Abstract
Necrobiotic Xanthogranuloma (NXG) was first described in 1980 by Kossad and Winkelmann in which they discussed 8 patients with xanthomatous plaques, noted to have monoclonal gammopathy, predominantly IgG kappa type1. Since then, more than 50 patients with this disorder have been described, with approximately 80% of them associated with a monoclonal gammopathy.
We describe the first case of NXG with associated monoclonal gammopathy, treated with thalidomide plus dexamethasone, achieving complete resolution of the skin lesions and sustaining response more than three years after treatment.
Case
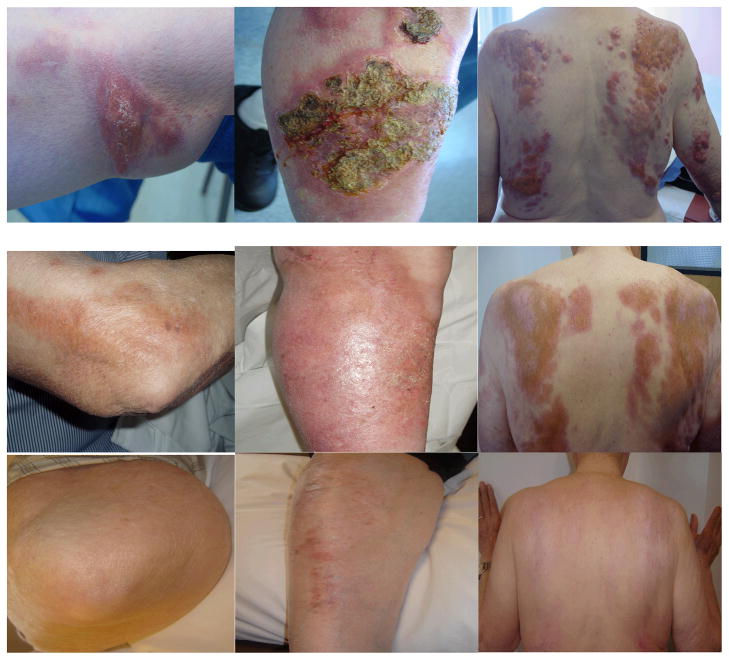
The patient is a 79 y/o male who presented in 2003 with multiple painful lesions of the skin (Figure 1). The lesions were raised and ulcerated. He had no facial or peri-orbital lesions. Biopsy of a lesion confirmed the diagnosis of NXG involving the deep dermis and subcutaneous fatty tissue. Granulomatous changes were seen in an ulcerative background. Plasma cells, which were faintly positive for kappa light chain, were found in small amounts through out. Work up included an IgG kappa monoclonal spike on serum protein electrophoresis, serum IgG of 1980mg/dl (normal: 751–1560), and Kappa of 2040mg/dl (normal: 629–1350). Hematocrit, urine protein electrophoresis, myeloma survey, liver and kidney function were normal. Bone marrow biopsy showed 10% plasma cells. He was diagnosed with NXG with smoldering myeloma. He was started on thalidomide and dexamethasone (TD, T 100mg daily, then 200mg after one month; D 20mg/day for 4 days/2 weeks, then 20mg/day for 4 days/month 6 months later). D was stopped 3 months later due to intolerance. Eight months after starting treatment, his lesions completely dried up (Figure 1). Thalidomide was stopped 2 years after starting it due to symptomatic bradycardia, otherwise, he tolerated it very well with no evidence of neuropathy. He has not required treatment since then and his lesions have remained closed almost 4 years later (Figure 1). Lowest IgG and kappa levels were 750mg/dl and 339mg/dl respectively, correlating with clinical response of the skin lesions.
Fig 1.
Initial presentation (top panel); 8 months into treatment (middle); 3yrs after end of treatment (bottom)
Discussion and Review of The Literature
Mehregan and Winkelmann reported in 1992 on 48 known cases 2 and Ugurlu et al further reported in 2000 on 28 additional cases 3. The clinical picture of NXG is a slowly progressive, destructive and infiltrating xanthomatous plagues and cutaneous lesions associated with paraproteinemia. The plaques and lesions may involve the trunk and extremities, but more than 80% of patients present with periorbital involvement. The lesions may ulcerate and most often there are areas of indurations consisting of yellow or xanthomatous discoloration. Histologically, NXG is characterized by granuloma formation within the subcutaneous and dermal layers, with focal areas of necrobiosis. The granulomas consist of multinucleated giant cells of several types. Cholesterol clefts within the areas of necrobiosis give the foamy appearance that is often seen Physical findings outside of the skin lesions are often unrevealing, but in the case series by Mehregan, more than 20% had hepatomegaly, and almost 20% had splenomegaly2. Most patients do not have pain or paresthesias, unlike our patient who did. Up to 80% of patients have monoclonal gammopathy of IgG type with either Kappa or Lambda light chain. Hematologic involvement may include neutropenia, cryoglobulinemia, hypocomplementemia, and hyperlipidemia. Systemic involvements have included multiple myeloma, Hodgkin lymphoma, non-Hodgkin lymphoma, chronic lymphocytic leukemia, lung and heart involvement 4–7. However, the most common association is monoclonal gammopathy of uncertain significance (MGUS).
The pathogenesis of NXG remains unclear. Proposed mechanism include foreign body giant cell reaction precipitated by deposition in the skin of increased serum immunoglobulins complexed with lipid8; secondary proliferation of macrophages caused by elevation of paraprotein9 and granuloma formation by paraprotein acting as lipoproteins, binding to histiocytes receptors10. NXG remains a rare condition, thus precluding it from being studied on a large scale. Management of NXG has included surgery, radiation, plasmapheresis, Intralesional corticosteroids, and systemic and cytotoxic agents such as chlorambucil, melphalan, interferon alpha-2b, cyclophosphamide, methotrexate, hydroxychloroquine, azathioprine, nitrogen mustard, and high dose steroids3,9,11–30. Two cases have reported use of thalidomide30,31. In the first, only half of the skin ulcers healed without modification of the xanthomatous skin lesions on thalidomide 200md/day30. Etretinate 50mg/day was added but patient relapsed 6 months later with leg ulcers. The second was a patient with scleritis, who was treated for an unknown duration and dose of thalidomide and dexamethasone. Our patient was treated with thalidomide 200mg/day for 2 years and dexamethasone for 9 months. Hence a longer duration and higher dose of thalidomide is likely needed to achieve prolonged response. A recent case report showed a complete response in a patient with NXG associated with MGUS treated with lenalidomide and dexamethosone32. Lenalidomide is a more potent analog of thalidomide. Our case is the first in using a combination of thalidomide and pulse dexamethasone, and achieving and sustaining complete response and resolution of lesions more than 3 years after cessation of treatment. Table 1 list cases reported from 1993 to current except cases from the mayo clinic, which have been reported by Ugurlu in 20003. Prior cases have been reported by Mehregan2.
Table 1.
Reported cases of necrobiotic xanthogranuloma.
| Author/yr | Age, y/sex | Location | Paraprotein | BM | Other organ involvement | Treatments received / outcome |
|---|---|---|---|---|---|---|
| Venencie12 1995 | 65/F | Periorbital, presternal, shoulders | IgG kappa | <10% plasma cells | none | Initial Melphalan+ prednisone, then Interferon alfa-2b+prednisone. Still on prednisone 1.5 yrs later. Lesions flattened with residual pigmentation |
| Barzilai 13 1996 | 85/F | Face, trunk extremities | IgG kappa | Not done | Possibly cardiac | None. Patient refused |
| Johnston14 1997 | 69/F | Thighs, arms, back | IgG kappa | Normal | None | Intralesional corticosteroid injection of symptomatic lesions. Outcome not noted |
| Georgiou15 1999 | 82/M | Chest, back | Not indicated | Not done | None | Interferon alpha -2a. Resolution after 4 months therapy. No recurrence 22 months after therapy |
| Nestle16 1999 | 77/F | Neck, trunk, arms, legs | IgG lambda | Normal | None | Initial PUVA and radiotherapy. Then melphalan x 6 cycles with resolution. No long-term follow up noted. |
| Randell17 1999 | 51/F | Periorbital | IgG lambda | Normal | None | Treatment not discussed. |
| Chave18 2001 | 66/F | Periorbital, neck, chest, abdomen | IgG kappa | Normal | None | Chlorambucil, cytoxan, melphalan, etoposide plasmapheresis and IFN-alph2b all ineffective. high-dose dexamethasone x 2 cycles with continued prednisolone with encouraging response |
| Chave 19 2001 | 75/M | Periorbital, Upper back, shoulders, arms, thigh | IgG kappa IgG lambda |
2% plasma cells | None | No systemic treatment at 1 year since presentation |
| Machado20 2001 | 51/M | Neck, trunk | IgG lambda | 5–10% plasma cells | Cryoglobulinemia, spleenomegaly | Chlorambucil x 7 mos with eventual disappearance of all lesions. No recurrence at 9 mos follow up |
| Vasconcellos21 2002 | 40/F | Periorbital, legs, thighs, back | IgG lambda | Normal | None | Melphalan +prednisone. Stopped treatment after 2 mos- reason not given |
| Burdick22 2003 | 57/F | Periorbital, upper body | IgG lambda | Xanthogranuloma within medullar No malignancy | Hepatomegaly | No treatment initiated |
| Fernandez23 2004 | 73/M | Periorbital | IgG kappa | 14% plasma cells | Multiple myeloma | Surgical removal of eyelid skin. Melphalan ongoing at 9 mos |
| Meyer24 2005 | 53/F | Periorbital | IgG kappa | 5% plasma cells | None | Numerous nonresponsive therapies. Stable therapeutic response after 9 cycles of intravenous cytoxan+dexamethasone (mesna given for bladder protection. Treatment was ongoing. |
| Viera25 2005 | 68/F | Periorbital, buttocks | IgG lambda | Not done | Prior history of lymphoplasmacytic lymphoma | Carbon dioxide laser for 3 sessions with residual lesions of NXG present. No relapse at 12 months follow-up. |
| Langlois26 2006 | 75/F | Periorbital, neck, arms, torso, neck, umbilical | IgG lambda | Not reported | Multiple myeloma | Melphalan+prednisone. Skin lesions faded after 2 courses. Length of treatment not noted |
| Oumeish27 2006 | 56/F | Periorbital, face, chest, back, | IgG kappa | NHL, CLL | NHL, CLL | Cytoxan, endoxan, leukeran, melphalan and prednisolone. Excellent response of the NHL and CLL. Unsatisfactory response of skin lesions despite cyclosporine and systemic steroids |
| Torabian28 2006 | 55/M | Periorbital, extremities, trunk | IgG lambda | 2% plasma cells | None | Chlorambucil. Flattening and disappearance of skin lesions but persistent Paraprotein spike at 6 mos of treatment |
| Ito29 2007 | 86/F | Limbs | IgG lambda | Patient refused | None | Patient died of myocardial infarction shortly after diagnosis |
| Silapunt 2010 | 81/M | Extremeties, trunk, face | IgG Kappa | 10% plasma cells | None | Lenalidomide and dexamethosone x 3 months with resolution of skin lesions.. no recurrence at 12 months follow-up |
CLL means chronic lymphocytic leukemia, NHL non hodgkins lymphoma
Conclusion
We describe the first case of necrobiotic xanthogranuloma and associated IgG kappa monoclonal gammopathy that responded very well to a combination of pulse dexamethasone and thalidomide and sustaining remission more than 3 years after cessation of treatment. The remission of the patient’s skin lesions has correlated with a decrease and stabilization of his IgG kappa levels, suggesting a correlation with his plasma cell dyscrasia and the activity of his skin disease. NXG has been treated with a wide range of therapies, including systemic cytotoxic drugs that have a wide range of toxic effects. Thalidomide in combination with pulse dexamethasone, which in our case was both successful and well tolerated, should be considered for first line treatment in NXG cases that need systemic therapy.
References
- 1.Kossard S, Winkelmann RK. Necrobiotic xanthogranuloma with paraproteinemia. J Am Acad Dermatol. 1980;3:257–270. doi: 10.1016/s0190-9622(80)80189-7. [DOI] [PubMed] [Google Scholar]
- 2.Mehregan DA, Winkelmann RK. Necrobiotic xanthogranuloma. Arch Dermatol. 1992;128:94–100. [PubMed] [Google Scholar]
- 3.Ugurlu S, Bartley GB, Gibson LE. Necrobiotic xanthogranuloma: long-term outcome of ocular and systemic involvement. Am J Ophthalmol. 2000;129:651–657. doi: 10.1016/s0002-9394(99)00469-9. [DOI] [PubMed] [Google Scholar]
- 4.Winkelmann RK, Litzow MR, Umbert IJ, Lie JT. Giant cell granulomatous pulmonary and myocardial lesions in necrobiotic xanthogranuloma with paraproteinemia. Mayo Clin Proc. 1997;72:1028–1033. doi: 10.4065/72.11.1028. [DOI] [PubMed] [Google Scholar]
- 5.Umbert I, Winkelmann RK. Necrobiotic xanthogranuloma with cardiac involvement. Br J Dermatol. 1995;133:438–443. doi: 10.1111/j.1365-2133.1995.tb02674.x. [DOI] [PubMed] [Google Scholar]
- 6.Hunter L, Burry AF. Necrobiotic xanthogranuloma: a systemic disease with paraproteinemia. Pathology. 1985;17:533–536. doi: 10.3109/00313028509105517. [DOI] [PubMed] [Google Scholar]
- 7.Novak PM, Robbins TO, Winkelmann RK. Necrobiotic xanthogranuloma with myocardial lesions and nodular transformation of the liver. Hum Pathol. 1992;23:195–196. doi: 10.1016/0046-8177(92)90244-w. [DOI] [PubMed] [Google Scholar]
- 8.Bullock JD, Bartley GB, Campbell RJ, Yanes B, Connelly PJ, Funkhouser JW. Necrobiotic xanthogranuloma with paraproteinemia. Case report and a pathogenetic theory. Ophthalmology. 1986;93:1233–1236. doi: 10.1016/s0161-6420(86)33605-4. [DOI] [PubMed] [Google Scholar]
- 9.Char DH, LeBoit PE, Ljung BM, Wara W. Radiation therapy for ocular necrobiotic xanthogranuloma. Arch Ophthalmol. 1987;105:174–175. doi: 10.1001/archopht.1987.01060020028014. [DOI] [PubMed] [Google Scholar]
- 10.Rappersberger K, Wrba F, Heinz R, Zonzits E, Honigsmann H. Necrobiotic xanthogranuloma in paraproteinemia. Hautarzt. 1989;40:358–363. [PubMed] [Google Scholar]
- 11.Finelli LG, Ratz JL. Plasmapheresis, a treatment modality for necrobiotic xanthogranuloma. J Am Acad Dermatol. 1987;17:351–354. doi: 10.1016/s0190-9622(87)70211-4. [DOI] [PubMed] [Google Scholar]
- 12.Venencie PY, Le Bras P, Toan ND, Tchernia G, Delfraissy JF. Recombinant interferon alfa-2b treatment of necrobiotic xanthogranuloma with paraproteinemia. J Am Acad Dermatol. 1995;32:666–667. doi: 10.1016/0190-9622(95)90370-4. [DOI] [PubMed] [Google Scholar]
- 13.Barzilai A, Trau H, Shpiro D, Yorav S. Necrobiotic xanthogranuloma with paraproteinemia. Cutis. 1996;57:320–322. [PubMed] [Google Scholar]
- 14.Johnston KA, Grimwood RE, Meffert JJ, Deering KC. Necrobiotic xanthogranuloma with paraproteinemia: an evolving presentation. Cutis. 1997;59:333–336. [PubMed] [Google Scholar]
- 15.Georgiou S, Monastirli A, Kapranos N, Pasmatzi E, Sakkis T, Tsambaos D. Interferon alpha-2a monotherapy for necrobiotic xanthogranuloma. Acta Derm Venereol. 1999;79:484–485. doi: 10.1080/000155599750010030. [DOI] [PubMed] [Google Scholar]
- 16.Nestle FO, Hofbauer G, Burg G. Necrobiotic xanthogranuloma with monoclonal gammopathy of the IgG lambda type. Dermatology. 1999;198:434–435. [PubMed] [Google Scholar]
- 17.Randell PL, Heenan PJ. Necrobiotic xanthogranuloma with paraproteinaemia. Australas J Dermatol. 1999;40:114–115. doi: 10.1046/j.1440-0960.1999.00334.x. [DOI] [PubMed] [Google Scholar]
- 18.Chave TA, Chowdhury MM, Holt PJ. Recalcitrant necrobiotic xanthogranuloma responding to pulsed high-dose oral dexamethasone plus maintenance therapy with oral prednisolone. Br J Dermatol. 2001;144:158–161. doi: 10.1046/j.1365-2133.2001.03967.x. [DOI] [PubMed] [Google Scholar]
- 19.Chave TA, Hutchinson PE. Necrobiotic xanthogranuloma with two monoclonal paraproteins and no periorbital involvement at presentation. Clin Exp Dermatol. 2001;26:493–496. doi: 10.1046/j.1365-2230.2001.00873.x. [DOI] [PubMed] [Google Scholar]
- 20.Machado S, Alves R, Lima M, Leal I, Massa A. Cutaneous necrobiotic xanthogranuloma (NXG)--successfully treated with low dose chlorambucil. Eur J Dermatol. 2001;11:458–462. [PubMed] [Google Scholar]
- 21.Criado PR, Vasconcellos C, Pegas JR, et al. Necrobiotic xanthogranuloma with lambda paraproteinemia: case report of successful treatment with melphalan and prednisone. J Dermatolog Treat. 2002;13:87–89. doi: 10.1080/095466302317584458. [DOI] [PubMed] [Google Scholar]
- 22.Burdick AE, Sanchez J, Elgart GW. Necrobiotic xanthogranuloma associated with a benign monoclonal gammopathy. Cutis. 2003;72:47–50. [PubMed] [Google Scholar]
- 23.Martinez Fernandez M, Rodriguez Prieto MA, Ruiz Gonzalez I, Sanchez Sambucety P, Delgado Vicente S. Necrobiotic xanthogranuloma associated with myeloma. J Eur Acad Dermatol Venereol. 2004;18:328–331. doi: 10.1111/j.1468-3083.2004.00906.x. [DOI] [PubMed] [Google Scholar]
- 24.Meyer S, Szeimies RM, Landthaler M, Hohenleutner S. Cyclophosphamide-dexamethasone pulsed therapy for treatment of recalcitrant necrobiotic xanthogranuloma with paraproteinemia and ocular involvement. Br J Dermatol. 2005;153:443–445. doi: 10.1111/j.1365-2133.2005.06737.x. [DOI] [PubMed] [Google Scholar]
- 25.Vieira V, Del Pozo J, Martinez W, Veiga-Barreiro JA, Fonseca E. Necrobiotic xanthogranuloma associated with lymphoplasmacytic lymphoma. Palliative treatment with carbon dioxide laser. Eur J Dermatol. 2005;15:182–185. [PubMed] [Google Scholar]
- 26.Langlois S, Brochot P, Reguiai Z, et al. Necrobiotic xanthogranuloma with multiple myeloma. Case report and pathogenic hypotheses. Joint Bone Spine. 2006;73:120–122. doi: 10.1016/j.jbspin.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 27.Oumeish OY, Oumeish I, Tarawneh M, Salman T, Sharaiha A. Necrobiotic xanthogranuloma associated with paraproteinemia and non-Hodgkin’s lymphoma developing into chronic lymphocytic leukemia: the first case reported in the literature and review of the literature. Int J Dermatol. 2006;45:306–310. doi: 10.1111/j.1365-4632.2006.02575.x. [DOI] [PubMed] [Google Scholar]
- 28.Torabian SZ, Fazel N, Knuttle R. Necrobiotic xanthogranuloma treated with chlorambucil. Dermatol Online J. 2006;12:11. [PubMed] [Google Scholar]
- 29.Ito Y, Nishimura K, Yamanaka K, et al. Necrobiotic xanthogranuloma with paraproteinemia; an atypical case. J Dtsch Dermatol Ges. 2008;6:40–43. doi: 10.1111/j.1610-0387.2007.06392.x. [DOI] [PubMed] [Google Scholar]
- 30.Hauser C, Schifferli J, Saurat JH. Complement consumption in a patient with necrobiotic xanthogranuloma and paraproteinemia. J Am Acad Dermatol. 1991;24:908–911. doi: 10.1016/0190-9622(91)70145-r. [DOI] [PubMed] [Google Scholar]
- 31.Wilhelmus KR, Yen MT, Rice L, Font RL. Necrobiotic xanthogranuloma with posterior scleritis. Arch Ophthalmol. 2006;124:748. doi: 10.1001/archopht.124.5.748. [DOI] [PubMed] [Google Scholar]
- 32.Silapunt S, Chon SY. Generalized necrobiotic xanthogranuloma successfully treated with lenalidomide. J Drugs Dermatol. 9:273–276. [PubMed] [Google Scholar]