Abstract
Purpose:
This study presents a retrospective case series of the clinical and structural outcomes (1.5 T MRI) of arthroscopic rotator cuff repair with acellular human dermal graft reinforcement performed by a single surgeon in patients with large, massive, and previously repaired rotator cuff tears.
Materials and Methods:
Fourteen patients with mean anterior to posterior tear size 3.87 ± 0.99 cm (median 4 cm, range 2.5–6 cm) were enrolled in the study and were evaluated for structural integrity using a high-field (1.5 T) MRI at an average of 16.8 months after surgery. The Constant-Murley scores, the Flexilevel Scale of Shoulder Function (Flex SF), scapular plane abduction, and strength were analyzed.
Results:
MRI results showed that the rotator cuff repair was intact in 85.7% (12/14) of the patients studied. Two patients had a Sugaya Type IV recurrent tear (2 of 14; 14.3%), which were both less than 1 cm. The Constant score increased from a preoperative mean of 49.72 (range 13–74) to a postoperative mean of 81.07 (range 45–92) (P value = 0.009). Flexilevel Scale of Shoulder Function (Flex SF) Score normalized to a 100-point scale improved from a preoperative mean of 53.69 to a postoperative mean of 79.71 (P value = 0.003). The Pain Score improved from a preoperative mean of 7.73 to a postoperative mean of 13.57 (P value = 0.008). Scapular plane abduction improved from a preoperative mean of 113.64° to a postoperative mean of 166.43° (P value = 0.010). The strength subset score improved from a preoperative mean of 1.73 kg to a postoperative mean of 7.52 kg (P value = 0.006).
Conclusions:
This study presents a safe and effective technique that may help improve the healing rates of large, massive, and revision rotator cuff tears with the use of an acellular human dermal allograft. This technique demonstrated favorable structural healing rates and statistically improved functional outcomes in the near term.
Level of Evidence:
4. Retrospective case series.
Keywords: Rotator cuff repair, shoulder arthroscopy, rotator cuff reinforcement graft, acellular human dermal graft, rotator cuff healing
INTRODUCTION
Rotator cuff tears greater than or equal to 3 cm along with previously failed or revision rotator cuff tears are considered the most challenging in achieving primary anatomic healing, with reported failure rates as high as 94%.[1–9] The strength of repair and biologic healing potential, coupled with the intrinsic limitations in the rotator cuff tendon tissue, are other potential variables responsible for these high failure rates.[3,10–21] Arthroscopic rotator cuff repair, reinforced with a graft, may offer the potential benefits of a scaffold for tissue replacement, structural support of the repair during the crucial healing period, and improved healing rates.[2,22–30] This study presents a retrospective case series of the clinical and structural outcomes (1.5 T MRI) of arthroscopic rotator cuff repair with acellular human dermal graft reinforcement performed by a single surgeon in patients with large, massive, and previously repaired rotator cuff tears.
MATERIALS AND METHODS
Patient selection
Patients diagnosed with a rotator cuff tear requiring either a primary or revision arthroscopic rotator cuff repair with reinforcement graft utilizing Allopatch HD™ Hydrated Ultra Thick (MTF Sports Medicine, Edison, NJ, USA) and who were at least 12 months from the index operation were identified through a retrospective chart review. In order to be eligible for study inclusion, the following criteria had to be met:
Rotator cuff tears greater than or equal to 3 cm.
Patients with recurrent rotator cuff tears (previously failed repair) – may be less than 3 cm.
All study patients received an arthroscopic rotator cuff repair with arthroscopic acellular human dermal graft reinforcement utilizing Allopatch HD Hydrated Ultra Thick (MTF Sports Medicine). The same surgeon using the same technique and graft material performed all surgeries. From September 2009 to February 2010, a total of 44 consecutive patients were identified for study inclusion.
44 patients: Preliminary patient pool
3 patients with bridging grafts were excluded
5 patients with active litigation or workers compensation claims were excluded.[31–33]
5 patients with concurrent subscapularis repairs were excluded
8 patients with postoperative injuries were excluded
5 patients were lost to follow-up
Of the 44 preliminary patients, 18 (40.9%) formed the final sample of patients eligible to participate in the study. Study protocol was fully approved by the Hospital Institutional Review Board and all the patients were enrolled in compliance with the protocol. Four patients (4 of 18; 22.2%) declined to participate in the study protocol. One of these four patients had an MRI at 7 months after surgery, demonstrating a fully healed (Sugaya Type I) rotator cuff repair, but did not return for a second evaluation as part of the study. Another patient with a massive revision rotator cuff repair had returned for a 1-year clinical follow-up visit (Constant-Murley Score 82, Flex SF 100, strength 8.16 kg), but due to metallic implants from previous shoulder surgery, did not want to proceed with a computed tomography (CT) arthrogram and elected to not participate. Two other patients chose not to participate in the study. Ten patients were males (71.4%) and four patients were females (28.6%), with an overall average age of 54.6 years (standard deviation 6.54) at the time of surgery (range 47–69). One patient had a 2.5 cm tear at surgery and was included for study because of a previously failed rotator cuff repair. Ten patients had large tears (3–5 cm) and three patients had massive tears (>5 cm). The tear was determined intraoperatively under direct arthroscopic visualization after debridement of the degenerated tendon edges. The size of the rotator cuff tear was measured in the greatest anterior–posterior dimension using a calibrated probe.[34]
Clinical outcome measures
All patients underwent a detailed workup and received appropriate conservative management prior to choosing arthroscopic treatment. Standardized and validated outcome measures for shoulder function, the Constant-Murley Score,[35] and Flexilevel Scale of Shoulder Function (Flex SF) Score[36,37] for each patient were collected preoperatively and at the clinic follow-up visit at 1 year. For ease of comparison, the Flex SF Score was normalized to a 100-point maximum scale. A postoperative visual analog scale (VAS) which asked patients to rate their shoulder function on a scale of 1–100 (100 being the best possible function) was administered at least 1 year post surgery.[38] One nurse performed the manual muscle strength portion of the Constant-Murley Score using a standardized position of abduction to 90° in the scapular plane and a calibrated portable digital dynamometer (Ametek Inc., Chatillon FCE-200, Largo, FL, USA). Co-morbid conditions and other relevant covariates such as patient age, smoking status, diabetes mellitus, the size of rotator cuff tears, and compliance with rehabilitation protocols were also collected.[14,19,39–45]
Operative technique
All surgeries were performed in the modified lateral decubitus position with balanced suspension (5–10 pounds) under general anesthesia with a preoperative brachial plexus catheter placed with ultrasound. All other shoulder pathologies were evaluated and treated prior to proceeding with the rotator cuff repair. One patient had a hereditary motor and sensory neuropathy 1a (Charcot–Marie–Tooth disease).[46] This patient and another study patient also had an ossified superior transverse scapular ligament (Bony SSN) that was decompressed.[47] Other procedures performed at the same time as the rotator cuff repair are presented in Table 1. After appropriate visualization and preparation of the rotator cuff tear, the size and pattern of the rotator cuff tear was determined. All the patients in the study had the same technique of arthroscopic rotator cuff repair: a dual row tension band repair with acellular human dermal graft reinforcement. The dual row portion of the repair started with a suture anchor at the medial aspect of the rotator cuff footprint at the anterior and posterior margins of the rotator cuff tear. A single suture pair was used from the medial row anchors and the second suture removed after anchor placement. The correct pattern of the rotator cuff tear was determined in order to restore equalized tension in the entire rotator cuff. Once the correct pattern was determined, the medial row sutures were passed through the appropriate area of the medial rotator cuff tendon. These sutures were retrieved via an accessory portal and saved for the graft reinforcement. The tension band technique was performed with dual loaded suture anchors placed distal to the rotator cuff footprint at the proximal lateral cortex of the humerus.[48] Based on the pattern of the tear, side-to-side sutures were passed and tied to achieve restoration of the rotator cuff footprint. Sutures were passed through the rotator cuff tendon with a Spectrum™ suture hook device (Linvatec CONMED, Utica, NY, USA). A PDS™ II (polydioxanone) suture (Ethicon, Somerville, NJ, USA) was utilized as a suture shuttle to allow placement of a permanent braided suture for side-to-side repairs – Orthocord™ Suture (DePuy Mitek, Raynham, MA, USA) or MaxBraid™ PE Suture (Biomet, Warsaw, IN, USA). Dual loaded suture anchors used for the study were either ALLthread™ LactoSorb L15 5.5 mm and 6.8 mm Suture Anchors (Biomet) or the Healix™ BR 4.5 mm and 5.5 mm Suture Anchors (DePuy Mitek). Each suture was placed and tied sequentially. All sutures were placed in a simple single passage configuration with the suture passed medially through the rotator cuff tendon, typically at least 10–15 mm from the lateral edge of the tendon. Additional suture anchors were placed at the proximal lateral cortex of the humerus to achieve complete repair [Figure 1]. Planning for the reinforcement graft, one pair of sutures was preserved from the lateral row of anchors at the very anterior and posterior corners of the tear. Allopatch HD Ultra Thick (1.8–3.9 mm) is an acellular human dermis graft (MTF Sports Medicine) that is packaged in alcohol and stored at ambient temperature. The 5 × 5 cm size was selected and prepared for implantation based on manufacturer's recommendations. The dimensions between each set of corner sutures from the medial and lateral row were measured with the graduated probe and transferred to the Allopatch HD graft on the back table. After trimming the graft to the appropriate dimensions, a single limb of the anterior and posterior lateral row sutures was retrieved through a single lateral cannula. Care was taken to keep the suture limbs parallel, while the remaining lateral limbs of suture were retrieved via another cannula to provide counter-traction. The anterior-lateral and posterior-lateral sutures were passed through the corresponding points of the Allopatch HD graft and with tension on both ends of the suture limbs. An arthroscopic grasper was used to push the medial limb of the graft first through the cannula, using the suture limbs as rails. Each corresponding pair of sutures was now retrieved and tied, resulting in stabilization and compression of the lateral edge of the graft beyond the lateral edge of the rotator cuff footprint. An arthroscopic grasper was used to provisionally tension the medial corners of the graft in order to determine the best location to pass the corresponding medial row sutures. One limb of each of the posterior medial and anterior medial sutures was shuttled through the graft using a Spectrum suture hook device (Linvatec CONMED) and PDS II (polydioxanone) suture (Ethicon). Each suture was then tied, creating tension in the Allopatch HD graft, while also compressing the entire rotator cuff footprint [Figure 2]. Additional tendon to graft sutures were passed to provide uniform draping and tension to the entire construct. Following routine closure of the portals with simple sutures, the patient was placed in an abductor pillow immobilizer (Shoulder Abduction Pillow, BREG, Vista, CA, USA).
Table 1.
Concurrent procedures performed in addition to the rotator cuff repair
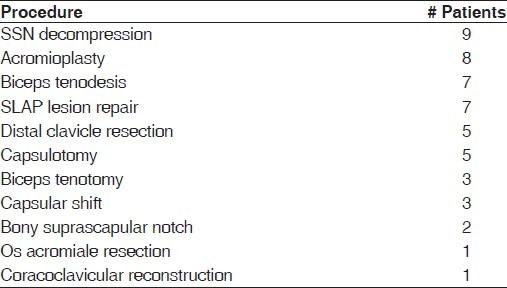
Figure 1.
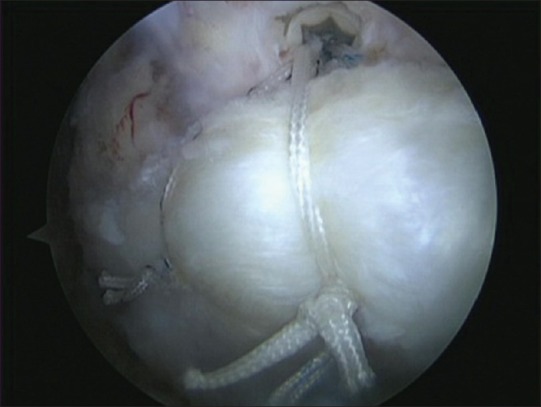
Tension band rotator cuff repair: Anchor placed distal to rotator cuff footprint
Figure 2.
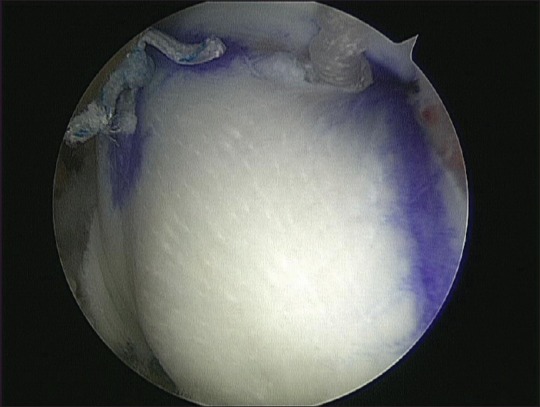
Completed rotator cuff repair with reinforcement Allopatch HD graft (MTF Sports Medicine, Edison, NJ, USA)
Postoperative rehabilitation
All patients participated in the same postoperative rehabilitation program. The Abduction Pillow was worn full time except for hand and elbow range-of-motion, and pendulum exercise 1 month following surgery. After the Abduction Pillow was discontinued, supine passive and active assisted exercises were initiated to restore range of motion at 1 month following surgery. Patients were advised not to try and actively lift the arm when upright until 3 months after surgery. Active supine range of motion exercises were started at 8 weeks following surgery, along with gradual muscle and functional strengthening exercises 12 weeks following surgery. Thereafter, activities were increased gradually as tolerated with a return to heavy manual labor delayed until 6 months following surgery.
Assessment of tendon healing
Anatomic assessment of tendon healing was performed with an MRI utilizing the grading scale described by Sugaya,[49,50] rotator cuff fatty infiltration using the Goutallier classification by Fuchs,[51] and significant clinical atrophy as per the tangent sign described by Zanetti.[52] All sequences were performed on a 1.5 T high-field scanner (Signa; GE Medical Systems, Milwaukee, WI, USA). Gradient-echo axial, proton density and T2-weighted oblique coronal and sagittal, and coronal fat-suppressed imaging of the shoulder was performed utilizing a dedicated shoulder coil. Sagittal T1 series were also obtained.
Two musculoskeletal fellowship trained radiologists, who were aware that the patients had undergone surgery for rotator cuff repair but were blinded to the size and location of the tear that had been repaired, reviewed the images. Postoperative MRIs were performed between 1 and 2 years following surgery, with an average time after surgery of 16.8 months (standard deviation: 1.67).
Statistical analysis
Pre-and post-surgical scores were compared using nonparametric Wilcoxon Signed Rank tests.
RESULTS
MRI results showed that the rotator cuff repair was structurally intact in 85.7% (12) of the 14 patients studied. These 12 patients included 9 Type I, sufficient thickness with homogenously low intensity (9 of 14; 64.2%), 2 Type II, sufficient thickness with partial high intensity (2 of 14; 14.3%), and 1 Type III, insufficient thickness without discontinuity (thinned cuff) (1 of 14; 7%) repairs. Two patients had a Type IV, presence of minor discontinuity, recurrent tear (2 of 14; 14.3%), which were both much smaller than their tears at surgery – less than 1 cm [Figure 3a–d]. There were no Type V, presence of a major discontinuity, recurrent tears. Further examination of the two patients with Type IV discontinuity revealed that one had a recurrent minor defect at the medial musculotendinous junction [Figure 4], while the other had a recurrent minor defect at the posterior aspect of the rotator cuff footprint. Of the 10 patients with large (3–5 cm) tears, 9 (90%) had intact repairs per MRI. Of the three patients with massive (>5 cm) tears, 2 (66.7%) had intact repairs per MRI. Our study population did not have any patient with advanced (Stage 3 or 4) fatty infiltration scores, but there were three patients with a positive tangent sign, consistent with clinically significant atrophy.[52] Two of the three patients with a positive tangent sign had a Sugaya Type IV tear, while the third patient had a Sugaya Type II repaired tendon [Table 2].
Figure 3.
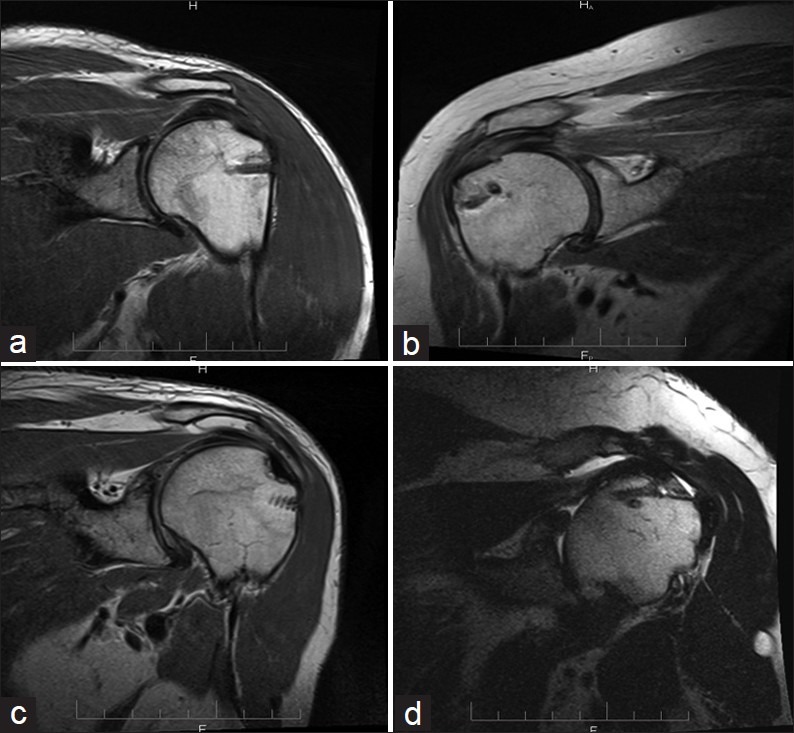
(a) Sugaya Type I, sufficient thickness with homogenously low intensity; (b) Sugaya Type II, sufficient thickness with partial high intensity; (c) Sugaya Type III, insufficient thickness without discontinuity (thinned cuff); (d) Sugaya Type IV, presence of minor discontinuity
Figure 4.
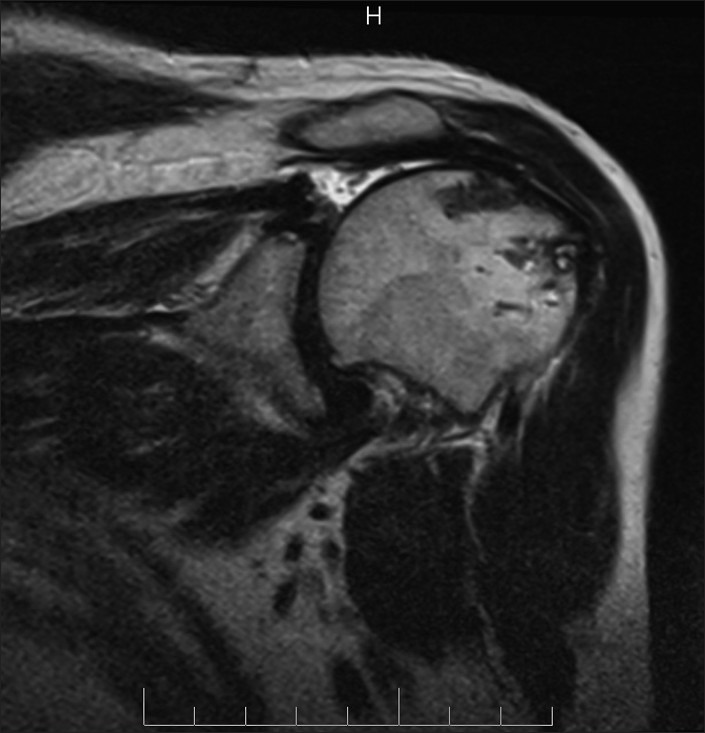
Sugaya Type IV, recurrent minor defect (less than 1 cm) at the medial musculotendinous junction
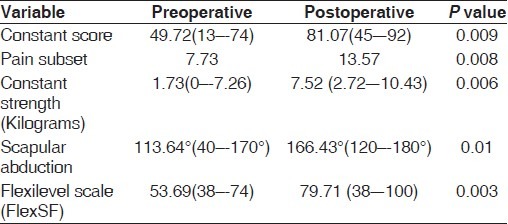
Table 2.
Rotator cuff integrity per MRI using the sugaya grading scale
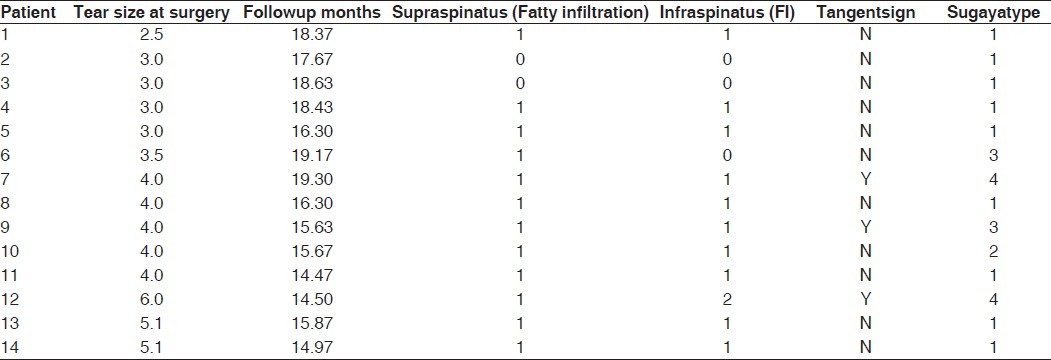
Assessment of functional outcome
The Constant-Murley Score increased from a preoperative mean of 49.72 (range 13–74) to a postoperative mean of 81.07 (range 45–92) (P value = 0.009). The Pain Score improved from a preoperative mean of 7.73 to a postoperative mean of 13.57 (P value = 0.008). Scapular plane abduction improved from a preoperative mean of 113.64° to a postoperative mean of 166.43° (P value = 0.010). The strength subset score improved from a preoperative mean of 1.73 kg to a postoperative mean of 7.52 kg (P value = 0.006). Flexilevel Scale of Shoulder Function (Flex SF) Score[36,37] normalized to a 100-point scale improved from a preoperative mean of 53.69 to a postoperative mean of 79.71 (P value = 0.003) [Table 3]. Both the patients with Sugaya Type IV tears, minor discontinuity, had excellent functional outcomes including postoperative strength values of 8.16 and 9.53 kg, respectively. Only one patient had lower strength and functional outcome scores following treatment. The patient with a 2.5 cm revision rotator cuff tear had multiple medical co-morbidities, and despite having a Sugaya Type I healed repair per MRI, had a poor functional outcome.
Table 3.
Functional outcomes
Subjective outcome
All study patients completed a questionnaire that asked them to rate their satisfaction and function with their shoulder repair on a scale of 0–100. The mean response to this question was 88.64 (standard deviation 19.37, range 30–100, median 96.5, mode 100).
Complications
There were no intraoperative or postoperative complications. No patients had neural injury, wound infection, or suture anchor problems. No graft-related complications were seen. We had the opportunity to take biopsies of a previously placed Allopatch HD graft for one of the patients excluded from the present study because of postoperative injury resulting in recurrent tear, and with his full consent, specimens were taken at revision arthroscopy, 4 months following the index procedure, from the edge and central portions of the graft and submitted for detailed histological evaluation. The specimens were prepared with toluidine blue, Masson's trichrome, and elastin stains, along with hematoxylin and eosin stains. The central portion of the biopsy specimen showed two-third acellular human graft material surrounded by a rim of proliferating fibroblastic tissue. The peripheral biopsy specimen showed orderly fibrotendinous connective tissue with mild neovascularization. There was no evidence of foreign body giant cell reaction or inflammation in both areas [Figure 5a, b].[53]
Figure 5.
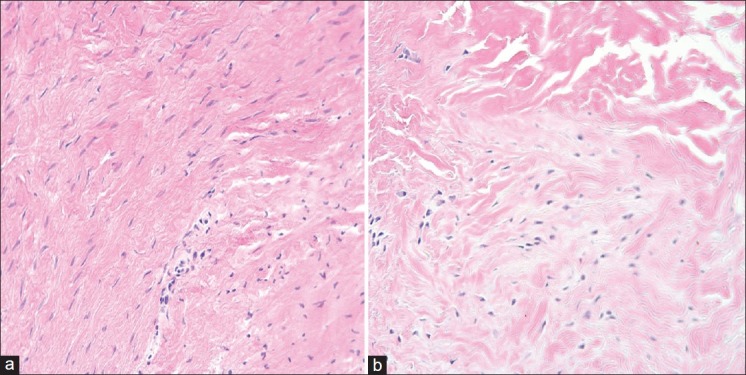
(a) Hematoxylin and eosin stain peripheral graft biopsy (20×). (b) Hematoxylin and eosin stain central graft biopsy (20×)
DISCUSSION
The process of tendon healing to bone occurs slowly, only achieving approximately one-third the ultimate load to failure of a normal tendon attachment at 12 weeks in a goat model.[54,55] Rotator cuff repair, reinforced with a graft, may offer the potential benefits of a scaffold for tissue replacement, structural support of the repair during the crucial healing period, and improved healing rates.[2,22–30]
Using an arthroscopic single row technique, Meyer et al. recently reported that 88% (15/17) of rotator cuff repairs evaluated by MR arthrography had either a small or large recurrent defect with no patients having a normal appearing footprint. The mean preoperative anterior posterior tear size was 1.73 ± 0.52 cm.[56] Utilizing variable arthroscopic repair techniques based on tendon mobility and quality, but voicing a preference for the suture bridge technique, Kowalsky et al. evaluated the structural integrity results in revision rotator cuff repair with ultrasound and reported that 10 (48%) of the 21 shoulders studied had an intact repair. Seven (70%) of the 10 single-tendon repairs were intact, compared with 3 (27%) of the 11 supraspinatus/infraspinatus repairs (P = 0.05).[57] Using an arthroscopic double-row suture bridge technique, Cho et al. recently analyzed their structural results using MRI and reported complete healing in 7 (100%) of 7 small tears, in 32 (78.0%) of 41 medium tears, in 16 (50.0%) of 32 large tears, and in 3 (42.9%) of 7 massive tears.[58] Using an arthroscopic dual row transosseous equivalent technique, Toussaint et al. in a recent multicenter study reviewed their structural results with either CT arthrogram or MR arthrogram and reported that 79% (37 of 47) of the small, 63% (55 of 88) of the large, and 63% (12 of 19) of the massive tears were intact, when grading only “watertight” repairs as intact.[59] Using an arthroscopic double-row rotator cuff repair technique, Tashjian et al. also recently reviewed their structural results with ultrasound evaluation and reported that of 49 repairs, 25 (51%) were healed. Healing rates were 67% in single-tendon tears (16 of 24 shoulders) and 36% in multi-tendon tears (9 of 25 shoulders). They concluded, “… in a large percentage of patients, failure of rotator cuff healing is likely due to patient related or biological factors. Future improvements in rotator cuff repairs will need to focus on biological improvements to aid in tendon healing, given that mechanical improvements may have been maximized.”[60] Duquin et al. performed a systematic analysis of structural integrity, regardless of surgical approach (open or arthroscopic), comparing single-row repairs with double-row repairs and found 476 tears that could be characterized as involving two or more tendons or being greater than 3 cm. The recurrent tear rate was 45% for the single-row methods and 26% for double-row methods.[61] The structural healing rate [85.7% (12/14)] or recurrent tear rate [14.3% (2/14)] in this study compares favorably with the overall healing rates reported in the literature.[61,62] The mean anterior to posterior tear size in this study was 3.86 ± 0.97 cm (median 4 cm, range 2.5–6 cm).
Although there has been much debate regarding the relationship of functional outcomes to structural outcomes, most studies that evaluate the strength subset of functional outcomes do report better results in patients with intact rotator cuff repairs.[62] Longer-term follow-up of patients with recurrent rotator cuff tears seems to indicate that strength continues to decrease with time and the size of tear continues to increase.[63,64]
This study found a statistically significant improvement in the postoperative Constant-Murley Score, the Flex SF Score, the Pain Score, the range-of-motion as measured by scapular plane abduction, and the strength score. The functional outcomes for this study were not significantly different for patients with healed tears compared to the ones with recurrent defects. This may be reflective of the relatively small (less than 1 cm) recurrent defects (Sugaya Type IV) for both patients and that the study population did not have any Sugaya Type V tears, showing the presence of a major discontinuity, similar to the prospective study evaluating structural and functional outcomes for dual row rotator cuff repairs, where Sugaya et al. reported that only the patients with Type V defects had significantly inferior functional and strength results.[50] Also, the small population of patients with a recurrent defect and relatively high rate of structural integrity make meaningful statistical evaluation of the effect of confounding variables such as medical co-morbidity, fatty infiltration, atrophy, and concurrent surgical procedures performed inconclusively.
There are many extracellular matrix scaffold devices available with varying histological, biologic, and mechanical properties,[24] and many factors should be considered when choosing a reinforcement patch, including tissue origin, graft processing, cross-linking, clinical experience, and physical properties.[24,65] Only a few clinical human studies are available to demonstrate histological behavior, clinical behavior, and outcomes for rotator cuff repair reinforced with an extracellular matrix scaffold, with no single study to date evaluating all three.[2,24,30,53,65–68] To our knowledge, this is the first study to demonstrate favorable structural healing rates, statistically significant improvement in functional outcomes, and a histological retrieval analysis utilizing an entirely arthroscopic technique for rotator cuff repair reinforced with an acellular human dermal matrix graft (Allopatch HD, MTF Sports Medicine).
Although few data are available on the functional and economic costs associated with failed rotator cuff repairs, rotator cuff repair has been shown to have an efficacy on par with other elective orthopedic procedures such as hip and knee replacement.[69] Higher cost and prolonged surgery time are among the possible concerns regarding application of an acellular dermal reinforcement graft (Allopatch HD, MTF Sports Medicine).[2] Arthroscopic graft reinforcement is a challenging technique with a steep learning curve. Currently, after significant experience and a technique that has also evolved with our progression along the learning curve, arthroscopic graft reinforcement typically requires 15 additional minutes of surgery time for our team. However, we believe that if we can provide better structural and functional outcomes for challenging rotator cuff tears, the slightly higher initial cost and surgery time will translate into significant long-term cost savings.
The strengths of this study include the use of a single technique, the availability of histological analysis at 4 months following implantation, and the use of a validated technique to assess structural rotator cuff integrity – high-field MRI (1.5 T).[53,70–75] While MRI, ultrasound, and arthrography with either CT or MRI have all been evaluated, in our setting, arthrography presented the challenge of asking an asymptomatic patient to undertake an invasive test and ultrasound was much more operator dependent.[7,76–80] Weaknesses of this study were the relatively small sample size of the study, the retrospective study design, and the relatively short-term follow-up. Jost et al., in a long-term structural and functional outcome study of 20 patients with recurrent tears at an average 7.6 years after surgery, found that recurrent tears smaller than 400 mm2 had the potential to heal with scar tissue.[81] In contrast, Dodson et al., in a structural and functional outcome study with 11 patients (13 shoulders) at an average of 7.9 years after surgery, found that there was a statistically significant increase in the mean size of the defect from 273 mm2 to 467 mm2 (P < 0.001) and patients did have significant progressive strength loss. Also, the size of the defect increased in all patients and no defects healed structurally.[63] Both the patients with a recurrent tear in the present study had recurrent defects less than 100 mm2 at early clinical follow-up and did not differ from the healed group with regard to strength or function. Compared to the postoperative strength subset score mean of 7.52 kg for the entire group, the two patients with recurrent minor defects had strength subset scores of 8.16 and 9.53 kg, respectively. Only longer follow-up will help define the behavior, remodeling characteristics, structural and clinical performance of Allopatch HD in this and other patient groups.
CONCLUSIONS
In conclusion, this study presents a safe and effective technique that may help improve the healing rates of large, massive, and revision rotator cuff tears with the use of an acellular human dermal allograft. This technique demonstrated favorable structural healing rates and statistically improved functional outcomes in the near term. Based on the favorable healing rates in this retrospective study, a prospective randomized study with a larger pool of patients and longer follow-up is planned for greater validation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86:219–24. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Wong I, Burns J, Snyder S. Arthroscopic Graft Jacket repair of rotator cuff tears. J Shoulder Elbow Surg. 2010;19:104–9. doi: 10.1016/j.jse.2009.12.017. [DOI] [PubMed] [Google Scholar]
- 3.Oh JH, Kim SH, Ji HM, Jo KH, Bin SW, Gong HS. Prognostic factors affecting anatomic outcome of rotator cuff repair and correlation with functional outcome. Arthroscopy. 2009;25:30–9. doi: 10.1016/j.arthro.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 4.Shen PH, Lien SB, Shen HC, Lee CH, Wu SS, Lin LC. Long-term functional outcomes after repair of rotator cuff tears correlated with atrophy of the supraspinatus muscles on magnetic resonance images. J Shoulder Elbow Surg. 2008;17:1S–7S. doi: 10.1016/j.jse.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 5.Burkhart SS, Barth JR, Richards DP, Zlatkin MB, Larsen M. Arthroscopic repair of massive rotator cuff tears with stage 3 and 4 fatty degeneration. Arthroscopy. 2007;23:347–54. doi: 10.1016/j.arthro.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 6.Mellado JM, Calmet J, Olona M, Ballabriga J, Camins A, Pérez del Palomar L, et al. MR assessment of the repaired rotator cuff: prevalence, size, location, and clinical relevance of tendon rerupture. Eur Radiol. 2006;16:2186–96. doi: 10.1007/s00330-006-0147-z. [DOI] [PubMed] [Google Scholar]
- 7.Mellado JM, Calmet J, Olona M, Esteve C, Camins A, Pérez Del Palomar L, et al. Surgically repaired massive rotator cuff tears: MRI of tendon integrity, muscle fatty degeneration, and muscle atrophy correlated with intraoperative and clinical findings. AJR Am J Roentgenol. 2005;184:1456–63. doi: 10.2214/ajr.184.5.01841456. [DOI] [PubMed] [Google Scholar]
- 8.Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007;35:719–28. doi: 10.1177/0363546506297539. [DOI] [PubMed] [Google Scholar]
- 9.Djurasovic M, Marra G, Arroyo JS, Pollock RG, Flatow EL, Bigliani LU. Revision rotator cuff repair: factors influencing results. J Bone Joint Surg Am. 2001;83:1849–55. doi: 10.2106/00004623-200112000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Rowshan K, Hadley S, Pham K, Caiozzo V, Lee TQ, Gupta R. Development of fatty atrophy after neurologic and rotator cuff injuries in an animal model of rotator cuff pathology. J Bone Joint Surg Am. 2010;92:2270–8. doi: 10.2106/JBJS.I.00812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oh JH, Kim SH, Kang JY, Oh CH, Gong HS. Effect of age on functional and structural outcome after rotator cuff repair. Am J Sports Med. 2010;38:672–8. doi: 10.1177/0363546509352460. [DOI] [PubMed] [Google Scholar]
- 12.Melis B, DeFranco MJ, Chuinard C, Walch G. Natural history of fatty infiltration and atrophy of the supraspinatus muscle in rotator cuff tears. Clin Orthop Relat Res. 2010;468:1498–505. doi: 10.1007/s11999-009-1207-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bedi A, Fox AJ, Harris PE, Deng XH, Ying L, Warren RF, et al. Diabetes mellitus impairs tendon-bone healing after rotator cuff repair. J Shoulder Elbow Surg. 2010;19:978–88. doi: 10.1016/j.jse.2009.11.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sherman SL, Lyman S, Koulouvaris P, Willis A, Marx RG. Risk factors for readmission and revision surgery following rotator cuff repair. Clin Orthop Relat Res. 2008;466:608–13. doi: 10.1007/s11999-008-0116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gimbel JA, Van Kleunen JP, Lake SP, Williams GR, Soslowsky LJ. The role of repair tension on tendon to bone healing in an animal model of chronic rotator cuff tears. J Biomech. 2007;40:561–8. doi: 10.1016/j.jbiomech.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 16.Matthews TJ, Hand GC, Rees JL, Athanasou NA, Carr AJ. Pathology of the torn rotator cuff tendon.Reduction in potential for repair as tear size increases. J Bone Joint Surg Br. 2006;88:489–95. doi: 10.1302/0301-620X.88B4.16845. [DOI] [PubMed] [Google Scholar]
- 17.Rubino LJ, Sprott DC, Stills HF, Jr, Crosby LA. Fatty infiltration does not progress after rotator cuff repair in a rabbit model. Arthroscopy. 2008;24:936–40. doi: 10.1016/j.arthro.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 18.Gerber C, Schneeberger AG, Hoppeler H, Meyer DC. Correlation of atrophy and fatty infiltration on strength and integrity of rotator cuff repairs: A study in thirteen patients. J Shoulder Elbow Surg. 2007;16:691–6. doi: 10.1016/j.jse.2007.02.122. [DOI] [PubMed] [Google Scholar]
- 19.Tashjian RZ, Henn RF, Kang L, Green A. Effect of medical comorbidity on self-assessed pain, function, and general health status after rotator cuff repair. J Bone Joint Surg Am. 2006;88:536–40. doi: 10.2106/JBJS.E.00418. [DOI] [PubMed] [Google Scholar]
- 20.Bedi A, Kovacevic D, Hettrich C, Gulotta LV, Ehteshami JR, Warren RF, et al. The effect of matrix metalloproteinase inhibition on tendon-to-bone healing in a rotator cuff repair model. J Shoulder Elbow Surg. 2010;19:384–91. doi: 10.1016/j.jse.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 21.Costouros JG, Porramatikul M, Lie DT, Warner JJ. Reversal of suprascapular neuropathy following arthroscopic repair of massive supraspinatus and infraspinatus rotator cuff tears. Arthroscopy. 2007;23:1152–61. doi: 10.1016/j.arthro.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 22.Cheung EV, Silverio L, Sperling JW. Strategies in biologic augmentation of rotator cuff repair: A review. Clin Orthop Relat Res. 2010;468:1476–84. doi: 10.1007/s11999-010-1323-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cole BJ, Gomoll AH, Yanke A, Pylawka T, Lewis P, Macgillivray JD, et al. Biocompatibility of a polymer patch for rotator cuff repair. Knee Surg Sports Traumatol Arthrosc. 2007;15:632–7. doi: 10.1007/s00167-006-0187-6. [DOI] [PubMed] [Google Scholar]
- 24.Derwin KA, Badylak SF, Steinmann SP, Iannotti JP. Extracellular matrix scaffold devices for rotator cuff repair. J Shoulder Elbow Surg. 2010;19:467–76. doi: 10.1016/j.jse.2009.10.020. [DOI] [PubMed] [Google Scholar]
- 25.Derwin KA, Codsi MJ, Milks RA, Baker AR, McCarron JA, Iannotti JP. Rotator cuff repair augmentation in a canine model with use of a woven poly-L-lactide device. J Bone Joint Surg Am. 2009;91:1159–71. doi: 10.2106/JBJS.H.00775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kovacevic D, Rodeo SA. Biological augmentation of rotator cuff tendon repair. Clin Orthop Relat Res. 2008;466:622–33. doi: 10.1007/s11999-007-0112-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moffat KL, Kwei AS, Spalazzi JP, Doty SB, Levine WN, Lu HH. Novel nanofiber-based scaffold for rotator cuff repair and augmentation. Tissue Eng Part A. 2009;15:115–26. doi: 10.1089/ten.tea.2008.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rodeo SA. Biologic augmentation of rotator cuff tendon repair. J Shoulder Elbow Surg. 2007;16:S191–7. doi: 10.1016/j.jse.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 29.Santoni BG, McGilvray KC, Lyons AS, Bansal M, Turner AS, Macgillivray JD, et al. Biomechanical analysis of an ovine rotator cuff repair via porous patch augmentation in a chronic rupture model. Am J Sports Med. 2010;38:679–86. doi: 10.1177/0363546510366866. [DOI] [PubMed] [Google Scholar]
- 30.Seldes RM, Abramchayev I. Arthroscopic insertion of a biologic rotator cuff tissue augmentation after rotator cuff repair. Arthroscopy. 2006;22:113–6. doi: 10.1016/j.arthro.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 31.Henn RF, 3rd, Kang L, Tashjian RZ, Green A. Patients with workers’ compensation claims have worse outcomes after rotator cuff repair. J Bone Joint Surg Am. 2008;90:2105–13. doi: 10.2106/JBJS.F.00260. [DOI] [PubMed] [Google Scholar]
- 32.Misamore GW, Ziegler DW, Rushton JL., 2nd Repair of the rotator cuff.A comparison of results in two populations of patients. J Bone Joint Surg Am. 1995;77:1335–9. doi: 10.2106/00004623-199509000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Watson EM, Sonnabend DH. Outcome of rotator cuff repair. J Shoulder Elbow Surg. 2002;11:201–11. doi: 10.1067/mse.2002.122271. [DOI] [PubMed] [Google Scholar]
- 34.DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am. 1984;66:563–7. [PubMed] [Google Scholar]
- 35.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987:160–4. [PubMed] [Google Scholar]
- 36.Cook KF, Roddey TS, Gartsman GM, Olson SL. Development and psychometric evaluation of the Flexilevel Scale of Shoulder Function. Med Care. 2003;41:823–35. doi: 10.1097/00005650-200307000-00006. [DOI] [PubMed] [Google Scholar]
- 37.Cook KF, Roddey TS, O’Malley KJ, Gartsman GM. Development of a Flexilevel Scale for use with computer-adaptive testing for assessing shoulder function. J Shoulder Elbow Surg. 2005;14:90S–4S. doi: 10.1016/j.jse.2004.09.024. [DOI] [PubMed] [Google Scholar]
- 38.Kupsch A, Kessler MA, Weis M, Imhoff A. Development of a questionnaire for patient self-assessment of shoulder function based on the Rowe score. Unfallchirurg. 2007;110:111–5. doi: 10.1007/s00113-006-1198-y. [DOI] [PubMed] [Google Scholar]
- 39.Checchia SL, Doneux PS, Miyazaki AN, Silva LA, Fregoneze M, Ossada A, et al. Biceps tenodesis associated with arthroscopic repair of rotator cuff tears. J Shoulder Elbow Surg. 2005;14:138–44. doi: 10.1016/j.jse.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 40.Tashjian RZ, Henn RF, Kang L, Green A. The effect of comorbidity on self-assessed function in patients with a chronic rotator cuff tear. J Bone Joint Surg Am. 2004;86-A:355–62. doi: 10.2106/00004623-200402000-00020. [DOI] [PubMed] [Google Scholar]
- 41.Vad VB, Southern D, Warren RF, Altchek DW, Dines D. Prevalence of peripheral neurologic injuries in rotator cuff tears with atrophy. J Shoulder Elbow Surg. 2003;12:333–6. doi: 10.1016/s1058-2746(03)00040-5. [DOI] [PubMed] [Google Scholar]
- 42.Chen AL, Shapiro JA, Ahn AK, Zuckerman JD, Cuomo F. Rotator cuff repair in patients with type I diabetes mellitus. J Shoulder Elbow Surg. 2003;12:416–21. doi: 10.1016/s1058-2746(03)00172-1. [DOI] [PubMed] [Google Scholar]
- 43.Clement ND, Hallett A, MacDonald D, Howie C, McBirnie J. Does diabetes affect outcome after arthroscopic repair of the rotator cuff? J Bone Joint Surg Br. 2010;92:1112–7. doi: 10.1302/0301-620X.92B8.23571. [DOI] [PubMed] [Google Scholar]
- 44.Mallon WJ, Misamore G, Snead DS, Denton P. The impact of preoperative smoking habits on the results of rotator cuff repair. J Shoulder Elbow Surg. 2004;13:129–32. doi: 10.1016/j.jse.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 45.Prasad N, Odumala A, Elias F, Jenkins T. Outcome of open rotator cuff repair.An analysis of risk factors. Acta Orthop Belg. 2005;71:662–6. [PubMed] [Google Scholar]
- 46.Videler AJ, Beelen A, van Schaik IN, de Visser M, Nollet F. Limited upper limb functioning has impact on restrictions in participation and autonomy of patients with hereditary motor and sensory neuropathy 1a. J Rehabil Med. 2009;41:746–50. doi: 10.2340/16501977-0419. [DOI] [PubMed] [Google Scholar]
- 47.Agrawal V. Arthroscopic decompression of a bony suprascapular foramen. Arthroscopy. 2009;25:325–8. doi: 10.1016/j.arthro.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 48.Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87:1229–40. doi: 10.2106/JBJS.D.02035. [DOI] [PubMed] [Google Scholar]
- 49.Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy. 2005;21:1307–16. doi: 10.1016/j.arthro.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 50.Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am. 2007;89:953–60. doi: 10.2106/JBJS.F.00512. [DOI] [PubMed] [Google Scholar]
- 51.Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8:599–605. doi: 10.1016/s1058-2746(99)90097-6. [DOI] [PubMed] [Google Scholar]
- 52.Zanetti M, Gerber C, Hodler J. Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Invest Radiol. 1998;33:163–70. doi: 10.1097/00004424-199803000-00006. [DOI] [PubMed] [Google Scholar]
- 53.Snyder SJ, Arnoczky SP, Bond JL, Dopirak R. Histologic evaluation of a biopsy specimen obtained 3 months after rotator cuff augmentation with GraftJacket Matrix. Arthroscopy. 2009;25:329–33. doi: 10.1016/j.arthro.2008.05.023. [DOI] [PubMed] [Google Scholar]
- 54.St Pierre P, Olson EJ, Elliott JJ, O‘Hair KC, McKinney LA, Ryan J. Tendon-healing to cortical bone compared with healing to a cancellous trough.A biomechanical and histological evaluation in goats. J Bone Joint Surg Am. 1995;77:1858–66. doi: 10.2106/00004623-199512000-00010. [DOI] [PubMed] [Google Scholar]
- 55.Lui P, Zhang P, Chan K, Qin L. Biology and augmentation of tendon-bone insertion repair. J Orthop Surg Res. 2010;5:59. doi: 10.1186/1749-799X-5-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Meyer M, Klouche S, Rousselin B, Boru B, Bauer T, Hardy P. Does arthroscopic rotator cuff repair actually heal? Anatomic evaluation with magnetic resonance arthrography at minimum 2 years follow-up. J Shoulder Elbow Surg. 2012;21:531–6. doi: 10.1016/j.jse.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 57.Kowalsky MS, Keener JD. Revision arthroscopic rotator cuff repair: repair integrity and clinical outcome: surgical technique. J Bone Joint Surg Am. 2011;93(Suppl 1):62–74. doi: 10.2106/JBJS.J.01173. [DOI] [PubMed] [Google Scholar]
- 58.Cho NS, Lee BG, Rhee YG. Arthroscopic rotator cuff repair using a suture bridge technique: Is the repair integrity actually maintained? Am J Sports Med. 2011;39:2108–16. doi: 10.1177/0363546510397171. [DOI] [PubMed] [Google Scholar]
- 59.Toussaint B, Schnaser E, Bosley J, Lefebvre Y, Gobezie R. Early structural and functional outcomes for arthroscopic double-row transosseous-equivalent rotator cuff repair. Am J Sports Med. 2011;39:1217–25. doi: 10.1177/0363546510397725. [DOI] [PubMed] [Google Scholar]
- 60.Tashjian RZ, Hollins AM, Kim HM, Teefey SA, Middleton WD, Steger-May K, et al. Factors affecting healing rates after arthroscopic double-row rotator cuff repair. Am J Sports Med. 2010;38:2435–42. doi: 10.1177/0363546510382835. [DOI] [PubMed] [Google Scholar]
- 61.Duquin TR, Buyea C, Bisson LJ. Which method of rotator cuff repair leads to the highest rate of structural healing? A systematic review. Am J Sports Med. 2010;38:835–41. doi: 10.1177/0363546509359679. [DOI] [PubMed] [Google Scholar]
- 62.Slabaugh MA, Nho SJ, Grumet RC, Wilson JB, Seroyer ST, Frank RM, et al. Does the literature confirm superior clinical results in radiographically healed rotator cuffs after rotator cuff repair? Arthroscopy. 2010;26:393–403. doi: 10.1016/j.arthro.2009.07.023. [DOI] [PubMed] [Google Scholar]
- 63.Dodson CC, Kitay A, Verma NN, Adler RS, Nguyen J, Cordasco FA, et al. The long-term outcome of recurrent defects after rotator cuff repair. Am J Sports Med. 2010;38:35–9. doi: 10.1177/0363546509341654. [DOI] [PubMed] [Google Scholar]
- 64.Zumstein MA, Jost B, Hempel J, Hodler J, Gerber C. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2008;90:2423–31. doi: 10.2106/JBJS.G.00677. [DOI] [PubMed] [Google Scholar]
- 65.Coons DA, Alan Barber F. Tendon graft substitutes-rotator cuff patches. Sports Med Arthrosc. 2006;14:185–90. doi: 10.1097/00132585-200609000-00011. [DOI] [PubMed] [Google Scholar]
- 66.Phipatanakul WP, Petersen SA. Porcine small intestine submucosaxenograft augmentation in repair of massive rotator cuff tears. Am J Orthop (Belle Mead NJ) 2009;38:572–5. [PubMed] [Google Scholar]
- 67.Bond JL, Dopirak RM, Higgins J, Burns J, Snyder SJ. Arthroscopic replacement of massive, irreparable rotator cuff tears using a GraftJacket allograft: Technique and preliminary results. Arthroscopy. 2008;24:403–9. doi: 10.1016/j.arthro.2007.07.033. e1. [DOI] [PubMed] [Google Scholar]
- 68.Iannotti JP, Codsi MJ, Kwon YW, Derwin K, Ciccone J, Brems JJ. Porcine small intestine submucosa augmentation of surgical repair of chronic two-tendon rotator cuff tears.A randomized, controlled trial. J Bone Joint Surg Am. 2006;88:1238–44. doi: 10.2106/JBJS.E.00524. [DOI] [PubMed] [Google Scholar]
- 69.Vitale MA, Vitale MG, Zivin JG, Braman JP, Bigliani LU, Flatow EL. Rotator cuff repair: an analysis of utility scores and cost-effectiveness. J Shoulder Elbow Surg. 2007;16:181–7. doi: 10.1016/j.jse.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 70.Bishop J, Klepps S, Lo IK, Bird J, Gladstone JN, Flatow EL. Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elbow Surg. 2006;15:290–9. doi: 10.1016/j.jse.2005.09.017. [DOI] [PubMed] [Google Scholar]
- 71.Tavernier T, Walch G, Noel E, Lapra C, Bochu M. MRI of the rotator cuff: evaluation of a new symptomatologic classification. J Radiol. 1995;76:251–7. [PubMed] [Google Scholar]
- 72.Singson RD, Hoang T, Dan S, Friedman M. MR evaluation of rotator cuff pathology using T2-weighted fast spin-echo technique with and without fat suppression. AJR Am J Roentgenol. 1996;166:1061–5. doi: 10.2214/ajr.166.5.8615243. [DOI] [PubMed] [Google Scholar]
- 73.Gusmer PB, Potter HG, Donovan WD, O’Brien SJ. MR imaging of the shoulder after rotator cuff repair. AJR Am J Roentgenol. 1997;168:559–63. doi: 10.2214/ajr.168.2.9016248. [DOI] [PubMed] [Google Scholar]
- 74.Spielmann AL, Forster BB, Kokan P, Hawkins RH, Janzen DL. Shoulder after rotator cuff repair: MR imaging findings in asymptomatic individuals-initial experience. Radiology. 1999;213:705–8. doi: 10.1148/radiology.213.3.r99dc09705. [DOI] [PubMed] [Google Scholar]
- 75.Zanetti M, Jost B, Hodler J, Gerber C. MR imaging after rotator cuff repair: full-thickness defects and bursitis-like subacromial abnormalities in asymptomatic subjects. Skeletal Radiol. 2000;29:314–9. doi: 10.1007/s002560000203. [DOI] [PubMed] [Google Scholar]
- 76.Duc SR, Mengiardi B, Pfirrmann CW, Jost B, Hodler J, Zanetti M. Diagnostic performance of MR arthrography after rotator cuff repair. AJR Am J Roentgenol. 2006;186:237–41. doi: 10.2214/AJR.04.1818. [DOI] [PubMed] [Google Scholar]
- 77.Morag Y, Jacobson JA, Miller B, De Maeseneer M, Girish G, Jamadar D. MR imaging of rotator cuff injury: what the clinician needs to know. Radiographics. 2006;26:1045–65. doi: 10.1148/rg.264055087. [DOI] [PubMed] [Google Scholar]
- 78.Potter HG, Jawetz ST, Foo LF. Imaging of the rotator cuff following repair: human and animal models. J Shoulder Elbow Surg. 2007;16:S134–9. doi: 10.1016/j.jse.2007.02.114. [DOI] [PubMed] [Google Scholar]
- 79.Fotiadou AN, Vlychou M, Papadopoulos P, Karataglis DS, Palladas P, Fezoulidis IV. Ultrasonography of symptomatic rotator cuff tears compared with MR imaging and surgery. Eur J Radiol. 2008;68:174–9. doi: 10.1016/j.ejrad.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 80.de Jesus JO, Parker L, Frangos AJ, Nazarian LN. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. AJR Am J Roentgenol. 2009;192:1701–7. doi: 10.2214/AJR.08.1241. [DOI] [PubMed] [Google Scholar]
- 81.Jost B, Zumstein M, Pfirrmann CW, Gerber C. Long-term outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2006;88:472–9. doi: 10.2106/JBJS.E.00003. [DOI] [PubMed] [Google Scholar]


