Abstract
Purpose:
Interprofessional collaboration in health care is believed to enhance patient outcomes. However, where professions have overlapping scopes of practice (eg, chiropractors and physical therapists), "turf wars" can hinder effective collaboration. Deep-rooted beliefs, identified as implicit attitudes, provide a potential explanation. Even with positive explicit attitudes toward a social group, negative stereotypes may be influential. Previous studies on interprofessional attitudes have mostly used qualitative research methodologies. This study used quantitative methods to evaluate explicit and implicit attitudes of physical therapy students toward chiropractic.
Methods:
A paper-and-pencil instrument was developed and administered to 49 individuals (students and faculty) associated with a Canadian University master's entry-level physical therapy program after approval by the Research Ethics Board. The instrument evaluated explicit and implicit attitudes toward the chiropractic profession. Implicit attitudes were determined by comparing response times of chiropractic paired with positive versus negative descriptors.
Results:
Mean time to complete a word association task was significantly longer (t = 4.75, p =.00) when chiropractic was associated with positive rather than negative words. Explicit and implicit attitudes were not correlated (r = 0.13, p =.38).
Conclusions:
While little explicit bias existed, individuals associated with a master's entry-level physical therapy program appeared to have a significant negative implicit bias toward chiropractic
Keywords: Attitude, Chiropractic, Education, Interprofessional Relations, Physical Therapy
Introduction
In 2009, the government of Ontario, Canada, provided a challenge to professional colleges and universities to incorporate appropriate interprofessional education (IPE) in their curricula. It is acknowledged that there is a need for professions to cooperate and that communication is sometimes hampered by cultural constraints and professional barriers.1,2 The evolution of professional cultures involves both education and personal attributes.3 As a result, new educational initiatives in this area should consider interprofessional attitudes. Lewitt and colleagues found that attitudinal concerns, such as stereotyping, were already in place at the undergraduate level and perceived as a barrier to effective IPE.4 The research reported here is a preliminary evaluation of professional attitudes that may affect the development of IPE involving the chiropractic profession.
Deep-rooted prejudices5 and professional “territoriality”6 challenge successful integration of disparate views and represent a significant barrier to interprofessional collaborative care. Enhanced patient outcomes are expected to result from successful collaboration between health care providers.7–9 However, collaborations are as complex as jurisdictional boundaries, historically associated with turf wars10 and by team members attempting to reach common goals.6,11 Of particular concern is a growing body of evidence indicating that some of the unnecessary error in patient management can be attributed to poor communication between health care professionals.12,13
Interprofessional disputes have been associated with the traditional approach of teaching professionals in silos.14 This information has led to an evolution in health care education, with movement toward an interprofessional curriculum in an attempt to improve collaborative practice.15 Unfortunately, results of such programs to date do not appear to have had the longitudinal effects that can be expected to translate into changes in behavior, since change in attitude has not been observed in some research.16
Currently, protocols are being developed to infuse permanent leadership into interprofessional education with the hope of maintaining sustainability.17 Evaluation of protocol success via monitoring change in student attitudes has been suggested as an essential component of interdisciplinary training.2 Attitudes therefore need to be identified and incorporated into these protocols. The basic foundational attitudes that define these protocols have not, however, been explored.
In addition, solving the challenges posed by the evolution of interprofessional care requires a clear understanding of the magnitude of the issues involved. Scant quantitative research has been dedicated to understanding the complex relationships between professions. Rather, the majority of studies have used qualitative methodologies to understand the issues that surround various collaborative ventures.18,19 From these studies, attitudes between team members have been identified as an underlying construct for optimal collaboration.4,19,20
The study of attitudes is challenging. Sensitive to societal norms of nondiscrimination and equality, respondents may try to avoid appearing prejudiced and adjust their answers accordingly.21 Conversely, it is believed that a person may hold positive attitudes toward a social group but may still be influenced by negative stereotypes.22 This disparity may be reflected by what has been referred to as “implicit” versus “explicit” attitudes. It is believed that implicit attitudes operate on an subconscious level, reflecting an automatic mental process, while explicit attitudes operate on a conscious level and are almost entirely under the control of the individual.21,23 Rydell and McConnell have demonstrated that people can hold different implicit and explicit attitudes toward the same object at the same time dependent on how the information activates different reasoning patterns.24
To understand attitudes toward the chiropractic profession and its relationship with other health care practitioners, it is important to discuss the musculoskeletal system and pain. Musculoskeletal pain represents a significant health care burden to society, with a total direct cost of 25.6 billion Canadian dollars (in 1994 Canadian dollars, $1.00 CDN is approximately $0.75 US), accounting for 3.4% of the gross domestic product.25 Several professions lay claim to this clinical territory, including, but not limited to, general practice physicians, physiatrists, orthopaedic surgeons, neurosurgeons, occupational therapists, physical therapists, and chiropractors. Overlapping scopes of practice could be anticipated to result in commonalities and the altruism on which collaborative care might be based.26 However, anticipated territorial behavior would suggest that altruism is unlikely to dominate, thus hampering the possibility of integrative knowledge that would optimize care and benefit the patient.
As a subset of practitioners with an interest in musculoskeletal pain, physical therapists and chiropractors have synergistic skills intended to benefit patient outcomes. For example, a chiropractor may choose to provide manipulation, and the physical therapist may supervise rehabilitative therapies. In the evolving health care system, patients should expect collaboration and interaction between these professions. However, little is known about the strength of their respective implicit and explicit attitudes toward each other's profession and whether such issues need to be considered at the professional education level.
This was a preliminary study designed to examine the implicit attitudes of physical therapy students and faculty involved in a university-based master's entry-level physical therapy (UBMELPT) program toward the chiropractic profession. It was hypothesized that, given societal influences related to a greater appreciation for complementary and alternative medicine (CAM), the explicit attitudes of physical therapy students would be positive, but the implicit attitudes would lag behind (influenced by previous stereotypes) and would therefore be negative.
Methods
This study was approved by the Research Ethics Board of the Canadian Memorial Chiropractic College and McMaster University. There were no external funds utilized in conducting this study.
An implicit association test (IAT) was developed using procedures outlined by Greenwald and colleagues to evaluate implicit attitudes toward chiropractic and medical care.27 The IAT was administered according to previous procedures by Greenwald et al (https://implicit.harvard.edu/implicit/research/—originally downloaded August 2008 and rechecked March 1, 2011). As per Wittenbrink and colleagues, the differences in response latencies between identifying groups with potentially associated stereotypes (eg, race) and either positive or negative descriptors were taken as evidence of the strength of the association made by the participant between the descriptors and groups.21 For the purpose of this study, the methods used by Greenwald et al were modified to allow administration of the test in pencil-and-paper format rather than via computer. Previous research suggests that the IAT shows predictive validity for social issues such as race, gender, ethnicity, sexual orientation, and age.28 Jurisdictional bias between professions has not previously been tested, and this is considered a limitation to this study.
A survey was conducted to determine which words best reflected the profession of either chiropractic or medicine. These words were used in the word association task of the IAT. Medicine was chosen as the contrasting profession because of its dominance in mainstream health care. Chiropractic has historically been chosen as the proxy for complementary and alternative practices29,30 and, in this study, represents the profession with which physical therapy, which has historically been accepted within the biomedical paradigm, could be considered to have substantial synergy.
Item Development
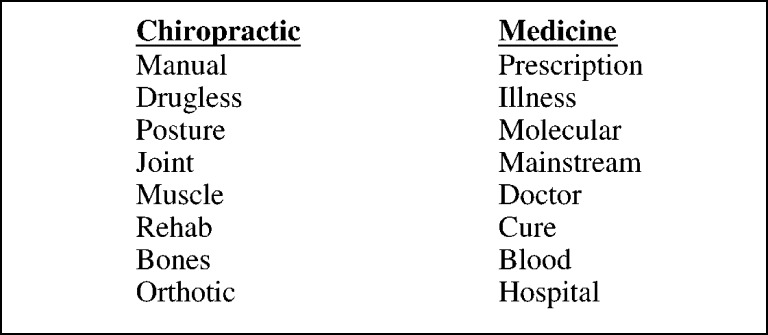
Because work in implicit attitudes between professionals has not been conducted previously, items related to the two professions under consideration had to be developed first. To provide an initial profession-based word set, the members of the Implicit Attitude Test–Canadian Memorial Chiropractic College (IAT-CMCC) (study authors) completed a focus group exercise. This resulted in the identification of 25 words intended to describe either chiropractic or medicine. This list of 25 words was provided to 100 individuals who were either members of a fitness facility (50 participants) or patients in one of three different rehabilitation clinics in the Greater Toronto Area (50 participants). These domains were selected in an attempt to garner representation from a wider range of a relevant population of patients who are interested in their musculoskeletal health and who interact with these professions. Each participant was asked to look at each word and determine if the word should be associated with chiropractic or medicine. Where 80% of participants agreed on an association with a particular profession, that word was accepted as a reasonable descriptor. No significant differences in word associations were found as a result of age, gender, or location (fitness facility or rehabilitation clinic). The final list of words (in no particular order) is provided in Figure 1.
Figure 1.
Words determined by preliminary study to be associated either with chiropractic or with medicine
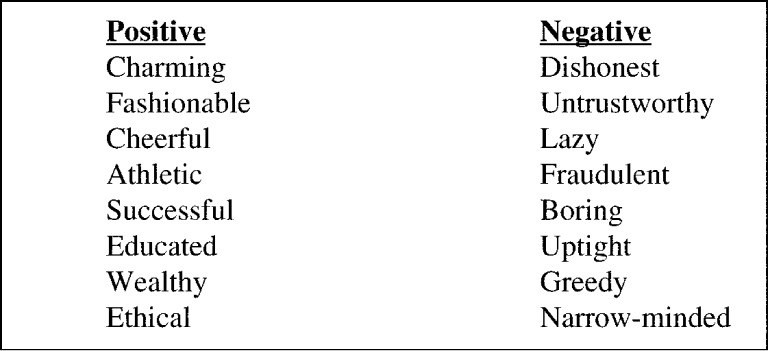
To complete the implicit association task as outlined by Greenwald and colleagues,27 an additional set of adjectives considered to be “positive” or “negative” were required. These words were selected from the list of 24 words developed by Wittenbrink et al21 for a test related to racial stereotypes. A consensus process including votes and followed by discussion and a subsequent vote was used among IAT-CMCC members to eliminate eight descriptors from the original list, yielding 16 words (8 positive and 8 negative) to match the 8 chiropractic and 8 medicine words listed in Figure 1. Finally, group consensus resulted in the elimination of three additional negative words that were relevant to the general public but less specific to negative comments made regarding the professions. These were replaced by profession-specific negative words. The word “fraudulent” was included as it appeared in association with chiropractic in four of eight articles published by the New York Times in 1976.31 The descriptor “untrustworthy” was added since the perception of fraudulent activity can be expected to breach the trust of the public. Finally, the descriptor “narrow-minded” was included based on public perception of mainstream medicine's initial view of CAM. The resultant list of positive and negative words is provided in Figure 2.
Figure 2.
Positive and negative descriptors for the word association task
Additionally, a total of 24 items were created for the explicit portion of the questionnaire. The first 10 were a request for demographic information (eg, age, gender) and the final 14 related to preferences regarding one profession over the other (eg, preference toward medicine vs. chiropractic). The explicit questionnaire was created by modifying the explicit questions utilized by Greenwald et al (https://implicit.harvard.edu/implicit/research/—originally downloaded August 2008 and rechecked March 1, 2011) and substituting chiropractic and medicine for the respective categories. These final 14 questions had Likert scales associated with each item so that the explicit statements could be scored accordingly. The participants were asked to score this series of statements by indicating on a 5-point scale on how they felt from strongly agree to strongly disagree.
Elements of the questionnaire were compiled so that explicit questions were completed first, followed by
Words describing the professions (to be categorized as medicine or chiropractic);
Positive and negative words (to be categorized as positive or negative);
All words (to be categorized as chiropractic or positive versus medicine or negative);
Words describing the professions (to be categorized as medicine or chiropractic); and
All words (to be categorized as chiropractic or negative versus medicine or positive).
Questionnaire Administration
A convenience sample was recruited from students and faculty associated with a UBMELPT program. All potential volunteers received an e-mail inviting them to participate in the study. Data collection occurred over a 2-day period. A recruitment station was set up to provide potential participants with information regarding the study. On completion of informed consent, participants were asked to register their names. This registration was not linked to their contact information but rather was used to prevent repeat enrollment of participants into the study.
The other stations were for questionnaire administration. Stations within rooms were separated by a partition to ensure privacy while the participants completed the questions and tasks. Participants were instructed to complete the explicit portion of the questionnaire first. On completion of that, a research associate provided participants with a hand-held stopwatch, which was used to record the times taken to complete the implicit tasks. The stopwatch had the time display covered to prevent awareness of time required to complete each of the implicit questionnaire tasks.
Once trained on the stopwatch, participants were provided with the first implicit task and instructed to start the timer when they were ready to begin the task and to stop the timer once they had completed the entire task. Participants were required to start and stop the timers to ensure that task times were accurately related to participant completion times. On completion of each task, the research associate assigned to the station retrieved both the stopwatch and implicit test responses. The participant was then provided with the subsequent task along with a new stopwatch and given the same instructions as with the previous task. While the participant was conducting the subsequent task, the research associate recorded the time on the stopwatch on the data collection sheet. This process was repeated until all five implicit tasks were complete. The participants were then escorted to a debriefing room where further information regarding the IAT was provided along with a complimentary lunch.
The questionnaire was arranged so that the first task primed participants to words that were determined to be related to chiropractic versus medicine. The second task primed participants to words that would be considered positive in contrast to words that would be considered negative. The third task assessed the time taken to categorize a word when the chiropractic profession was paired with positive terms and the medical profession was paired with negative terms. The fourth task was used as a washout period during which participants were asked again to categorize words as either chiropractic or medicine. The final task assessed the time taken to categorize a word when the chiropractic profession was paired with negative terms and the medical profession was paired with positive terms. Time to complete each task was recorded to the closest second. However, only the times recorded in tasks three and five were used to evaluate implicit attitudes toward the chiropractic profession.
Analysis
Implicit attitudes were demonstrated by measuring the categorization response time when chiropractic was paired with positive terms compared with negative terms. The total averages of times for each task were compared to estimate the implicit bias toward chiropractic. With time being the primary measure of implicit attitude, the difference between the two groups could be interpreted to either reflect attitudes toward or against either group. The interests of this study were explicitly related to chiropractic and, therefore, the results are reported from the viewpoint of this profession. Less time taken to categorize words when chiropractic was paired with negative as compared to the time to categorize words when chiropractic was paired with positive was taken as an implicit bias against chiropractic.27
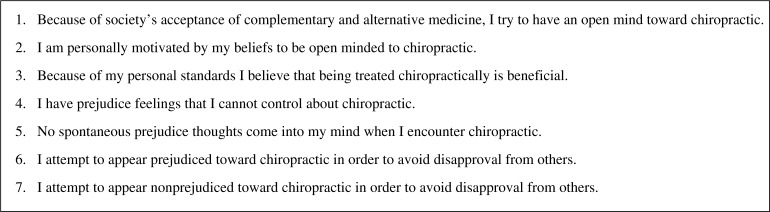
A series of items in the initial set of explicit statements was identified as pertaining directly to the notion of being “prejudiced” toward the chiropractic profession. These items were grouped together and formed the basis of the score for the explicit attitude portion of the study. Figure 3 provides a list of those statements.
Figure 3.
Statements indicating bias
Each statement that was scored by the participants from strongly agree to strongly disagree was converted to a Likert scale so that a score of 1 would be associated with being strongly in favor of chiropractic and a score of 5 was associated with being strongly against chiropractic. Antagonistic statements were inverted to maintain this association. The seven items were then added together and the average was taken as a measurement of the level of explicit prejudice against the profession. In order to determine the explicit bias, a percentage was determined from the total score out of 35 (5×7).
Descriptive statistics were used to provide an understanding of both the explicit and implicit attitudes of the respondents evaluated using the questionnaire. A paired t test was used to assess the time differences between the third and fifth task in order to examine for bias related to implicit attitude. A Pearson's correlation coefficient was used to examine the strength of the relationship between the time difference score in the implicit attitude portion of the questionnaire versus the total score for the explicit attitude portion of the study. Differences were deemed statistically significant at p≤ .05.
Results
A total of 49 participants volunteered to participate in this study. Their demographic profile is provided (Table 1). The majority of participants in the sample were female, with a mean age of 29 years.
Table 1.
Participant demographics
| Gender | Male = 13 |
| Female = 36 | |
| Age (yrs) | 29 (21–62) |
| Year of study | 1st = 42% |
| 2nd = 31% | |
| Masters in PT = 6.25% | |
| Professor of PT = 20.5% | |
| Treated | Yes = 29% |
| chiropractically | No = 71% |
The majority of individuals who participated (73%) were either in their 1st or 2nd year of the 2-year UBMELPT program. Relatively few (29%) reported having any previous experience with chiropractic care.
Results from initial questions regarding participant preferences either toward medicine or chiropractic are provided (Table 2). As illustrated in Table 2, participants in this investigation mostly preferred medical treatment and being treated “medically.” Approximately 92% of participants indicated that they preferred medical treatment and approximately 81% indicated that they agreed with medicine.
Table 2.
Treatment preferences
| Preference | Agree (%) | Neutral (%) | Disagree (%) |
| Preferred medicine to chiropractic | 68.08 | 27.66 | 4.26 |
| Preference toward medical treatment | 91.83 | 4.08 | 4.08 |
| Preference toward being treated medically | 91.84 | 4.08 | 2.04 |
| Preference toward chiropractic treatment | 44.89 | 34.69 | 20.40 |
| Preference toward being treated chiropractically | 36.73 | 22.45 | 40.81 |
| Agrees with chiropractic | 31.25 | 54.17 | 14.58 |
| Agrees with medicine | 81.25 | 16.67 | 2.08 |
A total of 48 of the 49 participants completed all of the questions relative to the explicit prejudice against chiropractic. Mean (± standard deviation) score for the explicit bias (as per questions from Figure 3) was 53.75% (±10.66) out of a possible 100%.
In terms of implicit attitude, the average time taken to complete the categorization task when chiropractic was paired with positive terms was 100.06 (±34.04) seconds. However, mean time taken to complete the categorization task when chiropractic was paired with a negative word was only 80.42 (±17.28) seconds. The average (paired) difference between these times was 19.63 seconds. This difference was statistically significant with t = 4.75 and p =.00.
Pearson's correlation coefficient was used to determine the correlation between the explicit and implicit biases. This correlation was calculated at r = 0.13 and was not statistically significant (p =.38).
Discussion
Given the substantial health care costs and economic burden (eg, due to loss of work days, etc) related to disorders of the musculoskeletal system,25,32 it is imperative that patient-centered solutions be found to increase the efficiency and effectiveness of collaborative care. A major initiative over the past decade has been the organization of interprofessional care teams based on the notion that cooperation between providers will optimize treatment plans and reduce wasted resources.
One might expect effective collaboration to occur more readily between professionals with overlapping scopes of practice and similar philosophies of care. For example, synergies between the chiropractic and physical therapy professions would intuitively be anticipated because both professions have an interest in conservative management of musculoskeletal disorders. Unfortunately, overlapping jurisdictions have also been associated with “turf wars” mitigating these synergies and resulting in barriers to collaboration.10 This study focused on understanding the attitudinal factors that may influence communication and foster patient care in the student population of one of these two professions.
It was hypothesized that, despite the general notion that CAM is popular in today's society, implicit attitudes regarding chiropractic may still reflect a negative bias that could hamper interprofessional relations. Results of the current study suggest that indeed there was a strong sentiment in favor of medical treatment. However, the average score for an explicit prejudice to chiropractic was only 53%. This 53% would be considered relatively “neutral” rather than explicitly prejudiced or explicitly accepting.
When implicit attitudes were tested, it was clear that a strong negative implicit bias existed with respect to the chiropractic profession. That is, the word association task took statistically significantly longer to complete when “chiropractic” was paired together with “positive” terms than when “chiropractic” was paired together with “negative” terms. As mentioned in the analysis section, this is interpreted from the viewpoint of the chiropractic profession and could of course also be considered as a strong positive implicit bias in favor of medicine.
Of interest, there was no statistically significant correlation between the implicit bias identified and the score related to explicit prejudice. This suggests that the implicit attitudes toward the chiropractic profession may be independent of the explicit attitudes elicited.
The neutrality of the explicit responses toward the chiropractic profession may be explained by societal pressures to suppress overt prejudice and increased emphasis on interprofessional education in the training of future health care providers.15 However, if the negative implicit attitudes are not addressed, the likelihood of achieving open communication and effective collaboration between physical therapists and chiropractors in clinical practice may be compromised.
To our knowledge, this is the first attempt to quantitatively understand and delineate explicit versus implicit attitudes of health care profession students who will share an overlapping scope of practice with chiropractic. It appears that, despite greater public acceptance of CAM, there remain differences between explicit and implicit attitudes among health care professional students. As interprofessional education and care move forward, emphasis should be placed on addressing implicit attitudes, particularly for professionals who share common skill sets and scopes of practice.15 In an effort to understand the impact of such education initiatives, it is suggested that the implicit attitude test be utilized to gauge the evolution of interprofessional synergy.
There are a number of limitations to this investigation. First, despite the preliminary work in questionnaire development, no reliability studies have been conducted on this particular variation of the implicit attitude test. As such, further research is needed to determine the stability of the results. Second, because the format of this questionnaire was paper and pencil rather than computer based, the times recorded are likely to be more variable. Given that the differences in time were statistically significantly different, however, this additional variability was considered to be within acceptable limits. Third, the implicit questionnaires were ordered so that task three associated chiropractic with negative and task five associated chiropractic with positive. This order could have potentially allowed participants to perform faster during the final tasks due to familiarity with the tasks and not due to an implicit bias. Again, however, the substantial difference in tasks would suggest that the direction of difference is accurate. Fourth, although the IAT-CMCC working group associated with this project included both physical therapy and chiropractic members, the development of the questionnaire may have benefited from a broader group of health care providers. Finally, the sample size for this investigation is rather small and consists mainly of students in a UBMELPT program. In addition, the sample originated only from one school in the Southern Ontario region. The results of this investigation may well have been different if the study had taken place among physical therapists practicing in an interdisciplinary environment with chiropractors, or in a different educational or geographical domain. Further study in this regard is recommended.
Conclusion
The results of this pilot study suggest that, while relatively little explicit prejudice was identified, individuals associated with a UBMELPT program appear to have a significant negative implicit bias toward the chiropractic profession. More research is needed to thoroughly understand the relationships between implicit and explicit attitudes and their prevalence among other educational institutions and professions as well as how these may affect collaborative practice. With the impetus toward interprofessional patient-centered care, it is suggested that more work be conducted to foster the already existing synergies between the chiropractic and physical therapy professions, especially in the related educational institutions.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Contributor Information
Chadwick L. R. Chung, Canadian Memorial Chiropractic College.
Jasmin Manga, Private Practice.
Marion McGregor, Canadian Memorial Chiropractic College.
Christos Michailidis, Private Practice.
Demetrios Stavros, Private Practice.
Linda J. Woodhouse, University of Alberta.
References
- 1.Bell C, Dunston R, Fitzgerald T, et al. Sydney, Australia: University of Sydney and University of Technology, Sydney; 2009. Interprofessional health education in Australia: the way forward. [Google Scholar]
- 2.Hawk C, Buckwalter K, Byrd L, Cigelman S, Dorfman L, Ferguson K. Health professions students’ perceptions of interprofessional relationships. Acad Med. 2002;77(4):354–7. doi: 10.1097/00001888-200204000-00020. [DOI] [PubMed] [Google Scholar]
- 3.Hall P. Interprofessional teamwork: professional cultures as barriers. J Interprof Care. 2005;19(suppl 1):188–96. doi: 10.1080/13561820500081745. [DOI] [PubMed] [Google Scholar]
- 4.Lewitt MS, Ehrenborg E, Scheja M, Brauner A. Stereotyping at the undergraduate level revealed during interprofessional learning between future doctors and biomedical scientists. J Interprof Care. 2010;24(1):53–62. doi: 10.3109/13561820902921704. [DOI] [PubMed] [Google Scholar]
- 5.Hiscock J, Pearson M. Looking inwards, looking outwards: dismantling the Berlin wall between health and social service. Soc Policy Adm. 1999;(33):150–63. [Google Scholar]
- 6.Axelsson SB, Axelsson R. From territoriality to altruism in interprofessional collaboration and leadership. J Interprof Care. 2009;23(4):320–30. doi: 10.1080/13561820902921811. [DOI] [PubMed] [Google Scholar]
- 7.Cullen L, Fraser D, Symonds I. Strategies for interprofessional education: the Interprofessional Team Objective Structured Clinical Examination for midwifery and medical students. Nurse Educ Today. 2003;23(6):427–33. doi: 10.1016/s0260-6917(03)00049-2. [DOI] [PubMed] [Google Scholar]
- 8.Reeves S, Freeth D. The London training ward: an innovative interprofessional learning initiative. J Interprof Care. 2002;16(1):41–52. doi: 10.1080/13561820220104159. [DOI] [PubMed] [Google Scholar]
- 9.Wee B, Hillier R, Coles C, Mountford B, Sheldon F, Turner P. Palliative care: a suitable setting for undergraduate interprofessional education. Palliat Med. 2001;15(6):487–92. doi: 10.1191/026921601682553978. [DOI] [PubMed] [Google Scholar]
- 10.Bate P. Changing the culture of a hospital: from hierarchy to networked community. Public Adm. 2000;78(3):485–512. [Google Scholar]
- 11.Abbott A. Chicago, IL: University of Chicago Press; 1988. The systems of professions. An essay on the division of expert labor. [Google Scholar]
- 12.Baker GR, Norton PG, Flintoft V, et al. The Canadian Adverse Events Study: the incidence of adverse events among hospital patients in Canada. Can Med Assoc J. 2004;170(11):1678–86. doi: 10.1503/cmaj.1040498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. Can Med Assoc J. 2005;173(5):510–5. doi: 10.1503/cmaj.045311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Margalit R, Thompson S, Visovsky C, et al. From professional silos to interprofessional education: campuswide focus on quality of care. Qual Manag Health Care. 2009;18(3):165–73. doi: 10.1097/QMH.0b013e3181aea20d. [DOI] [PubMed] [Google Scholar]
- 15.Blue AV, Mitcham M, Smith T, Raymond J, Greenberg R. Changing the future of health professions: embedding interprofessional education within an academic health center. Acad Med. 2010;85(8):1290–5. doi: 10.1097/ACM.0b013e3181e53e07. [DOI] [PubMed] [Google Scholar]
- 16.Curran VR, Sharpe D, Flynn K, Button P. Alongitudinal study of the effect of an interprofessional education curriculum on student satisfaction and attitudes towards interprofessional teamwork and education. J Interprof Care. 2010;24(1):41–52. doi: 10.3109/13561820903011927. [DOI] [PubMed] [Google Scholar]
- 17.Weaver L. Interprofessional education curricula models for health care providers in Ontario. Final report. Ontario, Canada: The Interprofessional Care Strategic Implementation Committee; October 22, 2009. [Google Scholar]
- 18.Morison S, Johnston J, Stevenson M. Preparing students for interprofessional practice: exploring the intra-personal dimension. . J Interprof Care. 2010;24(4):412–21. doi: 10.3109/13561820903373210. [DOI] [PubMed] [Google Scholar]
- 19.Rice K, Zwarenstein M, Conn LG, Kenaszchuk C, Russell A, Reeves S. An intervention to improve interprofessional collaboration and communications: a comparative qualitative study. J Interprof Care. 2010;24(4):350–61. doi: 10.3109/13561820903550713. [DOI] [PubMed] [Google Scholar]
- 20.Makowsky MJ, Schindel TJ, Rosenthal M, Campbell K, Tsuyuki RT, Madill HM. Collaboration between pharmacists, physicians and nurse practitioners: a qualitative investigation of working relationships in the inpatient medical setting. J Interprof Care. 2009;23(2):169–84. doi: 10.1080/13561820802602552. [DOI] [PubMed] [Google Scholar]
- 21.Wittenbrink B, Judd CM, Park B. Evidence for racial prejudice at the implicit level and its relationship with questionnaire measures. . J Pers Soc Psychol. 1997;72(2):262–74. doi: 10.1037//0022-3514.72.2.262. [DOI] [PubMed] [Google Scholar]
- 22.Devine PG. Stereotypes and prejudice: their automatic and controlled components. J Pers Soc Psychol. 1989;22:136–45. [Google Scholar]
- 23.Wilson TD, Lindsey S, Schooler TY. A model of dual attitudes. Psychol Rev. 2000;107(1):101–26. doi: 10.1037/0033-295x.107.1.101. [DOI] [PubMed] [Google Scholar]
- 24.Rydell RJ, McConnell AR. Understanding implicit and explicit attitude change: a system of reasoning analysis. J Pers Soc Psychol. 2006;91(6):995–1008. doi: 10.1037/0022-3514.91.6.995. [DOI] [PubMed] [Google Scholar]
- 25.Coyte PC, Asche CV, Croxford R, Chan B. The economic cost of musculoskeletal disorders in Canada. Arthritis Care Res. 1998;11(5):315–25. doi: 10.1002/art.1790110503. [DOI] [PubMed] [Google Scholar]
- 26.Turner BS. London: Sage; 1991. Medical power and social knowledge. [Google Scholar]
- 27.Greenwald AG, McGhee DE, Schwartz JL. Measuring individual differences in implicit cognition: the implicit association test. . J Pers Soc Psychol. 1998;74(6):1464–80. doi: 10.1037//0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- 28.Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the implicit association test. III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97(1):17–41. doi: 10.1037/a0015575. [DOI] [PubMed] [Google Scholar]
- 29.Scott WR, Ruef M, Mendel PJ, Caronna CA. Chicago, IL: University of Chicago Press; 2000. Institutional change and healthcare organizations: from professional dominance to managed care. [Google Scholar]
- 30.Winnick TA. Medical doctors and complementary and alternative medicine: the context of holistic practice. . Health (London) 2006;10(2):149–73. doi: 10.1177/1363459306061785. [DOI] [PubMed] [Google Scholar]
- 31.McGregor M. In Washington, DC: 2006. Climbing the stairs of professional credibility—the roles of discourse and knowledge. [Google Scholar]
- 32.Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81(9):646–56. [PMC free article] [PubMed] [Google Scholar]