Abstract
Ocular hypertension is the greatest known risk factor for glaucoma that affects an estimated 70 million people worldwide. Lowering intraocular pressure (IOP) remains the mainstay of therapy in the management of glaucoma. By means of microarray analysis, we have discovered that 1α,25-dihydroxyvitamin D3 (1,25-(OH)2D3) regulates genes that are known to be involved in the determination of intraocular pressure (IOP). Topical administration of 1,25-(OH)2D3 or its analog, 2-methylene-19-nor-(20S)-1α,25-dihydroxyvitamin D3 (2MD), markedly reduce IOP in non-human primates. The reduction in IOP is not the result of reduced aqueous humor formation, while a 35% increase in aqueous humor removal by 1,25(OH)2D3 was found but this increase did not achieve significance. Nevertheless, our results suggest that 1,25-(OH)2D3 or an analog thereof may present a new approach to the treatment of glaucoma.
Keywords: 1,25-dihydroxyvitamin D3; glaucoma; intraocular pressure; vitamin D receptor
Introduction
1α,25-Dihydroxyvitamin D3 (1,25(OH)2D3) is well established as the primary regulator of calcium and phosphorous homeostasis. Further research has suggested that vitamin D and analogs may be useful in the treatment of a number of diseases independent of calcium, phosphorus and bone [1–3]. The currently accepted mechanism is that vitamin D implements its functions through a single vitamin D receptor (VDR), that upon heterodimerization with the retinoid X receptor acts as a ligand-activated transcription factor [4]. VDR belongs to a superfamily of nuclear receptors with the highest similarity to the subfamily that includes retinoic acid receptor, thyroid hormone receptor and peroxisome proliferator activator receptor [4]. VDR binds to specific DNA sequences or vitamin D-responsive elements (VDREs) usually found in proximity to the start codon of the target genes thus transactivating or transrepressing their expression [4,5].
The glaucomas are a heterogeneous group of optic neuropathies that affect an estimated 70 million people. Asymptomatic in its earlier stages, the disease is one of the leading causes of irreversible blindness in the world. It is characterized by degeneration of the optic nerve and progressive visual field loss as the retinal ganglion cells die. The etiology of glaucoma is poorly understood. There is little understanding of the genetics and even less of the cell biology underlying glaucoma development and progression [6].
Ocular hypertension is the strongest known risk factor for open angle glaucoma (POAG), the most common form. Intraocular pressure (IOP) is determined by aqueous humor (AH) production by the ciliary body and by AH drainage through the trabecular and uveoscleral drainage pathways [6]. Elevated IOP occurs as a result of increased resistance to drainage of AH primarily through the trabecular (conventional) outflow system [7]. The molecular pathophysiology of IOP remains obscure [8].
The main goal of treatment for all forms of glaucoma is the preservation of visual function. Lowering IOP remains the mainstay of therapy in the management of glaucoma, since it has been shown to be effective in reducing optic nerve damage and loss of vision [6]. Thus, pharmaceuticals that are effective in lowering IOP represent an important approach to the treatment of glaucoma.
We discovered that 1,25-(OH)2D3 and other vitamin D analogs may represent such a pharmaceutical. Microarray experiments in vivo and in vitro revealed that 1,25-(OH)2D3 affects genes known to be involved in the regulation of IOP. As a result, we examined the effect of 1,25-(OH)2D3 and analogs on IOP in monkeys. Our results show that 1,25-(OH)2D3 applied topically to eyes causes a rapid drop in IOP.
Materials and methods
Vitamin D analogs
1,25-(OH)2D3 was purchased from Sigma Aldrich Fine Chemicals (Madison, WI). 2-methylene-19-nor-(20S)-1α,25-dihydroxyvitamin D3 (2MD) was synthesized in our laboratory [9]. 1,25-(OH)2D3 was quantitated by measurement of UV absorption at 265 nm using an extinction coefficient of 18,200 M−1cm−1 [10], while 2MD was quantitated by measurement of UV absorption at 252 nm with an extinction coefficient of 42,000 M−1cm−1 [9].
Animals
All animal experiments (mice, rats and monkeys) were conducted in accordance with the University of Wisconsin IACUC and National Institutes of Health guidelines, and the ARVO statement for the Use of Animals in Ophthalmic and Vision Research.
Rats
Male Sprague-Dawley weanling rats were obtained from Harlan Laboratories (Indianapolis, IN) and maintained on a highly purified vitamin D-deficient diet, containing 0.47% calcium and 0.3% phosphorus (Pi) supplemented 3 times a week with 500 μg DL-α-tocopherol, 60 μg menadione, and 40 μg β carotene in 0.1 ml soybean oil (AEK) [11]. Rats were housed in hanging wire cages and maintained on a 12 h light/dark cycle. Rats fed the vitamin D-deficient diet were maintained in a room with incandescent lighting, and all potential sources of ultraviolet light and vitamin D were excluded. At 14 wk of age, blood was taken from the tail for measurement of serum calcium concentration. Severe hypocalcemia was used to confirm vitamin D depletion.
Monkeys
Ocular normotensive adult cynomolgus monkeys (Macaca fascicularis), 4–18 years old, of either sex, weighing 3–14 kg were studied. Monkeys were anesthetized with intramuscular (i.m.) ketamine HCl (initial dose 3–25 mg/kg, supplemental dose 1–10 mg/kg) for IOP, topical drop administration and AH flow measurements. All monkeys were free of any ocular abnormalities according to slit lamp biomicroscopy at the time measurements were taken. For outflow facility measurements, anesthesia was induced with i.m. ketamine followed by intravenous sodium pentobarbital (15 mg/kg, supplemental dose 5–10 mg/kg).
Serum calcium analysis
Blood samples from rats were obtained from the tail artery. Blood samples from monkeys were obtained from the femoral artery. Whole blood was centrifuged at 1100 × g for 15 min at 25°C. Serum was removed and stored at −20°C until analysis. Serum was diluted 1:40 with 1 g/L lanthanum chloride (LaCl3) [12] and calcium concentration was determined using a 3110 atomic absorption spectrometer (Perkin Elmer, Norwalk, CT).
Rat microarray
Vitamin D-deficient rats were given a single intravenous dose of either 730 ng of 1,25-(OH)2D3/kg of body weight in ethanol or ethanol vehicle (control). Rats were anesthetized with isoflurane and decapitated 1, 3, 6, 10 and 24 h after injection of the dose or vehicle. There were three rats in each group for each time point. Blood was collected at the same time for determination of serum calcium concentration. For each rat, the first 15 cm of intestine (duodenum) was removed, slit longitudinally and scraped with a glass slide. The mucosa was placed in a vial with GTC extraction buffer supplemented with 2% β-mercaptoethanol (PolyATtract System 1000, Promega Corp., Madison, WI), homogenized at high speed with a PowerGen 700 (Fisher Scientific, Pittsburgh, PA), flash frozen in liquid N2 and stored at −80° C. Experiments were done in duplicate.
Rat mRNA
For each time point, Poly(A+) RNA was isolated from pooled homogenized mucosa of three 1,25-(OH)2D3 or three vehicle treated rats. The mRNA was isolated using the PolyATtract System 1000 (Promega Corp., Madison, WI) and purified using an RNeasy kit (Qiagen, Chatsworth, CA). The quality, integrity and quantity of the Poly(A+) RNA were determined by agarose gel electrophoresis, UV absorption spectrophotometry and the use of an Agilent Bioanalyzer 2100 (Agilent Technologies, Palo Alto, CA).
Mouse microarray
Primary fetal mouse calvarial cells were isolated and cultured in αMEM containing 10% FBS as described [13]. Cells were plated in 2 × 6-well plates (5×105 cells/well) and cultured with medium changes performed on days 1 and 4. On day 4, cells on 1 plate were treated with 1,25-(OH)2D3 (10 nM final concentration). A second plate was used as the control. After 24 h of incubation with 1,25-(OH)2D3, cells were harvested and total RNA was isolated with Trizol reagent (Invitrogen Life Technologies, Carlsbad, CA). The mRNA was further purified using an RNeasy kit (Qiagen, Chatsworth, CA). The quality, integrity and quantity of the total RNA were assessed by agarose gel electrophoresis and UV absorption spectrophotometry. Experiments were done in triplicate.
Microarray probe
Double-stranded cDNA was synthesized from 3 μg of rat polyadenylated poly(A+) RNA or 13 μg mouse total RNA using the Superscript Choice system (Invitrogen Life Technologies, Carlsbad, CA), all according to the Affymetrix Gene Expression manual (Affymetrix, Inc., Santa Clara, CA). Following phenol/chloroform extraction and ethanol precipitation, a biotin-labeled in vitro transcription reaction was performed using the cDNA template and BioArray High Yield In Vitro Transcription kit (Enzo Life Sciences, Farmingdale, NY). The cRNA was fragmented at 0.7 – 1.1 μg/μl final concentration in 1X fragmentation buffer (40 mM Tris-acetate, pH 8.1, 100 mM potassium acetate, 30 mM magnesium acetate). The size of cRNA before (0.5 kb and longer) and after (35–200 base fragments) fragmentation was checked by agarose gel electrophoresis.
Microarray hybridization
The hybridization reaction and the automated hybridization procedure were performed by the Gene Expression Center at the Biotechnology Center at the University of Wisconsin-Madison as described previously [2]. Each probe was tested on an Affymetrix Test3 Array and the quality of the cDNA and cRNA was determined by a 3’/5’ ratio of housekeeping genes within the array (ubiquitin, rat glyceraldehyde 3-phosphate dehydrogenase, β-actin, and hexokinase). If the sample passed the quality control on the Affymetrix Test3 Array, it was hybridized to Affymetrix high-density rat oligonucleotide arrays (Rat Expression Array 230 2.0) or to mouse arrays (Mouse Genome 430 2.0 Arrays). (Affymetrix GeneChip® Expression Analysis Technical Manual; http://www.affymetrix.com/support/technical/manual/expressionmanual.affx). Expression data were analyzed using the Affymetrix Microarrray Suite software version 5.0 (MAS 5.0). Comparison tables for each time point for 1,25-(OH)2D3 vs. vehicle-treated rats were generated in EXCEL (Microsoft). For each comparison, e.g. 1,25-(OH)2D3 treated relative to control (vehicle treated), and for each cDNA represented in the array, a ratio (e.g. 1,25(OH)2D3/control) and an absolute difference of intensities for 1,25(OH)2D3 and vehicle treated were calculated. Microarray data validation was done by Quantitative Real Time PCR (Q-PCR) as described previously [2].
Monkey treatments and IOP measurements
Baseline pretreatment IOP was determined by Goldmann applanation tonometry [14] with non-dairy creamer used as a tear film indicator [15]. Two or three baseline IOP measurements were taken 5 min apart. Eye drops were delivered in two different ways: 1. Delivery without occlusion of the nasolacrimal duct. Monkeys were treated topically with 5 μl of 1,25-(OH)2D3 (0.1–15 μg) to one eye and vehicle (propylene glycol) to the opposite eye twice daily for 5 treatments total. Drops were administered to the central cornea while the monkeys were in a supine position with their eyelids held open for at least 30 sec post drops; 2. Delivery with occlusion of the nasolacrimal duct. Eyelids were held open only long enough to ensure that the drop was delivered onto the cornea. Then the nasolacrimal duct was immediately occluded by digital pressure while the eyes were kept in an upright position for 2 min. At the end of the 2 min, any tears were gently blotted from the temporal corner of the eye with gauze (new gauze for each eye).
In some cases, IOP was also measured prior to the morning or afternoon treatment. On the third day, IOP was measured prior to the morning treatment. Following the fifth treatment, IOP was measured hourly for 6–8 h and, in some cases, also at 12, 24, and 48 h. Slit lamp examination (to determine the presence of biomicroscopic cells or flare) was performed prior to the 1st IOP measurement and at hours 3 and 6 (24 and 48 h where appropriate). Monkeys were allowed to rest for at least 2 wk between studies. There were usually 8 monkeys for each dose studied, treated in groups of 2 or 4.
Mean arterial blood pressure
Systolic and diastolic blood pressure values, MAP and heart rate were recorded via a cuff, attached to either a Dinamap PRO-100 monitor (Critikon, Tampa, FL) or a Cardell model 9402 monitor.
AH formation
AH formation rate was determined by ocular scanning fluorophotometry (Fluorotron Master, OcuMetrics Inc, Mountain View, CA) as previously described [16]. Fluorescein drops were administered at least 30 min after the fourth treatment (see above) with 1,25-(OH)2D3 or vehicle. On day 3, prior to the fifth treatment, biomicroscopy was done and IOP was measured. Following the fifth treatment, scans for treatment regimen 1 were taken hourly beginning 1 h after treatment until 6 duplicate scans were collected. IOP was measured at 1, 3, and 6 h. For treatment regimen 2, scans were taken at 30-min intervals, beginning 1 h after treatment, until 7 duplicate scans were collected. IOP response was verified at 2, 3, and 4 h. Baseline scans for both regimens were collected within 2 wk before the treatment study and, for treatment regimen 1, at least 2–3 wk after treatment. Post-treatment AH formation rates were compared to the average of the average of pre- and post-treatment baselines (regimen 1) or to pre-baseline rates (regimen 2) and to the rates in the vehicle treated eyes by the paired t-test for ratios different from 1.0. There was no baseline measurement after completion of treatments for monkeys used for regimen 2 since most of these monkeys were subsequently used for outflow facility determinations on day 4.
Outflow facility
Outflow facility was determined in pentobarbital-anesthetized monkeys [17] by two-level constant pressure perfusion of the anterior chamber with Bárány’s perfusand [18]. Since treatment regimen 1 usually produced a bilateral IOP response, intracameral bolus dosing was utilized in an attempt to achieve a unilateral response to 1,25-(OH)2D3 to assess the effect on outflow facility. Four monkeys (group A) received a single bolus injection of 1 μl containing 1 μg 1,25-(OH)2D3 into the anterior chamber of one eye (treated eye) or 1 μl of propylene glycol into the anterior chamber of the fellow eye (control eye). Four monkeys (group B) were treated topically with 5 μg of 1,25-(OH)2D3 in 5 μl of propylene glycol or vehicle (5 μl of propylene glycol) twice daily for two days in opposite eyes as described above. Then, following baseline outflow facility measurements on the third day, the fifth treatment was administered as a single bolus injection of 1 μl of propylene glycol containing 1 μg 1,25-(OH)2D3 into the anterior chamber of one eye (treated eye) or 1 μl of propylene glycol into the anterior chamber of fellow eye (control eye). Following injections, the treatment bolus was allowed to wash for 5 min with flow from external reservoirs containing Bárány’s perfusand. Then the contents of the anterior chamber were mixed by blowing cold air on the cornea to enhance convection. Reservoirs were closed for 75 min, then reopened and outflow facility measured for 60–90 min. Another group (group C) of monkeys was utilized to determine the effects on outflow facility of a single bolus injection of 1 μl of propylene glycol into one eye, Bárány’s perfusand into the opposite eye. Data were averaged for the entire 60–90 min period and for 30-min intervals and then were compared to baseline and to the vehicle treated eyes. Ratios were compared by the two-tailed paired t-test for ratios different from 1.0.
For treatment regimen 2, monkeys were treated topically with 5 μg of 1,25-(OH)2D3 in 5 μl of propylene glycol or vehicle (5 _l of propylene glycol) twice daily as described above with nasolacrimal duct occlusion (5–7 treatments). Then, following the fifth or seventh treatment on day 3 or 4, respectively, IOP was monitored for 1 or 2 h. Monkeys were then anesthetized with pentobarbital, each eye was cannulated with a single branched needle, and outflow facility measurements collected for 1.5–2 h during the interval 2–4 h post treatment. After 4–6 wk of recovery, baseline outflow facility measurements were collected in the same monkeys for 2 h. Baseline outflow facility data were collected after recovery from the treatment in order to include only monkeys that demonstrated an IOP response to 1,25-(OH)2D3 in the analysis. Data were averaged for the entire 90–120 min period and for 30-min intervals and then were compared to baseline and to the vehicle treated eyes. Ratios were compared by the two-tailed paired t-test for ratios different from 1.0.
Uveoscleral Outflow
An indication of whether or not uveoscleral outflow is involved in the IOP lowering mechanism was ascertained by blocking the uveoscleral outflow pathway through the ciliary muscle by precontracting the muscle with pilocarpine [19]. Monkeys were treated (regimen 2 with nasolacrimal duct occlusion) twice daily for two days with 5 μg of 1,25-(OH)2D3 in PG to both eyes. On the third day, prior to the fifth treatment, and following baseline IOP and biomicroscopy, monkeys were given an intramuscular injection of 0.01 mg/kg atropine to mitigate systemic effects of pilocarpine. This systemic atropine dose has little to no effect on the ocular responses to this large local dose of pilocarpine [20]. After 5 min, one eye received topical treatment with 1.0 mg of pilocarpine HCl (2×5 μl). IOP was measured 30 min later [19]. Then both eyes received the fifth 5 μg treatment of 1,25-(OH)2D3 and IOP was measured hourly for 6 h as above.
On a separate occasion, the effect of pilocarpine alone on IOP in 4 of the same monkeys was determined to confirm that pilocarpine produced an IOP response and to assess its magnitude. The IOP responses in both eyes after 1,25-(OH)2D3 treatment were compared to baseline before and after pilocarpine and to each other and after correction for the IOP response to pilocarpine alone.
Results
1α,25-(OH)2D3 modulates the expression of genes involved in the regulation of IOP
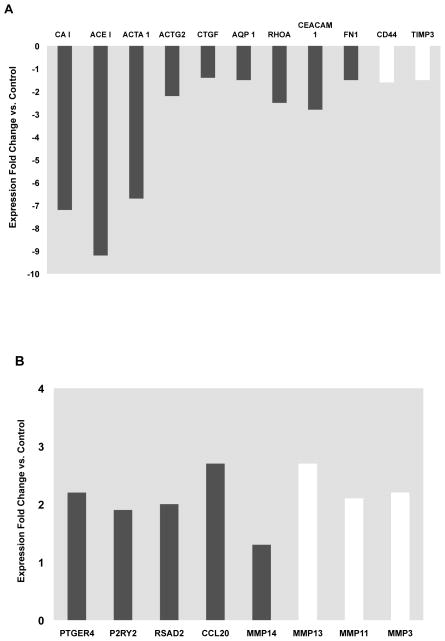
We used rat and mouse microarrays for identification of novel vitamin D target genes as described [2,3]. By comprehensive microarray data analysis we found that 1,25-(OH)2D3 altered the expression of genes known to be involved or relevant to the regulation of IOP. The strongest decreases in expression by 1,25-(OH)2D3 were observed for carbonic anhydrase I (CAI), angiotensin I converting enzyme (ACE) and actin alpha (ACTA1) (Fig. 1A). Also significantly down-regulated were actin gamma (ACTG2), connective tissue growth factor (CTGF), aquaporin 1 (AQP1), ras homolog gene family, member A (RHOA), carcinoembryonic antigen-related cell adhesion molecule 1 (CEACAM), fibronectin 1 (FN1), CD44 and tissue inhibitor of metalloproteinase 3 (TIMP3) (Fig. 1A). Significant increases were found in the expression of prostaglandin E receptor 4 for PGE2 (PTGER4), purinergic receptor P2Y, G-protein coupled, 2 (P2RY2), radical S-adenosyl methionine domain containing 2 (RSAD2) or Test5, chemokine (C-C motif) ligand 20 (CCL20) and matrix metalloproteinases 3 (MMP3), 11 (MMP11) and 13 (MMP13) and 14 (MMP14) (Fig. 1B).
Fig. 1. Expression of genes modulated by 1,25-(OH)2D3 that are involved in the regulation of IOP.
(A) genes down-regulated by 1,25-(OH)2D3. (B) Genes up-regulated by 1,25-(OH)2D3. Solid bars represent data from rat intestine and open bars represent data from mouse calvarial cells. For each gene, the fold change in expression was the average of 2–3 microarray experiments (6–9 rats per data point). The shown fold changes were statistically significant (p<0.05).
In our study, 1,25-(OH)2D3 decreased the expression of several other genes (vasoactive intestinal peptide, topoisomerase I, MMP2) (data not shown) that were consistently found to be up-regulated in human trabecular meshwork (TM) during a pressure-induced homeostatic response [21].
1,25-(OH)2D3 and analog markedly reduce IOP in nonhuman primates
Depending on the mode of application, the 1,25-(OH)2D3 drops could produce either bilateral (similar response in both eyes) or unilateral IOP responses.
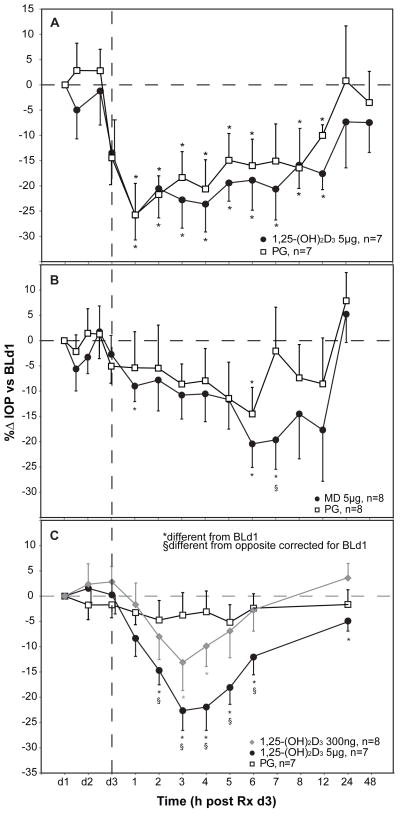
Without nasolacrimal duct occlusion, a bilateral IOP response was frequently observed for 1,25-(OH)2D3 (Fig. 2A). Prior to the fifth treatment with 5 μg of 1,25-(OH)2D3 on day 3 (d3), IOP had significantly decreased by approximately 20% in both eyes (p<0.05). Following the fifth topical treatment with the 5 μg dose of 1,25-(OH)2D3 or vehicle, IOP decreased bilaterally by an additional 10% over the next 1–4 h before gradually returning to near pretreatment baseline after 48 h (Fig. 2A). The contralateral vehicle response for the 5 μg dose was of the same magnitude or slightly greater than with propylene glycol alone (Fig. 2A). In a separate experiment, vehicle (propylene glycol) alone for 3 days with no treatment of the contralateral eye had little or no effect on IOP.
Figure 2. 1,25-(OH)2D3 and 2MD decrease IOP in cynomolgus monkey eyes in vivo.
A. Bilateral IOP response following unilateral topical treatment with 5 μg 1,25-(OH)2D3 to one eye (black circles), propylene glycol (PG) vehicle (white squares) to the opposite eye, without nasolacrimal duct occlusion. Baseline IOP (mmHg ± sem) prior to the first treatment on day 1 was: 1,25-(OH)2D3 = 18.6 ± 0.8; PG = 18.4 ± 1.0. N= 7 except at 48 h when n=5. B. Bilateral IOP response following unilateral topical treatment with 5 μg 2MD to one eye (black circles), PG vehicle to the opposite eye (white squares), without nasolacrimal duct occlusion. N=8 for all time-points except hrs 7, 8, and 12 where n=7. Baseline IOP (mmHg ± sem) prior to the first treatment on day 1 was: PG = 18.8 ± 0.8; 2MD = 18.9 ± 1.0. C. Unilateral IOP dose-response to 1,25-(OH)2D3 (5 μg - black circles; 300 ng – grey diamonds) or to PG vehicle (white squares) following treatment with nasolacrimal duct occlusion. Baseline IOP (mmHg ± sem) prior to the first treatment on day 1 was: PG = 19.2 ± 0.5; 300 ng 1,25-(OH)2D3 = 18.8 ± 0.5; 5 μg 1,25-(OH)2D3 = 19.1 ± 0.3 (see Materials and Methods for details). Data are mean ± sem. Significantly different from baseline on day 1, (*) (#) p<0.05 minimum; significantly different compared to the opposite eye after correction for baseline day 1; § p<0.05 minimum, d = day.
To investigate whether or not other vitamin D analogs can lower IOP, we treated monkey eyes with drops containing 5 μg the vitamin D analog 2MD (Fig. 2B). After the fifth unilateral topical application of 5 μg 2MD in one eye vs. PG vehicle in the contralateral eye, the IOP gradually decreased by 20% in the ipsilateral eye and 15% or less in the contralateral eye after 7–8 h, (4 h later compared to 1,25-(OH)2D3) with a few significant points (Fig. 2B).
When the nasolacrimal duct was occluded for 2 min post-treatment, a unilateral IOP response was found after unilateral treatment with 1,25-(OH)2D3, which was dose dependent (Fig. 2C). IOP in the control (PG treated) eye did not change during the time of the study. IOP at both the 300 ng and the 5 μg doses of 1,25-(OH)2D3 was significantly decreased in the treated eyes at 2–6 h compared to the contralateral vehicle control eyes (Fig. 2C).
Effects of topical application of 1,25-(OH)2D3 on serum calcium level or mean arterial pressure in monkeys
Since vitamin D functions to maintain serum calcium level [1], we monitored the serum calcium levels as well as mean arterial pressure in monkeys as indicators of whether or not the topically applied 1,25-(OH)2D3 reaches sufficient levels to produce a systemic effect. Topical treatment with 5 μg of 1,25-(OH)2D3 for 3 days without nasolacrimal duct occlusion did not significantly elevate serum calcium levels.
Following the 5th topical treatment with 5 μg of 1,25-(OH)2D3, without nasolacrimal duct occlusion, the mean arterial pressure (MAP) in monkeys tended to decrease compared to the baseline MAP measured prior to the first treatment (not shown).
Effect of 1,25-(OH)2D3 on AH dynamics in eyes of nonhuman primates
Since IOP is determined by AH production by the ciliary body and by AH drainage through the trabecular and uveoscleral drainage pathways we investigated the effect of 1,25-(OH)2D3 on AH dynamics.
There were no changes in the AH formation rates during the interval of maximum IOP response in vehicle control or in 5 μg 1,25-(OH)2D3 treated eyes compared to baseline or to each other at any time interval regardless of whether nasolacrimal duct occlusion was used during treatments (Table 1, data for separate time intervals are not shown).
Table 1.
Aqueous humor formation (AHF) in cynomolgus monkeys after multiple topical applications of 5 μg 1,25-(OH)2D3 or vehicle (propylene glycol).
| AHF (μl/min) | |||
|---|---|---|---|
| Treated | Vehicle | Treated/Control | |
| Bilateral IOP response without nasolacrimal duct occlusion (n=6) | |||
| Hours 1–6 | |||
| Baseline | 1.36 ± 0.11 | 1.46 ± 0.08 | 0.93 ± 0.06 |
| 1,25-(OH)2D3 | 1.53 ± 0.10 | 1.52 ± 0.10 | 1.01 ± 0.07 |
| 1,25-(OH)2D3/BL | 1.14 ± 0.06 | 1.05 ± 0.06 | 1.10 ± 0.07 |
| Unilateral IOP response with nasolacrimal duct occlusion (n=8) | |||
| Hours 1–4 | |||
| Baseline | 1.44 ± 0.17 | 1.35 ± 0.14 | 1.07 ± 0.05 |
| 1,25-(OH)2D3 | 1.65 ± 0.22 | 1.54 ± 0.19 | 1.06 ± 0.03 |
| 1,25-(OH)2D3/BL | 1.29 ± 0.20 | 1.29 ± 0.18 | 1.00 ± 0.05 |
Data are mean ± sem. AHF units are μl/min; ratios are unitless. BL, baseline.
AH formation (μl/min) was measured by fluorophotometry after the 5th topical bid treatment with 1,25-(OH)2D3 or vehicle to opposite eyes with or without nasolacrimal duct occlusion as indicated. There was no effect of 1,25-(OH)2D3 on AHF.
Comparison of the cumulative 90-min outflow facilities after intracameral bolus injection of 1,25-(OH)2D3 or vehicle to their respective baselines showed that outflow facility increased over the entire 90-min period for both eyes with no significant differences between them for either treatment regimen (Table 2A,B). Since outflow facilities in both 1,25-(OH)2D3 and vehicle treated eyes increased compared to baseline by the same extent, we attribute this bilateral outflow facility increase simply to the “washout” phenomenon inherent in anterior chamber perfusions [16,22–25]. Intracameral PG alone had no effect on outflow facility (Table 2C). Outflow facility measured from 2–4 h after the 5th or 7th topical treatment of 1,25-(OH)2D3 with nasolacrimal duct occlusion showed an insignificant 35% increase in outflow facility compared to the contralateral eye corrected for baseline measured on a separate day (Table 2D).
Table 2.
Outflow facility in monkeys after topical and/or intracameral 1,25-(OH)2D3
| Outflow facility (μl/min/mmHg) | |||
|---|---|---|---|
| Treated | Control | Treated/Control | |
| A. 1 μg Intracameral (n=4) | |||
| Baseline | 0.24 ± 0.08 | 0.29 ± 0.07 | 0.90 ± 0.34 |
| 1,25-(OH)2D3 | 0.37 ± 0.07 | 0.47 ± 0.05 | 0.82 ± 0.20 |
| 1,25-(OH)2D3/BL | 1.80 ± 0.30 | 1.79 ± 0.30 | 1.04 ± 0.13 |
| B. 5 μg Topical (bid, 4 treatments); 1 μg Intracameral (n=4) | Treated | Control | Treated/Control |
| Baseline | 0.31 ± 0.12 | 0.38 ± 0.23 | 1.11 ± 0.17 |
| 1,25-(OH)2D3 | 0.51 ± 0.26 | 0.68 ± 0.43 | 0.91 ± 0.27 |
| 1,25-(OH)2D3/BL | 1.38 ± 0.23 | 1.74 ± 0.20 | 0.84 ± 0.18 |
| Combined data from A and B (n=8) | Treated | Control | Treated/Control |
| Baseline | 0.28 ± 0.07 | 0.34 ± 0.11 | 1.00 ± 0.18 |
| 1,25-(OH)2D3 | 0.44 ± 0.13 | 0.58 ± 0.20 | 0.87 ± 0.16 |
| 1,25-(OH)2D3/BL | 1.59 ± 0.19* | 1.77 ± 0.16* | 0.94 ± 0.11 |
| C. 1 μl intracameral propylene glycol (n=5) | Treated | Control | Treated/Control |
| Baseline | 0.34 ± 0.04 | 0.47 ± 0.11 | 0.90 ± 0.28 |
| Propylene Glycol | 0.34 ± 0.06 | 0.49 ± 0.10 | 0.72 ± 0.06* |
| PropGly/BL | 1.03 ± 0.18 | 1.09 ± 0.17 | 1.03 ± 0.18 |
| D. 5 μg topical VitD (5–7 treatments) with nasolacrimal duct occlusion (n=8) | Treated | Control | Treated/Control |
| Baseline | 0.38 ± 0.05 | 0.45 ± 0.04 | 0.85 ± 0.10 |
| 1,25-(OH)2D3 | 0.45 ± 0.05 | 0.46 ± 0.06 | 1.03 ± 0.10 |
| 1,25-(OH)2D3/BL | 1.25 ± 0.12 | 1.05 ± 0.14 | 1.35 ± 0.24 |
Data are mean ± sem. Outflow facility units are μl/min/mmHg; ratios are unitless. BL, baseline. A. Following baseline measurements, intracameral 1,25-(OH)2D3 was administered to one eye; propylene vehicle (1 μl) to the contralateral control eye. Outflow facility measurements post treatment were begun 75 min after 1,25-(OH)2D3 administration and continued for 90 min. B. Topical administration bid for 2 days (4 treatments) with intracameral treatment on the 3rd day as for A. C. Intracameral bolus injection of 1 μl propylene glycol to one eye, Barany’s perfusand to the contralateral control eye. Outflow facility measurements were begun 75 min post treatment and continued for 90 min. D. Outflow facility was measured on day 3 or 4 following twice daily treatment with 5 μg 1,25-(OH)2D3 to one eye or 5 μl propylene glycol to the contralateral control eye. The nasolacrimal duct was occluded for 2 min following each administration which resulted in a unilateral IOP reduction. Outflow facility was measured for 2 h during the interval 2–4 h after the 5th or 7th treatment. Baseline was measured on a separate day.
No significant difference was found between eyes after correction for baseline when the data for the entire 90–120 min period were analyzed or when 30 min increments were analyzed (not shown). Significantly different from 1.0 by the two-tailed paired t-test:
p<0.05
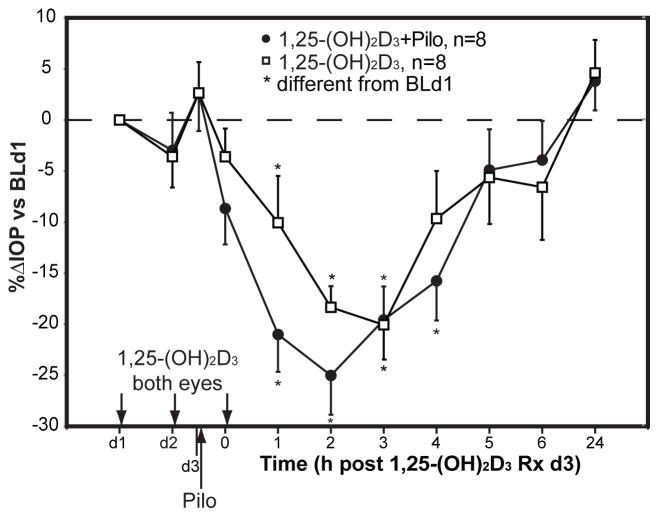
Precontraction of the ciliary muscle with pilocarpine to block uveoscleral outflow prior to 1,25-(OH)2D3 treatment suggested that uveoscleral outflow was not involved in the IOP-lowering response to 1,25-(OH)2D3. The pilocarpine effect on IOP was somewhat additive to that of 1,25-(OH)2D3 (Fig. 3). However, the magnitude of the pilocarpine response alone was of the similar magnitude to that of 1,25-(OH)2D3. In the separate experiment, unilateral application of 1 mg pilocarpine to the eye followed by bilateral PG application produced a unilateral IOP reduction, confirming the effectiveness of the pilocarpine treatment.
Fig. 3. IOP response to 5 μg 1,25-(OH)2D3 after pretreatment with pilocarpine (Pilo) to block uveoscleral outflow.
Monkeys were treated twice daily with 5 μg 1,25-(OH)2D3 to both eyes. Prior to the 5th 1,25-(OH)2D3 treatment on day 3, one eye was treated with 1mg Pilo to contract the ciliary muscle and block uveoscleral outflow and after 30 min both eyes received the fifth 5 μg treatment of 1,25-(OH)2D3 (see Materials and Methods for details). White squares represent the IOP change in the eye treated with 1,25-(OH)2D3 only and black circles represent the IOP change in the eye pretreated first with pilocarpine and then treated with 1,25-(OH)2D3. After the 5th treatment with 1,25-(OH)2D3, there was no apparent suppression of the IOP response to 1,25-(OH)2D3 as a result of pilocarpine pretreatment. Data are mean ± sem. Significantly different from 0.0: *p<0.05, minimum. IOP (mmHg ± sem) prior to the first treatment on day 1 was: 1,25-(OH)2D3 = 18.9 ± 1.0; 1,25-(OH)2D3+Pilo = 19.1 ± 0.9.
Discussion
During the course of our investigation of the molecular mechanism whereby 1,25-(OH)2D3 induces intestinal calcium absorption in rats in vivo [2], regulates genes responsible for detoxication of endo- and xenobiotics [3], and stimulates bone formation in mouse cells in vitro [13], we carried out a microarray study to discover possible genes involved in these processes. We unexpectedly found that 1,25-(OH)2D3 and 2MD regulate expression of genes that are involved in the regulation of IOP. This finding prompted an investigation into whether vitamin D analogs affect IOP.
1,25-(OH)2D3 markedly suppressed expression of angiotensin I converting enzyme (ACE), carbonic anhydrase (CAI) and Ras homolog gene family, member A (RHOA) and significantly increased expression of chemokine (C-C motif) ligand 20 (CCL20) (Fig. 1A) [2]. Carbonic anyhydrase inhibitors are widely employed for glaucoma therapy [26].
It also became clear that 1,25-(OH)2D3 strongly down-regulates the expression of cytoskeleton genes (alpha and gamma actins), cell adhesion genes (CEACAM and CD44), and major extracellular matrix (ECM) genes (RHOA and fibronectin I) (Fig. 1A). 1,25-(OH)2D3 also increased expression of several other ECM genes: matrix metalloproteinases 3, 11, 13, 14 (Fig. 1B) while decreasing expression of their inhibitor TIMP3 (Fig. 1A). Reductions in RHOA, fibronectin 1, CD44 and elevated level of matrix metalloproteinases after the 1,25-(OH)2D3 treatment can remodel the ECM, resulting in an enhancement of fluid outflow by decreasing the outflow resistance due to disruption of the cellular adhesions and reductions in contractility molecules [27,28]. Actin disruptions can lead to alterations in cellular morphology and/or adhesions, which, in the anterior segment of the eye, can result in relaxation of the trabecular meshwork resulting in fluid outflow, thereby reducing IOP [28].
Other genes affected by 1,25-(OH)2D3 that could be involved in regulating IOP are aquaporin 1 channel (AQP1) (Fig. 1A) and purinergic receptors P2Y, G-protein coupled, 2 (P2RY2) (Fig. 1B). AQP1 is a water channel and is expressed at sites of aqueous fluid production and outflow. Mice deficient in AQP1 gene have lower AH inflow and lower IOP than normal controls therefore inhibition of AQP1 might be considered for glaucoma therapy [29]. P2Y2 receptor activation stimulated release of prostaglandin E2 in rat kidney [30] and caused vasodilatation [31].
Recent studies in hypertensive rats suggested a strong positive correlation between blood pressure and IOP [32,33]. ACE expression is markedly decreased by 1,25-(OH)2D3 [2]. ACE is known to be a key part of the renin angiotensin system that stimulates blood pressure by the conversion of angiotensin I (AngI) to angiotensin II (AngII). ACE can also inactivate the vasodilatator bradykinin [33]. Both of these effects elevate arterial blood pressure, and ACE inhibitors are widely used for the treatment of hypertension. The eye is also believed to contain a renin-angiotensin system that may be involved in the regulation of IOP. The presence of ACE activity, the concentrations of angiotensinogen and angiotensin II, and the density of angiotensin-II AT1 receptors in ocular tissues and fluids have been demonstrated in several species, including humans [32,34–36]. Intracameral infusion of angiotensin in monkey eyes in vivo decreases outflow facility [37]. IOP and BP correlation have also been established in a comprehensive human study suggesting a common mechanism or common genes that may be controlling pressure both in the eye and in the vascular system [38,39]. Topical and oral administration of ACE inhibitors have been shown to lower IOP in animal models and in humans; they are currently under development as glaucoma therapeutic agents [40,41]. Epidemiological and clinical studies over many years have established an inverse relationship between vitamin D and blood pressure in the human population [42,43].
We found that 1,25-(OH)2D3 up-regulated expression of genes such as chemokine (C-C motif) 20 (CCL20) and radical S-adenosyl methionine domain containing 2 (RSAD2) and down-regulated the expression of connective tissue growth factor (CTGF Fig. 1A,B), the genes that counteract the induced ocular hypertension [44].
Our current studies show that both 1,25-(OH)2D3 and 2MD significantly lower IOP in nonhuman primates following topical application. The effect of 1,25-(OH)2D3 can last for more than 12 h (Fig. 2E), although 2MD is more potent than 1,25-(OH)2D3 in some physiological responses in other organs [13], 2MD proved to be less effective than 1,25-(OH)2D3 in lowering IOP. The reason 2MD is less effective than 1,25-(OH)2D3 in the eye is unknown. However, 2MD is either equally or less potent than 1,25-(OH)2D3 on intestine while being 30–100 times more potent than 1,25-(OH)2D3 on bone [13]. Likely, 2MD is a selectively potent analog that is less effective than 1,25-(OH)2D3 on intestine and in the eye. Of all the compounds tested so far, 1,25-(OH)2D3 is the most active.
Interestingly, we observed two types of IOP responses to 1,25-(OH)2D3 treatment: a strong bilateral IOP lowering response when applied unilaterally without nasolacrimal duct occlusion or a unilateral IOP lowering response when applied unilaterally with nasolacrimal duct occlusion (Fig. 2A,C). Cannabinoids, opioids [16,45], Ca2+ channel blockers [46] and α2- and β-adrenergic blockers [47,48] also decrease IOP bilaterally but not to the same extent as we observed for 1,25-(OH)2D3. The mechanism of bilateral IOP decrease by ocular agents is not clearly understood or explained but there is the possibility that CNS or peripheral nervous systems might be involved [49]. However, our results suggest that 1,25-(OH)2D3 was transferred to the untreated eye via the nasolacrimal duct.
The dose of 1,25-(OH)2D3 needed appeared large and un-physiologic (1–5 μg). However, only about 1% of a topically administered dose of most agents ever enters the eye [50]. Thus, 10–50 ng (1% of our dose) is in the physiologic range.
The balance between the AH formation and drainage determines the intraocular pressure. The IOP lowering effect by all currently clinically available medications for glaucoma therapy is achieved either by decreasing the production of AH (α and β-adrenergic blockers, carbonic anhydrase inhibitors and Na+/K+-ATPase inhibitors) or by improving its outflow either through the conventional pathway through the TM and canal of Schlemm (cholinergics, indirectly via ciliary muscle contraction), β2-adrenergic agonists (epinephrine, direct effects on TM and Schlemm’s canal cells), or via the uveoscleral outflow pathway (prostaglandins) [7,51–55].
The mechanism by which 1,25-(OH)2D3 reduces IOP is not clear at this time. 1,25-(OH)2D3 did not decrease AH formation or increase AH uveoscleral outflow (Tables 1, 2 and Fig. 3). We did find the 35% increase with 1,25-(OH)2D3 in outflow facility but the change did not achieve statistical significance (Table 2D). Our experiment to block uveoscleral outflow with pilocarpine suggested that this did not affect the IOP-lowering response to 1,25-(OH)2D3. However, the magnitude of the pilocarpine response alone was of a similar magnitude to that of 1,25-(OH)2D3, confounding interpretation.
IOP is also determined by other factors such as 1) episcleral vein pressure [56], which is not easily measured in the cynomolgus monkey [57,58]; 2) ocular blood flow [59]. It is possible that the IOP lowering effect of vitamin D analogs may be the result of incremental contribution of multiple factors.
In any case, the present results may provide a new therapeutic approach for the treatment of elevated IOP and thus glaucoma.
Highlights.
Vitamin D modulates genes that regulate intraocular pressure.
Topical administration of 1,25-(OH)2D or an analog markedly reduce IOP in monkeys.
1,25-(OH)2D did not change aqueous humor formation or uveoscleral outflow.
1,25-(OH)2D3 or analogs provide a new approach for the treatment of glaucoma.
Acknowledgments
This work was supported by the Wisconsin Alumni Research foundation (HFD), the American Health Assistance Foundation (PLK), an unrestricted grant from Research to Prevent Blindness (PLK), the Core Grant for Vision Research (NEI P30 EY016665) (PLK), and the Ocular Physiology Research and Education Foundation (PLK). We cordially thank Wayne Davis and Sandra Splinter BonDurant from the Gene Expression Center at the Biotechnology Center of UW-Madison, Dr. N. K. Shevde, Prof. J. W. Pike and Pat Mings from the Biochemistry Department, UW-Madison.
Abbreviations Used
- 1,25-(OH)2D3
1α,25-dihydroxyvitamin D3
- 2MD
2-methylene-19-nor-(20S)-1,25-dihydroxyvitamin D3
- IOP
intraocular pressure
- AH
aqueous humor
- TM
trabecular meshwork
- ECM
extracellular matrix
- PG
propylene glycol
- CAI
carbonic anhydrase I
- ACE
angiotensin I converting enzyme
- ACTA1
actin alpha
- ACTG2
actin gamma
- CTGF
connective tissue growth factor
- AQP1
aquaporin
- RHOA
ras homolog gene family, member A
- CEACAM
carcinoembryonic antigen-related cell adhesion molecule 1
- FN1
fibronectin 1
- TIMP3
tissue inhibitor of metalloproteinase 3
- PTGER4
prostaglandin E receptor 4
- P2Y
purinergic receptor
- P2RY2
G-protein coupled, 2
- RSAD2
radical S-adenosyl methionine domain containing 2
- C-C motif
chemokine
- CCL20
chemokine ligand 20
- MMP3
matrix metalloproteinases 3
Footnotes
The authors have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.DeLuca HF. Nutr Rev. 2008;66:S73–S87. doi: 10.1111/j.1753-4887.2008.00105.x. [DOI] [PubMed] [Google Scholar]
- 2.Kutuzova GD, DeLuca HF. Arch Biochem Biophys. 2004;432:152–166. doi: 10.1016/j.abb.2004.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kutuzova GD, DeLuca HF. Toxicol Appl Pharmacol. 2007;218:37–44. doi: 10.1016/j.taap.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Jones G, Strugnell AA, DeLuca HF. Physiol Rev. 1998;78:1193–1231. doi: 10.1152/physrev.1998.78.4.1193. [DOI] [PubMed] [Google Scholar]
- 5.DeLuca HF. Am J Clin Nutr. 2004;80:1689S–1696S. doi: 10.1093/ajcn/80.6.1689S. [DOI] [PubMed] [Google Scholar]
- 6.Kaufman PL, Gabelt BT. In: Essentials in Ophthalmology. Stamper R, Grehn F, editors. Springer-Verlapg; Heidelberg: 2006. pp. 138–155. [Google Scholar]
- 7.Clark AF, Yorio T. Nat Rev Drug Discov. 2003;2:448–459. doi: 10.1038/nrd1106. [DOI] [PubMed] [Google Scholar]
- 8.Tan JC, Peters DM, Kaufman PL. Curr Opin Ophthalmol. 2006;17:168–174. doi: 10.1097/01.icu.0000193079.55240.18. [DOI] [PubMed] [Google Scholar]
- 9.Sicinski RR, Prahl JM, Smith CM, DeLuca HF. J Med Chem. 1998;41:4662–4674. doi: 10.1021/jm9802618. [DOI] [PubMed] [Google Scholar]
- 10.Mellon WS, DeLuca HF. J Biol Chem. 1980;255:4081–4086. [PubMed] [Google Scholar]
- 11.Suda T, DeLuca HF, Tanaka Y. J Nutr. 1970;100:1049–1052. doi: 10.1093/jn/100.9.1049. [DOI] [PubMed] [Google Scholar]
- 12.Halloran BP, DeLuca HF. Arch Biochem Biophys. 1981;208:477–486. doi: 10.1016/0003-9861(81)90534-8. [DOI] [PubMed] [Google Scholar]
- 13.Shevde NK, Plum LA, Clagett-Dame M, Yamamoto H, Pike JW, DeLuca HF. Proc Natl Acad Sci USA. 2002;9:13487–13491. doi: 10.1073/pnas.202471299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaufman PL, Davis GE. Arch Ophthalmol. 1980;98:542–546. doi: 10.1001/archopht.1980.01020030538022. [DOI] [PubMed] [Google Scholar]
- 15.Croft MA, Kiland J, Gange SJ, Aref A, Pelzek CD, Kaufman PL. Basic and Clinical Applications of Vision Science. The Professore Jay M. Enoch Festschrift Volume. In: Lakshminarayanan V, editor. Documenta Ophthalmologica Proceedings Series. Kluwer; The Netherlands: 1997. pp. 213–216. [Google Scholar]
- 16.Rasmussen CA, Gabelt BT, Kaufman PL. Trans Am Ophthalmol Soc. 2007;105:225–238. [PMC free article] [PubMed] [Google Scholar]
- 17.Gabelt BT, Hennes EA, Seeman JL, Tian B, Kaufman PL. Invest Ophthalmol Vis Sci. 2004;45:2732–2736. doi: 10.1167/iovs.04-0083. [DOI] [PubMed] [Google Scholar]
- 18.Bárány EH. Invest Ophthalmol. 1964;3:135–143. [PubMed] [Google Scholar]
- 19.Crawford K, Kaufman PL. Arch Ophthalmol. 1987;105:1112–1116. doi: 10.1001/archopht.1987.01060080114039. [DOI] [PubMed] [Google Scholar]
- 20.Tornqvist G. Acta Phthalmol. 1967;45:429–460. doi: 10.1111/j.1755-3768.1967.tb06508.x. [DOI] [PubMed] [Google Scholar]
- 21.Vittitow J, Borrás T. J Cell Physiol. 2004;201:126–137. doi: 10.1002/jcp.20030. [DOI] [PubMed] [Google Scholar]
- 22.Sabanay I, Tian B, Gabelt BT, Geiger B, Kaufman PL. Exp Eye Res. 2006;82:236–246. doi: 10.1016/j.exer.2005.06.017. [DOI] [PubMed] [Google Scholar]
- 23.Tian B, Kaufman PL. Exp Eye Res. 2005;80:215–225. doi: 10.1016/j.exer.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 24.Volberg T, Tian B, Kaufman PL, Geiger B. Exp Eye Res. 2002;74:411–416. doi: 10.1006/exer.2001.1143. [DOI] [PubMed] [Google Scholar]
- 25.Peterson JA, Tian B, Geiger B, Kaufman PL. Exp Eye Res. 2000;70:307–313. doi: 10.1006/exer.1999.0797. [DOI] [PubMed] [Google Scholar]
- 26.Supuran CT. Nat Rev Drug Discov. 2008;7:168–181. doi: 10.1038/nrd2467. [DOI] [PubMed] [Google Scholar]
- 27.Faralli JA, Schwinn MK, Gonzalez JM, Jr, Filla MS, Peters DM. Exp Eye Res. 2009;88:689–693. doi: 10.1016/j.exer.2008.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tian B, Gabelt BT, Geiger B, Kaufman PL. Exp Eye Res. 2009;88:713–717. doi: 10.1016/j.exer.2008.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang D, Vetrivel L, Verkman AS. J Gen Physiol. 2002;119:561–569. doi: 10.1085/jgp.20028597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Welch BD, Carlson NG, Shi H, Myatt L, Kishore BK. Am J Physiol Renal Physiol. 2003;285:711–721. doi: 10.1152/ajprenal.00096.2003. [DOI] [PubMed] [Google Scholar]
- 31.Marrelli SP. Am J Physiol Heart Circ Physiol. 2001;281:1759–1766. doi: 10.1152/ajpheart.2001.281.4.H1759. [DOI] [PubMed] [Google Scholar]
- 32.Vaajanen A, Luhtala S, Oksala O, Vapaatalo H. Ann Med. 2008;40:418–427. doi: 10.1080/07853890802043924. [DOI] [PubMed] [Google Scholar]
- 33.Vaajanen A, Mervaala E, Oksala O, Vapaatalo H. Curr Eye Res. 2008;33:325–332. doi: 10.1080/02713680802011679. [DOI] [PubMed] [Google Scholar]
- 34.Wallow IH, Sramek SJ, Bindley CD, Darjatmoko SR, Gange SJ. Curr Eye Res. 1993;12:945–950. doi: 10.3109/02713689309020401. [DOI] [PubMed] [Google Scholar]
- 35.Cullinane AB, Leung PS, Ortego J, Coca-Prados M, Harvey BJ. Br J Ophthalmol. 2002;86:676–683. doi: 10.1136/bjo.86.6.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Luhtala S, Vaajanen A, Oksala O, Valjakka J, Vapaatalo H. J Ocul Pharmacol Ther. 2009;25:23–28. doi: 10.1089/jop.2008.0081. [DOI] [PubMed] [Google Scholar]
- 37.Kaufman PL, Bárány EH. Invest Ophthalmol Vis Sci. 1981;20:644–651. [PubMed] [Google Scholar]
- 38.Klein BE, Klein R, Knudson MD. Br J Ophthalmol. 2005;89:284–287. doi: 10.1136/bjo.2004.048710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Duggal P, Klein AP, Lee KE, Klein R, Klein BE, Bailey-Wilson JE. Arch Ophthalmol. 2007;125:74–79. doi: 10.1001/archopht.125.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Constad WH, Fiore P, Samson C, Cinotti AA. Am J Ophthalmol. 1988;105:674–677. doi: 10.1016/0002-9394(88)90063-3. [DOI] [PubMed] [Google Scholar]
- 41.Costagliola C, Di Benedetto R, De Caprio L, Verde R, Mastropasqua L. Eur J Ophthalmol. 1995;5:19–25. doi: 10.1177/112067219500500104. [DOI] [PubMed] [Google Scholar]
- 42.Li YC. J Cell Biochem. 2003;88:327–331. doi: 10.1002/jcb.10343. [DOI] [PubMed] [Google Scholar]
- 43.Li YC, Qiao G, Uskokovic M, Xiang W, Zheng W, Kong J. J Steroid Biochem Mol Biol. 2004;89–90:387–392. doi: 10.1016/j.jsbmb.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 44.Comes N, Borrás T. Physiol Genomics. 2009;38:205–25. doi: 10.1152/physiolgenomics.90261.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kaufman PL. Exp Eye Res. 2008;86:3–17. doi: 10.1016/j.exer.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang RF, Gagliuso DJ, Podos SM. J Glaucoma. 2008;17:73–78. doi: 10.1097/IJG.0b013e318133a845. [DOI] [PubMed] [Google Scholar]
- 47.Gabelt BT, Robinson JC, Hubbard WC, Peterson CM, Debink N, Wadhwa A, Kaufman PL. Exp Eye Res. 1994;59:633–644. doi: 10.1006/exer.1994.1149. [DOI] [PubMed] [Google Scholar]
- 48.Piltz J, Gross R, Shin DH, Beiser JA, Dorr DA, Kass MA, Gordon MO. Am J Ophthalmol. 2000;130:441–453. doi: 10.1016/s0002-9394(00)00527-4. [DOI] [PubMed] [Google Scholar]
- 49.Trzeciakowski JP. J Ocul Pharmacol. 1987;3:367–378. doi: 10.1089/jop.1987.3.367. [DOI] [PubMed] [Google Scholar]
- 50.Kaur IP, Kanwar M. Drug Dev Ind Pharm. 2002;28(5):473–93. doi: 10.1081/ddc-120003445. [DOI] [PubMed] [Google Scholar]
- 51.Nilsson SF, Drecoll E, Lutjen-Drecoll E, Toris CB, Krauss AH, Kharlamb A, Nieves A, Guerra T, Woodward DF. Invest Ophthalmol Vis Sci. 2006;47:4042–4049. doi: 10.1167/iovs.05-1627. [DOI] [PubMed] [Google Scholar]
- 52.Glaucoma and optic neuropathies program. NIH; Bethesda, MD: 2006. National Eye Institute (NEI) National Plan for Eye and Vision Research. [Google Scholar]
- 53.Orihashi M, Shima Y, Tsuneki H, Kimura I. Biol Pharm Bull. 2005;28:65–68. doi: 10.1248/bpb.28.65. [DOI] [PubMed] [Google Scholar]
- 54.Marquis RE, Whitson JT. Drugs Aging. 2005;22:1–21. doi: 10.2165/00002512-200522010-00001. [DOI] [PubMed] [Google Scholar]
- 55.Brubaker RF. Survey Ophthalmol. 2003;48:S17–S20. doi: 10.1016/s0039-6257(03)00003-1. [DOI] [PubMed] [Google Scholar]
- 56.Selbach JM, Posielek K, Steuhl KP, Kremmer S. Ophthalmologica. 2005;219:357–361. doi: 10.1159/000088378. [DOI] [PubMed] [Google Scholar]
- 57.Mäepea O, Bill A. Exp Eye Res. 1989;49:645–663. doi: 10.1016/s0014-4835(89)80060-0. [DOI] [PubMed] [Google Scholar]
- 58.Gaasterland DE, Pederson JE. Invest Ophthalmol Vis Sci. 1983;24:1417–1422. [PubMed] [Google Scholar]
- 59.Kiel JW. The Ocular Circulation. San Rafael (CA): Morgan & Claypool Publishers; 2010. [PubMed] [Google Scholar]