Abstract
Clinical pharmacology and therapeutics is the academic discipline that informs rational prescribing of medicines. There is accumulating evidence that a significant minority of prescriptions in the UK National Health Service contain errors. This comes at a time when the approach to and success of undergraduate education in this area has been called into question. Various stakeholders are now in agreement that this challenging area of undergraduate education needs to be strengthened. The principles that should form the basis of future educational strategy include greater visibility of clinical pharmacology and therapeutics in the curriculum, clear learning outcomes that are consistent with national guidance, strong and enthusiastic leadership, a student formulary, opportunities to practice prescribing, a robust assessment of prescribing competencies and external quality control. Important new developments in the UK are Prescribe, a repository of e-learning materials to support education in clinical pharmacology and prescribing, and the Prescribing Skills Assessment, a national online assessment designed to allow medical students to demonstrate that they have achieved the core competencies required to begin postgraduate training.
Background
The mission of clinical pharmacology and therapeutics (CPT) is ‘to improve the care of patients by promoting safe and effective use of medicines and to evaluate and introduce new therapies’[1]. Education of the prescribers who direct the use of medicines in healthcare for the benefit of public health, at both undergraduate and postgraduate levels, is an important part of fulfilling that mission. Indeed, the principles of clinical pharmacology are the basis of good patient-centred prescribing.
Many would argue that teaching medical students to prescribe medicines is currently the greatest challenge in modern undergraduate education. Prescribing is a complex task that requires diagnostic skills, knowledge of medicines, communication skills, an understanding of the principles of clinical pharmacology, appreciation of risk and uncertainty, and critical judgement. The challenge would be lessened if graduates were provided with a carefully supervised and gradual introduction to practice. However, the reality is that newly qualified doctors find themselves thrust into a busy clinical environment, in which they are often required to write many more prescriptions on their first day than they have practised writing during their whole undergraduate careers, and usually with minimal supervision. They will be regularly called on to write prescriptions for drugs about which they know little and have had little experience. Furthermore, the demands on each new cohort are ever increasing, because of several well-documented trends, including increasing polypharmacy, often appropriate, more complicated regimens, increasingly vulnerable patients, higher patient throughput and shorter training hours.
Clinical pharmacology and therapeutics emerged as a new discipline in the 1950s and 1960s as the rate of drug development increased, and many schools incorporated it into their curriculum as a discrete course. At the beginning of the 1990s, it was still common for medical schools to provide courses in both basic pharmacology and CPT, and for each to be individually assessed. However, in response to concerns that students were overburdened with scientific facts and were being taught in rigidly traditional, discipline-based courses, the General Medical Council signalled a dramatic change with the publication of Tomorrow's Doctors in 1993 [2]. This promoted a ‘reduction in factual burden’, integration of the curriculum ‘both vertically and horizontally’, learning based on body systems, and ‘avoided all reference to traditional subjects and disciplines’ . . . urging the advantages of ‘interdisciplinarity’. These changes undoubtedly weakened CPT, a traditional discipline that is factually rich and not organ based. Identifiable courses and assessments in pharmacology and CPT disappeared in many schools, along with their associated assessments, with the consequent loss of the teachers and departments who had delivered them [3]. Research assessment exercises, which have concentrated increasingly on molecular science at the expense of clinical science [4], have exacerbated the problem. Medical students now have little exposure to CPT or clinical pharmacologists. This lack of specialists in a discipline dedicated to fostering safe and rational use of medicines has even induced some schools to call on pharmaceutical companies for teaching support [5].
These changes prompted concerns, which were voiced initially by clinical pharmacologists [6], and which have been echoed more recently by others, including students themselves [7]. While those who expressed concern would have to concede that there had never been a ‘golden age’ for CPT education to which we might return, the new mantra of Tomorrow's Doctors made it harder to put in place measures that would address the very real prescribing problems that were emerging in the National Health Service (NHS).
Drivers for change
Prescribing is now recognized by those responsible for managing health services as a ‘high-risk’ area of practice and a major clinical governance issue. A study from the North of England suggested that around one in 10 prescriptions written by recent graduates contains an error [8], and this has been corroborated by data from Scotland [9]. The service is now increasingly looking to medical schools to ensure that their graduates have the necessary skills and knowledge when they enter the workforce. Several studies have shown that a lack of training and unfamiliarity with drugs among junior prescribers is an important factor in serious medication incidents [10]. It is also well documented that new graduates rate prescribing as the most challenging aspect of their jobs and the one for which they are least prepared [11], [12]. Importantly, educational interventions such as the ‘WHO Good Prescribing Guide’ have been shown to improve prescribing performance [13], [14].
With concerns mounting about the preparedness of new graduates to prescribe in the NHS, the General Medical Council and the Medical Schools Council set up a Safe Prescribing Working Group in 2007. This also contained representatives from other key stakeholders, including the British Pharmacological Society (BPS), Postgraduate Deans, NHS employers, the National Prescribing Centre and the British Medical Association. The group formed a consensus on five important points, including the outcomes of undergraduate medical education (Table 1), the need for an national e-learning strategy to support medical students in achieving those outcomes, the need for assessments that would demonstrate that they had been achieved, the need to develop national prescribing documentation and the need for all students to have access to the British National Formulary[15]. The competency outcomes were incorporated into the latest version of Tomorrow's Doctors, along with a welcome increase in emphasis on safe practices in relation to medicines [16]. A subsequent survey suggested that many medical schools will need to make significant revisions to their approach to teaching and learning in this area if they are to meet the new requirements [17]. There is now a shortage of clinical pharmacologists to support this process [3].
Table 1.
The competency outcomes in relation to prescribing to be expected of all graduates of UK medical schools as defined by the Safe Prescribing Working Group convened by the General Medical Council and Medical Schools Council in 2007 [15]
| All new medical graduates should be able to: |
| • Establish an accurate drug history |
| • Plan appropriate therapy for common indications |
| • Write a safe and legal prescription |
| • Appraise critically the prescribing of others |
| • Calculate appropriate doses |
| • Provide patients with appropriate information about their medicines |
| • Access reliable information about medicines |
| • Detect and report adverse drug reactions |
Basic principles for undergraduate education
The current challenge for medical schools is to deliver graduates who meet these expectations and are capable of responding to the complexities of modern pharmacotherapy, often in curricula without clinical pharmacology modules or assessments. The BPS published a detailed statement on the content, delivery and assessment of clinical pharmacology and prescribing in 2003 [18], which informed much of the direction of the recent guidance. These recommendations took account of the marked diversity that exists in medical curricula. These range from a traditional structure, with preclinical phases consisting of sciences taught as disciplines, often by lecture, through to those that are based entirely on problem-based learning in small groups. Education for safe prescribing can thrive in all settings but should follow some important principles, as outlined below.
Organization
Clinical pharmacology should be identified as an important vertical theme that is visible throughout the medical curriculum, integrating with and identifiable within relevant horizontal modules and culminating with an emphasis on practical prescribing. Medical curricula are now very varied, and it is impossible to be didactic about the ways in which this theme is delivered. Ensuring visibility is easy within more traditional arrangements, in which horizontal modules in pharmacology and clinical pharmacology survive. The delivery is more challenging when discipline-protected time has been removed to produce a truly integrated curriculum, often with an emphasis on problem-based learning. In these circumstances, CPT learning objectives must compete simultaneously with many others, usually dispersed across many different modules and through several years of the course. This poses practical difficulties for those leading the theme, who must co-ordinate learning opportunities across many modules over which they have limited influence. Nevertheless, the importance of CPT should be emphasized in all clinical modules in which there are continuous opportunities for observing and critically appraising patients' drug charts, for seeing the beneficial and adverse effects of drugs and for practising relevant skills, including practical prescribing, dosage calculations, drug preparation and administration, and searching for good-quality information to inform prescribing decisions. Students should also be expected to observe the process of prescribing from the perspective of other healthcare professionals, such as nurses and pharmacists, for example by participating in a ward drug round.
Learning outcomes
Students should be made aware of the core learning outcomes, including knowledge of and understanding about medicines, skills related to prescribing and attitudes towards drug therapy. Headline areas can be found in the current version of Tomorrow's Doctors[16], but each school must develop more detailed outcomes, ideally based on those identified by the BPS [18], [19].
Leadership
A key factor in the successful delivery of learning outcomes, particularly in an integrated course, will be strong and enthusiastic leadership. All medical schools should be able to identify an individual who will oversee delivery and ensure that the generic principles of safe and effective use of medicines are highlighted throughout the course. That individual does not have to be a clinical pharmacologist, but should champion the importance of prescribing as a clinical skill and ensure that the relevant opportunities are available to allow the relevant learning outcomes to be met. Many individuals who have been trained in departments of clinical pharmacology specialize finally in other disciplines [20], and their expertise could advantageously be harnessed.
Student formulary
Medical students are often overwhelmed by the large number of drugs that they hear about and encounter during their training. The factual burden imposed should be eased by prioritizing learning around a core list of around 100 commonly used drugs (a student formulary) [21]. A limited formulary offers students a learning target that is realistic and attainable. The list should comprise drugs that are commonly used in treating common illnesses, that are representative of important drug classes and that a newly qualified doctor might be expected to initiate or prescribe under the direction of a senior doctor. For each drug or drug class, students might be expected to have an understanding of the mechanism of action, to recognize the appropriate indications, to know the appropriate route of administration, the important contraindications and potential adverse reactions and interactions, to know how to monitor the drug's beneficial and harmful effects and to be able to explain the salient features of all the above to the patient. Although students should not be expected to know specific drug doses as part of core knowledge, it might be reasonable to expect them to identify dangerously inappropriate doses of very commonly used drugs. The list of core drugs can be organized by organ system and set alongside the common therapeutic circumstances in which they are used. This arrangement emphasizes the suitability of a problem-based approach to the development of learning about CPT and the ease with which CPT can be integrated in a system-based curriculum.
Prescribing training
It is important that the CPT theme culminates in a strong emphasis on prescribing. Too many students reach the end of their studies without having been faced with the challenge of writing prescriptions and weighing up the hazards and benefits of medicines in the presence of potential contraindications, coexistent morbidities or interacting drugs, and of selecting appropriate dosage regimens. The opportunities for students to ‘pre-prescribe’ under supervision, to gain experience from junior doctors (‘near-peer’ education) [22] or to undertake simulated prescribing exercises should be considered vital developments that might help to move beyond the current ‘in at the deep end’ experience. The diet of clinical specialty modules should provide greater experience of prescribing than it currently appears to do. Students should be drawn to their future responsibilities for completing and reviewing prescription charts at every patient's bedside.
Learning style
The successful delivery of learning in CPT will involve a variety of learning styles, including lectures and problem-based tutorials, depending on local educational preferences, but the content should, as far as possible, be centred on inquisitive rather than passive learning. There should be an appropriate balance of different forms of tuition, including teaching in large groups, teaching in small groups, practical classes and opportunities for self-directed learning (e.g. e-Learning). The core curriculum in CPT is well suited to take advantage of the increasingly popular style of problem-based learning. Most prescribing episodes are a direct attempt to solve a clinical problem, and they require the appropriate knowledge, skills and attitudes outlined in the BPS curriculum [18]. Several schools have developed a series of ‘therapeutics cases’, which offer students a case vignette and pose direct problems relating to prescribing and therapeutics. These may be undertaken in live time, even within relatively large groups, or they may be researched and discussed at intervals over several weeks. Other approaches to CPT involve writing case reports containing discussions about therapeutic aspects (e.g. portfolio cases), discussing prescribing decisions with patients as part of communicating skills, critique of clinical trials involving medicines, appraising claims for new medicines and searching for information about medicines. In schools that lack a clear CPT presence, learning opportunities are devolved to many teachers across the course, often within organ-based specialties. Those teachers should be encouraged to emphasize the principles of rational prescribing and to remind students about the effects of medicinal products beyond individual organ systems. Simply providing a link between medicines and clinical conditions is insufficient to develop an appreciation of the complex considerations that surround the decision to initiate a prescription. Clinical pharmacists, who are usually available in greater numbers than CPT specialists, also have an important role to play in reinforcing learning during clinical attachments.
e-Learning
Many medical schools have now embraced Web-based opportunities to deliver learning and self-assessment in a virtual learning environment. This can be a very powerful tool for drawing the attention of students to the theme of clinical pharmacology and prescribing, especially where there is scarcity of relevant specialists and poor visibility. Online resources can provide attractive active learning experiences that are constantly accessible. These may aid understanding of key principles, support a student formulary [23], offer skills practice [24] and provide case-based therapeutic problems [25]. As the change from paper to electronic prescribing spreads worldwide, aided by advances in virtual reality environments, this approach will be able to provide increasingly realistic simulation of real-world prescribing.
Assessment
There should be an identifiable and robust assessment that tests whether the knowledge and skills outcomes related to CPT and prescribing have been achieved. Although this might form part of an integrated assessment, it should never be possible to compensate for a poor performance in prescribing by a good performance in other items. The assessment strategy will be critical in emphasizing the importance of CPT in the course and ensuring that graduates are fit to practise. It is important too that assessments should not simply be knowledge based but should also test the acquisition of practical skills, including writing a prescription, offering information to a patient about a drug and spotting potentially dangerous prescriptions. Students should also be provided with formative assessments and chances for self-assessment at regular intervals during the medical course.
Quality assurance
All medical schools should have some form of external quality assurance, to ensure that the learning opportunities and assessments they provide are suitable to develop graduates who have the necessary competencies and to identify any who do not. The appointment of external examiners with relevant expertise and interests might also help to ensure that appropriate standards are being met.
Current developments
Two important approaches in CPT education are currently being developed by the BPS and are intended to support medical schools in the task of delivering prescribers ready to meet the challenge of the modern NHS, namely the e-learning repository Prescribe and a prescribing skills assessment.
Prescribe, a repository of e-learning materials, is being designed to help medical students to develop a firm grounding in the principles of clinical pharmacology and to meet the outcomes identified by Tomorrow's Doctors. Prescribe will contain interactive learning sessions in four sections, covering the principles of clinical pharmacology, common drugs, common therapeutic problems and skills relating to prescribing (Figure 1). It will also include a student formulary and opportunities for practising key skills, such as prescribing and dosage calculations, using online simulators. There will also be self-assessment exercises, a library of important publications, a glossary and links to other resources. The materials are intended to complement existing teaching initiatives and will be available free of charge to medical students registered with UK universities.
Figure 1.
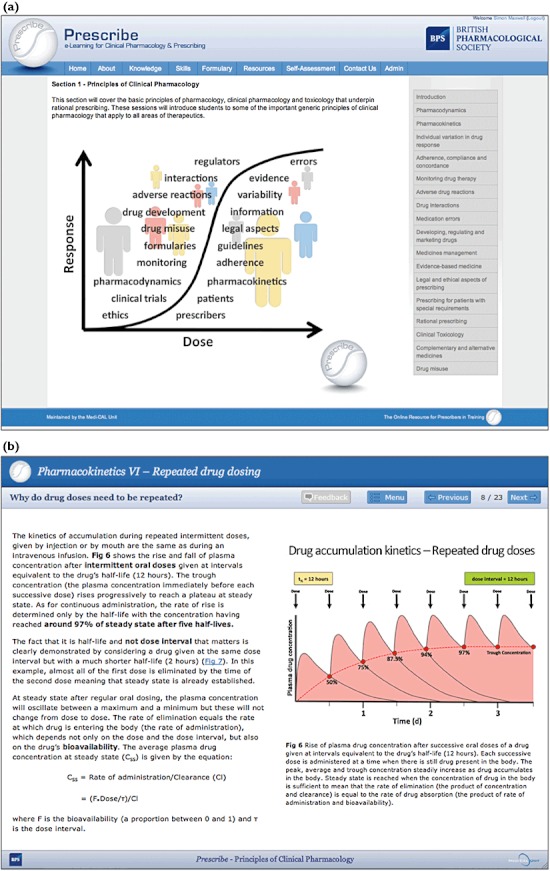
The Prescribe online learning project. (a) The modules available in the clinical pharmacology section. (b) A learning session in the pharmacokinetics module
The Prescribing Skills Assessment is being developed in collaboration with the Medical Schools Council and will be a summative assessment of knowledge, judgement and skills related to prescribing medicines in the NHS. It is intended primarily for medical students at or near the end of their training and is based on the competencies identified in Tomorrow's Doctors. These include writing new prescriptions, reviewing existing prescriptions, calculating drug dosages, identifying and avoiding both adverse drug reactions and medication errors, and amending prescribing to suit individual patient circumstances (Figure 2). The development of the Prescribing Skills Assessment is being driven by a cross-sector steering group, with representatives from a broad range of stakeholders, including medical students. The Prescribing Skills Assessment will be delivered online and is intended to be taken in the final few months of the medical course, with opportunities for retakes for students who fail. There will be further pilot work during 2011–2012, and it is expected that it will be implemented during the following academic year.
Figure 2.
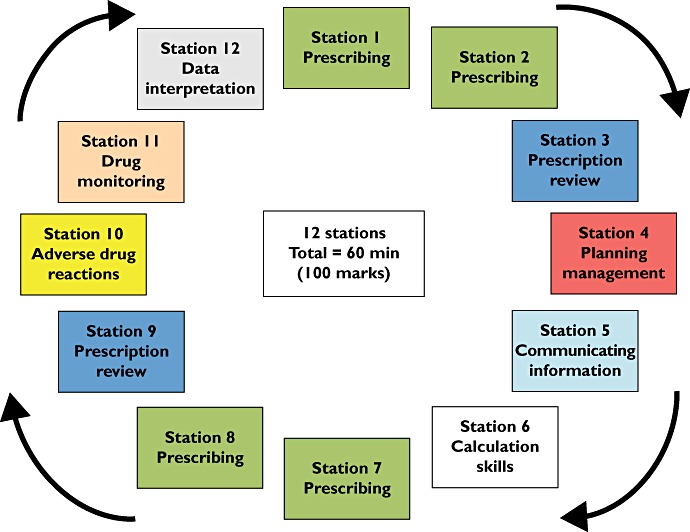
The twelve stations of the Prescribing Skills Assessment
A vision for the future
What should be the vision for undergraduate education in the next 10 years? The potential implementation of a national assessment is to be welcomed as an important measure that should increase the emphasis on the safe use of medicines in medical education. It should foster improvements in the standards of education in all institutions, based on the principles set out above, and renew awareness of the contribution that clinical pharmacologists can make to this process, supporting the re-emergence of CPT as an important academic discipline and signposting it as a potential career for graduates. The development of a reliable test of competency, if it can be validated against real-world practice, might also be the basis of better research into education and other influences on prescribing.
It is imperative that the medical students be provided with more opportunities to practise their skills during training. A greater emphasis on workplace experiential learning and the emergence of simulated environments should help to achieve this. The latter might be part of a larger e-learning strategy that supports (but will not replace) strong local leadership. Such a strategy should help to create a seamless move from the undergraduate to the postgraduate environment, where the development of prescribing can continue.
Competing Interests
There are no competing interests to declare.
REFERENCES
- 1.Royal College of Physicians. Clinical Pharmacology and Therapeutics in a Changing World. Report of a Working Party. London: RCP; 1999. [PMC free article] [PubMed] [Google Scholar]
- 2.General Medical Council. Tomorrow's Doctors. London: General Medical Council; 1993. [Google Scholar]
- 3.Maxwell SR, Webb DJ. Clinical pharmacology – too young to die? Lancet. 2006;367:799–800. doi: 10.1016/S0140-6736(06)68316-5. [DOI] [PubMed] [Google Scholar]
- 4.Rothwell PM. Medical academia is failing patients and clinicians: the neglect of basic observational clinical research. BMJ. 2006;332:863–4. doi: 10.1136/bmj.332.7546.863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hahn J, Hargreaves R, Hinde A, Huggins JP, Cohen J, Gillen D. An academia–industry partnership in health care. Lancet. 2009;373:1504–5. doi: 10.1016/S0140-6736(09)60836-9. [DOI] [PubMed] [Google Scholar]
- 6.Aronson JK, Henderson G, Webb DJ, Rawlins MD. A prescription for better prescribing. BMJ. 2006;333:459–60. doi: 10.1136/bmj.38946.491829.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heaton A, Webb DJ, Maxwell SRJ. Undergraduate preparation for prescribing: the views of 2413 UK medical students and recent graduates. Br J Clin Pharmacol. 2008;66:128–34. doi: 10.1111/j.1365-2125.2008.03197.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dornan T, Ashcroft AD, Heathfield H, Lewis P, Miles J, Taylor D, Tully M, Was V. An in Depth Investigation into Causes of Prescribing Errors by Foundation Trainees in Relation to Their Medical Education – EQUIP Study. London: General Medical Council; 2009. Available at http://www.gmc-uk.org/FINAL_Report_prevalence_and_causes_of_prescribing_errors.pdf_28935150.pdf (last accessed 15 March 2012) [Google Scholar]
- 9.Ryan C, Davey P, Francis J, Johnston M, Ker J, Lee AJ, MacLeod MJ, Maxwell S, McKay G, McLay J, Ross S, Webb D, Bond C. The prevalence of prescribing errors amongst junior doctors in Scotland. Basic Clin Pharmacol Toxicol. 2011;109(Suppl. 1):35. [Google Scholar]
- 10.Dean B, Schachter M, Vincent C, Barber N. Causes of prescribing errors in hospital inpatients: a prospective study. Lancet. 2002;359:1373–8. doi: 10.1016/S0140-6736(02)08350-2. [DOI] [PubMed] [Google Scholar]
- 11.Illing J, Morrow G, Kergon C, Burford B, Spencer J, Peile E, Davies C, Baldauf B, Allen M, Johnson N, Morrison J, Donaldson M, Whitelaw M, Field M. How prepared are medical graduates to begin practice? A comparison of three diverse UK medical schools. Final summary and conclusions for the GMC Education Committee, 15 December 2008. Available at http://www.gmc-uk.org/FINAL_How_prepared_are_medical_graduates_to_begin_practice_September_08.pdf_29697834.pdf (last accessed 8 July 2011)
- 12.Skills for Health. Junior Doctors in the NHS: Preparing Medical Students for Employment and Post-graduate Training. 2009.
- 13.Ross S, Loke Y. Do educational interventions improve prescribing by medical students and junior doctors? A systematic review. Br J Clin Pharmacol. 2009;67:662–70. doi: 10.1111/j.1365-2125.2009.03395.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Vries TP, Henning RH, Hogerzeil HV, Bapna JS, Bero L, Kafle KK, Mabadeje A, Santoso B, Smith AJ. Impact of a short course in pharmacotherapy for undergraduate medical students: an international randomised controlled study. Lancet. 1995;346:1454–7. doi: 10.1016/s0140-6736(95)92472-8. [DOI] [PubMed] [Google Scholar]
- 15.Medical Schools Council. Safe Prescribing Working Group. Outcomes of the Medical Schools Council Safe Prescribing Working Group. Available at http://www.medschools.ac.uk/AboutUs/Projects/Documents/Outcomes%20of%20the%20Medical%20Schools%20Council%20Safe%20Prescribing%20Working%20Group.pdf (last accessed 17 June 2011)
- 16.General Medical Council. Tomorrow's Doctors. 2009. Available at http://www.gmc-uk.org/education/undergraduate/tomorrows_doctors_2009.asp (last accessed 17 June 2011)
- 17.O'Shaughnessy L, Haq I, Maxwell S, Llewelyn M. Teaching of clinical pharmacology and therapeutics in UK medical schools: current status in 2009. Br J Clin Pharmacol. 2010;70:143–8. doi: 10.1111/j.1365-2125.2010.03665.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maxwell S, Walley T. Teaching safe and effective prescribing in UK medical schools: a core curriculum for tomorrow's doctors. Br J Clin Pharmacol. 2003;55:496–503. doi: 10.1046/j.1365-2125.2003.01878.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ross S, Maxwell S. Prescribing and the core curriculum for tomorrow's doctors: BPS curriculum in clinical pharmacology and prescribing for medical students. Br J Clin Pharmacol. 2012 doi: 10.1111/j.1365-2125.2012.04186.x. doi: 10.1111/j.1365-2125.2012.04186.x. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aronson JK. What do clinical pharmacologists do? A questionnaire survey of senior UK clinical pharmacologists. Br J Clin Pharmacol. 2012;73:161–9. doi: 10.1111/j.1365-2125.2011.04079.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baker E, Roberts AP, Wilde K, Walton H, Suri S, Rull G, Webb A. Development of a core drug list towards improving prescribing education and reducing errors in the UK. Br J Clin Pharmacol. 2011;71:190–8. doi: 10.1111/j.1365-2125.2010.03823.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rodrigues J, Sengupta A, Mitchell A, Kane C, Kane C, Maxwell SRJ, Cameron H, Ross M, Ford M. The South-East Scotland Foundation doctor teaching programme? Is near-peer teaching feasible, efficacious and sustainable on a regional scale? Med Teach. 2009;31:e51–7. doi: 10.1080/01421590802520915. [DOI] [PubMed] [Google Scholar]
- 23.Maxwell SRJ, McQueen DS, Ellaway R. eDrug: a dynamic interactive electronic drug formulary for medical students. Br J Clin Pharmacol. 2006;62:673–81. doi: 10.1111/j.1365-2125.2006.02777.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McQueen DS, Begg M, Maxwell SRJ. eDrugCalc: an online self-assessment package to enhance medical students' drug dose calculation skills. Br J Clin Pharmacol. 2010;70:492–9. doi: 10.1111/j.1365-2125.2010.03609.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith A, Tasioulas T, Cockayne N, Misan G, Walker G, Quick G. Construction and evaluation of a web-based interactive prescribing curriculum for senior medical students. Br J Clin Pharmacol. 2006;62:653–9. doi: 10.1111/j.1365-2125.2006.02651.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


