Abstract
Peyronie's disease is still a therapeutic dilemma for the urologist. Although medical treatment includes multiple versions, few therapeutic agents had significant effects. The combination between oral therapy and intralesional agents can improve the quality of life of the patients with Peyronie's disease.
Keywords: Peyronie disease, verapamil, vitamin E, colchicine
Introduction
Peyronie's disease is a disorder manifested by the abnormal penis curvature during erection, due to the development of fibrous nodules in the albuginée, first described in 1743 by Francois Gigot de La Peyronie [1], associated or not with pain and the inability to achieve a satisfactory sexual intercourse. The best therapy of Peyronie's disease remains controversial, in part because the etiology and natural history of the disease are not sufficiently known, and the treatment aims not to the disease itself but its effects (penile curvature and erectile dysfunction). The disease was associated with other systemic conditions such as hypertension and diabetes, Dupuytren's disease and Ledderhose’s disease.
While severe deformities and erectile dysfunctionare best treated surgically, for light and medium curvatures, pain and slow disease progression is preferred to a conservative approach by oral and intralesional therapy [2,3].
Methods
During 2004-2012, 350 patients diagnosed with Peyronie's disease, were treated as it follows: group I consisted of 125 patients treated with intralesional injections of verapamil; second group of 100 patients were treated with Vitamin E and Colchicine; third group consisted of 125 patients treated with verapamil, vitamin E and Colchicine (Fig. 1). The age of patients was between 19 and 72 years.
Fig. 1.
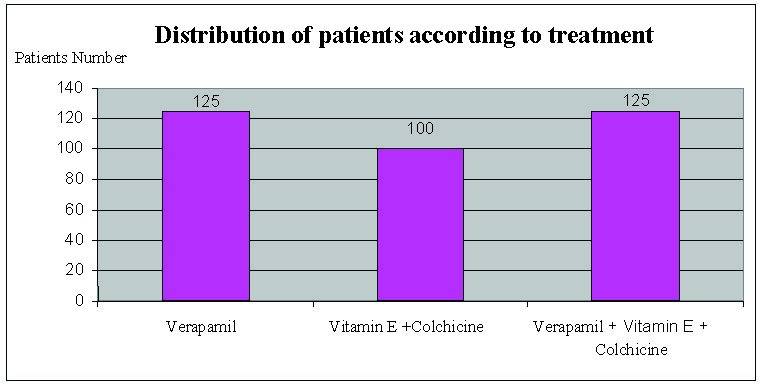
Therapeutical study groups
The group of patients underwent a comprehensive diagnostic protocol that included medical history, clinical examination, self-photography, penile Doppler ultrasound in patients with associated erectile dysfunction. Following investigations and clinical examination have determined the way the disease started, the place of the injury, size and number of calcifications present, presence of pain, degree of penile deviation, associated erectile dysfunction and the presence of other affections.
Treatment protocol included 10 mg Verapamil, one injection per week for a period of 12 to 15 weeks, 200 mg vitamin E twice daily in combination with Colchicine 1mg twice a day for a period of 3 to 6 months and the association of the three therapeutic agents for a period of 3 months.
Drug therapy was administered as it follows: local anesthesia with lidocaine after local aseptic Betadine; infiltration is carried out in several places in the plaque to ensure the uniform distribution of the injected drug and then the place must be compressed for a few minutes in order to reduce local bruising. The injection was done with care to avoid the damage of the neurovascular bundle and the penetration of the drug in the corpus cavernosum.
Results
In the first group (125 patients) treated with verapamil, followed by a period of 12 to 15 weeks, we found the following results (Fig. 2):
Fig. 2.
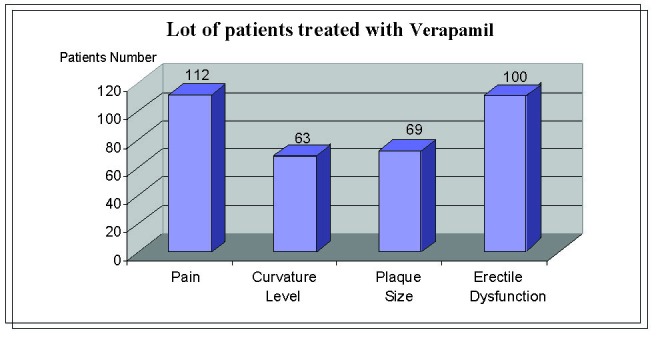
Results in patients treated with verapamil
- Pain resolved completely or partially in 90% of the patients (112 patients)
- Curvature level decreased by 10 – 30 in 50% of the patients (63 patients), while for the rest there was no change in the deviation
- Plaque size decreased to about 55% of the patients (69 patients), while the rest remained unchanged
- improved erectile dysfunction in 80% of the patients (100 patients)
In the group of 100 patients treated with vitamin E and colchicine, we have noticed the following (Fig. 3):
- pain resolved completely or partially in 87% of the patients (87 patients)
- curvature level decreased by 10 – 20 in 40% of the patients (40 patients), while for the rest there was no change in the deviation
- plaque size decreased to about 30% of the patients (30 patients), while the rest remained unchanged
- improved erectile dysfunction in 75% of the patients (75 patients)
Fig. 3.
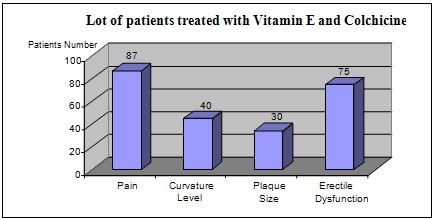
Results in patients treated with vitamin E and colchicine
For the group of 125 patients treated with verapamil in combination with Vitamin E and Colchicine, the results were the following (Fig. 4):
Fig. 4.
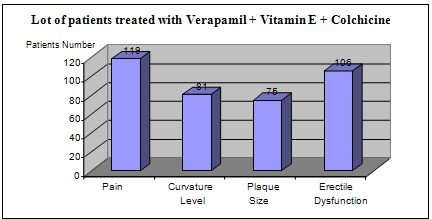
Results in patients treated with verapamil, vitamin E and colchicine
- pain resolved completely or partially in 95% of the patients (119 patients)
- curvature level decreased by 20 – 45 in 65% of the patients (81 patients), while for the rest there was no change in the deviation
- plaque size decreased to about 60% of the patients (75 patients), while the rest remained unchanged
- improved erectile dysfunction in approx. 85% of the patients (106 patients)
Table 1.
Results in all three cases (treatment with verapamil; vitamin E and colchicine; verapamil, vitamin E and colchicine)
| Verapamil | Vitamin E + Colchicine | Verapamil + Vitamin E + Colchicine | |
|---|---|---|---|
| Total patients | 125 patients | 100 patients | 125 patients |
| Pain – resolved | 90 % - 112 patients | 87 % - 87 patients | 95% - 119 patients |
| Curvature Level – decreased | 50 % - 63 patients 10 º -30º | 40 % - 40 patients 10 º -20º | 65% - 81 patients 20 º -45 º |
| Plaque Size – decreased | 55 % - 69 patients | 30 % - 30 patients | 60% - 75 patients |
| Erectile Dysfunction – improved | 80 % - 100 patients | 75 % - 75 patients | 85% - 106 patients |
Discussions
Candidates for medical treatment of Peyronie's disease are patients with an early stage disease, those with progressive deformity and unstable plaque and those with painful erections.
Relatively recent studies have shown that calcium channel blockers (especially verapamil) are effective in the treatment of Peyronie's disease when administered intralesional (or perilesional). When administered orally, verapamil is effective for cardiologic use. Verapamil has the following benefic effects in this condition: increase in extracellular collagenase activity, decreased metabolic activity of fibroblasts, extracellular collagen deposit reduction [4-6]. Several regimens such as the following can be used: 10 mg per week for 10 weeks or 10 mg every two weeks – 10 doses. Other schemes require 2-3 cures repeated at various intervals, using the same dose (10 mg every week or at 2 weeks). The following were reported as side effects: bruises, hematomas, abnormal sensitivity (temporary). There were no reported episodes of hypotension, cardiac arrhythmias or local infection after intralesional administration of verapamil in literature. In assessing the therapeutic efficacy, the following were evaluated: plaque size, penile curvature level, severity of pain in erection. In 1996, Levine studied 38 patients treated with verapamil 10 mg for 2 weeks (12 infiltrations). He noted a rapid reduction in pain in 97% of the patients, subjective improved of curvature in 76% of the patients, reduced plaque thickness in 86% of the patients, improved rigidity distal in 93% and improved erectile performance in 72% of the patients. Plaque volume increased in 43% of the patients, but gradually decreased after 6-18 months. In 65% of the patients with disease duration less than one year, the curvature decreased by 21 on average and 44% of those with disease duration longer than one year, the curvature decreased by 23. Complications or side effects were minimal, with no infection, hypotension or arrhythmias [7-9].
Vitamin E has been much used in the treatment of Peyronie's disease for its antioxidant effect to prevent fibrosis. Although changes of curvature and plaque are not significant [10], because it is a cheap drug, and it has an apparent effect of pain reduction and reduced side effects, vitamin E can be considered in the treatment of Peyronie's disease. Yet, early studies showed reduced curvature in 78% of the patients and reduction in size calcifications in 91% of the patients [11-13].
Colchicine was recently recognized as having a therapeutic potential in Peyronie's disease. It works by blocking the path of arachidonic acid lipoxygenase, thus preventing leukotriene formation by reducing inflammation and chemotaxis and interferes with procollagen transcellular migration, reducing the formation of procollagen and enhancing the production of collagenase [14]. Therefore, it has antifibrotic, antimitotic and anti-inflammatory effects. Akkus et al. [15] published the first pilot study in which they administered oral colchicine for 3–5 months to a group of 24 patients with Peyronie’s disease, with encouraging results.
Conclusions
Treatment with intralesional Verapamil proved to be extremely useful in the early stages of Peyronie's disease with positive effects on pain, curvature and plaque size. However, the association of Verapamil with Vitamin E and Colchicine showed better pain control while reducing penile curvature, dimensions of calcification and the degree of erectile dysfunction, thus improving the quality of life.
References
- 1.Musitelli S, Bossi M, Jallous H. A brief historical survey of ‘‘Peyronie disease.’’. J Sex Med. 2008;5:1737–1746. doi: 10.1111/j.1743-6109.2007.00692.x. [DOI] [PubMed] [Google Scholar]
- 2.Fitkin J, Ho GT. Peyronie’s disease: current management. Am Fam Physician. 1999;60:549–552. [PubMed] [Google Scholar]
- 3.Tunuguntlas HS. Management of Peyronie’s disease: a review. World J Urol. 2001;19:244–250. doi: 10.1007/s003450100209. [DOI] [PubMed] [Google Scholar]
- 4.Lee RC, Ping J. Calcium antagonists retard extracellular matrix production in connective tissue equivalent. J Surg Res. 1990;49:463–466. doi: 10.1016/0022-4804(90)90197-a. [DOI] [PubMed] [Google Scholar]
- 5.Doong H, Dissanayake S, Gowrishankar TR. The 1996 Lindberg Award. Calcium antagonists alter cell shape and induce procollagenase synthesis in keloid and normal human dermal fibroblasts. J Burn Care Rehabil. 1996;17:497–514. [PubMed] [Google Scholar]
- 6.Roth M, Eickelberg O, Kohler E. Ca2+ channel blockers modulate metabolism of collagenase within the extracellular matrix. Proc Natl Acad Sci USA. 1996;93:5478–5482. doi: 10.1073/pnas.93.11.5478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arena F, Peracchia G, Di Stefano C. Clinical effects of verapamil in the treatment of Peyronie’s disease. Acta Biomed Ateneo Parmense. 1995;66:269–272. [PubMed] [Google Scholar]
- 8.Lasser A, Vandenberg TL, Vincent MJ. Intraplaque verapamil injection for treatment of Peyronie’s disease. J La State Med Soc. 1998;150:431–434. [PubMed] [Google Scholar]
- 9.Rehman J, Benet A, Melman A. Use of intralesional verapamil to dissolve Peyronie’s disease plaque: a long-term single-blind study. Urology. 1998;51:620–625. doi: 10.1016/s0090-4295(97)00700-0. [DOI] [PubMed] [Google Scholar]
- 10.Hashimoto K, Hisasue S, Kato R . Outcome analysis for conservative management of Peyronie disease. Int J Urol. 2006;13:244–247. doi: 10.1111/j.1442-2042.2006.01270.x. [DOI] [PubMed] [Google Scholar]
- 11.Chesney J. Peyronie’s disease. Br J Urol. 1975;47:209–218. doi: 10.1111/j.1464-410x.1975.tb03950.x. [DOI] [PubMed] [Google Scholar]
- 12.Scott WW, Scardino PL. New concept in treatment of Peyronie’s disease. South Med J. 1947;41:173–177. doi: 10.1097/00007611-194802000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Scardino PL, Scott WW. The use of tocopherols in the treatment of Peyronie’s disease. Ann NY Acad Sci. 1949;52:390–401. [Google Scholar]
- 14.Anderson MS, Shankey TV, Lubrano T. Inhibition of Peyronie’s plaque fibroblast proliferation by biologic agents. Int J Impot Res. 2000;12:S25–S31. doi: 10.1038/sj.ijir.3900558. [DOI] [PubMed] [Google Scholar]
- 15.Akkus E, Carrier S, Rehman J. Is colchicine effective in Peyronie’s disease? A pilot study. Urology. 1994;44:291–295. doi: 10.1016/s0090-4295(94)80155-x. [DOI] [PubMed] [Google Scholar]


