V, Wise RJ, Brooks DJ, Dolan RJ, Frackowiak RS. The functional anatomy of motor recovery after stroke in humans: a study with positron emission tomography. Ann Neurol. 1991;29:63–71. doi: 10.1002/ana.410290112. [DOI] [PubMed] [Google Scholar]
- Christian BT, Vandehey NT, Floberg JM, Mistretta CA. Dynamic PET denoising with HYPR processing. J Nucl Med. 2010;51:1147–1154. doi: 10.2967/jnumed.109.073999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chugani HT, Kumar A, Kupsky W, Asano E, Sood S, Juhasz C. Clinical and histopathologic correlates of 11C-alpha-methyl-L-tryptophan (AMT) PET abnormalities in children with intractable epilepsy. Epilepsia. 2011;52:1692–1698. doi: 10.1111/j.1528-1167.2011.03103.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chugani HT, Phelps ME. Maturational changes in cerebral function in infants determined by 18FDG positron emission tomography. Science. 1986;231:840–843. doi: 10.1126/science.3945811. [DOI] [PubMed] [Google Scholar]
- Coope DJ, Cizek J, Eggers C, Vollmar S, Heiss WD, Herholz K. Evaluation of primary brain tumors using 11C-methionine PET with reference to a normal methionine uptake map. J Nucl Med. 2007;48:1971–1980. doi: 10.2967/jnumed.107.043240. [DOI] [PubMed] [Google Scholar]
- Cunningham VJ, Jones T. Spectral analysis of dynamic PET studies. J Cereb Blood Flow Metab. 1993;13:15–23. doi: 10.1038/jcbfm.1993.5. [DOI] [PubMed] [Google Scholar]
- Cunningham VJ, Parker CA, Rabiner EA, Gee AD, Gunn RN. PET studies in drug development: methodological considerations. Drug Discov Today Technol. 2005;2:311–315. doi: 10.1016/j.ddtec.2005.11.003. [DOI] [PubMed] [Google Scholar]
- de la Fuente-Fernandez R, Ruth TJ, Sossi V, Schulzer M, Calne DB, Stoessl AJ. Expectation and dopamine release: mechanism of the placebo effect in Parkinson's disease. Science. 2001;293:1164–1166. doi: 10.1126/science.1060937. [DOI] [PubMed] [Google Scholar]
- Di Chiro G, Oldfield E, Wright DC, De Michele D, Katz DA, Patronas NJ, Doppman JL, Larson SM, Ito M, Kufta CV. Cerebral necrosis after radiotherapy and/or intraarterial chemotherapy for brain tumors: PET and neuropathologic studies. AJR Am J Roentgenol. 1988;150:189–197. doi: 10.2214/ajr.150.1.189. [DOI] [PubMed] [Google Scholar]
- Diksic M, Sako K, Feindel W, Kato A, Yamamoto YL, Farrokhzad S, Thompson C. Pharmacokinetics of positron-labeled 1,3-bis(2-chloroethyl)nitrosourea in human brain tumors using positron emission tomography. Cancer Res. 1984;44:3120–3124. [PubMed] [Google Scholar]
- Doder M, Rabiner EA, Turjanski N, Lees AJ, Brooks DJ. Tremor in Parkinson's disease and serotonergic dysfunction: an 11C-WAY 100635 PET study. Neurology. 2003;60:601–605. doi: 10.1212/01.wnl.0000031424.51127.2b. [DOI] [PubMed] [Google Scholar]
- Dolan RJ, Fink GR, Rolls E, Booth M, Holmes A, Frackowiak RS, Friston KJ. How the brain learns to see objects and faces in an impoverished context. Nature. 1997;389:596–599. doi: 10.1038/39309. [DOI] [PubMed] [Google Scholar]
- Drevets WC, Frank E, Price JC, Kupfer DJ, Holt D, Greer PJ, Huang Y, Gautier C, Mathis C. PET imaging of serotonin 1A receptor binding in depression. Biol Psychiatry. 1999;46:1375–1387. doi: 10.1016/s0006-3223(99)00189-4. [DOI] [PubMed] [Google Scholar]
- Eidelberg D, Moeller JR, Dhawan V, Spetsieris P, Takikawa S, Ishikawa T, Chaly T, Robeson W, Margouleff D, Przedborski S, Fahn S. The metabolic topography of parkinsonism. J Cereb Blood Flow Metab. 1994;14:783–801. doi: 10.1038/jcbfm.1994.99. [DOI] [PubMed] [Google Scholar]
- Farde L. The advantage of using positron emission tomography in drug research. Trends Neurosci. 1996;19:211–214. doi: 10.1016/0166-2236(96)40002-9. [DOI] [PubMed] [Google Scholar]
- Farde L, Gustavsson JP, Jonsson E. D2 dopamine receptors and personality traits. Nature. 1997;385:590. doi: 10.1038/385590a0. [DOI] [PubMed] [Google Scholar]
- Farde L, Nordstrom AL, Wiesel FA, Pauli S, Halldin C, Sedvall G. Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine. Relation to extrapyramidal side effects. Arch Gen Psychiatry. 1992;49:538–544. doi: 10.1001/archpsyc.1992.01820070032005. [DOI] [PubMed] [Google Scholar]
- Farde L, Wiesel FA, Halldin C, Sedvall G. Central D2-dopamine receptor occupancy in schizophrenic patients treated with antipsychotic drugs. Arch Gen Psychiatry. 1988;45:71–76. doi: 10.1001/archpsyc.1988.01800250087012. [DOI] [PubMed] [Google Scholar]
- Feigin A, Leenders KL, Moeller JR, Missimer J, Kuenig G, Spetsieris P, Antonini A, Eidelberg D. Metabolic network abnormalities in early Huntington's disease: an [(18)F]FDG PET study. J Nucl Med. 2001;42:1591–1595. [PubMed] [Google Scholar]
- Feigin A, Tang C, Ma Y, Mattis P, Zgaljardic D, Guttman M, Paulsen JS, Dhawan V, Eidelberg D. Thalamic metabolism and symptom onset in preclinical Huntington's disease. Brain. 2007;130:2858–2867. doi: 10.1093/brain/awm217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldmann M.2011. Personal communication
- Fox PT, Burton H, Raichle ME. Mapping human somatosensory cortex with positron emission tomography. J Neurosurg. 1987a;67:34–43. doi: 10.3171/jns.1987.67.1.0034. [DOI] [PubMed] [Google Scholar]
- Fox PT, Miezin FM, Allman JM, Van Essen DC, Raichle ME. Retinotopic organization of human visual cortex mapped with positron-emission tomography. J Neurosci. 1987b;7:913–922. doi: 10.1523/JNEUROSCI.07-03-00913.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox PT, Raichle ME. Focal physiological uncoupling of cerebral blood flow and oxidative metabolism during somatosensory stimulation in human subjects. Proc Natl Acad Sci USA. 1986;83:1140–1144. doi: 10.1073/pnas.83.4.1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frackowiak RS, Lenzi GL, Jones T, Heather JD. Quantitative measurement of regional cerebral blood flow and oxygen metabolism in man using 15O and positron emission tomography: theory, procedure, and normal values. J Comput Assist Tomogr. 1980;4:727–736. doi: 10.1097/00004728-198012000-00001. [DOI] [PubMed] [Google Scholar]
- Frackowiak RS, Pozzilli C, Legg NJ, Du Boulay GH, Marshall J, Lenzi GL, Jones T. Regional cerebral oxygen supply and utilization in dementia. A clinical and physiological study with oxygen-15 and positron tomography. Brain. 1981;104:753–778. doi: 10.1093/brain/104.4.753. [DOI] [PubMed] [Google Scholar]
- Frankle WG, Cho RY, Narendran R, Mason NS, Vora S, Litschge M, Price JC, Lewis DA, Mathis CA. Tiagabine increases [11C]flumazenil binding in cortical brain regions in healthy control subjects. Neuropsychopharmacology. 2009;34:624–633. doi: 10.1038/npp.2008.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freed CR, Greene PE, Breeze RE, Tsai WY, DuMouchel W, Kao R, Dillon S, Winfield H, Culver S, Trojanowski JQ, Eidelberg D, Fahn S. Transplantation of embryonic dopamine neurons for severe Parkinson's disease. N Engl J Med. 2001;344:710–719. doi: 10.1056/NEJM200103083441002. [DOI] [PubMed] [Google Scholar]
- Freeman TB, Olanow CW, Hauser RA, Nauert GM, Smith DA, Borlongan CV, Sanberg PR, Holt DA, Kordower JH, Vingerhoets FJ, Snow BJ, Calne DB, Gauger LL. Bilateral fetal nigral transplantation into the postcommissural putamen in Parkinson's disease. Ann Neurol. 1995;38:379–388. doi: 10.1002/ana.410380307. [DOI] [PubMed] [Google Scholar]
- Freis ED. Mental depression in hypertensive patients treated for long periods with large doses of reserpine. N Engl J Med. 1954;251:1006–1008. doi: 10.1056/NEJM195412162512504. [DOI] [PubMed] [Google Scholar]
- Friedland RP, Budinger TF, Ganz E, Yano Y, Mathis CA, Koss B, Ober BA, Huesman RH, Derenzo SE. Regional cerebral metabolic alterations in dementia of the Alzheimer type: positron emission tomography with [18F]fluorodeoxyglucose. J Comput Assist Tomogr. 1983;7:590–598. doi: 10.1097/00004728-198308000-00003. [DOI] [PubMed] [Google Scholar]
- Friston KJ, Holmes AP, Worsley KJ, Poline J-P, Frith CD, Frackowiak RSJ. Statistical parametric maps in functional imaging: a general linear approach. Hum Brain Mapp. 1994;2:189–210. [Google Scholar]
- Frokjaer VG, Mortensen EL, Nielsen FA, Haugbol S, Pinborg LH, Adams KH, Svarer C, Hasselbalch SG, Holm S, Paulson OB, Knudsen GM. Frontolimbic serotonin 2A receptor binding in healthy subjects is associated with personality risk factors for affective disorder. Biol Psychiatry. 2008;63:569–576. doi: 10.1016/j.biopsych.2007.07.009. [DOI] [PubMed] [Google Scholar]
- Frokjaer VG, Vinberg M, Erritzoe D, Baare W, Holst KK, Mortensen EL, Arfan H, Madsen J, Jernigan TL, Kessing LV, Knudsen GM. Familial risk for mood disorder and the personality risk factor, neuroticism, interact in their association with frontolimbic serotonin 2A receptor binding. Neuropsychopharmacology. 2010;35:1129–1137. doi: 10.1038/npp.2009.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frokjaer VG, Vinberg M, Erritzoe D, Svarer C, Baare W, Budtz-Joergensen E, Madsen K, Madsen J, Kessing LV, Knudsen GM. High familial risk for mood disorder is associated with low dorsolateral prefrontal cortex serotonin transporter binding. Neuroimage. 2009;46:360–366. doi: 10.1016/j.neuroimage.2009.02.008. [DOI] [PubMed] [Google Scholar]
- Frost JJ, Mayberg HS, Fisher RS, Douglass KH, Dannals RF, Links JM, Wilson AA, Ravert HT, Rosenbaum AE, Snyder SH, Wagner HN., Jr Mu-opiate receptors measured by positron emission tomography are increased in temporal lobe epilepsy. Ann Neurol. 1988;23:231–237. doi: 10.1002/ana.410230304. [DOI] [PubMed] [Google Scholar]
- Gallezot JD, Nabulsi N, Neumeister A, Planeta-Wilson B, Williams WA, Singhal T, Kim S, Maguire RP, McCarthy T, Frost JJ, Huang Y, Ding YS, Carson RE. Kinetic modeling of the serotonin 5-HT(1B) receptor radioligand [(11)C]P943 in humans. J Cereb Blood Flow Metab. 2010;30:196–210. doi: 10.1038/jcbfm.2009.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnett ES, Firnau G, Nahmias C. Dopamine visualized in the basal ganglia of living man. Nature. 1983;305:137–138. doi: 10.1038/305137a0. [DOI] [PubMed] [Google Scholar]
- Garraux G, Peigneux P, Carson RE, Hallett M. Task-related interaction between basal ganglia and cortical dopamine release. J Neurosci. 2007;27:14434–14441. doi: 10.1523/JNEUROSCI.1595-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerhard A, Schwarz J, Myers R, Wise R, Banati RB. Evolution of microglial activation in patients after ischemic stroke: a [11C](R)-PK11195 PET study. Neuroimage. 2005;24:591–595. doi: 10.1016/j.neuroimage.2004.09.034. [DOI] [PubMed] [Google Scholar]
- Gibbs JM, Wise RJ, Leenders KL, Jones T. Evaluation of cerebral perfusion reserve in patients with carotid-artery occlusion. Lancet. 1984;1:310–314. doi: 10.1016/s0140-6736(84)90361-1. [DOI] [PubMed] [Google Scholar]
- Ginovart N, Meyer JH, Boovariwala A, Hussey D, Rabiner EA, Houle S, Wilson AA. Positron emission tomography quantification of [11C]-harmine binding to monoamine oxidase-A in the human brain. J Cereb Blood Flow Metab. 2006;26:330–344. doi: 10.1038/sj.jcbfm.9600197. [DOI] [PubMed] [Google Scholar]
- Goerendt IK, Messa C, Lawrence AD, Grasby PM, Piccini P, Brooks DJ. Dopamine release during sequential finger movements in health and Parkinson's disease: a PET study. Brain. 2003;126:312–325. doi: 10.1093/brain/awg035. [DOI] [PubMed] [Google Scholar]
- Goffin K, Van Paesschen W, Van Laere K. In vivo activation of endocannabinoid system in temporal lobe epilepsy with hippocampal sclerosis. Brain. 2011;134:1033–1040. doi: 10.1093/brain/awq385. [DOI] [PubMed] [Google Scholar]
- Greenwald MK, Johanson CE, Moody DE, Woods JH, Kilbourn MR, Koeppe RA, Schuster CR, Zubieta JK. Effects of buprenorphine maintenance dose on mu-opioid receptor availability, plasma concentrations, and antagonist blockade in heroin-dependent volunteers. Neuropsychopharmacology. 2003;28:2000–2009. doi: 10.1038/sj.npp.1300251. [DOI] [PubMed] [Google Scholar]
- Guadagno JV, Jones PS, Aigbirhio FI, Wang D, Fryer TD, Day DJ, Antoun N, Nimmo-Smith I, Warburton EA, Baron JC. Selective neuronal loss in rescued penumbra relates to initial hypoperfusion. Brain. 2008;131:2666–2678. doi: 10.1093/brain/awn175. [DOI] [PubMed] [Google Scholar]
- Gunn RN, Lammertsma AA, Hume SP, Cunningham VJ. Parametric imaging of ligand-receptor binding in PET using a simplified reference region model. Neuroimage. 1997;6:279–287. doi: 10.1006/nimg.1997.0303. [DOI] [PubMed] [Google Scholar]
- Gunn RN, Salinas CA, Read KR, Searle G, Ruffo AD, Parker CA, Stevens AJ, Bonasera T, Jeffrey PM, Laruelle MA. Combining PET and equilibrium dialysis to assess blood-brain-barrier transport. J Cereb Blood Flow Metab. 2007;27:4–14. [Google Scholar]
- Guo Q, Brady M, Gunn RN. A biomathematical modeling approach to central nervous system radioligand discovery and development. J Nucl Med. 2009;50:1715–1723. doi: 10.2967/jnumed.109.063800. [DOI] [PubMed] [Google Scholar]
- Gustavsson A, Svensson M, Jacobi F, Allgulander C, Alonso J, Beghi E, Dodel R, Ekman M, Faravelli C, Fratiglioni L, Gannon B, Jones DH, Jennum P, Jordanova A, Jönsson L, Karampampa K, Knapp M, Kobelt G, Kurth T, Lieb R, Linde M, Ljungcrantz C, Maercker A, Melin B, Moscarelli M, Musayev A, Norwood F, Preisig M, Pugliatti M, Rehm J, Salvador-Carulla L, Schlehofer B, Simon R, Steinhausen H-C, Stovner LJ, Vallat J-M, den Bergh PV, van Os J, Vos P, Xu W, Wittchen H-U, Jönsson B, Olesen J. Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21:718–779. doi: 10.1016/j.euroneuro.2011.08.008. [DOI] [PubMed] [Google Scholar]
- Hamill TG, Lin LS, Hagmann W, Liu P, Jewell J, Sanabria S, Eng W, Ryan C, Fong TM, Connolly B, Vanko A, Hargreaves R, Goulet MT, Burns HD. PET imaging studies in rhesus monkey with the cannabinoid-1 (CB1) receptor ligand [11C]CB-119. Mol Imaging Biol. 2009;11:246–252. doi: 10.1007/s11307-008-0194-8. [DOI] [PubMed] [Google Scholar]
- Hammers A, Asselin MC, Hinz R, Kitchen I, Brooks DJ, Duncan JS, Koepp MJ. Upregulation of opioid receptor binding following spontaneous epileptic seizures. Brain. 2007;130:1009–1016. doi: 10.1093/brain/awm012. [DOI] [PubMed] [Google Scholar]
- Hammers A, Koepp MJ, Richardson MP, Labbe C, Brooks DJ, Cunningham VJ, Duncan JS. Central benzodiazepine receptors in malformations of cortical development: a quantitative study. Brain. 2001;124:1555–1565. doi: 10.1093/brain/124.8.1555. [DOI] [PubMed] [Google Scholar]
- Heinz A, Reimold M, Wrase J, Hermann D, Croissant B, Mundle G, Dohmen BM, Braus DF, Schumann G, Machulla HJ, Bares R, Mann K. Correlation of stable elevations in striatal mu-opioid receptor availability in detoxified alcoholic patients with alcohol craving: a positron emission tomography study using carbon 11-labeled carfentanil. Arch Gen Psychiatry. 2005a;62:57–64. doi: 10.1001/archpsyc.62.1.57. [DOI] [PubMed] [Google Scholar]
- Heinz A, Siessmeier T, Wrase J, Buchholz HG, Grunder G, Kumakura Y, Cumming P, Schreckenberger M, Smolka MN, Rosch F, Mann K, Bartenstein P. Correlation of alcohol craving with striatal dopamine synthesis capacity and D2/3 receptor availability: a combined [18F]DOPA and [18F]DMFP PET study in detoxified alcoholic patients. Am J Psychiatry. 2005b;162:1515–1520. doi: 10.1176/appi.ajp.162.8.1515. [DOI] [PubMed] [Google Scholar]
- Heiss WD, Kracht LW, Thiel A, Grond M, Pawlik G. Penumbral probability thresholds of cortical flumazenil binding and blood flow predicting tissue outcome in patients with cerebral ischaemia. Brain. 2001;124:20–29. doi: 10.1093/brain/124.1.20. [DOI] [PubMed] [Google Scholar]
- Herholz K. Cerebral glucose metabolism in preclinical and prodromal Alzheimer's disease. Expert Rev Neurother. 2010;10:1667–1673. doi: 10.1586/ern.10.136. [DOI] [PubMed] [Google Scholar]
- Hietala J, Syvalahti E, Vuorio K, Rakkolainen V, Bergman J, Haaparanta M, Solin O, Kuoppamaki M, Kirvela O, Ruotsalainen U, Vuorio K, Rakkolainen V, Bergman J, Solin O, Kirvela O, Salokangas RKR. Presynaptic dopamine function in striatum of neuroleptic-naive schizophrenic patients. Lancet. 1995;346:1130–1131. doi: 10.1016/s0140-6736(95)91801-9. [DOI] [PubMed] [Google Scholar]
- Hilker R, Thomas AV, Klein JC, Weisenbach S, Kalbe E, Burghaus L, Jacobs AH, Herholz K, Heiss WD. Dementia in Parkinson disease. Neurology. 2005;65:1716–1722. doi: 10.1212/01.wnl.0000191154.78131.f6. [DOI] [PubMed] [Google Scholar]
- Hoffman EJ, Huang SC, Phelps ME. Quantitation in positron emission computed tomography: 1. Effect of object size. J Comput Assist Tomogr. 1979;3:299–308. doi: 10.1097/00004728-197906000-00001. [DOI] [PubMed] [Google Scholar]
- Hostetler ED, Eng W, Joshi AD, Sanabria-Bohorquez S, Kawamoto H, Ito S, O'Malley S, Krause S, Ryan C, Patel S, Williams M, Riffel K, Suzuki G, Ozaki S, Ohta H, Cook J, Burns HD, Hargreaves R. Synthesis, characterization, and monkey PET studies of [(1)F]MK-1312, a PET tracer for quantification of mGluR1 receptor occupancy by MK-5435. Synapse. 2011a;65:125–135. doi: 10.1002/syn.20826. [DOI] [PubMed] [Google Scholar]
- Hostetler ED, Sanabria-Bohorquez S, Fan H, Zeng Z, Gantert L, Williams M, Miller P, O'Malley S, Kameda M, Ando M, Sato N, Ozaki S, Tokita S, Ohta H, Williams D, Sur C, Cook JJ, Burns HD, Hargreaves R. Synthesis, characterization, and monkey positron emission tomography (PET) studies of [18F]Y1-973, a PET tracer for the neuropeptide Y Y1 receptor. Neuroimage. 2011b;54:2635–2642. doi: 10.1016/j.neuroimage.2010.11.014. [DOI] [PubMed] [Google Scholar]
- Howes OD, Montgomery AJ, Asselin MC, Murray RM, Valli I, Tabraham P, Bramon-Bosch E, Valmaggia L, Johns L, Broome M, McGuire PK, Grasby PM. Elevated striatal dopamine function linked to prodromal signs of schizophrenia. Arch Gen Psychiatry. 2009;66:13–20. doi: 10.1001/archgenpsychiatry.2008.514. [DOI] [PubMed] [Google Scholar]
- Hubner KF, Krauss S, Washburn LC, Gibbs WD, Holloway EC. Tumor detection with 1-aminocyclopentane and 1-aminocyclobutane C-11-carboxylic acid using positron emission computerized tomography. Clin Nucl Med. 1981;6:249–252. doi: 10.1097/00003072-198106000-00004. [DOI] [PubMed] [Google Scholar]
- Ido T, Wan CN, Casella V, Fowler JS, Wolf AP, Reivich M, Kuhl DE. Labeled 2-deoxy-D-glucose analogs. 18F-labeled 2-deoxy-2-fluoro-D-glucose, 2-deoxy-2-fluoro-D-mannose and 14C-2-deoxy-2-fluoro-D-glucose. J Labelled Comp Radiopharm. 1978;14:175–183. [Google Scholar]
- Ishii K, Sakamoto S, Sasaki M, Kitagaki H, Yamaji S, Hashimoto M, Imamura T, Shimomura T, Hirono N, Mori E. Cerebral glucose metabolism in patients with frontotemporal dementia. J Nucl Med. 1998;39:1875–1878. [PubMed] [Google Scholar]
- Jack CR, Jr, Wiste HJ, Vemuri P, Weigand SD, Senjem ML, Zeng G, Bernstein MA, Gunter JL, Pankratz VS, Aisen PS, Weiner MW, Petersen RC, Shaw LM, Trojanowski JQ, Knopman DS. Brain beta-amyloid measures and magnetic resonance imaging atrophy both predict time-to-progression from mild cognitive impairment to Alzheimer's disease. Brain. 2010;133:3336–3348. doi: 10.1093/brain/awq277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang Z, Reilly J, Everatt B, Briard E. A rapid vesicle electrokinetic chromatography method for the in vitro prediction of non-specific binding for potential PET ligands. J Pharm Biomed Anal. 2011;54:722–729. doi: 10.1016/j.jpba.2010.11.004. [DOI] [PubMed] [Google Scholar]
- Johnson S, Stockmeier CA, Meyer JH, Austin MC, Albert PR, Wang J, May WL, Rajkowska G, Overholser JC, Jurjus G, Dieter L, Johnson C, Sittman DB, Ou XM. The reduction of R1, a novel repressor protein for monoamine oxidase a, in major depressive disorder. Neuropsychopharmacology. 2011;36:2139–2148. doi: 10.1038/npp.2011.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones T, Chesler DA, Ter-Pogossian MM. The continuous inhalation of oxygen-15 for assessing regional oxygen extraction in the brain of man. Br J Radiol. 1976;49:339–343. doi: 10.1259/0007-1285-49-580-339. [DOI] [PubMed] [Google Scholar]
- Kadrmas DJ, Casey ME, Conti M, Jakoby BW, Lois C, Townsend DW. Impact of time-of-flight on PET tumor detection. J Nucl Med. 2009;50:1315–1323. doi: 10.2967/jnumed.109.063016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalbitzer J, Erritzoe D, Holst KK, Nielsen FA, Marner L, Lehel S, Arentzen T, Jernigan TL, Knudsen GM. Seasonal changes in brain serotonin transporter binding in short serotonin transporter linked polymorphic region-allele carriers but not in long-allele homozygotes. Biol Psychiatry. 2010;67:1033–1039. doi: 10.1016/j.biopsych.2009.11.027. [DOI] [PubMed] [Google Scholar]
- Kalbitzer J, Frokjaer VG, Erritzoe D, Svarer C, Cumming P, Nielsen FA, Hashemi SH, Baare WF, Madsen J, Hasselbalch SG, Kringelbach ML, Mortensen EL, Knudsen GM. The personality trait openness is related to cerebral 5-HTT levels. Neuroimage. 2009;45:280–285. doi: 10.1016/j.neuroimage.2008.12.001. [DOI] [PubMed] [Google Scholar]
- Kapoor RR, Gilbert C, Mohnike K, Blankenstein O, Fuechtner F, Hussain K. Congenital hyperinsulinism: [F]DOPA PET/CT scan of a focal lesion in the head of the pancreas. BMJ Case Rep. 2009;2009:bcr2007121178. doi: 10.1136/bcr.2007.121178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapur S, Remington G, Jones C, Wilson A, DaSilva J, Houle S, Zipursky R. High levels of dopamine D2 receptor occupancy with low-dose haloperidol treatment: a PET study. Am J Psychiatry. 1996;153:948–950. doi: 10.1176/ajp.153.7.948. [DOI] [PubMed] [Google Scholar]
- Karabanov A, Cervenka S, de Manzano O, Forssberg H, Farde L, Ullen F. Dopamine D2 receptor density in the limbic striatum is related to implicit but not explicit movement sequence learning. Proc Natl Acad Sci USA. 2010;107:7574–7579. doi: 10.1073/pnas.0911805107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson H, Hirvonen J, Kajander J, Markkula J, Rasi-Hakala H, Salminen JK, Nagren K, Aalto S, Hietala J. Research letter: Psychotherapy increases brain serotonin 5-HT1A receptors in patients with major depressive disorder. Psychological Medicine. 2010;40:523–528. doi: 10.1017/S0033291709991607. [DOI] [PubMed] [Google Scholar]
- Kegeles LS, Slifstein M, Xu X, Urban N, Thompson JL, Moadel T, Harkavy-Friedman JM, Gil R, Laruelle M, Abi-Dargham A. Striatal and extrastriatal dopamine D2/D3 receptors in schizophrenia evaluated with [18F]fallypride positron emission tomography. Biol Psychiatry. 2010;68:634–641. doi: 10.1016/j.biopsych.2010.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiesewetter DO, Jagoda EM, Starrett JE, Jr, Gribkoff VK, Hewawasam P, Srinivas N, Salazar D, Eckelman WC. Radiochemical synthesis and biodistribution of a novel maxi-K potassium channel opener. Nucl Med Biol. 2002;29:55–59. doi: 10.1016/s0969-8051(01)00281-5. [DOI] [PubMed] [Google Scholar]
- Kim YH, Kang HC, Kim DS, Kim SH, Shim KW, Kim HD, Lee JS. Neuroimaging in identifying focal cortical dysplasia and prognostic factors in pediatric and adolescent epilepsy surgery. Epilepsia. 2011;52:722–727. doi: 10.1111/j.1528-1167.2010.02950.x. [DOI] [PubMed] [Google Scholar]
- Kling MA, Carson RE, Borg L, Zametkin A, Matochik JA, Schluger J, Herscovitch P, Rice KC, Ho A, Eckelman WC, Kreek MJ. Opioid receptor imaging with positron emission tomography and [(18)F]cyclofoxy in long-term, methadone-treated former heroin addicts. J Pharmacol Exp Ther. 2000;295:1070–1076. [PubMed] [Google Scholar]
- Klunk WE, Engler H, Nordberg A, Wang Y, Blomqvist G, Holt DP, Bergstrom M, Savitcheva I, Huang GF, Estrada S, Ausen B, Debnath ML, Barletta J, Price JC, Sandell J, Lopresti BJ, Wall A, Koivisto P, Antoni G, Mathis CA, Langstrom B. Imaging brain amyloid in Alzheimer's disease with Pittsburgh Compound-B. Ann Neurol. 2004;55:306–319. doi: 10.1002/ana.20009. [DOI] [PubMed] [Google Scholar]
- Koepp MJ, Gunn RN, Lawrence AD, Cunningham VJ, Dagher A, Jones T, Brooks DJ, Bench CJ, Grasby PM. Evidence for striatal dopamine release during a video game. Nature. 1998a;393:266–268. doi: 10.1038/30498. [DOI] [PubMed] [Google Scholar]
- Koepp MJ, Richardson MP, Brooks DJ, Cunningham VJ, Duncan JS. Central benzodiazepine/gamma-aminobutyric acid A receptors in idiopathic generalized epilepsy: an [11C]flumazenil positron emission tomography study. Epilepsia. 1997;38:1089–1097. doi: 10.1111/j.1528-1157.1997.tb01198.x. [DOI] [PubMed] [Google Scholar]
- Koepp MJ, Richardson MP, Brooks DJ, Duncan JS. Focal cortical release of endogenous opioids during reading-induced seizures. Lancet. 1998b;352:952–955. doi: 10.1016/s0140-6736(97)09077-6. [DOI] [PubMed] [Google Scholar]
- Koeppe RA, Gilman S, Junck L, Wernette K, Frey KA. Differentiating Alzheimer's disease from dementia with Lewy bodies and Parkinson's disease with (+)-[11C]dihydrotetrabenazine positron emission tomography. Alzheimers Dement. 2008;4:S67–S76. doi: 10.1016/j.jalz.2007.11.016. [DOI] [PubMed] [Google Scholar]
- Koivunen J, Scheinin N, Virta JR, Aalto S, Vahlberg T, Nagren K, Helin S, Parkkola R, Viitanen M, Rinne JO. Amyloid PET imaging in patients with mild cognitive impairment: a 2-year follow-up study. Neurology. 2011;76:1085–1090. doi: 10.1212/WNL.0b013e318212015e. [DOI] [PubMed] [Google Scholar]
- Kordower JH, Freeman TB, Snow BJ, Vingerhoets FJ, Mufson EJ, Sanberg PR, Hauser RA, Smith DA, Nauert GM, Perl DP, Olanow CW. Neuropathological evidence of graft survival and striatal reinnervation after the transplantation of fetal mesencephalic tissue in a patient with Parkinson's disease. N Engl J Med. 1995;332:1118–1124. doi: 10.1056/NEJM199504273321702. [DOI] [PubMed] [Google Scholar]
- Kuhl DE, Hoffman EJ, Phelps ME, Ricci AR, Reivich M. Design and application of the Mark IV scanning system for radionuclide computed tomography of the brain. IAEA Symp Med Radionuclide Imaging. 1976;1:309–320. [Google Scholar]
- Kuhl DE, Koeppe RA, Minoshima S, Snyder SE, Ficaro EP, Foster NL, Frey KA, Kilbourn MR. In vivo mapping of cerebral acetylcholinesterase activity in aging and Alzheimer's disease. Neurology. 1999;52:691–699. doi: 10.1212/wnl.52.4.691. [DOI] [PubMed] [Google Scholar]
- Kumar A, Juhasz C, Asano E, Sood S, Muzik O, Chugani HT. Objective detection of epileptic foci by 18F-FDG PET in children undergoing epilepsy surgery. J Nucl Med. 2010;51:1901–1907. doi: 10.2967/jnumed.110.075390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamare F, Hinz R, Gaemperli O, Pugliese F, Mason JC, Spinks T, Camici PG, Rimoldi OE. Detection and quantification of large-vessel inflammation with 11C-(R)-PK11195 PET/CT. J Nucl Med. 2011;52:33–39. doi: 10.2967/jnumed.110.079038. [DOI] [PubMed] [Google Scholar]
- Lammertsma AA, Hume SP. Simplified reference tissue model for PET receptor studies. Neuroimage. 1996;4:153–158. doi: 10.1006/nimg.1996.0066. [DOI] [PubMed] [Google Scholar]
- Lammertsma AA, Jones T. Correction for the presence of intravascular oxygen-15 in the steady-state technique for measuring regional oxygen extraction ratio in the brain: 1. Description of the method. J Cereb Blood Flow Metab. 1983;3:416–424. doi: 10.1038/jcbfm.1983.67. [DOI] [PubMed] [Google Scholar]
- Lange K, Carson R. EM reconstruction algorithms for emission and transmission tomography. J Comp Assist Tomogr. 1984;8:306. [PubMed] [Google Scholar]
- Lanzenberger RR, Mitterhauser M, Spindelegger C, Wadsak W, Klein N, Mien LK, Holik A, Attarbaschi T, Mossaheb N, Sacher J, Geiss-Granadia T, Kletter K, Kasper S, Tauscher J. Reduced serotonin-1A receptor binding in social anxiety disorder. Biol Psychiatry. 2007;61:1081–1089. doi: 10.1016/j.biopsych.2006.05.022. [DOI] [PubMed] [Google Scholar]
- Laruelle M. Imaging synaptic neurotransmission with in vivo binding competition techniques: a critical review. J Cereb Blood Flow Metab. 2000;20:423–451. doi: 10.1097/00004647-200003000-00001. [DOI] [PubMed] [Google Scholar]
- Laruelle M, Abi-Dargham A, Gil R, Kegeles L, Innis R. Increased dopamine transmission in schizophrenia: relationship to illness phases. Biol Psychiatry. 1999;46:56–72. doi: 10.1016/s0006-3223(99)00067-0. [DOI] [PubMed] [Google Scholar]
- Laruelle M, Kegeles LS, Abi-Dargham A. Glutamate, dopamine, and schizophrenia: from pathophysiology to treatment. Ann NY Acad Sci. 2003;1003:138–158. doi: 10.1196/annals.1300.063. [DOI] [PubMed] [Google Scholar]
- Laufs H, Richardson MP, Salek-Haddadi A, Vollmar C, Duncan JS, Gale K, Lemieux L, Loscher W, Koepp MJ. Converging PET and fMRI evidence for a common area involved in human focal epilepsies. Neurology. 2011;77:904–910. doi: 10.1212/WNL.0b013e31822c90f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leblanc R, Tyler JL, Mohr G, Meyer E, Diksic M, Yamamoto L, Taylor L, Gauthier S, Hakim A. Hemodynamic and metabolic effects of cerebral revascularization. J Neurosurg. 1987a;66:529–535. doi: 10.3171/jns.1987.66.4.0529. [DOI] [PubMed] [Google Scholar]
- Leblanc R, Yamamoto YL, Tyler JL, Diksic M, Hakim A. Borderzone ischemia. Ann Neurol. 1987b;22:707–713. doi: 10.1002/ana.410220606. [DOI] [PubMed] [Google Scholar]
- Lenzi GL, Frackowiak RS, Jones T. Cerebral oxygen metabolism and blood flow in human cerebral ischemic infarction. J Cereb Blood Flow Metab. 1982;2:321–335. doi: 10.1038/jcbfm.1982.33. [DOI] [PubMed] [Google Scholar]
- Lenzi GL, Jones T, McKenzie CG, Moss S. Non-invasive regional study of chronic cerebrovascular disorders using the oxygen-15 inhalation technique. J Neurol Neurosurg Psychiatry. 1978;41:11–17. doi: 10.1136/jnnp.41.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenzi GL, Jones T, Reid JL, Moss S. Regional impairment of cerebral oxidative metabolism in Parkinson's disease. J Neurol Neurosurg Psychiatry. 1979;42:59–62. doi: 10.1136/jnnp.42.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyton M, Boileau I, Benkelfat C, Diksic M, Baker G, Dagher A. Amphetamine-induced increases in extracellular dopamine, drug wanting, and novelty seeking: a PET/[11C]raclopride study in healthy men. Neuropsychopharmacology. 2002;27:1027–1035. doi: 10.1016/S0893-133X(02)00366-4. [DOI] [PubMed] [Google Scholar]
- Lingford-Hughes A, Reid AG, Myers J, Feeney A, Hammers A, Taylor L, Rosso L, Turkheimer F, Brooks DJ, Grasby P, Nutt DJ. A [11c]Ro15 4513 PET study suggests that alcohol dependence in man is associated with reduced α5 benzodiazepine receptors in limbic regions. J Psychopharmacol. 2012;26:273–81. doi: 10.1177/0269881110379509. [DOI] [PubMed] [Google Scholar]
- Lueck CJ, Zeki S, Friston KJ, Deiber MP, Cope P, Cunningham VJ, Lammertsma AA, Kennard C, Frackowiak RS. The colour centre in the cerebral cortex of man. Nature. 1989;340:386–389. doi: 10.1038/340386a0. [DOI] [PubMed] [Google Scholar]
- Ma Y, Tang C, Chaly T, Greene P, Breeze R, Fahn S, Freed C, Dhawan V, Eidelberg D. Dopamine cell implantation in Parkinson's disease: long-term clinical and (18)F-FDOPA PET outcomes. J Nucl Med. 2010;51:7–15. doi: 10.2967/jnumed.109.066811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald SW, Cervenka S, Farde L, Nyberg L, Backman L. Extrastriatal dopamine D2 receptor binding modulates intraindividual variability in episodic recognition and executive functioning. Neuropsychologia. 2009;47:2299–2304. doi: 10.1016/j.neuropsychologia.2009.01.016. [DOI] [PubMed] [Google Scholar]
- Marazano C, Maziere M, Berger G, Comar D. Synthesis of methyl iodide-11 C and formaldehyde-11 C. Int J Appl Radiat Isot. 1977;28:49–52. doi: 10.1016/0020-708x(77)90159-4. [DOI] [PubMed] [Google Scholar]
- Marchal G, Rioux P, Petit-Tabou MC, Derlon JM, Baron JC, Serrati C, Viader F, de la Sayette V, Le Doze F, Lochon P, Petit-Taboué MC, Orgogozo JM. PET imaging of cerebral perfusion and oxygen consumption in acute ischaemic stroke: relation to outcome. Lancet. 1993;341:925–927. doi: 10.1016/0140-6736(93)91214-7. [DOI] [PubMed] [Google Scholar]
- Marner L, Gillings N, Comley RA, Baare WFC, Rabiner EA, Wilson AA, Houle S, Hasselbalch SG, Svarer C, Gunn RN, Laruelle M, Knudsen GM. Kinetic Modeling of 11C-SB207145 Binding to 5-HT4 Receptors in the Human Brain In Vivo. J Nucl Med. 2009;50:900–908. doi: 10.2967/jnumed.108.058552. [DOI] [PubMed] [Google Scholar]
- Martinez D, Gil R, Slifstein M, Hwang DR, Huang Y, Perez A, Kegeles L, Talbot P, Evans S, Krystal J, Laruelle M, Abi-Dargham A. Alcohol dependence is associated with blunted dopamine transmission in the ventral striatum. Biol Psychiatry. 2005;58:779–786. doi: 10.1016/j.biopsych.2005.04.044. [DOI] [PubMed] [Google Scholar]
- Martinez D, Greene K, Broft A, Kumar D, Liu F, Narendran R, Slifstein M, Van Heertum R, Kleber HD. Lower level of endogenous dopamine in patients with cocaine dependence: findings from PET imaging of D(2)/D(3) receptors following acute dopamine depletion. Am J Psychiatry. 2009;166:1170–1177. doi: 10.1176/appi.ajp.2009.08121801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez D, Narendran R. Imaging neurotransmitter release by drugs of abuse. Curr Top Behav Neurosci. 2010;3:219–245. doi: 10.1007/7854_2009_34. [DOI] [PubMed] [Google Scholar]
- Martinez D, Narendran R, Foltin RW, Slifstein M, Hwang DR, Broft A, Huang Y, Cooper TB, Fischman MW, Kleber HD, Laruelle M. Amphetamine-induced dopamine release: markedly blunted in cocaine dependence and predictive of the choice to self-administer cocaine. Am J Psychiatry. 2007;164:622–629. doi: 10.1176/ajp.2007.164.4.622. [DOI] [PubMed] [Google Scholar]
- McKenzie CG, Lenzi GL, Jones T, Moss S. Radioactive oxygen 15O studies in cerebral neoplasms. J R Soc Med. 1978;71:417–425. [PMC free article] [PubMed] [Google Scholar]
- Melcher CL, Schweitzer JS. A promising new scintillator: cerium-doped lutetium oxyorthosilicate. Nucl Instrum Methods Phys Res A. 1992;314:212–214. [Google Scholar]
- Melichar JK, Hume SP, Williams TM, Daglish MR, Taylor LG, Ahmad R, Malizia AL, Brooks DJ, Myles JS, Lingford-Hughes A, Nutt DJ. Using [11C]diprenorphine to image opioid receptor occupancy by methadone in opioid addiction: clinical and preclinical studies. J Pharmacol Exp Ther. 2005;312:309–315. doi: 10.1124/jpet.104.072686. [DOI] [PubMed] [Google Scholar]
- Mentis MJ, Dhawan V, Nakamura T, Ghilardi MF, Feigin A, Edwards C, Ghez C, Eidelberg D. Enhancement of brain activation during trial-and-error sequence learning in early PD. Neurology. 2003;60:612–619. doi: 10.1212/01.wnl.0000044154.92143.dc. [DOI] [PubMed] [Google Scholar]
- Meyer JH. Applying neuroimaging ligands to study major depressive disorder. Semin Nucl Med. 2008;38:287–304. doi: 10.1053/j.semnuclmed.2008.02.007. [DOI] [PubMed] [Google Scholar]
- Meyer JH, Ginovart N, Boovariwala A, Sagrati S, Hussey D, Garcia A, Young T, Praschak-Rieder N, Wilson AA, Houle S. Elevated monoamine oxidase a levels in the brain: an explanation for the monoamine imbalance of major depression. Arch Gen Psychiatry. 2006;63:1209–1216. doi: 10.1001/archpsyc.63.11.1209. [DOI] [PubMed] [Google Scholar]
- Meyer JH, Goulding VS, Wilson AA, Hussey D, Christensen BK, Houle S. Bupropion occupancy of the dopamine transporter is low during clinical treatment. Psychopharmacology. 2002;163:102–105. doi: 10.1007/s00213-002-1166-3. [DOI] [PubMed] [Google Scholar]
- Meyer JH, McMain S, Kennedy SH, Korman L, Brown GM, DaSilva JN, Wilson AA, Blak T, Eynan-Harvey R, Goulding VS, Houle S, Links P. Dysfunctional attitudes and 5-HT2 receptors during depression and self-harm. Am J Psychiatry. 2003;160:90–99. doi: 10.1176/appi.ajp.160.1.90. [DOI] [PubMed] [Google Scholar]
- Meyer JH, Wilson AA, Sagrati S, Hussey D, Carella A, Potter WZ, Ginovart N, Spencer EP, Cheok A, Houle S. Serotonin transporter occupancy of five selective serotonin reuptake inhibitors at different doses: an [11C]DASB positron emission tomography study. Am J Psychiatry. 2004;161:826–835. doi: 10.1176/appi.ajp.161.5.826. [DOI] [PubMed] [Google Scholar]
- Meyer JH, Wilson AA, Sagrati S, Miler L, Rusjan P, Bloomfield PM, Clark M, Sacher J, Voineskos AN, Houle S. Brain monoamine oxidase A binding in major depressive disorder: relationship to selective serotonin reuptake inhibitor treatment, recovery, and recurrence. Arch Gen Psychiatry. 2009;66:1304–1312. doi: 10.1001/archgenpsychiatry.2009.156. [DOI] [PubMed] [Google Scholar]
- Minoshima S, Frey KA, Cross DJ, Kuhl DE. Neurochemical imaging of dementias. Semin Nucl Med. 2004;34:70–82. doi: 10.1053/j.semnuclmed.2003.09.008. [DOI] [PubMed] [Google Scholar]
- Mintun MA, Raichle ME, Martin WR, Herscovitch P. Brain oxygen utilization measured with O-15 radiotracers and positron emission tomography. J Nucl Med. 1984;25:177–187. [PubMed] [Google Scholar]
- Miyake N, Skinbjerg M, Easwaramoorthy B, Kumar D, Girgis RR, Xu X, Slifstein M, Abi-Dargham A. Imaging changes in glutamate transmission in vivo with the metabotropic glutamate receptor 5 tracer [11C] ABP688 and N-acetylcysteine challenge. Biol Psychiatry. 2011;69:822–824. doi: 10.1016/j.biopsych.2010.12.023. [DOI] [PubMed] [Google Scholar]
- Moresco FM, Dieci M, Vita A, Messa C, Gobbo C, Galli L, Rizzo G, Panzacchi A, De Peri L, Invernizzi G, Fazio F. In vivo serotonin 5HT(2A) receptor binding and personality traits in healthy subjects: a positron emission tomography study. Neuroimage. 2002;17:1470–1478. doi: 10.1006/nimg.2002.1239. [DOI] [PubMed] [Google Scholar]
- Moustafa RR, Izquierdo-Garcia D, Jones PS, Graves MJ, Fryer TD, Gillard JH, Warburton EA, Baron JC. Watershed infarcts in transient ischemic attack/minor stroke with > or = 50% carotid stenosis: hemodynamic or embolic. Stroke. 2010;41:1410–1416. doi: 10.1161/STROKEAHA.110.580415. [DOI] [PubMed] [Google Scholar]
- Muller-Gartner HW, Links JM, Prince JL, Bryan RN, McVeigh E, Leal JP, Davatzikos C, Frost JJ. Measurement of radiotracer concentration in brain gray matter using positron emission tomography: MRI-based correction for partial volume effects. J Cereb Blood Flow Metab. 1992;12:571–583. doi: 10.1038/jcbfm.1992.81. [DOI] [PubMed] [Google Scholar]
- Muraishi K, Kameyama M, Sato K, Sirane R, Ogawa A, Yoshimoto T, Hatazawa J, Itoh M. Cerebral circulatory and metabolic changes following EC/IC bypass surgery in cerebral occlusive diseases. Neurol Res. 1993;15:97–103. doi: 10.1080/01616412.1993.11740117. [DOI] [PubMed] [Google Scholar]
- Nakamura T, Dhawan V, Chaly T, Fukuda M, Ma Y, Breeze R, Greene P, Fahn S, Freed C, Eidelberg D. Blinded positron emission tomography study of dopamine cell implantation for Parkinson's disease. Ann Neurol. 2001;50:181–187. doi: 10.1002/ana.1075. [DOI] [PubMed] [Google Scholar]
- Nash JR, Sargent PA, Rabiner EA, Hood SD, Argyropoulos SV, Potokar JP, Grasby PM, Nutt DJ. Serotonin 5-HT1A receptor binding in people with panic disorder: positron emission tomography study. Br J Psychiatry. 2008;193:229–234. doi: 10.1192/bjp.bp.107.041186. [DOI] [PubMed] [Google Scholar]
- Neumeister A, Bain E, Nugent AC, Carson RE, Bonne O, Luckenbaugh DA, Eckelman W, Herscovitch P, Charney DS, Drevets WC. Reduced serotonin type 1A receptor binding in panic disorder. J Neurosci. 2004;24:589–591. doi: 10.1523/JNEUROSCI.4921-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolaus S, Antke C, Beu M, Muller HW. Cortical GABA, striatal dopamine and midbrain serotonin as the key players in compulsive and anxiety disorders—results from in vivo imaging studies. Rev Neurosci. 2010;21:119–139. doi: 10.1515/revneuro.2010.21.2.119. [DOI] [PubMed] [Google Scholar]
- Nord M, Farde L. Antipsychotic occupancy of dopamine receptors in schizophrenia. CNS Neurosci Ther. 2011;17:97–103. doi: 10.1111/j.1755-5949.2010.00222.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nortje J, Coles JP, Timofeev I, Fryer TD, Aigbirhio FI, Smielewski P, Outtrim JG, Chatfield DA, Pickard JD, Hutchinson PJ, Gupta AK, Menon DK. Effect of hyperoxia on regional oxygenation and metabolism after severe traumatic brain injury: preliminary findings. Crit Care Med. 2008;36:273–281. doi: 10.1097/01.CCM.0000292014.60835.15. [DOI] [PubMed] [Google Scholar]
- Nutt R, Vento LJ, Ridinger MH. In vivo molecular imaging biomarkers: clinical pharmacology's new ‘PET'. Clin Pharmacol Ther. 2007;81:792–795. doi: 10.1038/sj.clpt.6100213. [DOI] [PubMed] [Google Scholar]
- Okello A, Koivunen J, Edison P, Archer HA, Turkheimer FE, Nagren K, Bullock R, Walker Z, Kennedy A, Fox NC, Rossor MN, Rinne JO, Brooks DJ. Conversion of amyloid positive and negative MCI to AD over 3 years: an 11C-PIB PET study. Neurology. 2009;73:754–760. doi: 10.1212/WNL.0b013e3181b23564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olanow CW, Goetz CG, Kordower JH, Stoessl AJ, Sossi V, Brin MF, Shannon KM, Nauert GM, Perl DP, Godbold J, Freeman TB. A double-blind controlled trial of bilateral fetal nigral transplantation in Parkinson's disease. Ann Neurol. 2003;54:403–414. doi: 10.1002/ana.10720. [DOI] [PubMed] [Google Scholar]
- Oswald LM, Wong DF, Zhou Y, Kumar A, Brasic J, Alexander M, Ye W, Kuwabara H, Hilton J, Wand GS. Impulsivity and chronic stress are associated with amphetamine-induced striatal dopamine release. Neuroimage. 2007;36:153–166. doi: 10.1016/j.neuroimage.2007.01.055. [DOI] [PubMed] [Google Scholar]
- Pantano P, Baron JC, Samson Y, Bousser MG, Derouesne C, Comar D. Crossed cerebellar diaschisis. Further studies. Brain. 1986;109 (Part 4:677–694. doi: 10.1093/brain/109.4.677. [DOI] [PubMed] [Google Scholar]
- Passchier J, Gentile G, Porter R, Herdon H, Salinas C, Jakobsen S, Audrain H, Laruelle M, Gunn RN. Identification and evaluation of [11C]GSK931145 as a novel ligand for imaging the type 1 glycine transporter with positron emission tomography. Synapse. 2010;64:542–549. doi: 10.1002/syn.20760. [DOI] [PubMed] [Google Scholar]
- Pauleit D, Floeth F, Hamacher K, Riemenschneider MJ, Reifenberger G, Muller HW, Zilles K, Coenen HH, Langen KJ. O-(2-[18F]fluoroethyl)-L-tyrosine PET combined with MRI improves the diagnostic assessment of cerebral gliomas. Brain. 2005;128:678–687. doi: 10.1093/brain/awh399. [DOI] [PubMed] [Google Scholar]
- Paulesu E, Frith CD, Frackowiak RS. The neural correlates of the verbal component of working memory. Nature. 1993;362:342–345. doi: 10.1038/362342a0. [DOI] [PubMed] [Google Scholar]
- Petersen SE, Fox PT, Posner MI, Mintun M, Raichle ME. Positron emission tomographic studies of the cortical anatomy of single-word processing. Nature. 1988;331:585–589. doi: 10.1038/331585a0. [DOI] [PubMed] [Google Scholar]
- Phelps ME, Hoffman EJ, Mullani NA, Ter-Pogossian MM. Application of annihilation coincidence detection to transaxial reconstruction tomography. J Nucl Med. 1975;16:210–224. [PubMed] [Google Scholar]
- Phelps ME, Huang SC, Hoffman EJ, Selin C, Sokoloff L, Kuhl DE. Tomographic measurement of local cerebral glucose metabolic rate in humans with (F-18)2-fluoro-2-deoxy-D-glucose: validation of method. Ann Neurol. 1979;6:371–388. doi: 10.1002/ana.410060502. [DOI] [PubMed] [Google Scholar]
- Piccini P, Brooks DJ, Bjorklund A, Gunn RN, Grasby PM, Rimoldi O, Brundin P, Hagell P, Rehncrona S, Widner H, Lindvall O. Dopamine release from nigral transplants visualized in vivo in a Parkinson's patient. Nat Neurosci. 1999;2:1137–1140. doi: 10.1038/16060. [DOI] [PubMed] [Google Scholar]
- Piccini P, Lindvall O, Bjorklund A, Brundin P, Hagell P, Ceravolo R, Oertel W, Quinn N, Samuel M, Rehncrona S, Widner H, Brooks DJ. Delayed recovery of movement-related cortical function in Parkinson's disease after striatal dopaminergic grafts. Ann Neurol. 2000;48:689–695. [PubMed] [Google Scholar]
- Pinching AJ, Travers RL, Hughes GR, Jones T, Moss S. Oxygen-15 brain scanning for detection of cerebral involvement in systemic lupus erythematosus. Lancet. 1978;1:898–900. doi: 10.1016/s0140-6736(78)90680-3. [DOI] [PubMed] [Google Scholar]
- Posner MI, Petersen SE, Fox PT, Raichle ME. Localization of cognitive operations in the human brain. Science. 1988;240:1627–1631. doi: 10.1126/science.3289116. [DOI] [PubMed] [Google Scholar]
- Powers WJ, Martin WR, Herscovitch P, Raichle ME, Grubb RL., Jr Extracranial-intracranial bypass surgery: hemodynamic and metabolic effects. Neurology. 1984;34:1168–1174. doi: 10.1212/wnl.34.9.1168. [DOI] [PubMed] [Google Scholar]
- Praschak-Rieder N, Willeit M, Wilson AA, Houle S, Meyer JH. Seasonal variation in human brain serotonin transporter binding. Arch Gen Psychiatry. 2008;65:1072–1078. doi: 10.1001/archpsyc.65.9.1072. [DOI] [PubMed] [Google Scholar]
- Price CJ, Wang D, Menon DK, Guadagno JV, Cleij M, Fryer T, Aigbirhio F, Baron JC, Warburton EA. Intrinsic activated microglia map to the peri-infarct zone in the subacute phase of ischemic stroke. Stroke. 2006;37:1749–1753. doi: 10.1161/01.STR.0000226980.95389.0b. [DOI] [PubMed] [Google Scholar]
- Rabiner EA, Beaver J, Makwana A, Searle G, Long C, Nathan PJ, Newbould RD, Howard J, Miller SR, Bush MA, Hill S, Reiley R, Passchier J, Gunn RN, Matthews PM, Bullmore ET.2011Pharmacological differentiation of opioid receptor antagonists by molecular and functional imaging of target occupancy and food reward-related brain activation in humans Mol Psychiatry 16826–835.785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabiner EA, Bhagwagar Z, Gunn RN, Sargent PA, Bench CJ, Cowen PJ, Grasby PM. Pindolol augmentation of selective serotonin reuptake inhibitors: PET evidence that the dose used in clinical trials is too low. Am J Psychiatry. 2001;158:2080–2082. doi: 10.1176/appi.ajp.158.12.2080. [DOI] [PubMed] [Google Scholar]
- Rabiner EA, Gunn RN, Castro ME, Sargent PA, Cowen PJ, Koepp MJ, Meyer JH, Bench CJ, Harrison PJ, Pazos A, Sharp T, Grasby PM. β-blocker binding to human 5-HT1A receptors in vivo and in vitro: Implications for antidepressant therapy. Neuropsychopharmacology. 2000;23:285–293. doi: 10.1016/S0893-133X(00)00109-3. [DOI] [PubMed] [Google Scholar]
- Rabiner EA, Messa C, Sargent PA, Husted-Kjaer K, Montgomery A, Lawrence AD, Bench CJ, Gunn RN, Cowen P, Grasby PM. A database of [(11)C]WAY-100635 binding to 5-HT(1A) receptors in normal male volunteers: normative data and relationship to methodological, demographic, physiological, and behavioral variables. Neuroimage. 2002;15:620–632. doi: 10.1006/nimg.2001.0984. [DOI] [PubMed] [Google Scholar]
- Ramsay SC, Weiller C, Myers R, Cremer JE, Luthra SK, Lammertsma AA, Frackowiak RS. Monitoring by PET of macrophage accumulation in brain after ischaemic stroke. Lancet. 1992;339:1054–1055. doi: 10.1016/0140-6736(92)90576-o. [DOI] [PubMed] [Google Scholar]
- Raynaud C, Todd-Pokropek AE, Comar D, Pizer SM, Kacperek A, Maziere M. A method for investigating regional variations of cerebral uptake of 11C psychotropic drugs in man. International Atomic Energy Agency; Dynamic studies with radioisotopes in medicine. 1974;vol. SM 185/84:45–56. [Google Scholar]
- Reader AJ, Sureau FC, Comtat C, Trebossen R, Buvat I. Joint estimation of dynamic PET images and temporal basis functions using fully 4D ML-EM. Phys Med Biol. 2006;51:5455–5474. doi: 10.1088/0031-9155/51/21/005. [DOI] [PubMed] [Google Scholar]
- Reimold M, Batra A, Knobel A, Smolka MN, Zimmer A, Mann K, Solbach C, Reischl G, Schwarzler F, Grunder G, Machulla HJ, Bares R, Heinz A.2008Anxiety is associated with reduced central serotonin transporter availability in unmedicated patients with unipolar major depression: a [11C]DASB PET study Mol Psychiatry 13606–613.557 [DOI] [PubMed] [Google Scholar]
- Rhodes CG, Wise RJ, Gibbs JM, Frackowiak RS, Hatazawa J, Palmer AJ, Thomas DG, Jones T. In vivo disturbance of the oxidative metabolism of glucose in human cerebral gliomas. Ann Neurol. 1983;14:614–626. doi: 10.1002/ana.410140604. [DOI] [PubMed] [Google Scholar]
- Richardson MP, Koepp MJ, Brooks DJ, Duncan JS. 11C-flumazenil PET in neocortical epilepsy. Neurology. 1998;51:485–492. doi: 10.1212/wnl.51.2.485. [DOI] [PubMed] [Google Scholar]
- Ridler K, Plisson C, Rabiner EA, Gunn RN, Easwaramoorthy B, Abi-Dargham A, Laruelle M, Slifstein M. Characterization of in vivo pharmacological properties and sensitivity to endogenous serotonin of [11C] P943: a positron emission tomography study in Papio anubis. Synapse. 2011;65:1119–1127. doi: 10.1002/syn.20946. [DOI] [PubMed] [Google Scholar]
- Rudd JH, Warburton EA, Fryer TD, Jones HA, Clark JC, Antoun N, Johnstrom P, Davenport AP, Kirkpatrick PJ, Arch BN, Pickard JD, Weissberg PL. Imaging atherosclerotic plaque inflammation with [18F]-fluorodeoxyglucose positron emission tomography. Circulation. 2002;105:2708–2711. doi: 10.1161/01.cir.0000020548.60110.76. [DOI] [PubMed] [Google Scholar]
- Ruhe HG, Booij J, Reitsma JB, Schene AH. Serotonin transporter binding with [123I]beta-CIT SPECT in major depressive disorder versus controls: effect of season and gender. Eur J Nucl Med Mol Imaging. 2009;36:841–849. doi: 10.1007/s00259-008-1057-x. [DOI] [PubMed] [Google Scholar]
- Ryvlin P, Bouvard S, Le Bars D, De Lamerie G, Gregoire MC, Kahane P, Froment JC, Mauguiere F. Clinical utility of flumazenil-PET versus [18F]fluorodeoxyglucose-PET and MRI in refractory partial epilepsy. A prospective study in 100 patients. Brain. 1998;121 (Part 11:2067–2081. doi: 10.1093/brain/121.11.2067. [DOI] [PubMed] [Google Scholar]
- Sacher J, Houle S, Parkes J, Rusjan P, Sagrati S, Wilson AA, Meyer JH. Monoamine oxidase A inhibitor occupancy during treatment of major depressive episodes with moclobemide or St. John's wort: an [(11)C]-harmine PET study. J Psychiatry Neurosci. 2011;36:375–382. doi: 10.1503/jpn.100117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacher J, Wilson AA, Houle S, Rusjan P, Hassan S, Bloomfield PM, Stewart DE, Meyer JH. Elevated brain monoamine oxidase A binding in the early postpartum period. Arch Gen Psychiatry. 2010;67:468–474. doi: 10.1001/archgenpsychiatry.2010.32. [DOI] [PubMed] [Google Scholar]
- Saleem A, Brown GD, Brady F, Aboagye EO, Osman S, Luthra SK, Ranicar AS, Brock CS, Stevens MF, Newlands E, Jones T, Price P. Metabolic activation of temozolomide measured in vivo using positron emission tomography. Cancer Res. 2003;63:2409–2415. [PubMed] [Google Scholar]
- Samson Y, Baron JC, Bousser MG, Rey A, Derlon JM, David P, Comoy J. Effects of extra-intracranial arterial bypass on cerebral blood flow and oxygen metabolism in humans. Stroke. 1985;16:609–616. doi: 10.1161/01.str.16.4.609. [DOI] [PubMed] [Google Scholar]
- Sanabria-Bohorquez SM, Joshi AD, Holahan M, Daneker L, Riffel K, Williams M, Li W, Cook JJ, Hamill TG. Quantification of the glycine transporter 1 in rhesus monkey brain using [(18)F]MK-6577 and a model-based input function. Neuroimage. 2012;59:2589–99. doi: 10.1016/j.neuroimage.2011.08.080. [DOI] [PubMed] [Google Scholar]
- Sargent PA, Kjaer KH, Bench CJ, Rabiner EA, Messa C, Meyer J, Gunn RN, Grasby PM, Cowen PJ. Brain serotonin1A receptor binding measured by positron emission tomography with [11C]WAY-100635: effects of depression and antidepressant treatment. Arch Gen Psychiatry. 2000;57:174–180. doi: 10.1001/archpsyc.57.2.174. [DOI] [PubMed] [Google Scholar]
- Savic I, Pauli S, Thorell JO, Blomqvist G. In vivo demonstration of altered benzodiazepine receptor density in patients with generalised epilepsy. J Neurol Neurosurg Psychiatry. 1994;57:797–804. doi: 10.1136/jnnp.57.7.797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savic I, Persson A, Roland P, Pauli S, Sedvall G, Widen L. In-vivo demonstration of reduced benzodiazepine receptor binding in human epileptic foci. Lancet. 1988;2:863–866. doi: 10.1016/s0140-6736(88)92468-3. [DOI] [PubMed] [Google Scholar]
- Savitz JB, Drevets WC. Imaging phenotypes of major depressive disorder: genetic correlates. Neuroscience. 2009;164:300–330. doi: 10.1016/j.neuroscience.2009.03.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnell O, Krebs B, Carlsen J, Miederer I, Goetz C, Goldbrunner RH, Wester HJ, Haubner R, Popperl G, Holtmannspotter M, Kretzschmar HA, Kessler H, Tonn JC, Schwaiger M, Beer AJ. Imaging of integrin alpha(v)beta(3) expression in patients with malignant glioma by [18F] Galacto-RGD positron emission tomography. Neuro Oncol. 2009;11:861–870. doi: 10.1215/15228517-2009-024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreckenberger M, Klega A, Grunder G, Buchholz HG, Scheurich A, Schirrmacher R, Schirrmacher E, Muller C, Henriksen G, Bartenstein P. Opioid receptor PET reveals the psychobiologic correlates of reward processing. J Nucl Med. 2008;49:1257–1261. doi: 10.2967/jnumed.108.050849. [DOI] [PubMed] [Google Scholar]
- Searle G, Beaver JD, Comley RA, Bani M, Tziortzi A, Slifstein M, Mugnaini M, Griffante C, Wilson AA, Merlo-Pich E, Houle S, Gunn R, Rabiner EA, Laruelle M. Imaging dopamine D3 receptors in the human brain with positron emission tomography, [11C]PHNO, and a selective D3 receptor antagonist. Biol Psychiatry. 2010;68:392–399. doi: 10.1016/j.biopsych.2010.04.038. [DOI] [PubMed] [Google Scholar]
- Serrati C, Marchal G, Rioux P, Viader F, Petit-Taboue MC, Lochon P, Luet D, Derlon JM, Baron JC. Contralateral cerebellar hypometabolism: a predictor for stroke outcome. J Neurol Neurosurg Psychiatry. 1994;57:174–179. doi: 10.1136/jnnp.57.2.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sette G, Baron JC, Mazoyer B, Levasseur M, Pappata S, Crouzel C. Local brain haemodynamics and oxygen metabolism in cerebrovascular disease. Positron emission tomography. Brain. 1989;112 (Part 4:931–951. doi: 10.1093/brain/112.4.931. [DOI] [PubMed] [Google Scholar]
- Silbersweig DA, Stern E, Frith C, Cahill C, Holmes A, Grootoonk S, Seaward J, McKenna P, Chua SE, Schnorr L, Jones T, Frackowiak RSJ. A functional neuroanatomy of hallucinations in schizophrenia. Nature. 1995;378:176–179. doi: 10.1038/378176a0. [DOI] [PubMed] [Google Scholar]
- Silbersweig DA, Stern E, Frith CD, Cahill C, Schnorr L, Grootoonk S, Spinks T, Clark J, Frackowiak R, Jones T. Detection of thirty-second cognitive activations in single subjects with positron emission tomography: a new low-dose H2(15)O regional cerebral blood flow three-dimensional imaging technique. J Cereb Blood Flow Metab. 1993;13:617–629. doi: 10.1038/jcbfm.1993.80. [DOI] [PubMed] [Google Scholar]
- Smith DF, Jakobsen S. Molecular tools for assessing human depression by positron emission tomography. Eur Neuropsychopharmacol. 2009;19:611–628. doi: 10.1016/j.euroneuro.2009.04.005. [DOI] [PubMed] [Google Scholar]
- Snow BJ, Tooyama I, McGeer EG, Yamada T, Calne DB, Takahashi H, Kimura H. Human positron emission tomographic [18F]fluorodopa studies correlate with dopamine cell counts and levels. Ann Neurol. 1993;34:324–330. doi: 10.1002/ana.410340304. [DOI] [PubMed] [Google Scholar]
- Sobesky J, Thiel A, Ghaemi M, Hilker RH, Rudolf J, Jacobs AH, Herholz K, Heiss WD. Crossed cerebellar diaschisis in acute human stroke: a PET study of serial changes and response to supratentorial reperfusion. J Cereb Blood Flow Metab. 2005a;25:1685–1691. doi: 10.1038/sj.jcbfm.9600162. [DOI] [PubMed] [Google Scholar]
- Sobesky J, Weber OZ, Lehnhardt F-G, Hesselmann V, Neveling M, Jacobs A, Heiss W-D. Does the mismatch match the penumbra. Stroke. 2005b;36:980–985. doi: 10.1161/01.STR.0000160751.79241.a3. [DOI] [PubMed] [Google Scholar]
- Sokoloff L, Reivich M, Kennedy C, Des Rosiers MH, Patlak CS, Pettigrew KD, Sakurada O, Shinohara M. The [14C]deoxyglucose method for the measurement of local cerebral glucose utilization: theory, procedure, and normal values in the conscious and anesthetized albino rat. J Neurochem. 1977;28:897–916. doi: 10.1111/j.1471-4159.1977.tb10649.x. [DOI] [PubMed] [Google Scholar]
- Soliman A, Bagby RM, Wilson AA, Miler L, Clark M, Rusjan P, Sacher J, Houle S, Meyer JH. Relationship of monoamine oxidase A binding to adaptive and maladaptive personality traits. Psychol Med. 2011;41:1051–1060. doi: 10.1017/S0033291710001601. [DOI] [PubMed] [Google Scholar]
- Soloff PH, Price JC, Mason NS, Becker C, Meltzer CC. Gender, personality, and serotonin-2A receptor binding in healthy subjects. Psychiatry Res. 2010;181:77–84. doi: 10.1016/j.pscychresns.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sossi V, de La Fuente-Fernandez R, Holden JE, Doudet DJ, McKenzie J, Stoessl AJ, Ruth TJ. Increase in dopamine turnover occurs early in Parkinson's disease: evidence from a new modeling approach to PET 18 F-fluorodopa data. J Cereb Blood Flow Metab. 2002;22:232–239. doi: 10.1097/00004647-200202000-00011. [DOI] [PubMed] [Google Scholar]
- Souza F, Simpson N, Raffo A, Saxena C, Maffei A, Hardy M, Kilbourn M, Goland R, Leibel R, Mann JJ, Van Heertum R, Harris PE. Longitudinal noninvasive PET-based beta cell mass estimates in a spontaneous diabetes rat model. J Clin Invest. 2006;116:1506–1513. doi: 10.1172/JCI27645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spence AM, Muzi M, Swanson KR, O'Sullivan F, Rockhill JK, Rajendran JG, Adamsen TC, Link JM, Swanson PE, Yagle KJ, Rostomily RC, Silbergeld DL, Krohn KA. Regional hypoxia in glioblastoma multiforme quantified with [18F]fluoromisonidazole positron emission tomography before radiotherapy: correlation with time to progression and survival. Clin Cancer Res. 2008;14:2623–2630. doi: 10.1158/1078-0432.CCR-07-4995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoessl AJ, Brooks DJ, Eidelberg D. Milestones in neuroimaging. Mov Disord. 2011;26:868–978. doi: 10.1002/mds.23679. [DOI] [PubMed] [Google Scholar]
- Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352:987–996. doi: 10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- Sureau FC, Reader AJ, Comtat C, Leroy C, Ribeiro MJ, Buvat I, Trebossen R. Impact of image-space resolution modeling for studies with the high-resolution research tomograph. J Nucl Med. 2008;49:1000–1008. doi: 10.2967/jnumed.107.045351. [DOI] [PubMed] [Google Scholar]
- Takasawa M, Jones PS, Guadagno JV, Christensen S, Fryer TD, Harding S, Gillard JH, Williams GB, Aigbirhio FI, Warburton EA, Ostergaard L, Baron JC. How reliable is perfusion MR in acute stroke? Validation and determination of the penumbra threshold against quantitative PET. Stroke. 2008;39:870–877. doi: 10.1161/STROKEAHA.107.500090. [DOI] [PubMed] [Google Scholar]
- Tang CC, Poston KL, Dhawan V, Eidelberg D. Abnormalities in metabolic network activity precede the onset of motor symptoms in Parkinson's disease. J Neurosci. 2010;30:1049–1056. doi: 10.1523/JNEUROSCI.4188-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tauscher J, Bagby RM, Javanmard M, Christensen BK, Kasper S, Kapur S. Inverse relationship between serotonin 5-HT(1A) receptor binding and anxiety: a [(11)C]WAY-100635 PET investigation in healthy volunteers. Am J Psychiatry. 2001;158:1326–1328. doi: 10.1176/appi.ajp.158.8.1326. [DOI] [PubMed] [Google Scholar]
- Tauscher J, Kapur S. Choosing the right dose of antipsychotics in schizophrenia: lessons from neuroimaging studies. CNS Drugs. 2001;15:671–678. doi: 10.2165/00023210-200115090-00001. [DOI] [PubMed] [Google Scholar]
- Ter-Pogossian MM, Eichling JO, Davis DO, Welch MJ. The measure in vivo of regional cerebral oxygen utilization by means of oxyhemoglobin labeled with radioactive oxygen-15. J Clin Invest. 1970;49:381–391. doi: 10.1172/JCI106247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ter-Pogossian MM, Herscovitch P. Radioactive oxygen-15 in the study of cerebral blood flow, blood volume, and oxygen metabolism. Semin Nucl Med. 1985;15:377–394. doi: 10.1016/s0001-2998(85)80015-5. [DOI] [PubMed] [Google Scholar]
- Ter-Pogossian MM, Phelps ME, Hoffman EJ, Mullani NA. A positron-emission transaxial tomograph for nuclear imaging (PETT) Radiology. 1975;114:89–98. doi: 10.1148/114.1.89. [DOI] [PubMed] [Google Scholar]
- Ter-Pogossian MM, Powers WE. Radioisotopes in Scientific Research, volume 3. Proceedings of the 1st UNESCO International Conference (Paris) Paris: Pergamon Press; 1957. The use of radioactive oxygen-15 in the determination of oxygen content in malignant neoplasms. [Google Scholar]
- Ter-Pogossian MM, Taveras JM, Davis DO, Eichling JO.1969A study of regional cerebral oxygen supply and utilization by means of radioactive oxygen-15 Recent advances in the study of circulation(Taveras JM, Fischgold H, Dilenge D, eds).Springfield, Illanois: Thomas; 156–174. [Google Scholar]
- The theory and practice of 3D PET(Bendrium B, Townsend DW, eds). Dordrecht: Kluwer Academic Publisher; 1998 [Google Scholar]
- Tomasi G, Bertoldo A, Bishu S, Unterman A, Smith CB, Schmidt KC. Voxel-based estimation of kinetic model parameters of the L-[1-(11)C]leucine PET method for determination of regional rates of cerebral protein synthesis: validation and comparison with region-of-interest-based methods. J Cereb Blood Flow Metab. 2009;29:1317–1331. doi: 10.1038/jcbfm.2009.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turkheimer FE, Banati RB, Visvikis D, Aston JA, Gunn RN, Cunningham VJ. Modeling dynamic PET-SPECT studies in the wavelet domain. J Cereb Blood Flow Metab. 2000;20:879–893. doi: 10.1097/00004647-200005000-00015. [DOI] [PubMed] [Google Scholar]
- Vaishnavi SN, Vlassenko AG, Rundle MM, Snyder AZ, Mintun MA, Raichle ME. Regional aerobic glycolysis in the human brain. Proc Natl Acad Sci USA. 2010;107:17757–17762. doi: 10.1073/pnas.1010459107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Assema DME, Lubberink M, Bauer M, van der Flier WM, Schuit RC, Windhorst AD, Comans EFI, Hoetjes NJ, Tolboom N, Langer O, Muller M, Scheltens P, Lammertsma AA, van Berckel BNM. Blood-brain barrier P-glycoprotein function in Alzheimer's disease. Brain. 2012;135:181–9. doi: 10.1093/brain/awr298. [DOI] [PubMed] [Google Scholar]
- van Berckel BN, Bossong MG, Boellaard R, Kloet R, Schuitemaker A, Caspers E, Luurtsema G, Windhorst AD, Cahn W, Lammertsma AA, Kahn RS. Microglia activation in recent-onset schizophrenia: a quantitative (R)-[11C]PK11195 positron emission tomography study. Biol Psychiatry. 2008;64:820–822. doi: 10.1016/j.biopsych.2008.04.025. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Wang GJ, Fowler JS, Logan J, Gatley SJ, Hitzemann R, Chen AD, Dewey SL, Pappas N. Decreased striatal dopaminergic responsiveness in detoxified cocaine-dependent subjects. Nature. 1997;386:830–833. doi: 10.1038/386830a0. [DOI] [PubMed] [Google Scholar]
- Wagner HN, Jr, Burns HD, Dannals RF, Wong DF, Langstrom B, Duelfer T, Frost JJ, Ravert HT, Links JM, Rosenbloom SB, Lukas SE, Kramer AV, Kuhar MJ. Imaging dopamine receptors in the human brain by positron tomography. Science. 1983;221:1264–1266. doi: 10.1126/science.6604315. [DOI] [PubMed] [Google Scholar]
- Weiller C, Isensee C, Rijntjes M, Huber W, Muller S, Bier D, Dutschka K, Woods RP, Noth J, Diener HC. Recovery from Wernicke's aphasia: a positron emission tomographic study. Ann Neurol. 1995;37:723–732. doi: 10.1002/ana.410370605. [DOI] [PubMed] [Google Scholar]
- Wenning GK, Odin P, Morrish P, Rehncrona S, Widner H, Brundin P, Rothwell JC, Brown R, Gustavii B, Hagell P, Jahanshahi M, Sawle G, Bjorklund A, Brooks DJ, Marsden CD, Quinn NP, Lindvall O. Short- and long-term survival and function of unilateral intrastriatal dopaminergic grafts in Parkinson's disease. Ann Neurol. 1997;42:95–107. doi: 10.1002/ana.410420115. [DOI] [PubMed] [Google Scholar]
- Wienhard K, Schmand M, Casey ME, Baker K, Bao J, Eriksson L, Jones WF, Knoess C, Lenox M, Lercher M, Luk P, Michel C, Reed JH, Richerzhagen N, Treffert J, Vollmar S, Young JW, Heiss WD, Nutt R. The ECAT HRRT: performance and first clinical application of the new high resolution research tomograph. IEEE Trans Nucl Sci. 2002;49:104–110. [Google Scholar]
- Willemsen AT, van Waarde A, Paans AM, Pruim J, Luurtsema G, Go KG, Vaalburg W. In vivo protein synthesis rate determination in primary or recurrent brain tumors using L-[1-11C]-tyrosine and PET. J Nucl Med. 1995;36:411–419. [PubMed] [Google Scholar]
- Williams TM, Daglish MR, Lingford-Hughes A, Taylor LG, Hammers A, Brooks DJ, Grasby P, Myles JS, Nutt DJ. Brain opioid receptor binding in early abstinence from opioid dependence: positron emission tomography study. Br J Psychiatry. 2007;191:63–69. doi: 10.1192/bjp.bp.106.031120. [DOI] [PubMed] [Google Scholar]
- Williams TM, Davies SJ, Taylor LG, Daglish MR, Hammers A, Brooks DJ, Nutt DJ, Lingford-Hughes A. Brain opioid receptor binding in early abstinence from alcohol dependence and relationship to craving: an [11C]diprenorphine PET study. Eur Neuropsychopharmacol. 2009;19:740–748. doi: 10.1016/j.euroneuro.2009.06.007. [DOI] [PubMed] [Google Scholar]
- Willmann O, Wennberg R, May T, Woermann FG, Pohlmann-Eden B. The contribution of 18F-FDG PET in preoperative epilepsy surgery evaluation for patients with temporal lobe epilepsy A meta-analysis. Seizure. 2007;16:509–520. doi: 10.1016/j.seizure.2007.04.001. [DOI] [PubMed] [Google Scholar]
- Wise RJ, Bernardi S, Frackowiak RS, Legg NJ, Jones T. Serial observations on the pathophysiology of acute stroke. The transition from ischaemia to infarction as reflected in regional oxygen extraction. Brain. 1983;106 (Pt 1:197–222. doi: 10.1093/brain/106.1.197. [DOI] [PubMed] [Google Scholar]
- Witte AV, Floel A, Stein P, Savli M, Mien LK, Wadsak W, Spindelegger C, Moser U, Fink M, Hahn A, Mitterhauser M, Kletter K, Kasper S, Lanzenberger R. Aggression is related to frontal serotonin-1A receptor distribution as revealed by PET in healthy subjects. Hum Brain Mapp. 2009;30:2558–2570. doi: 10.1002/hbm.20687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolk DA, Price JC, Saxton JA, Snitz BE, James JA, Lopez OL, Aizenstein HJ, Cohen AD, Weissfeld LA, Mathis CA, Klunk WE, De-Kosky ST. Amyloid imaging in mild cognitive impairment subtypes. Ann Neurol. 2009;65:557–568. doi: 10.1002/ana.21598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zald DH, Cowan RL, Riccardi P, Baldwin RM, Ansari MS, Li R, Shelby ES, Smith CE, McHugo M, Kessler RM. Midbrain dopamine receptor availability is inversely associated with novelty-seeking traits in humans. J Neurosci. 2008;28:14372–14378. doi: 10.1523/JNEUROSCI.2423-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamuner S, Gomeni R, Bye A. Estimate the time varying brain receptor occupancy in PET imaging experiments using non-linear fixed and mixed effect modeling approach. Nucl Med Biol. 2002;29:115–123. doi: 10.1016/s0969-8051(01)00275-x. [DOI] [PubMed] [Google Scholar]
- Zaro-Weber O, Moeller-Hartmann W, Heiss WD, Sobesky J. The performance of MRI-based cerebral blood flow measurements in acute and subacute stroke compared with 15O-water positron emission tomography: identification of penumbral flow. Stroke. 2009;40:2413–2421. doi: 10.1161/STROKEAHA.108.540914. [DOI] [PubMed] [Google Scholar]
- Zaro-Weber O, Moeller-Hartmann W, Heiss WD, Sobesky J. Maps of time to maximum and time to peak for mismatch definition in clinical stroke studies validated with positron emission tomography. Stroke. 2010;41:2817–2821. doi: 10.1161/STROKEAHA.110.594432. [DOI] [PubMed] [Google Scholar]
- Zubieta JK, Gorelick DA, Stauffer R, Ravert HT, Dannals RF, Frost JJ. Increased mu opioid receptor binding detected by PET in cocaine-dependent men is associated with cocaine craving. Nat Med. 1996;2:1225–1229. doi: 10.1038/nm1196-1225. [DOI] [PubMed] [Google Scholar]
- Zubieta JK, Smith YR, Bueller JA, Xu Y, Kilbourn MR, Jewett DM, Meyer CR, Koeppe RA, Stohler CS. Regional mu opioid receptor regulation of sensory and affective dimensions of pain. Science. 2001;293:311–315. doi: 10.1126/science.1060952. [DOI] [PubMed] [Google Scholar]