Abstract
Data from the longitudinal West of Scotland Twenty-07 Study: Health in the Community was used to examine whether, over a 20 year period, the self-reported health of people living in deprived areas became poorer faster compared to those living in more affluent areas. Three cohorts (born in the early 1930s, 1950s and 1970s) are included, covering 60 years of the life span. Using multilevel growth curve models, a 40% probability of reporting poor health was predicted among residents of more deprived areas at an earlier age (66) compared to those living in more affluent areas (83). Wider area differences were seen for men than for women. Our findings indicate that attempts to reduce area differences in health should start young but also continue throughout the lifespan.
Keywords: Area deprivation, Neighbourhood, Self-reported health, Longitudinal study, Health trajectories
Highlights
► Longitudinal data used to examine changes in self-reported health over a 20 year period. ► Health of people in poorer areas deteriorated faster than those in more affluent areas. ► 16 year gap between richer and poorer areas in odds of reporting poor health. ► Wider area differences were seen for men than for women.
1. Introduction
A number of studies have shown that living in a more deprived area (variously defined) is associated with poorer health, controlling for individual characteristics such as age, sex and socio-economic status (Pickett and Pearl, 2001; Riva et al., 2007). This has been found for total and coronary heart disease (CHD) mortality (DiezRoux et al., 1997), CHD prevalence and risk factors (Davey Smith et al., 1998) morbidity (Jones and Duncan, 1995; White et al., 2011) mental health and functioning (Beard et al., 2009; Kim 2008; Walters et al., 2004), and health behaviours such as diet, physical activity, smoking and alcohol consumption (Amuzu et al., 2009; Ecob and Macintyre, 2000; Ellaway and Macintyre, 1996). However, most studies to date have been of cross sectional design, which are unable to rule out self-selection (the possibility that people will be selected or select themselves into residential areas on the basis of their health or individual characteristics, which are themselves related to health (Plantinga and Bernell, 2007b, Plantinga and Bernell, 2007a)) and correspondingly limited capacity to explore the plausible causal pathways through which area level exposures might influence health (Macintyre et al., 2002) . Moreover, of the limited number of longitudinal studies, which have been undertaken, most have examined individual and area level exposures at one point in time in relation to health or behavioural outcomes by a single point in time several years later (Giskes et al., 2006; Haan et al., 1987; Pollack et al., 2005, Stafford et al., 2008; Yen and Kaplan, 1998,1999); exceptions include studies of trajectories in Body Mass Index (Ruel et al., 2010; Stafford et al., 2010)). Examining trajectories in health is important for improving our understanding of life course influences on health, as is determining at what age neighbourhood differences are more or less observable (Ahluwalia et al., 2007).
A number of mechanisms through which area of residence may influence health (including major causes of death such as cardiovascular disease (Chaix, 2009; Daniel et al., 2008)), over and above individual characteristics have been suggested. Mechanisms include the hypothesis of differential ‘weathering’ (Bird et al., 2010; Geronimus et al., 2006), which suggests that earlier health deterioration is a consequence of the cumulative impact of repeated experience of social or economic adversity and political marginalisation, and is similar to the ‘more miles on the clock’ metaphor used to explain the earlier health disadvantage experienced by residents of Glasgow compared to residents of Edinburgh, Scotland (Watt and Ecob, 1992; Watt, 1993).
The aim of this paper is to investigate whether the self-reported health of people living in deprived areas becomes poorer over time faster than among residents living in more affluent areas, and to estimate at what age any differences in self-reported health emerge. We also explore whether there are any gender differences in trajectories or age effects, since some studies have found differences between men and women in the magnitude of associations between individual health and experiences of neighbourhood conditions (Chuang and Chuang, 2008; Ellaway and Macintyre, 2001,2009; Kavanagh et al., 2006, Molinari, 1998; Naimi et al., 2009; Parkes and Kearns, 2006; Poortinga et al., 2008; Stafford et al., 2005). To examine these questions we draw upon the ‘West of Scotland Twenty-07 Study’ (Benzeval et al., 2008), which is well placed to address this issue, being sampled from a well-characterised geographic region and using three age cohorts, who have been followed for 20 years thereby encompassing 60 years of the lifespan.
2. Data
The Twenty-07 Study has been following people in three age cohorts—born in the early 1930s, 1950s, and 1970s—for 20 years, sampled from the Central Clydeside Conurbation, West of Scotland (Benzeval et al., 2008). Baseline interviews (n=4510) were carried out in 1987/1988 when respondents were aged approximately 15, 35 and 55, and there have been four follow-ups (1990/1992; 1995/1997; 2000/2004; 2007/2008). At the most recent wave respondents were aged approximately 35, 55 and 75. Respondents who participated at baseline have been shown to be representative of the general population of the sampled area (Der, 1998). Ethics approval was gained for each wave from appropriate NHS and/or University of Glasgow Research Ethics Committees.
3. Measures
The self-assessed health question asked was: over the last 12 months how would you say that your health on the whole has been…? excellent, good, fair, poor. This has been modelled as a binary outcome (0=‘excellent/good’, 1=‘fair/poor’; with ‘fair/poor’ health hereafter referred to as poor health). Self-assessed health has been shown to be related to specific and all cause mortality (Idler and Benyamini, 1997; Burström and Fredlund, 2001). Area deprivation at baseline is based on Carstairs' score for postcode sectors (average population=5,000) derived from the 1991 Census (McLoone and Boddy, 1994). Carstairs' scores provide an index of deprivation based on an unweighted combination of four census variables comprising the proportion of: households in the area that are overcrowded; heads of household in the area that are in social classes IV and V; male heads of household in the area that are unemployed and households in the area that do not have access to a car. Based on these scores, the areas have been divided into seven deprivation categories (hereafter referred to as depcats); in this paper we have grouped them further for ease of presentation into three groups: 1 and 2, ‘most affluent’; 3, 4 and 5, ‘middling’; 6 and 7, ‘most deprived’. Baseline social class was coded according to the Registrar General’s 1980 classification (OPCS, 1980) for head of household's current or previous occupation. Length of residence at baseline was measured by asking respondents how long they had lived at their current address.
The distribution of respondents at each wave according to these key baseline characteristics is shown in Table 1. The proportion of respondents who were in the oldest cohort, in poor health, in manual classes or living in the most disadvantaged areas at baseline has declined over the 20 years of the study. However, the final column shows the data used for the models in this paper (person-waves) and these are relatively similar to the baseline sample for most characteristics except area deprivation.
Table 1.
Proportion (%) of respondents taking part in each wave by their baseline characteristics.
| Baseline characteristics | Wave 1 1987/1988 | Wave 2 1990/1992 | Wave 3 1995/1997 | Wave 4 2000/2004 | Wave 5 2007/2008 | Modelling dataa |
|---|---|---|---|---|---|---|
| % 1970s cohort | 33.6 | 35.2 | 30.8 | 31.7 | 36.2 | 34.1 |
| % 1950s cohort | 32.0 | 31.9 | 34.5 | 36.8 | 38.4 | 33.3 |
| % 1930s cohort | 34.4 | 33.0 | 34.7 | 31.5 | 25.5 | 32.6 |
| % men | 46.5 | 46.1 | 44.6 | 45.0 | 44.6 | 46.2 |
| % women | 53.5 | 53.9 | 55.4 | 55.0 | 55.4 | 53.8 |
| % good starting healthb | 72.7 | 76.1 | 76.6 | 78.6 | 80.4 | 78.1 |
| % poor starting healthb | 23.4 | 22.8 | 22.3 | 20.3 | 18.2 | 20.8 |
| % missing starting healthb | 3.9 | 1.1 | 1.1 | 1.1 | 1.4 | 1.1 |
| % non-manual classes | 42.0 | 43.7 | 46.3 | 48.0 | 48.5 | 48.0 |
| % manual classes | 54.0 | 52.9 | 50.6 | 48.6 | 47.6 | 52.0 |
| % missing class | 4.0 | 3.5 | 3.1 | 3.5 | 3.9 | N/A |
| % depcat 1 or 2 (affluent) | 15.2 | 15.9 | 16.9 | 17.9 | 18.4 | 17.5 |
| % depcat 3, 4 or 5 | 45.9 | 47.4 | 49.6 | 49.0 | 48.6 | 49.0 |
| % depcat 6 or 7 (disadvantaged) | 38.8 | 36.6 | 33.5 | 33.1 | 33.0 | 33.5 |
| Total interviewed | 4510 | 3820 | 2972 | 2661 | 2604 | 11607 |
Data modelled as person-waves using Waves 2–5.
Question wording and response categories for self-rated health differed slightly for the 1970s cohort at baseline.
4. Modelling strategy
Given the clustered nature of the data — both geographically and within individuals — hierarchical repeat measures models, also known as growth curve models, were employed, which use pseudo-maximum likelihood estimators to adjust for non-response under the assumption that any missing data are missing at random (Clarke and Hardy, 2007). Data were included in the analysis for each wave in which respondents participated, thus only missed waves were excluded, reducing potential attrition bias. Multilevel models also allow variation between the original sampling areas to be distinguished from variation between individuals within areas so that the area variation can be examined explicitly. Models were fitted in MLwiN version 2.15 (Rasbash et al., 2009) with three levels-measurement points (level 1, N=11,607) nested within individuals (level 2, N=3,683) nested within the original sampling units (level 3, N=62 postcode sectors). The significance of individual variables was assessed using the Wald test. Baseline social class was split into a dichotomous variable (non-manual vs. manual). To keep the estimates for other parameters neutral (Sacker et al., 2005), gender has been coded −0.5 for men and 0.5 for women, and a similar centring was used for the dichotomised baseline social class variable. Length of residence at baseline and age were included in models as continuous variables (centred on their respective means). Dummy variables for cohort (reference cohort—1950s) were used in most analyses and these were switched to dummy variables for study wave (reference wave—1990/1992) in a range of sensitivity analyses as described below.
The first step was to examine health outcomes at waves 2–5 with explanatory variables (age, gender and social class) measured at wave 1. Modelling was performed in four main stages. First, drawing on other work (Benzeval et al., submitted for publication) the best fitting age function (cubic) was used to model the age–health trajectory, adjusting for gender and cohort, to establish the extent to which self-reported health varied across areas (in this case postcode sectors) and act as a benchmark to compare other findings (Model 1, not shown). Next, to investigate whether area deprivation explained variation across places and whether this varied as respondents aged, area deprivation was added to Model 1 as a main effect and interaction with age (Model 2). Thirdly, we investigated whether any differences by area deprivation could be explained by individual level socio-economic status by adding individuals' social class at baseline (as a main effect and interactions with age) to the model (Model 3). Finally, to understand the extent to which individual effects by themselves explained the between place variation in health trajectories, we also constructed a model using only age, cohort, baseline class and gender without area deprivation (Model 4), and examined the proportion of the area variance explained for each model. Each of these models was repeated stratified by gender. To investigate further the extent to which individual or area deprivation explains the between place differences in the health trajectories, we examined the proportion of area variance in self-rated health explained by the different sets of explanatory factors. The proportion of the total variation that was attributable to areas was calculated following the calculations of intraclass correlation coefficients for logistic regression models based on the assumption of a threshold model (Snijders and Bosker, 1999).
In order to assess whether the associations were robust to adjustment we undertook a range of separate sensitivity analyses. Length of residence at baseline was added to the model and interactions with depcat and depcat by age were tested to see if effects were stronger for those who had been resident in their respective areas for longer periods. The dummy variables for cohort were replaced with dummy variables for study wave to assess period effects. The analysis was also repeated for two sub-samples of respondents: those person-waves where the respondent remained resident in their baseline postcode sector (n=7076 person-waves) to remove potential migration effects, and those respondents who had participated in all survey waves (n=7368 person-waves) to investigate whether the associations differed for those followed for the full 20 years. Random intercept models were used, with the relationship between age and self-reported health assumed to be constant across areas.
Results are presented graphically as growth curves of predicted probabilities (from the fixed part of the models, the method of constructing these is given in the online supplementary material associated with this paper), with their 95% confidence intervals (represented by the shaded grey bands). The age at which respondents from different area deprivation categories experience the same probability of reporting poor health has also been calculated to illustrate the degree to which those in more disadvantaged areas ‘get sicker’ at younger ages than others.
5. Results
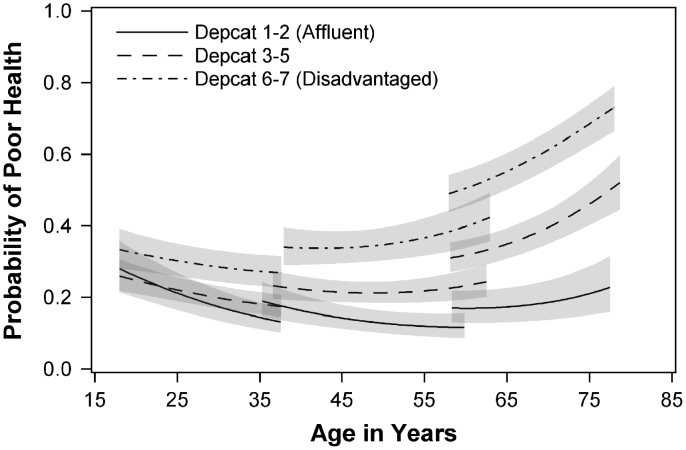
Fig. 1 illustrates the poor health trajectories of the three cohorts for the three area deprivation groups, and is derived from Model 2 (i.e. the model with area deprivation, age, cohort, gender and the interaction between area deprivation and age). Respondents living in the most deprived areas at baseline have higher probabilities of reporting poor health than others at all ages; but the gap between them and those living in the most affluent areas widens as people age. The same is true of the middle group (depcats 3, 4 and 5), which has a similar shaped age trajectory, but a lower probability of poor health than that of those from the most deprived areas.
Fig. 1.
Predicted trajectories in probability of poor health⁎ by age and area deprivation, adjusting for gender. (⁎Modelling began by examining health at Wave 2–5. There is a slight overlap in ages between consecutive cohorts at Waves 2 and 5 for a small number of cases (due to variations in dates of birth and interview dates)).
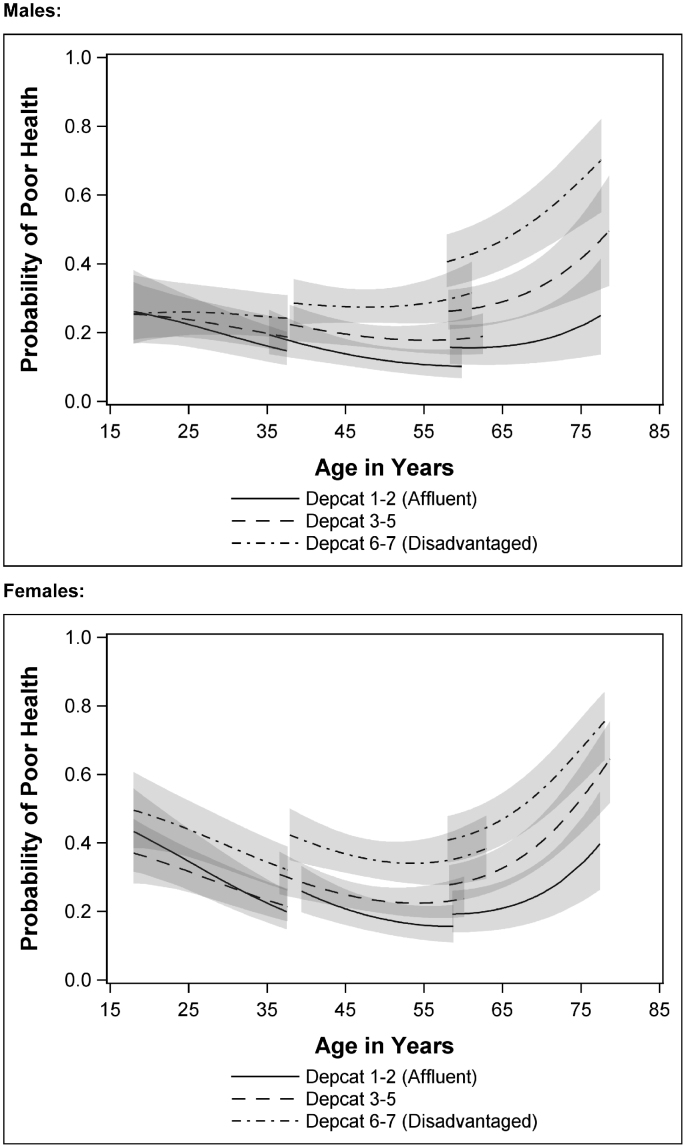
Fig. 2 shows age-trajectories by area deprivation categories for men and women separately, controlling for individual social class (Model 3). Women have a higher starting level of poor health (at age 18) than men, and while not statistically significant (at the 95% level) more of a difference in initial health by area deprivation can be seen for women than for men in the younger cohorts. Inequalities between those living in deprived areas at baseline and others grow for both men and women thereafter, becoming significant around the age of 38. From these ages the area inequalities gap between those living in affluent and deprived areas grows as people age and appears to widen more steeply for men than for women.
Fig. 2.
Predicted trajectories in probability of poor health⁎ by gender and area deprivation, adjusting for individual social class. (⁎Modelling health began with examining health at Waves 2–5, explanatory variables (age, gender, social class and area of residence) are measured at Wave 1).
In order to investigate further the extent to which individual or area deprivation explains the between place differences in the health trajectories, we examined the proportion of area variance in self-rated health explained by the different sets of explanatory factors. The area level variance accounted for 6.67% of the total variance in the model based on the combined sample of men and women, 5.78% in the male only model and 5.58% in the women only model. Table 2 shows that adding area deprivation (in Model 2) explained almost three quarters of the area level variance (72.3%). The addition of individual social class (Model 3) explained a further 12.3%, suggesting that this factor is also patterned by area of residence. Subtracting the total contribution of class, age, cohort and gender (from Model 4: 44.1%) from the combined effect of area and individual factors, suggests that 40.5% of the area level variation is uniquely explained by area deprivation and its interaction with age. Area deprivation explains relatively less of the area level variation in women than it does in men (Model 2: 93.1% for men compared to 73.9% for women), and for men the combination of area deprivation, class and gender entirely explains the area level variation in health, whereas only 84.7% is explained for women (Model 3). Subtracting the explained variance for individual factors only (Model 4) from these totals suggests that area deprivation uniquely accounts for 40.3% of the area variation in men and 37.9% in women.
Table 2.
Proportion of variance explained by each model.
| Model | Variables | Percentage of model 1 area level variance explained |
|---|---|---|
| All | ||
| 1 | Constant, age, age-squared, age-cubed, gender and cohort | n/a |
| 2 | As model 1 adding depcat, and depcat×agea | 72.2 |
| 3 | As model 2 adding class, class×age, class×age-squared, class×age-cubed | 84.6 |
| 4 | As model 3 without depcat or depcat×age | 44.1 |
| Males | ||
| 1 | Constant, age, age-squared, age-cubed, and cohort | n/a |
| 2 | As model 1 adding depcat, and depcat×agea | 93.1 |
| 3 | As model 2 adding class, class×age, class×age-squared, class×age-cubed | 100.0 |
| 4 | As model 3 without depcat or depcat×age | 59.7 |
| Females | ||
| 1 | Constant, age, age-squared, age-cubed, and cohort | n/a |
| 2 | As model 1 adding depcat, and depcat×agea | 73.9 |
| 3 | As model 2 adding class, class×age, class×age-squared, class×age-cubed | 84.7 |
| 4 | As model 3 without depcat or depcat×age | 46.8 |
Interactions between depcat and age-squared or age-cubed were left out as they were not significant at the p<0.05 level in most models. For females only the interaction effect between age-squared and being in the most deprived category was significant in Model 2 but not in model 3, suggesting that this was mainly due to effects of individual class, and so this has been left out for consistency with the overall and male only models.
Table 3 illustrates the age gap between living in the two most deprived depcats at baseline and elsewhere for different probabilities of reporting ill health. The age estimates in Table 3 are derived from Model 3; they are adjusted for gender and baseline social class. So, for example, those living in the most deprived areas (depcats 6 and 7) at baseline would reach a 40% probability of reporting poor health at around age 66, while those living in the most affluent areas would not reach this probability until they were almost 83 years old, a difference of around 16 years. Even those living in the ‘middling’ deprived areas at baseline will not reach the same probability of ill health until 9 years after those in the poorest areas, at the age of 75. For men the difference between the most and least deprived areas was almost 20 years, while for women the same difference was just over 15 years, showing wider area inequalities in men’s compared to women's health.
Table 3.
Ages at which particular probabilities for reporting poor health are predicted for respondents in different area deprivation categories.
| Age at which probability of poor health is attained… | Agea (differenceb) all |
Agea (differenceb) males |
Agea (differenceb) females |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Depcats 6 and 7 | Depcat 3–5 | Depcat 1 and 2 | Depcat 6 and 7 | Depcat 3–5 | Depcat 1 and 2 | Depcat 6 and 7 | Depcat 3–5 | Depcat 1 and 2 | |
| Probability of 0.4c | 66.4 (−) | 75.4 (+9.0) | 82.8 (+16.4) | 68.6 (−) | 79.5 (+10.9) | 88.1 (+19.5) | 64.2 (−) | 72.6 (+8.4) | 79.4 (+15.2) |
| Probability of 0.5c | 71.9 (−) | 78.9 (+7.0) | 85.5 (+13.6) | 73.9 (−) | 83.0 (+9.1) | 90.7 (+16.8) | 70.3 (−) | 76.2 (+5.9) | 82.2 (+11.9) |
| Probability of 0.6c | 75.8 (−) | 81.8 (+6.0) | 87.8 (+12.0) | 77.9 (−) | 85.9 (+8.0) | 93.0 (+15.1) | 74.4 (−) | 79.1 (+4.7) | 84.7 (+10.3) |
Values for all respondents are adjusted for gender and baseline social class, and figures for males and females are adjusted for baseline social class (i.e. Model 3). All values are calculated for a respondent from the 1950s cohort.
The term in brackets represents the predicted difference in years with depcats 6 and 7 as the reference category.
In some instances the model also predicts a probability of poor health at or above this level at younger ages as well but the focus of comparison was the point at which the predicted probability curve crosses from below to above these thresholds with increasing age.
A number of sensitivity analyses were performed (results are provided in the online supplementary material associated with this paper). The relationship between area deprivation, age and the probability of poor health was found to be robust to adjustment for period effects and the length of residence at the baseline postcode sector. Repeating the modelling using only those person-waves where respondents were still resident at their baseline postcode at the end of the 20-year follow-up did not substantively alter the results, nor did repeating the modelling using only those respondents who had participated at every wave.
6. Discussion
We have shown that, during a 20 year period between 1987 and 2007, in a large urban and periurban region in the West of Scotland, there are differences in reporting poor self-rated health by deprivation of place of residence at baseline, controlling for age, cohort, gender and socioeconomic status; with those in poorer neighbourhoods reporting poor health at much younger ages, and the likelihood of reporting poor health in deprived neighbourhoods increasing more steeply with age, than for those in better off neighbourhoods. Adding to current debates about differential place effects by gender (Frye et al., 2008), we also found wider area differences in old-age for men than for women, although overall, women were more likely to report poor health at an earlier age than men. These findings were robust for control for period effects and length of residence. The estimated age differences in the probability of reporting poor health are substantial; for a 40% probability, the middling areas would report poor health some 9 years after those in the poorest neighbourhoods, and those in the richest neighbourhoods would not have this probability of reporting poor health for an additional 7 years.
There are a number of important implications of these findings, some methodological, some theoretical and some practical. Our analysis of area differences reveals important evidence as to how the relationship between age and poor health not only varies by deprivation categories but also how age-trajectories vary by place of residence. Routinely controlling for age in an analysis of area differences may well mask such evidence. One theoretical implication is that both low socioeconomic status and neighbourhood deprivation seem to have cumulative, long-term, effects on self-reported health. Whether this results from a critical period process (living in poor circumstances at a particular stage in life programmes the body to deteriorate more rapidly subsequently) or from cumulative exposure or vulnerability to adverse, and possibly worsening, circumstances cannot be answered from this analysis, but could be the subject of further analysis on this or other cohorts.
Practical implications are that neighbourhood deprivation differences in poor self rated health may start relatively early in life, and exist over and above individual socio-economic differences. This suggests that attempts to reduce inequalities in health should focus on places as well as people, and recognise a greater burden of morbidity among both poor places and poor people. The other major practical implication is that attempts to reduce area inequalities in health should start young (Curtis et al., 2004), to avoid the initial development of area differences, but also may need to be continued throughout the lifespan to avoid continued divergence between social groups.
6.1. Limitations
While the Twenty-07 Study ranges in age from 15 to 76 (in three separate cohorts), it does not cover childhood or older old-age. This is a limitation shared in much of the literature, reflecting the length and scope of many longitudinal studies. This paper focuses on self-assessed health, which has been shown to be a good predictor of mortality and morbidity, but the way people answer the question may change with age and period (Hoeymans et al., 1997). It has been hypothesised that there may also be SES differences in response to this question (Burström and Fredlund, 2001; Singh-Manoux et al., 2007). However, we found this was not the case with longstanding illness in the Twenty-07 Study (Macintyre et al., 2005). In this analysis we have looked at area of residence at baseline, rather than at every wave of contact, so have not been able to examine moves between different types of area, or any self-selective processes involved in residential migration. Similarly, and by definition, we have not been able to examine health or other social characteristics preceding the residence ascertained at baseline, so have not been able to examine selection processes directly. Finally, our measure of the area of residence is based on postal geography, not respondent defined neighbourhoods, and a pre-existing measure of area deprivation, rather than a richer measure of area characteristics based on a larger set of contextual measures. However the Carstairs score was developed in a way which captured postcode sector differences in mortality, and is widely used in health geography in the UK.
Strengths of this study are that it uses a general population sample from a socially and geographically heterogeneous region, rather than an occupational cohort (e.g. Stafford et al., 2008), covers 60 years of the life course, can control for period and cohort effects, and includes a range of small areas with varying social and material conditions.
Our findings are consistent with those reported from other studies in a range of different countries in showing an association between area deprivation and poor self-rated health, controlling for individual characteristics (Pickett and Pearl, 2001; Riva et al., 2007). However we have been able to add to these predominantly cross-sectional studies by showing that this association strengthens with age, and that these trajectories are robust to control for prior length of residence and for remaining in the area. These results are consistent with the hypothesis of differential ‘weathering’ (Bird et al., 2010; Geronimus et al., 2006) and our findings suggest that this weathering process is related not only to individual or family socioeconomic adversity, but also to area level adversity.
Acknowledgement
We are grateful to all of the participants in the Twenty-07 Study, and to the survey staff and research nurses who carried it out. The West of Scotland Twenty-07 Study is funded by the UK Medical Research Council (MC_US_A540_0080) and the data were originally collected by the MRC Social and Public Health Sciences Unit. AE, SM, MB and MG are funded by the MRC (MC_US_A540_0073; MC_US_A540_0056) and AL by the Chief Scientist Office of the Scottish Government Health Directorates (MC_US_A540_0001).
Footnotes
Supplementary materials associated with this article can be found in the online version at doi:10.1016/j.healthplace.2011.08.005.
Appendix A. Supplementary materials
Supplementary materials
References
- Ahluwalia J.S., Nollen N., Kaur H., James A.J., Mayo M., Resnicow K. Pathways to health: cluster-randomized trial to increase fruit and vegetable consumption among smokers in public housing. Health Psychology. 2007;26:214–221. doi: 10.1037/0278-6133.26.2.214. [DOI] [PubMed] [Google Scholar]
- Amuzu A., Carson C., Watt H., Lawlor D., Ebrahim S. Influence of area and individual lifecourse deprivation on health behaviours: findings from the British Women's Heart and Health Study. European Journal of Cardiovascular Prevention and Rehabilitation : Official Journal of the European Society of Cardiology, Working Groups on Epidemiology & Prevention and Cardiac Rehabilitation and Exercise Physiology. 2009;16:169–173. doi: 10.1097/HJR.0b013e328325d64d. [DOI] [PubMed] [Google Scholar]
- Beard J., Cerda M., Blaney S., Ahern J., Vlahov D., GALEA S. Neighborhood characteristics and change in depressive symptoms among older residents of New York city. American Journal of Public Health. 2009;99:1308–1314. doi: 10.2105/AJPH.2007.125104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benzeval M., Der G., Ellaway A., Hunt K., Sweeting H., West P. Cohort profile: west of Scotland Twenty-07 Study: health in the community. International Journal of Epidemiology. 2008 doi: 10.1093/ije/dyn213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benzeval, M., Green, M. & Leyland, A. submitted for publication. Do social inequalities in health widen or converge with age? Longitudinal evidence from three cohorts in the west of Scotland. [DOI] [PMC free article] [PubMed]
- Bird C.E., Seeman T., Escarce J.J., Basurto-Davila R., Finch B.K., Dubowitz T., Heron M., Hale L., Merkin S.S., Weden M., Lurie N. Neighbourhood socioeconomic status and biological 'wear and tear' in a nationally representative sample of US adults. Journal of Epidemiology and Community Health. 2010;64:860–865. doi: 10.1136/jech.2008.084814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burström B., Fredlund P. Self rated health: is it as good a predictor of subsequent mortality among adults in lower as well as in higher social classes? Journal of Epidemiology and Community Health. 2001;55:836–840. doi: 10.1136/jech.55.11.836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaix B. Geographic life environments and coronary heart disease: a literature review, theoretical contributions, methodological updates, and a research agenda. Annual Review of Public Health. 2009;30:81–105. doi: 10.1146/annurev.publhealth.031308.100158. [DOI] [PubMed] [Google Scholar]
- Chuang Y.C., Chuang K.Y. Gender differences in relationships between social capital and individual smoking and drinking behavior in Taiwan. Social Science and Medicine. 2008;67:1321–1330. doi: 10.1016/j.socscimed.2008.06.033. [DOI] [PubMed] [Google Scholar]
- Clarke P., Hardy R. Methods for handling missing data. In: Pickles A.M.B., Wadsworth M., editors. Epidemiological Methods in Life Course Research. Oxford University Press; Oxford: 2007. [Google Scholar]
- Curtis S., Southall H., Congdon P., Dodgeon B. Area effects on health variation over the life-course: analysis of the longitudinal study sample in area of residence England using new data on in childhood. Social Science and Medicine. 2004;58:57–74. doi: 10.1016/s0277-9536(03)00149-7. [DOI] [PubMed] [Google Scholar]
- Daniel M., Moore S., Kestens Y. Framing the biosocial pathways underlying associations between place and cardiometabolic disease. Health and Place. 2008;14:117–132. doi: 10.1016/j.healthplace.2007.05.003. [DOI] [PubMed] [Google Scholar]
- Davey Smith G., Hart C., Watt G., Hole D., Hawthorne V. Individual social class, area-based deprivation, cardiovascular disease risk-factors and mortality: the Renfrew and Paisley study. Journal of Epidemiology and Community Health. 1998;52:399–405. doi: 10.1136/jech.52.6.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Der G. MRC Medical Sociology Unit; Glasgow: 1998. A Comparison of the West of Scotland Twenty-07 Study Sample and the 1991 Census SARs. [Google Scholar]
- Diezroux A.V., Nieto F.J., Muntaner C., Tyroler H.A., Comstock G.W., Shahar E., Cooper L.S., Watson R.L., Szklo M. Neighborhood environments and coronary heart disease: a multilevel analysis. American Journal of Epidemiology. 1997;146:48–63. doi: 10.1093/oxfordjournals.aje.a009191. [DOI] [PubMed] [Google Scholar]
- Ecob R., Macintyre S. Small area variations in health related behaviours; do these depend on the behaviour itself, its measurement, or on personal characteristics? Health and Place. 2000;6:261–274. doi: 10.1016/s1353-8292(00)00008-3. [DOI] [PubMed] [Google Scholar]
- Ellaway A., Macintyre S. Does where you live predict health related behaviours? A case study in Glasgow. Health Bulletin. 1996;54:443–446. [PubMed] [Google Scholar]
- Ellaway, A. & Macintyre,, S. 2001. Women in their place: gender and perceptions of neighbourhoods in the West of Scotland. In: Dyck, I., Davis Lewis, N., Mclafferty, S. (Eds.), Geographies of Women's Health.
- Ellaway A., Macintyre S. Are perceived neighbourhood problems associated with the likelihood of smoking? Journal of Epidemiology and Community Health. 2009;63:78–90. doi: 10.1136/jech.2007.068767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frye V., Putnam S., O'campo P. Whither gender in urban health? Health and Place. 2008;14:616–622. doi: 10.1016/j.healthplace.2007.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus A.T., Hicken M., Keene D., Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health. 2006;96:826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giskes K., Van Lenthe F., Turrell G., Brug J., Mackenbach J. Smokers living in deprived areas are less likely to quit: a longitudinal follow-up. Tobacco Control. 2006;15:485–488. doi: 10.1136/tc.2006.015750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haan M., Kaplan G.A., Camacho T. Poverty and health—prospective evidence from the Alameda County Study. American Journal of Epidemiology. 1987;125:989–998. doi: 10.1093/oxfordjournals.aje.a114637. [DOI] [PubMed] [Google Scholar]
- Hoeymans N., Feskens E.J.M., Van Den Bos G.A.M., Kromhout D. Age, time, and cohort effects on functional status and self-rated health in elderly men. American Journal of Public Health. 1997;87:1620–1625. doi: 10.2105/ajph.87.10.1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler E., Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Jones K., Duncan C. Individuals and their ecologies: analysing the geography of chronic illness within a multilevel modelling framework. Health and Place. 1995;1:27–40. [Google Scholar]
- Kavanagh A.M., Bentley R., Turrell G., BROOM D.H., Subramanian S.V. Does gender modify associations between self rated health and the social and economic characteristics of local environments? Journal of Epidemiology and Community Health. 2006;60:490–495. doi: 10.1136/jech.2005.043562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D. Blues from the neighborhood? Neighborhood characteristics and depression. Epidemiologic Reviews. 2008;30:101–117. doi: 10.1093/epirev/mxn009. [DOI] [PubMed] [Google Scholar]
- Macintyre S., Der G., Norrie J. Are there socioeconomic differences in responses to a commonly used self report measure of chronic illness? International Journal of Epidemiology. 2005;34:1284–1290. doi: 10.1093/ije/dyi200. [DOI] [PubMed] [Google Scholar]
- Macintyre S., Ellaway A., Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Social Science and Medicine. 2002;55:125–139. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- Mcloone P., Boddy F. Deprivation and mortality in Scotland, 1981 and 1991. British Medical Journal. 1994;309:1465–1470. doi: 10.1136/bmj.309.6967.1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molinari C. The relationship of community quality to the health of women and men. Social Science and Medicine. 1998;47:1113–1120. doi: 10.1016/s0277-9536(98)00114-2. [DOI] [PubMed] [Google Scholar]
- Naimi A.I., Paquet C., Gauvin L., DANIEL M. Associations between area-level unemployment, body mass index, and risk factors for cardiovascular disease in an urban area. International Journal of Environmental Research and Public Health. 2009;6:3082–3096. doi: 10.3390/ijerph6123082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OPCS . HMSO; London: 1980. Classification of Occupations and Coding Index. [Google Scholar]
- Parkes A., Kearns A. The multi-dimensional neighbourhood and health: a cross-sectional analysis of the Scottish Household Survey, 2001. Health and Place. 2006;12:1–18. doi: 10.1016/j.healthplace.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Pickett K., Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcome: a critical review. Journal of Epidemiology and Community Health. 2001;55:111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plantinga A.J., Bernell S. The association between urban sprawl and obesity: is it a two-way street? Journal of Regional Science. 2007;47:857–879. [Google Scholar]
- Plantinga A.J., Bernell S. Can urban planning reduce obesity? The role of self-selection in explaining the link between weight and urban sprawl. Review of Agricultural Economics. 2007;29:557–563. [Google Scholar]
- Pollack C.E., Cubbin C., Ahn D., Winkleby M. Neighbourhood deprivation and alcohol consumption: does the availability of alcohol play a role? International Journal of Epidemiology. 2005;34:772–780. doi: 10.1093/ije/dyi026. [DOI] [PubMed] [Google Scholar]
- Poortinga W., Dunstan F.D., Fone D.L. Neighbourhood deprivation and self-rated health: the role of perceptions of the neighbourhood and of housing problems. Health and Place. 2008;14:562–575. doi: 10.1016/j.healthplace.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Rasbash J., Charlton C., Brown W.J., Healy M., Cameron B. University of Bristol; 2009. MLwiN Version 2.1. Centre for Multilevel Modelling. [Google Scholar]
- Riva M., Gauvin L., Barnett T. Toward the next generation of research into small area effects on health: a synthesis of multilevel investigations published since July 1998. Journal of Epidemiology and Community Health. 2007;61:853–861. doi: 10.1136/jech.2006.050740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruel E., Reither E., Robert S., Lantz P. Neighborhood effects on BMI trends: examining BMI trajectories for Black and White women. Health and Place. 2010;16:191–198. doi: 10.1016/j.healthplace.2009.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacker A., Clarke P., Wiggins R., Bartley M. Social dynamics of health inequalities: a growth curve analysis of aging and self assessed health in the British household panel survey 1991–2001. Journal of Epidemiology and Community Health. 2005;59:495–501. doi: 10.1136/jech.2004.026278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh-Manoux A., Dugravot A., Shipley M.J., Ferrie J.E., Martikainen P., Goldberg M., Zins M. The association between self-rated health and mortality in different socioeconomic groups in the GAZEL cohort study. International Journal of Epidemiology. 2007;36:1222–1228. doi: 10.1093/ije/dym170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snijders T., Bosker R. Sage; London: 1999. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modelling. [Google Scholar]
- Stafford M., Brunner E., Head J., Ross N. Deprivation and the development of obesity. American Journal of Preventive Medicine. 2010;39:130–139. doi: 10.1016/j.amepre.2010.03.021. [DOI] [PubMed] [Google Scholar]
- Stafford M., Cummins S., Macintyre S., Ellaway A., Marmot M. Gender differences in the associations between health and neighbourhood environment. Social Science and Medicine. 2005;60:1681–1692. doi: 10.1016/j.socscimed.2004.08.028. [DOI] [PubMed] [Google Scholar]
- Stafford M., Gimeno D., Marmot M. Neighbourhood characteristics and trajectories of health functioning: a multilevel analysis. European Journal of Public Health. 2008;18:604–610. doi: 10.1093/eurpub/ckn091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters K., Breeze E., Wilkinson P., Price G., Bulpitt C., Fletcher A. Local area deprivation and urban–rural differences in anxiety and depression among people older than 75 years in Britain. American Journal of Public Health. 2004;94:1768–1774. doi: 10.2105/ajph.94.10.1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt G., Ecob R. Mortality in Glasgow and Edinburgh: a paradigm of inequality in health. Journal of Epidemiology and Community Health. 1992;46:498–505. doi: 10.1136/jech.46.5.498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt G.C.M. Differences in expectation of life between Edinburgh and Glasgow: implications for health policy in Scotland. Health Bulletin. 1993;51:407–417. [PubMed] [Google Scholar]
- White H.L., Matheson F.I., Moineddin R., Dunn J.R., Glazier R.H. Neighbourhood deprivation and regional inequalities in self-reported health among Canadians: are we equally at risk? Health and Place. 2011;17:361–369. doi: 10.1016/j.healthplace.2010.11.016. [DOI] [PubMed] [Google Scholar]
- Yen I.H., Kaplan G.A. Poverty area residence and changes in physical activity level: evidence from the Alameda County Study. American Journal of Public Health. 1998;88:1709–1712. doi: 10.2105/ajph.88.11.1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen I.H., Kaplan G.A. Poverty area residence and changes in depression and perceived health status: evidence from the Alameda County Study. International Journal of Epidemiology. 1999;28:90–94. doi: 10.1093/ije/28.1.90. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary materials