Abstract
Background:
Currently there is no objective measure to determine disease severity in patients with acute influenza infection. During acute viral infections, C-reactive protein (CRP) has been shown to be elevated.
Aim:
To study the relationship between the symptoms of acute influenza A infection and correlate them with the level of inflammation as measured by serum CRP levels.
Settings and Design:
Prospective study.
Materials and Methods:
We enrolled a convenience sample of adults presenting to an urban academic emergency department (ED), who had positive Enzyme-linked immunosorbent assay detection of the influenza A antigen. The subjects were excluded if they had immunosuppression, liver disease or were currently taking antiviral medication. A previously validated severity of symptom (SOS) score was calculated by asking the participants to record the severity of seven symptoms associated with influenza infection. The subjects had the serum C-reactive protein (CRP) levels tested during their ED visit.
Statistical Analysis:
A linear regression model was used with CRP as a predictor of the SOS score. Pearson's product-moment coefficient was used to measure the dependence between the two quantities.
Results:
Thirty-two subjects were enrolled from January through March 2009, and of those, eight patients were excluded from the analysis, leaving 24 study subjects: 58% were women, of ages 18 to 63 years, with a mean age of 31 years (95% CI 25, 37). The mean SOS score was 14.1 ranging from 6 to 21 (95% CI 12.6, 26.4). The mean CRP score was 24.6 ranging from 0 to 64.7 (95% CI 15.8, 33.4). The correlation coefficient between the SOS score and CRP levels was r = 0.65 (P=0.00056).
Conclusion:
The severity of symptoms associated with acute influenza A infection correlateswith the serum CRP levels.
Keywords: C-reactive protein, illness severity, influenza, seasonal influenza
INTRODUCTION
The influenza virus affects anywhere between 5 and 20% of the population in the United States every year. Among that population there is a significant number of influenza-associated hospitalizations each year (up to 500,000 hospitalizations / year), and its complications are, most notably, secondary bacterial infections.[1] Prior studies have shown that influenza infection has caused significant morbidity, mortality, and cost to the healthcare system.[2] Currently there exists no objective means to determine the disease severity and the necessity for hospitalization or antiviral / antibiotic treatment in patients presenting with acute infection. Emergency department (ED) clinicians are the regular first-line providers in making important evaluations and treatment decisions for patients presenting with influenza infection. However, there is a great deal of heterogenicity in ED testing and treatment practices.[3] There exists ample opportunity for the identification and development of biomarkers within the process of the acute phase response in humans, to influenza infection, to help guide patient management.
During the acute phase response there is an increase in hepatic synthesis and plasma concentration of a group of proteins, which are involved in the inflammatory process as immune regulators.[4] One of these proteins, the C-reactive protein (CRP), has been shown to be markedly elevated in bacterial infections and is associated with less of a vigorous response in viral infections.[5] With either infection or tissue inflammation, interleukin-6, interleukin-1β, and the tumor necrosis factor-α, stimulate the hepatocytes to CRP synthesis.[6] It has been previously demonstrated that lower levels of CRP production are seen in viral or mycoplasma respiratory infections when compared to other bacterial etiologies.[7] Currently there is a lack of a routine laboratory study to help determine the severity of influenza infections. In individuals infected with Influenza A, there is a peak concentration of CRP in the serum one-to-two days after symptom onset and the CRP levels vary among adults with subclinical symptoms and those with severe influenza infections.[4] These results suggest that the level of the CRP might serve as a tool to determine the severity of disease in a patient infected with influenza. To our knowlede there is only one other study that has attempted to describe the acute phase reactants in acute influenza infection and associate them with the patients’ symptoms.[4]
We hypothesize that there exists a relationship between the severity of symptoms associated with influenza infection and the level of inflammation, as measured by CRP. Identifying markers that can predict disease severity would have immediate implications on how physicians evaluate and manage an individual with acute influenza infection.
MATERIALS AND METHODS
Study design
This is a prospective, observational study, approved by the Institutional Review Board, of a convenience sample of patients presenting to the ED with symptoms of influenza-like illness, which included cough and fever. The patients who presented during the influenza season with these two symptoms defined the term influenza-like illness.[8] Written informed consent was obtained from all patients and the study was approved by the hospital Institutional Review Board.
Study setting and population
The study was conducted from January through March 2009, at an urban academic Level 1 Trauma Center with an annual census greater than 100,000 patients. Patients (ages 18 to 65 years of age) presenting to the ED suspected of having an acute infection with influenza A were screened by the rapid point of care Enzyme-Linked ImmunoSorbent Assay (ELISA). Patients who were non-English speaking, had symptoms for greater than two days, had a history of liver disease, were currently taking immunosuppressant medications, had been previously diagnosed with pneumonia, or were currently taking either antibiotic or antiviral medication, were excluded. After enrollment, the patients were excluded if they had been diagnosed and treated for a bacterial process either during their ED stay or any time within two weeks after the initial visit. This was determined by a telephone follow-up survey conducted three weeks following their ED visit.
Study protocol
We collected all information using a standardized case reporting form. The participants were asked a series of questions to obtain their pertinent medical history. A severity of symptoms (SOS) score was calculated by asking the participants to record the severity of seven influenza symptoms including cough, nasal obstruction, sore throat, fatigue, headache, myalgia, and feverishness. We used a four point scale, zero being absent to three being severe, to record a total out of a possible 21 points. This type of scoring system was validated and previously reported in the literature.[9] The participants were subsequently contacted in a follow-up phone survey conducted three weeks after the initial presentation, to determine the total duration of symptoms and complications of infection. The diagnosis of concomitant bacterial infection was made by radiological data, blood or sputum culture results or the treating physician's determination. Peripheral blood was collected from each subject. The samples were processed for CRP levels by the accredited hospital laboratory, using standard methodologies. Research assistants reviewed the charts of all of the patients, who had a positive ELISA assay, for influenza A antigen, in order to record the demographic and outcome data.
Statistical analysis
Subject demographics are presented as means, with 95% confidence intervals. A linear regression model was used with the CRP as a predictor of the SOS score. Pearson's product-moment coefficient was used to measure the correlation between the two quantities.
RESULTS
During the study period there were 83 influenza antigen-positive adults, who presented to the ED, 43 of whom were screened. Eleven patients were excluded, due to unwillingness to comply with the study requirements. An additional eight patients were excluded after enrollment; four of these eight subjects were diagnosed with a concomitant bacterial process, and four patients were lost to follow-up, leaving only 24 subjects.
The demographics pattern in our study population and that of the total influenza-positive population were similar. The average age of the subjects enrolled was 30.9 years (95% CI 25, 36.8) compared to the total flu-positive population, with a mean age of 32.6 years (95% CI 28.8, 36.5). Our study population consisted of 58% women, compared to 64% in the total flu-positive patients. Of our study patients, 16.7% were admitted (19.2% in all flu-positive patients) and 11.1% had a concomitant bacterial process (12% of the total flu population).
The mean duration of symptoms prior to presentation was 2.5 days for all symptoms and 1.7 days for fever. The mean SOS score was 14.1 ranging from 6 to 21 (95% CI 12.6, 26.4). The average total duration of symptoms was 10.4 days (95% CI 7.5, 13.3) with a wide range of days reported (5 to 25 days). The mean CRP value was 24.6 mg / l ranging from 0 to 64.7 mg / l (95% CI 15.8, 33.4). The correlation coefficient between the SOS score and CRP levels was r = 0.65 (P=0.00056). Figure 1 is a graphical representation of the CRP values against the SOS score for each patient with a regression line. There was no correlation between the CRP values and the need for hospitalization or the total duration of symptoms.
Figure 1.
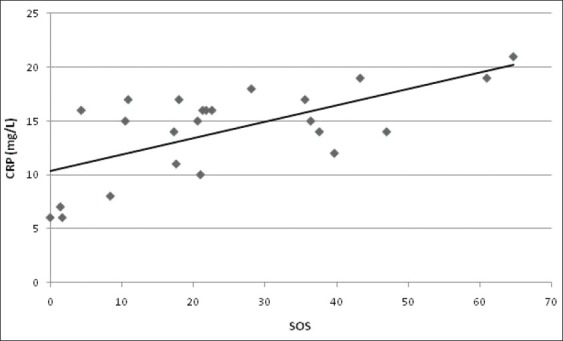
CRP = C-reactive protein expressed in milligrams per liter, SOS = Severity of Symptom Score; Each point represents an individual study subject, trendline is the linear black line
All patients were followed up with a three-week phone survey, to determine the total duration of symptoms from their initial visit to the ED and for any complications of the influenza infection, including repeat healthcare visits, subsequent bacterial infection, and the need for hospitalization. Patients who had a higher CRP level at presentation had a longer duration of symptoms than those with lower CRP values (P=0.024). Patients with CRP values greater than 25 mg / L had an average symptom duration that was significantly longer than those with a CRP less than 25 mg / L (P=0.024). Patients with CRP greater than 25 mg / L had a symptom duration of 13.44 days (95% CI 7.59, 19.30) compared to 8.18 days (95% CI 5.30, 11.06) in the less than 25mg / L group. We did not observe any relationship between the CRP levels and the complications of influenza infection or for the need for hospitalization during the initial ED visit.
In this study we performed a post-hoc analysis for statistical power using a linear regression model. With the 24 patients analyzed indicating a correlation of r = 0.65 and using an alpha level of 0.05, we calculated an observed power of 0.948, thus confirming adequate power in this study.
DISCUSSION
Patients presenting to the hospital with influenza-like symptoms pose a unique challenge to the emergency physician. The majority of these patients will require little diagnostic evaluation with only medical intervention for symptomatic complaints. However, each year there are a significant number of influenza-associated hospitalizations and complications with repeat healthcare visitis and subsequent admissions to the hospital.
In April of 2009, a novel influenza virus of swine origin emerged in North America. The virus, H1N1 was antigenetically unrelated to human seasonal influenza viruses, yet was related to viruses know to circulate in the swine.[10] In contrast to seasonal infleunza, most serious illnesses were among younger adults with approximately 90% of the deaths occuring between the ages of 18 and 65 years of age.[11] The emergency of this virus highlighted how little we knew about a patient's response to influenza infection and a lack of objective laboratory data to help the physician to identify those in need of antiviral medication.
Our study was performed prior to the H1N1 pandemic. However, our data suggests that patients with higher CRP levels report more severe symptom manifestions as measured by the SOS score and also had a longer duration of illness from their infleunza infection. This information is useful to the ED provider in two ways. First, it provides a quantifying tool on how sick a patient feels when he / she presents to the ED. Second, it gives the provider information pertaining to how long the patient will experience the effects of their infection. This provides valuable information on the patient, as to how ‘sick’ they really are. The CRP vaules greater than 25 mg / L equate to about a week longer in the duration of symptoms compared to patients with a CRP level less than 25 mg / L. Providing the patient with this information may lead to less future healthcare visits, and an overall better patient understanding of their own illness. Patients with higher CRP values may benefit from either a short inpatient stay or closer outpatient follow-up, in the management of their infection. This issue, however, is not addressed in this study. Antiviral medication such as Oseltamivir has been shown to reduce the symptoms of influenza anywhere by one to three days. However, guidelines for its use are vague and left up to the providing ED physician's judgment.[9] If using the CRP levels helps to identify patients at risk for a longer disease course, we may then be able to target individuals who would benefit the greatest from antiviral therapy. Our study is not statistically powered to show a relationship between the need for hospitalization and complications of influenza illness with a higher CRP level.
This is the first study that demonstrates that the severity of symptoms from an influenza infection with which an individual presents to the ED correlates to the CRP level, and that this level can then be predictive of the duration of the illness. Our goal was not to study concomitant bacterial infections. However, of our excluded patients, who had concurrent bacterial infections, the average CRP was 192.4 mg / l ranging from 72.2 to 477. This concomitant bacterial / influenza positive population had a significantly higher average and range of CRP. The CRP was shown to be of utility in diagnosing community-acquired pneumonia, with CRP levels > 50mg / L having a 74% sensitivity and 96% specificity.[12] This data provided a starting point for further investigations into the utility of CRP in the influenza-infected individual and its utility in identifying patients who may be harboring another bacterial illness, in addition to their influenza infection.
Limitations
A selection bias toward healthier patients was observed, with the exclusion of elderly and young patients. This study had a limited number of patients enrolled and thus could be possibly confounded by other variables that influence CRP production rather than infection, such as, location and lifestyle. We did screen a significant number of patients with a positive antigen test (52%), however, we had a significant number excluded from our final analysis. There remains a possible confounder that one of subjects in this study did have a bacterial process, and that subjects with bacterial infection were included in our analysis. We attempted to control for undiagnosed bacterial infection at the time of ED presentation by conducting a two-week phone follow-up survey to screen for any patients who subsequently had a bacterial infection diagnosed by another provider and / or were given antibiotics after their initial ED visit. Our study was also subject to the current ED practice during this time period, where there exists a selection bias among the ED practitioner, with regard to, whom the rapid influenza test should be performed on. This study also relied on rapid antigen positive individuals, where there was a reported sensitivity of 98%, however, the specificity varied between 50 and 90%, thus missing a potential population for enrollment, who tested as false negative on our screening protocol.[13]
CONCLUSION
There is a correlation between the severity of symptoms of ED patients with seasonal influenza A and the severity of inflammation as measured by serum CRP. Furthermore patients with higher CRP levels (> 25mg / L) had a longer total duration of their symptoms by nearly one week. This is the first study to describe a biomarker that correlates to a patient's symptoms and is also predictive of the disease duration, drawn during that patient's initial presentation to the ED with a febrile illness. Further studies are needed to address whether CRP can be used to predict the need for hospitalization, the necessity for prescribing antiviral medication, the development of flu-related complications, and the presence of concomitant bacterial infection.
Footnotes
Source of Support: Intradepartmental grant through the Department of Emergency Medicine (University Emergency Medicine Foundation)
Conflict of Interest: None declared.
REFERENCES
- 1.Thompson WW, Shay DK, Weintraub E, Brammer L, Bridges CB, Cox NJ, et al. Influenza-associated hospitalizations in the United States. JAMA. 2004;292:1333–40. doi: 10.1001/jama.292.11.1333. [DOI] [PubMed] [Google Scholar]
- 2.Barenfanger J, Drake C, Leon N, Mueller T, Troutt T. Clinical and financial benefits of rapid detection of respiratory viruses: An outcomes study. J Clin Microbiol. 2000;38:2824–8. doi: 10.1128/jcm.38.8.2824-2828.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mueller MR, Smith PJ, Baumbach JP, Palumbo JP, Meek JI, Gershman K, et al. Influenza testing and antiviral prescribing practices among emergency department clinicians in 9 states during the 2006 to 2007 influenza season. Ann Emerg Med. 2010;55:32–9. doi: 10.1016/j.annemergmed.2009.09.019. [DOI] [PubMed] [Google Scholar]
- 4.Whicher JT, Chambers RE, Higginson J, Nashef L, Higgins PG. Acute phase response of serum amyloid A protein and C reactive protein to the common cold and influenza. J Clin Pathol. 1985;38:312–6. doi: 10.1136/jcp.38.3.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Falsey AR, Walsh EE, Francis CW, Looney RJ, Kolassa JE, Hall WJ, et al. Response of C-reactive protein and serum amyloid A to influenza A infection in older adults. J Infect Dis. 2001;183:995–9. doi: 10.1086/319275. [DOI] [PubMed] [Google Scholar]
- 6.Summah H, Qu JM. Biomarkers: A definitive plus in pneumonia. Mediators Inflamm. 2009;2009:675753. doi: 10.1155/2009/675753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lehtomaki K, Leinonen M, Takala A, Hovi T, Herva E, Koskela M. Etiological diagnosis of pneumonia in military conscripts by combined use of bacterial culture and serological methods. Eur J Clin Microbiol Infect Dis. 1988;7:348–54. doi: 10.1007/BF01962335. [DOI] [PubMed] [Google Scholar]
- 8.Monto AS, Gravenstein S, Elliott M, Colopy M, Schweinle J. Clinical signs and symptoms predicting influenza infection. Arch Intern Med. 2000;160:3243–7. doi: 10.1001/archinte.160.21.3243. [DOI] [PubMed] [Google Scholar]
- 9.Treanor JJ, Hayden FG, Vrooman PS, Barbarash R, Bettis R, Riff D, et al. Efficacy and safety of the oral neuraminidase inhibitor oseltamivir in treating acute influenza: A randomized controlled trial. US Oral Neuraminidase Study Group. JAMA. 2000;283:1016–24. doi: 10.1001/jama.283.8.1016. [DOI] [PubMed] [Google Scholar]
- 10.Peiris JS, Poon LL, Guan Y. Emergence of a novel swine-origin influenza A virus (S-OIV) H1N1 virus in humans. J Clin Virol. 2009;45:169–73. doi: 10.1016/j.jcv.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bautista E, Chotpitayasunondh T, Gao Z, Harper SA, Shaw M, Uyeki TM, et al. Clinical aspects of pandemic 2009 influenza A (H1N1) virus infection. N Engl J Med. 2010;362:1708–19. doi: 10.1056/NEJMra1000449. [DOI] [PubMed] [Google Scholar]
- 12.Flanders SA, Stein J, Shochat G, Sellers K, Holland M, Maselli J, et al. Performance of a bedside C-reactive protein test in the diagnosis of community-acquired pneumonia in adults with acute cough. Am J Med. 2004;116:529–35. doi: 10.1016/j.amjmed.2003.11.023. [DOI] [PubMed] [Google Scholar]
- 13.National Center for Immunization and Respiratory Diseases [Internet]. Atlanta. National Center for Immunization and Respiratory Diseases [Internet]. Atlanta. [updated 2011 Sep 30, Last cited on 2011 Nov 28]. Available from: http://www.cdc.gov/flu/professionals/diagnosis/


