Abstract
Objective
It is uncertain whether migraine prevalence has increased in modern society. The aim of this study was to assess any change in migraine prevalence over an 8-year period among the adult population in Denmark.
Design
Prospective longitudinal population-based study.
Setting
30 000 twin individuals were invited to participate in two cross-sectional questionnaire surveys containing validated questions to diagnose migraine in 1994 and 2002. The twins are representative of the Danish population with regard to migraine and other somatic diseases.
Participants
The 1994 cohort comprised 28 571 twin individuals aged 12–41 years and the 2002 cohort 31 865 twin individuals aged 20–71 years.
Outcome measures
Sex-, age- and subtype-specific incidence and lifetime prevalence as well as 1-year prevalence of migraine.
Results
1-year prevalence in 2002 was 12.3% for migraine, 4.1% for migraine with aura and 8.2% for migraine without aura. Lifetime prevalence of migraine was 16.1% in 1994 (aged 12–41 years) and 25.2% in 2002 (aged 20–71 years). Lifetime prevalence of migraine for age 20–41 was increased from 1994 to 2002 (18.5% vs 24.5%) by 32.2% (95% CI 27.0% to 37.3%; p<0.001). The difference was primarily seen in the population older than 32 years. The increase was especially evident in migraine with aura (5.6% vs 9.4%, p<0.001) but also a significant increase in migraine without aura was found (13.0% vs 15.1%, p<0.001). Eight-year period incidence rate of migraine was 0.141 corresponding to an average annual incidence rate of 17.6 per 1000 person-years.
Conclusions
Lifetime prevalence of migraine in Denmark increased substantially from 1994 to 2002. Part of the increase may be due to increased medical consultation resulting in increased rate of physician diagnosis or awareness due to previously participation in the 1994 survey. It is pertinent to study the environmental causes of the increase and to implement preventive measures.
Article summary
Article focus
Has migraine prevalence increased in modern society?
Key messages
Self-reported migraine prevalence increased substantially in the Danish young adult population.
Sex- and age-specific prevalence and incidence of migraine and its subtypes were estimated in a large population-based sample.
Strengths and limitations of this study
Large sample size made it possible to differentiate between migraine with aura and migraine without aura using the validated diagnostic questions and furthermore subdivide between men and women and to distinguish between age groups.
The validation of the two questions used to identify migraine cases showed that self-reported migraine was only correct in 74.5% of cases, and furthermore, approximately 23.8% of the migraine patients were not identified. Thus, our estimates would tend to be conservative.
Introduction
In 2001, migraine was ranked by the WHO as the 19th of disabling diseases1 causing great societal costs. In 2010, the total societal cost in Europe was estimated to be €18.5 billion per year for the 50 million migraine sufferers.2 Migraine prevalence has been assessed in several large-scale population-based studies,3 4 but studies of incidence are sparse. It is uncertain whether migraine prevalence has increased in modern society. Replicate studies of migraine prevalence in the adult population using the same methodology at all evaluations showed conflicting results.5–9 Furthermore, only few studies have distinguished between migraine with aura (MA) and migraine without aura (MO).
‘The Danish Twin Omnibus 1994 and 2002’ were questionnaire studies among almost 30 000 and 35 000 twin individuals, respectively.10 11 Both studies used the same validated questions to diagnose migraine and its subtypes. In the present publication, the twin status is disregarded and the material is presented as a random sample from the Danish population, which is acceptable since these twins are representative of the whole Danish population with regard to migraine.12
The aim of our study was to estimate sex-, age- and subtype-specific incidence and lifetime prevalence as well as 1-year prevalence of migraine and to assess any change in migraine prevalence over an 8-year period among the young adult population in Denmark.
Materials and methods
The study populations were based on twin cohorts enrolled in the Danish Twin Registry, one of the oldest and most complete population-based twin registries in the world.10 The ascertainment of twins enrolled in this study was done using the Danish Civil Registration System as primary source. This system had since 1 April 1968 registered all persons living in Denmark.10 11 13 The twin cohorts from 1953 to 1982 were identified in 1991 by the mother assuming that a woman had twins if she gave birth to more than one child within three consecutive days.14 Identification of twins born between 1931 and 1952 was based on an algorithm extracting all persons born on the same date, in the same parish and with the same historical surname.10 The Danish Twin Registry is validated and representative of the Danish population as a whole.12 15–17 The lifetime and 1-year prevalence of migraine did not differ in monozygotic twins, dizygotic twins and single individuals.12 The twins were therefore regarded as single individuals in the present study.
The ‘Twin Omnibus 1994’ comprised twin individuals from the cohorts 1953 to 1982 and the ‘Twin Omnibus 2002’ twin individuals from the cohorts 1931 to 1982. The questionnaires investigated self-reported migraine and the cases were identified based on the following questions:
Have you ever had migraine?
Have you ever had visual disturbances that lasted from 5 to 60 min and were succeeded by a headache?
Subjects were classified as having migraine if they answered ‘yes’ to question 1. The second question was to determine whether they had MA or MO. MA was defined as subjects answering ‘yes’ to both questions and MO was defined as subjects answering ‘yes’ to question 1 and ‘no’ to question 2. Subjects answering ‘no’ to question 1 were considered healthy. Any questionnaires containing blanks in these two questions were excluded for the purpose of the present study. Validation of the screening questions showed that it was possible to identify 76% of all subjects with migraine, 85% of all with MA and 72% of all with MO. A detailed description of the validation of screening questions has been published elsewhere.18
In the survey from 2002, participants who answered yes to question 1 were asked to specify whether they had had migraine in the past year or not. This was not a part of the 1994 survey; therefore, 1-year prevalence was only estimated in 2002. The 1-year prevalence rate was calculated as the number of subjects reporting that they had had migraine in the past year divided by the total number of subjects, and the lifetime prevalence rate as the number of subjects reporting migraine in the past year or before that divided by the total number of subjects. Because the age range of the two cohorts was different in 1994 and 2002, comparison of the two prevalence rates was conducted only for twins aged 20–41 years. Comparison of the two groups was performed with χ2 test. The incidence cases were defined as subjects reporting migraine in 2002 who did not report migraine in 1994. The average annual incidence rate was estimated as per 1000 person-years (PYs). Prevalence and incidence estimates were stratified by sex, age and subtypes. Data analyses were performed with PASW Statistics V.18.0 by SPSS Inc.
Results
Participants
Of all the subjects who returned the questionnaire in 1994, 97.1% (n=28 571) had answered both migraine questions. More women (66.0%) had migraine than men (34.0%), whereas a more even distribution of sex was seen in the group without migraine (49% women and 51% men). The migraine group was older than the no-migraine group (men: median =30 vs 27 and mean =29 vs 27; women: median =30 vs 26 and mean =29 vs 26).
In 2002, 91.2% (n=31 865) of all returned questionnaires were complete with regard to both migraine questions. There were more women (69.6%) than men (30.4%) in the migraine group, whereas only little difference was found in the group without migraine (49% women and 51% men). The median and mean age differed with 1 year between the migraine group and the group without migraine (men: median and mean =45 vs 44; women: median =43 vs 42 and mean =44 vs 43).
1-year prevalence
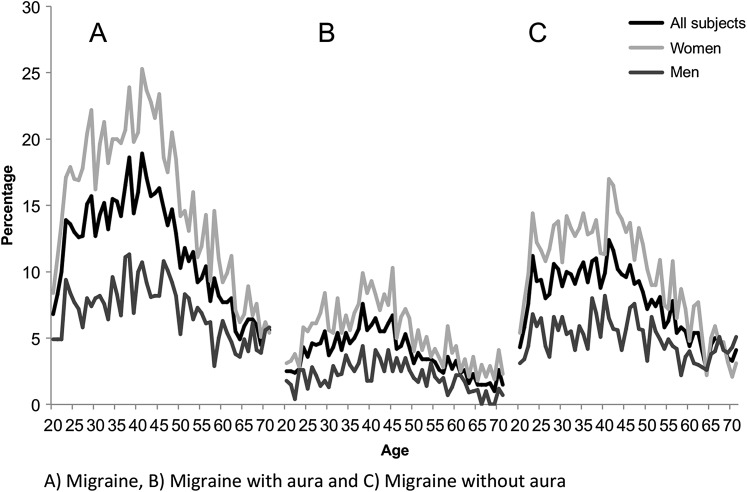
The 1-year prevalence in 2002 was 12.3%. Table 1 shows the sex- and subtype-specific prevalences. The age-specific 1-year prevalence of migraine, MA and MO, is shown in figure 1A–C. The prevalence peaked around age 38–40 in both men and women. For MO, the 1-year prevalence showed a plateau between age 25 and 40, whereas for MA, a sharp peak was seen around age 40.
Table 1.
Sex-specific 1-year prevalence rates of migraine, migraine with aura (MA) and migraine without aura (MO) in 2002 (31 865 subjects aged 20–71 years)
| 2002 | Migraine |
MA |
MO |
||||||
| Rate (%) | 95% CI | n, crude | Rate (%) | 95% CI | n, crude | Rate (%) | 95% CI | n, crude | |
| All subjects | 12.3 | 11.9 to 12.7 | 3927 | 4.1 | 3.9 to 4.3 | 1307 | 8.2 | 7.9 to 8.5 | 2620 |
| Women | 16.5 | 15.9 to 17.2 | 2855 | 5.7 | 5.3 to 6.1 | 983 | 10.8 | 10.4 to 11.3 | 1872 |
| Men | 7.3 | 6.9 to 7.8 | 1072 | 2.2 | 2.0 to 2.5 | 324 | 5.1 | 4.8 to 5.5 | 748 |
Figure 1.
(A–C) The age- and sex-specific 1-year prevalence of migraine and its subtypes in 2002.
Lifetime prevalence
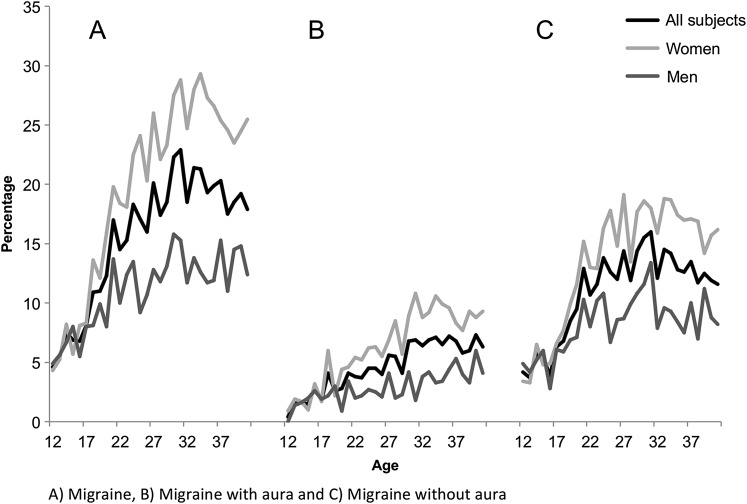
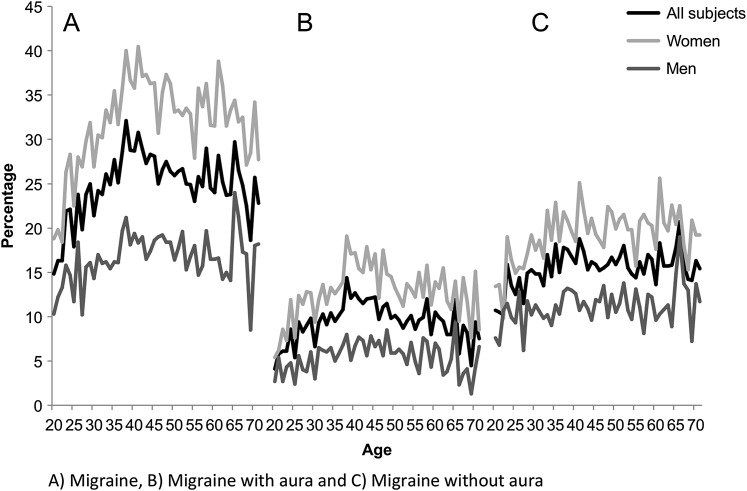
The lifetime prevalence was 16.1% in 1994 (age 12–41) and 25.2% in 2002 (age 20–71). The sex- and subtype-specific prevalence rates for both years are presented in table 2. In 1994, the age-specific lifetime prevalence of migraine in women peaked in the early 30s followed by a small decrease, whereas the prevalence in men showed a plateau between age 27 and 41 (figure 2A–C). The prevalence of MO peaked around age 27–34 in women and around age 31 in men. The MA prevalence slowly increased with age. In 2002, the prevalence of migraine peaked around age 40 and slowly decreased (figure 3A–C). For MO, the prevalence increased to age 40 where it reached plateau. For MA, the prevalence peaked around age 38.
Table 2.
Sex-specific lifetime prevalence rates of migraine, migraine with aura (MA) and migraine without aura (MO) in 1994 (28 571 subjects aged 11–41 years) and 2002 (31 865 subjects aged 20–71 years)
| Migraine |
MA |
MO |
|||||||
| Rate (%) | 95% CI | n, crude | Rate (%) | 95% CI | n, crude | Rate (%) | 95% CI | n, crude | |
| 1994 | |||||||||
| All subjects | 16.1 | 15.6 to 16.6 | 4593 | 4.8 | 4.5 to 5.0 | 1368 | 11.3 | 10.9 to 11.7 | 3225 |
| Women | 20.5 | 19.8 to 21.3 | 3031 | 6.5 | 6.1 to 6.9 | 963 | 14.0 | 13.4 to 14.6 | 2068 |
| Men | 11.3 | 10.8 to 11.9 | 1562 | 2.9 | 2.7 to 3.2 | 405 | 8.4 | 7.9 to 8.9 | 1157 |
| 2002 | |||||||||
| All subjects | 25.2 | 24.7 to 25.8 | 8044 | 9.7 | 9.3 to 10.0 | 3086 | 15.6 | 15.1 to 16.0 | 4958 |
| Women | 32.4 | 31.6 to 33.3 | 5597 | 13.1 | 12.6 to 13.7 | 2265 | 19.3 | 18.7 to 20.0 | 3332 |
| Men | 16.8 | 16.1 to 17.4 | 2447 | 5.6 | 5.2 to 6.0 | 821 | 11.1 | 10.6 to 11.7 | 1626 |
Figure 2.
(A–C) The age- and sex-specific lifetime prevalence of migraine and its subtypes in 1994.
Figure 3.
(A–C) The age- and sex-specific lifetime prevalence of migraine and its subtypes in 2002.
Change in prevalence
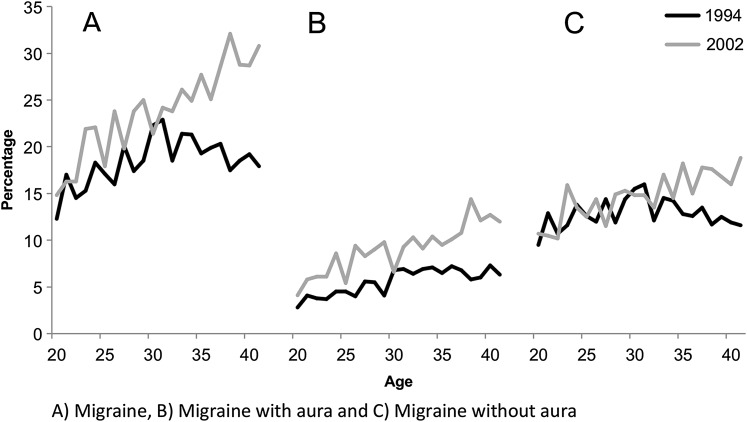
In order to estimate possible changes in prevalence, we compared the subjects aged 20–41 years, which comprised 22 053 persons in the 1994 cohort and 14 810 persons in the 2002 cohort. The 2002 cohort was slightly older than the 1994 cohort (median =32 vs 30, mean =31 vs 30 and 90% percentiles 21–41 vs 21–40). The lifetime prevalence for age 20–41 was increased from 1994 to 2002 (18.5% vs 24.5%) by 32.2% (95% CI 27.0% to 37.3%; p<0.001). The difference was primarily seen in the population older than 32 years (figure 4A–C). The increase was especially evident in MA (5.6% vs 9.4%, p<0.001), but we also found a significant increase in MO as well (13.0% vs 15.1%, p<0.001). The prevalence increased significantly in women from 24.0% to 30.9% and in men from 12.6% to 16.1%. The relative increase was similar for both sexes (27.8% vs 28.8%).
Figure 4.
(A–C) Comparison of lifetime prevalence rates of 1994 with 2002 for subjects aged 20–41 years.
Incidence
Nineteen thousand five hundred and eighty-six subjects had completed both twin surveys with regard to migraine. Sixteen thousand four hundred and forty-two subjects aged 12–41 years did not report having migraine in 1994. Of those, 2318 subjects reported migraine in 2002 resulting in an 8-year period incidence rate of 0.141 corresponding to an average annual incidence rate of migraine of 17.6 per 1000 PYs. The incidence rates of migraine and its subtypes are listed in table 3. We did not find any significant difference in incidence between age groups 20–29 and 30–39 (p=0.0834) nor 30–39 and 40–49 (p=0.0762); however, a significantly higher incidence was found in the group aged 20–29 than 40–49 (p=0.0007). Decreasing incidence rate with age was especially seen in MO subjects. There were 2206 subjects reported having MO in 1994 who had also completed the 2002 survey. The average annual incidence rate of MA in these subjects was 25.8 PYs (95% CI 23.5 to 28.3, n crude =456).
Table 3.
The sex-specific average annual incidence rates per 1000 person-years (PYs) from 1994 to 2002 of migraine, migraine with aura (MA) and migraine without aura (MO) in 16 442 subjects aged 20–49 years
| All subjects |
Women |
Men |
|||||||
| 1000 PYs | 95% CI | n, crude | 1000 PYs | 95% CI | n, crude | 1000 PYs | 95% CI | n, crude | |
| Migraine | 17.6 | 16.9 to 18.4 | 2318 | 23.4 | 22.3 to 24.6 | 1617 | 11.2 | 10.4 to 12.1 | 701 |
| MA | 5.6 | 5.2 to 6.1 | 741 | 8.0 | 7.4 to 8.7 | 553 | 3.0 | 2.6 to 3.5 | 188 |
| MO | 12.0 | 11.4 to 12.6 | 1577 | 15.4 | 14.5 to 16.4 | 1064 | 8.2 | 7.5 to 9.0 | 513 |
Discussion
The present study demonstrated a significant increase of self-reported migraine prevalence in the Danish young adult population from 1994 to 2002. The increase was especially evident in MA and the increase in MO was also significant. The increase was primarily seen in the population older than 32 years.
Migraine lifetime prevalence
The lifetime prevalence has been estimated in several population-based studies with large variation between 11.2% and 27.5% in questionnaire-based studies and between 12% and 19% in interview-based studies in the developed countries.3 The variation seen may be due to difference in methodology. One might wonder why the prevalence of lifetime migraine in 2002 was unexpectedly high in our study compared with the lifetime prevalence in the other developed countries. However, when comparing the prevalence found in other large-scale comparable European population-based questionnaire studies our results were similar; for references, see Stovner and Andree.4 This was true for both men and women. One explanation could be that patients in Europe were more likely to receive a medical diagnosis than for example in the USA.19 Very few studies have estimated the lifetime prevalence of migraine subtypes. A previous Danish study20 showed a higher lifetime prevalence of MA than the one we found in 1994 (6% vs 4.8%). However, the prevalence of MO was lower than ours (8% vs 11.3%). Another study found lower prevalence rates of both MA and MO, 3.3% and 7.1%.21 We expected to see increasing lifetime prevalence with advancing age; however, the prevalence was decreasing after the fifth decade. A decrease was especially seen in MA, whereas the prevalence in MO reached a plateau. This is likely due to recall bias as discussed previously.22 23 MA patients tend to neglect having migraine compared with MO patients because MA attacks are less frequent and less severe.24 That may explain the pronounced difference in MA and MO patients.
Is the migraine prevalence increasing?
We found a 32% increase in the lifetime prevalence of migraine in a period of 8 years. Change in lifetime as well as 1-year prevalence has previously been investigated in replicate studies. A large-scale study investigating subjects aged 12 years and older found that the lifetime prevalence of migraine increased significantly by 16% over a period of 4 years in women (10.1% vs 11.7%, p≤0.01), but a non-significant decrease was seen in men (4.3% vs 3.8%).6 The group of 25–54 years that is more comparable with our study population also showed a significant increase in women and a non-significant increase in men. Our study showed a significant increase in both sexes. The difference seen may be due to different study population or sample size. A Danish study investigating both lifetime and 1-year prevalence of migraine from 1989 to 2001 found no significant changes, as only a tendency towards an increase was observed (14.5% vs 18.4%, difference −3.9, 95% CI −11.5 to 3.8 for the lifetime prevalence; 11.3% vs 15.5%, difference −4.1, 95% CI −11.1 to 2.8 for the 1-year prevalence).8 This increasing trend was also seen for 1-year prevalence in women (15.6% vs 23.5%, p=0.14). However, this study had a small sample size (n=211 and 207) and must be interpreted with caution. A recent large-scale population-based study found a small increase in the 1-year prevalence (12.1% vs 13.2%, p<0.001).9 A marked increase in 6 months prevalence over a period of 28 years (1.9%–5.7%) was found in a study investigating 7-year-old children.25 Other large-scale studies demonstrated no change in migraine prevalence over time.5 7 A true increase in prevalence would be attributed to rising incidence. However, part of the increase may also be due to rising public awareness of migraine or increased medical consultation resulting in an increased rate of physician diagnosis.26 27 We do not know of any approaches to increase awareness of migraine in Denmark. However, an increase in medical consultation has been shown.28 Subjects born in 1953–1982 were invited to participate in both surveys. This means that the group of subjects who did participate in both surveys would have experienced the migraine questions already. It is possible that these subjects became more aware of migraine to the second survey. On balance, our data convincingly show an increase in prevalence, but the size of the increase may not be as high as our finding of 32%. Due to the short time span of 8 years, this must be caused by environmental factors and not by genes. Mutations cannot increase the migraine prevalence so quickly in a general population. Currently, we do not know about any potential environmental factors or its nature or course. Some factors, such as social economic status,5 smoking and alcohol,29 have been suggested based on cross-sectional studies, but to our knowledge, very few longitudinal studies have investigated risk factors for migraine. One cohort study reported that smokers have a higher risk of developing self-reported migraine.30 Apparently, the need of more longitudinal studies is wanted.
Migraine 1-year prevalence
Although our lifetime prevalence was high, the 1-year prevalence was found to match the lower range of the prevalence rates in Europe based on large-scale comparable questionnaire studies (11.6% to 16.3%, 7.5% to 9.5% in men and 15.6% to 25% in women) as well as in interview-based studies.4 Comparing the 1-year migraine prevalence in 2002 with the lifetime prevalence in 2002, we found that more than 50% reporting lifetime migraine did not experience attacks during the last year. This speaks for a favourable course of migraine. Only few studies24 27 31–34 have investigated the 1-year prevalence of migraine subtypes showing a range for MA of 0.6% to 3.7% in men and 3.6% to 10.8% in women and for MO 2% to 7.3% and 7.5% to 11.9%, respectively. Our prevalence estimates were similar to those found previously in Denmark and the UK.24 33 The American Migraine study revealed increasing prevalence in both male and female subjects from age 12 until approximately age 40, after which a decreasing prevalence was noted.35 This is in keeping with our findings (see figure 1A–C).
Incidence
A great variation is found in the literature for the incidence rate of migraine in the adult population (1.4–5.0 per 1000 PYs in men and 2.9–22 per 1000 PYs in women).36–39 Our incidence rate in women is in keeping with previous findings; however, the rate in men is somewhat higher. A previous small-scale study in Denmark found an incidence of 8.1 per 1000 PYs in 2001 in subjects aged 25–64 years.40 We found an annual incidence rate of 17.6 per 1000 PYs for migraine. The difference seen could be due to different methodology or that our population was younger (20–49 years old).
Methodological considerations
It was possible in this study to differentiate between MA and MO because of the use of validated diagnostic questions.18 Furthermore, it was possible to subdivide between men and women and to distinguish between age groups because of the large sample size. However, the present study also has weaknesses. The validation of the two questions used to identify migraine cases showed that self-reported migraine was only correct in 74.5% of cases, and furthermore, approximately 23.8% of the migraine subjects were not identified. Thus, our estimates would tend to be conservative. However, the sensitivity of our questions was higher than the sensitivity of a questionnaire modified according to the criteria of the International Classification of Headache Disorders 2nd edition9; therefore, our questions should be valid as a tool for identifying migraine and determining the prevalence and incidence.
Conclusions
Our most important finding was a substantial increase in the lifetime prevalence of self-reported migraine in Denmark from 1994 to 2002 confirming previous studies. Part of the increase may be due to increased medical consultation resulting in an increased rate of physician diagnosis or awareness due to previous participation in the 1994 survey. It seems pertinent to study the causes of the increase and to implement preventive measures.
Supplementary Material
Acknowledgments
We thank Secretary Jytte Duerlund for her assistance in carrying out the ‘Twin Omnibus 2002’ study. She did not receive compensation for her assistance.
Footnotes
To cite: Le H, Tfelt-Hansen P, Skytthe A, et al. Increase in self-reported migraine prevalence in the Danish adult population: a prospective longitudinal population-based study. BMJ Open 2012;2:e000962. doi:10.1136/bmjopen-2012-000962
Contributors: All authors had full access to all the data (including statistical reports and tables) in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. HL and JO accept full responsibility for this work and act as the guarantors for the study. HL: (1) conception and design and analysis and interpretation of data; (2) drafting the manuscript; (3) final approval of the version to be published. PT-H: (1) conception and design and analysis and interpretation of data; (2) revising the manuscript critically for important intellectual content; (3) final approval of the version to be published. AS: (1) acquisition of data; (2) revising the manuscript critically for important intellectual content; (3) final approval of the version to be published. KOK: (1) conception and design and acquisition of data; (2) revising the manuscript critically for important intellectual content; (3) final approval of the version to be published. JO: (1) conception and design and analysis and interpretation of data; (2) revising the manuscript critically for important intellectual content; (3) final approval of the version to be published.
Funding: The project was funded by the Department of Neurology Research Fund, Glostrup Hospital. The funding bodies had no role in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Competing interests: None.
Ethics approval: This study was a registry study based solely on questionnaires and did not require any approval from the ethics committee according to national regulations.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Leonardi M, Steiner TJ, Scher AT, et al. The global burden of migraine: measuring disability in headache disorders with WHO's Classification of Functioning, Disability and Health (ICF). J Headache Pain 2005;6:429–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gustavsson A, Svensson M, Jacobi F, et al. Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol 2011;21:718–79 [DOI] [PubMed] [Google Scholar]
- 3.Stovner L, Hagen K, Jensen R, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia 2007;27:193–210 [DOI] [PubMed] [Google Scholar]
- 4.Stovner LJ, Andree C. Prevalence of headache in Europe: a review for the Eurolight project. J Headache Pain 2010;11:289–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lipton RB, Stewart WF, Diamond S, et al. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache 2001;41:646–57 [DOI] [PubMed] [Google Scholar]
- 6.Gilmour H, Wilkins K. Migraine. Health Rep 2001;12:23–40 [PubMed] [Google Scholar]
- 7.Henry P, Auray JP, Gaudin AF, et al. Prevalence and clinical characteristics of migraine in France. Neurology 2002;59:232–7 [DOI] [PubMed] [Google Scholar]
- 8.Lyngberg AC, Rasmussen BK, Jorgensen T, et al. Has the prevalence of migraine and tension-type headache changed over a 12-year period? A Danish population survey. Eur J Epidemiol 2005;20:243–9 [DOI] [PubMed] [Google Scholar]
- 9.Linde M, Stovner LJ, Zwart JA, et al. Time trends in the prevalence of headache disorders. The Nord-Trondelag Health Studies (HUNT 2 and HUNT 3). Cephalalgia 2011;31:585–96 [DOI] [PubMed] [Google Scholar]
- 10.Skytthe A, Kyvik K, Holm NV, et al. The Danish Twin Registry: 127 birth cohorts of twins. Twin Res 2002;5:352–7 [DOI] [PubMed] [Google Scholar]
- 11.Skytthe A, Kyvik K, Bathum L, et al. The Danish Twin Registry in the new millennium. Twin Res Hum Genet 2006;9:763–71 [DOI] [PubMed] [Google Scholar]
- 12.Ulrich V, Gervil M, Fenger K, et al. The prevalence and characteristics of migraine in twins from the general population. Headache 1999;39:173–80 [DOI] [PubMed] [Google Scholar]
- 13.Kyvik KO, Christensen K, Skytthe A, et al. The Danish Twin Register. Dan Med Bull 1996;43:467–70 [PubMed] [Google Scholar]
- 14.Kyvik KO, Green A, Beck-Nielsen H. The new Danish Twin Register: establishment and analysis of twinning rates. Int J Epidemiol 1995;24:589–96 [DOI] [PubMed] [Google Scholar]
- 15.Christensen K, Vaupel JW, Holm NV, et al. Mortality among twins after age 6: fetal origins hypothesis versus twin method. BMJ 1995;310:432–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kyvik KO, Green A, Beck-Nielsen H. Concordance rates of insulin dependent diabetes mellitus: a population based study of young Danish twins. BMJ 1995;311:913–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Skadhauge LR, Christensen K, Kyvik KO, et al. Genetic and environmental influence on asthma: a population-based study of 11,688 Danish twin pairs. Eur Respir J 1999;13:8–14 [DOI] [PubMed] [Google Scholar]
- 18.Le H, Tfelt-Hansen P, Russell MB, et al. Co-morbidity of migraine with somatic disease in a large population-based study. Cephalalgia 2011;31:43–64 [DOI] [PubMed] [Google Scholar]
- 19.Lipton RB, Scher AI, Steiner TJ, et al. Patterns of health care utilization for migraine in England and in the United States. Neurology 2003;60:441–8 [DOI] [PubMed] [Google Scholar]
- 20.Russell MB, Rasmussen BK, Thorvaldsen P, et al. Prevalence and sex-ratio of the subtypes of migraine. Int J Epidemiol 1995;24:612–18 [DOI] [PubMed] [Google Scholar]
- 21.Svensson DA, Ekbom K, Larsson B, et al. Lifetime prevalence and characteristics of recurrent primary headaches in a population-based sample of Swedish twins. Headache 2002;42:754–65 [DOI] [PubMed] [Google Scholar]
- 22.Bille B. A 40-year follow-up of school children with migraine. Cephalalgia 1997;17:488–91 [DOI] [PubMed] [Google Scholar]
- 23.Rasmussen BK. Epidemiology of headache. Cephalalgia 1995;15:45–68 [DOI] [PubMed] [Google Scholar]
- 24.Rasmussen BK, Olesen J. Migraine with aura and migraine without aura: an epidemiological study. Cephalalgia 1992;12:221–8 [DOI] [PubMed] [Google Scholar]
- 25.Sillanpaa M, Anttila P. Increasing prevalence of headache in 7-year-old schoolchildren. Headache 1996;36:466–70 [DOI] [PubMed] [Google Scholar]
- 26.Lipton RB, Stewart WF, Simon D. Medical consultation for migraine: results from the American Migraine Study. Headache 1998;38:87–96 [DOI] [PubMed] [Google Scholar]
- 27.Lipton RB, Scher AI, Kolodner K, et al. Migraine in the United States: epidemiology and patterns of health care use. Neurology 2002;58:885–94 [DOI] [PubMed] [Google Scholar]
- 28.Lyngberg AC, Rasmussen BK, Jorgensen T, et al. Secular changes in health care utilization and work absence for migraine and tension-type headache: a population based study. Eur J Epidemiol 2005;20:1007–14 [DOI] [PubMed] [Google Scholar]
- 29.Aamodt AH, Stovner LJ, Hagen K, et al. Headache prevalence related to smoking and alcohol use. The Head-HUNT Study. Eur J Neurol 2006;13:1233–8 [DOI] [PubMed] [Google Scholar]
- 30.Hozawa A, Houston T, Steffes MW, et al. The association of cigarette smoking with self-reported disease before middle age: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Prev Med 2006;42:193–9 [DOI] [PubMed] [Google Scholar]
- 31.Lampl C, Buzath A, Baumhackl U, et al. One-year prevalence of migraine in Austria: a nation-wide survey. Cephalalgia 2003;23:280–6 [DOI] [PubMed] [Google Scholar]
- 32.Sakai F, Igarashi H. Prevalence of migraine in Japan: a nationwide survey. Cephalalgia 1997;17:15–22 [DOI] [PubMed] [Google Scholar]
- 33.Steiner TJ, Scher AI, Stewart WF, et al. The prevalence and disability burden of adult migraine in England and their relationships to age, gender and ethnicity. Cephalalgia 2003;23:519–27 [DOI] [PubMed] [Google Scholar]
- 34.Zivadinov R, Willheim K, Jurjevic A, et al. Prevalence of migraine in Croatia: a population-based survey. Headache 2001;41:805–12 [DOI] [PubMed] [Google Scholar]
- 35.Stewart WF, Lipton RB, Celentano DD, et al. Prevalence of migraine headache in the United States. Relation to age, income, race, and other sociodemographic factors. JAMA 1992;267:64–9 [PubMed] [Google Scholar]
- 36.Becker C, Brobert GP, Almqvist PM, et al. Migraine incidence, comorbidity and health resource utilization in the UK. Cephalalgia 2008;28:57–64 [DOI] [PubMed] [Google Scholar]
- 37.Breslau N, Davis GC, Andreski P. Migraine, psychiatric disorders, and suicide attempts: an epidemiologic study of young adults. Psychiatry Res 1991;37:11–23 [DOI] [PubMed] [Google Scholar]
- 38.Stang PE, Yanagihara PA, Swanson JW, et al. Incidence of migraine headache: a population-based study in Olmsted County, Minnesota. Neurology 1992;42:1657–62 [DOI] [PubMed] [Google Scholar]
- 39.Rozen TD, Swanson JW, Stang PE, et al. Increasing incidence of medically recognized migraine headache in a United States population. Neurology 1999;53:1468–73 [DOI] [PubMed] [Google Scholar]
- 40.Lyngberg AC, Rasmussen BK, Jorgensen T, et al. Incidence of primary headache: a Danish epidemiologic follow-up study. Am J Epidemiol 2005;161:1066–73 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.