ABSTRACT
Aim: To evaluate the real incidence of contact dermatitis, to identify the most common allergens, the favoring factors, to establish the prophylaxis methods, the key for a correct management of the patient with contact dermatitis.
Method: A retrospective study, on the patients that refers to the Dermatology Clinic, "St. Spiridon" Emergency Hospital Iasi, between 01.01.2006 and 31.12. 2009, based on demographic items, the type of contact dermatitis and the allergens implicated.
Results: we enrolled 353 patients between 2006-2009, representing 3,89% from the hospitalized patients; the study reveals a higher incidence at women (60,27%), similar with data from literature; the majority of the patients was aged over 45, with the higher rate in the interval of 45-65 years old; the most frequent implicated allergens and irritants were plants (26,31% - 92 patients) and topical drugs and antiseptics (25,65% - 89 patients); the area most affected was the face (25%) and the hands (19,07%), from which almost 80-90% was occupational dermatitis. The distribution of cases depending on the type of contact dermatitis indicates an approximate percentage of those allergic to those irritant.
Conclusions: The real prevalence of this disease is unknown, being frequently a missed diagnosis (other kinds of eczema), the key of the correct diagnose being a repeated, exhaustive anamnesis, revealing all the favoring conditions and possible contact allergens.
Keywords: contact dermatitis, contact allergen, epidemiology, clinical aspects
INTRODUCTION
The contact dermatitis is an inflammatory reaction due to skin contact with chemical substances (1). These reactions can be allergic and irritant. Many of the eczema cases with unknown etiology are, in fact, clinical forms of contact dermatitis (2).
Contact dermatitis diagnosis can be achieved only after the study of multiple variables. A good knowledge of the different skin reactions, data about varied important contact substances, is mandatory in order to give a correct diagnosis. The most common reaction is the eczematous type, but other types of lesions can be seen, such as erythema multiform, purpuric rash, exanthema, erythroderma, lichenoid eruption, contact allergic granuloma, toxic epidermal necrolysis, photosensitivity reactions, pigmented lesions (3). These clinical aspects of contact dermatitis may present specific features based on various factors: the age (every age group has a different exposure to chemicals in the environment); sex: allergic contact dermatitis and irritant contact dermatitis are more common at women than at men, this may be the consequence of a different mode of exposure to the challenging substances (1,3,4); particular predisposition: genetic factors have special importance in the development of irritant-type reactions (atopy); patients with acute or debilitating diseases (AIDS, autoimmune disorders, cancer, Hodgkin disease, lymphoma,) have a reduced capacity to develop contact dermatitis due to a reduced responsiveness or an absent responsiveness of the immune system (3).
The regional factors also play an important role in the onset and clinical aspect of the lesions in contact dermatitis: the integrity of the skin, oclusal factors, anatomical region (1-4). ❑
AIM OF THE STUDY
The study aims to identify demographical characteristics of contact dermatitis, the frequent implicated allergens, the more frequent clinical aspect meet in contact dermatitis. ❑
MATERIAL AND METHODS
Data underlying this study come from clinical-epidemiological observation of cases of contact dermatitis diagnosed and hospitalized in the Dermatology Department, "St. Spiridon" Hospital, Iasi. These are included in the extended squad of patients hospitalized in the clinic during the 1st of January 2006 and 31st of December 2009. During this period, in the Dermatology Department were recorded a total of 9059 hospitalizations (2125 in 2006, 2564 in 2007, 2305 in 2008 and 2065 in 2009).
We study a number of 353 patients with contact dermatitis (61 in 2006, 65 in 2007, 121 in 2008, and 106 in 2009).
The descriptive epidemiological research follows variables which refer to the type of person (demographic, social, and related lifestyle) and area of origin:
demographic variables – age, gender, the native environment (urban, rural, the distribution of cases on the counties of origin);
social variables - level training, socio-economic status;
variables related to lifestyle - characteristics of the profession and their impact on the health of the injured, drug use (alcohol, tobacco, coffee);
variables related to the temporal factor – the time of onset and the evolution of the disease.
It was intended to specify the type of contact dermatitis of the cases studied. Clinically we could highlight the appearance of lesions, their location and the emergence of injuries or complications in the course of the evolution of the disease or treatment. Based on the information gathered there were identified certain etiological factors that have been implicated in triggering and aggravation of the disease. A part of the patients included in the study were patch tested for a precise positive diagnose, some of the tested substances having a dual character (allergen and irritant). ❑
RESULTS
The distribution of contact dermatitis cases by sex revealed the predominance of the disease on females; report frequency was women: men - 1.83: 1. The repartition of cases of contact dermatitis among urban and rural areas, revealed a distribution of 1.35: 1 case.
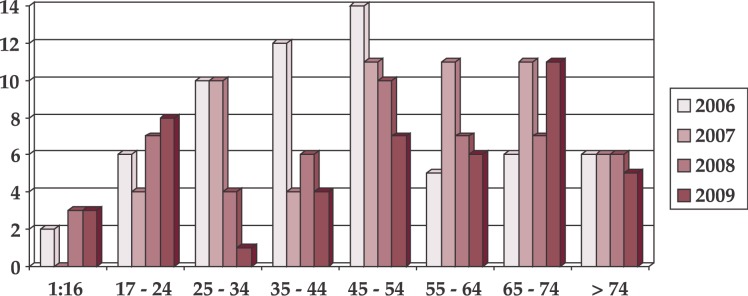
Regarding the age groups with important increases in the incidence of the contact dermatitis, it turned out to be those aged 45 to 74 years old (Figure 1).
Figure 1. Distribution of cases of contact dermatitis by groups of age.
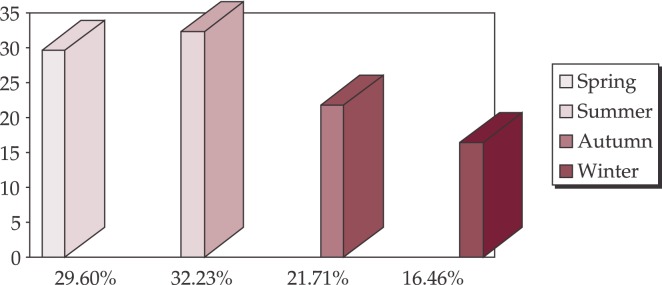
Dynamics of hospitalizations for contact dermatitis, depending on the time of the year, the group of the majority of cases reported during the spring (29.6%) - summer (32.23%) period, in which the risk of contact with the various allergens is significantly increased (Figure 2).
Figure 2. Dynamics of hospitalization for contact dermatitis by seasons.
The vast majority of cases investigated by the contact dermatitis has consisted of a single factor from etiological point of presence (236 cases), but there have been 79 cases in which the disease was triggered by 2 factors and 37 cases with 3 or more etiological factors.
There is an increased incidence (>10%) of plants (26.31%), antiseptics and topical drugs (25.65%) and detergents/soaps (11.84%) (Table 1).
Table 1.
The occurrence frequency of etiological factors in the onset of contact dermatitis
| Nr. | Etiological factors | No Cases | % |
|---|---|---|---|
| 1 | Plants | 92 | 26.14 |
| 2 | Antiseptics and topical drugs | 89 | 25.28 |
| 3 | Detergents/soaps | 41 | 11.64 |
| 4 | Various chemicals | 32 | 9.09 |
| 5 | Cosmetic | 30 | 8.52 |
| 6 | Ultraviolet radiation | 20 | 5.68 |
| 7 | Building materials | 15 | 4.26 |
| 8 | Propolis | 12 | 3.41 |
| 9 | Footwear | 9 | 2.84 |
| 10 | Textile | 5 | 1.42 |
| 11 | Metals | 5 | 1.42 |
| 12 | Others | 2 | 0.57 |
| TOTAL | 352 | 100 |
From plants, the most frequent ones have a well-established medicinal use: marigold 30%, chamomile 20%, and comfrey 17.5%. Disinfectants and topical drugs rank two in the etiology of contact dermatitis, and notably are: antiseptics (alcohol, isopropyl alcohol, iod alcohol 1% etc.), nonsteroid anti-inflammatory drugs (diclofenac, ibuprofen, and acetylsalicylic acid), topical antibiotics (e.g. gentamicin, neomycin, penicillin, rifampicine) (Table 2).
Table 2.
Antiseptic and topical drugs in the etiology of contact dermatitis
| Nr. | Antiseptics and topical medications | No Cases | % |
|---|---|---|---|
| 1 | Antiseptic | 31 | 35.89 |
| 2 | Steroidal anti-inflammatory agents | 16 | 17.94 |
| 3 | Antibiotics | 14 | 15.39 |
| 4 | Corticosteroids topics | 14 | 15.39 |
| 5 | Other medicines | 14 | 15.39 |
| TOTAL | 89 | 100 |
The distribution of cases depending on the type of contact dermatitis indicates an approximate percentage of those allergic to those irritant. From the perspective of the clinical and biological evolution the vast cases of contact dermatitis were acute (59.21%) and subacute (21.06%) forms (Table 3).
Table 3.
The distribution of cases depending on the type of contact dermatitis
| Nr. | Contact Dermatitis type | No Cases | % |
|---|---|---|---|
| 1 | Allergic | 162 | 45.39 |
| 2 | Irritant | 163 | 46.72 |
| 3 | Photoallergic | 7 | 1.98 |
| 4 | Phototoxic Response | 18 | 5.26 |
| 5 | Phytophotodermatosis | 2 | 0.65 |
| TOTAL | 352 | 100 |
The most frequent affected areas were the face (25%) and the hands (19.07%).
Some of the patients diagnosed with contact dermatitis have associated other diseases, considered important in the evolution and in the treatment of the cases (Table 4).
Table 4.
The general diseases associated with contact dermatitis
| Nr. | Associated diseases | No Cases | % |
|---|---|---|---|
| 1 | Cardiovascular disease | 123 | 34.86 |
| 2 | Respiratory diseases | 21 | 5.92 |
| 3 | Digestive diseases | 53 | 15.13 |
| 4 | Diseases of nutrition and metabolism | 16 | 4.6 |
| 5 | Uro-genital diseases | 21 | 5.92 |
| 6 | Rheumatic diseases | 32 | 9.21 |
| 7 | Neurological diseases | 16 | 4.6 |
| 8 | Without General disorders | 70 | 19.73 |
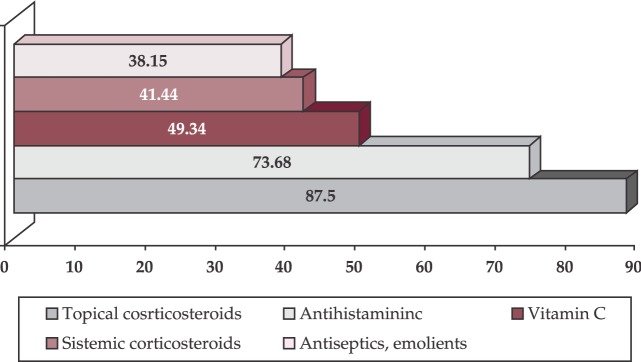
Therapy applied to the hospitalized patients was based on topical drugs (87.5%), corticosteroids, associated with classic and modern antihistaminic drugs, the antiH1 and antiH2 (73.68%), non-specific medication (calcium, vitamin C) (Figure 3). ❑
Figure 3. The treatment used in contact dermatitis.
DISCUSSIONS
The achieved study reflects a frequency of contact dermatitis cases of 3.89% relative to other dermatological disorders for which patients refer to Dermatological Clinic from the1st of January 2006 to the 31st of December 2009. This incidence corresponds to the data published in the literature, in which it is estimated that the prevalence varies between 1.7-6.3%.
Johnson estimated that 1-2% of patients hospitalized in the United States suffer from contact dermatitis. In the Netherlands the rate of incidence of contact dermatitis as primary diagnosis is about 9 per 100,000 inhabitants per year, which represents 6% of the total of dermatological patients and less than 1% of total hospitalizations in 1988 (5).
Regarding the area of origin it is found a relatively constant rate of incidence, both in urban and rural areas (urban – rural: 57.38% - 42.62%). These values of incidence are explained by the frequency of such diseases among the population irrespective of the origin.
Concerning the studied cases of contact dermatitis depending on sex, it was found more frequently at females 66.47%, compared with 33.53% recorded at males.
A series of studies conducted in European countries have revealed the following results: Netherlands (women 8%, men 4.4%), Norway (women 13.2%, men 4.9%), Sweden (women 14.6%, men 8.9%). These results indicate that the rate of incidence of the disorders is higher at females (1,3).
Although the data obtained in a variety of studies could not established an unanimous conclusion, clinical practice shows that females are most affected.
The distribution of cases of contact dermatitis by age groups indicates that the most affected by the condition were the age groups ranging from 46 to 74 years, patients over 45 years representing 64.46% of all cases studied. In United States the prevalence seems to increase with age, and after a series of publications edited in Sweden, the Netherlands and Norway, the rate of incidence tends to decrease slightly after the age of 50 years (5).
The study conducted by Johnson and Roberts tied to the prevalence of contact dermatitis by sex and age groups shows that there is a clear trend of increase in prevalence at males [6]. At women the increased prevalence rate is generally around the age of 40 years, many of those practicing domestic activities.
In conclusion, all these studies suggest that the age and sex – by themselves – are not risk factors for contact dermatitis, but may become in association with exposure to different professional and household activities.
Dynamics of hospitalization after the season reflects an increase in the number of hospitalization in summer (32.23%), which proves the impact of climatic conditions (ultra violet radiation, temperature) on the onset and exacerbation of this condition.
From the etiological point, the study shows a variety of factors involved in triggering and exacerbating the disease. From the etiological factors, it needs to be mentioned: plants – 26.14%, topical drugs and antiseptics – 25.28%, cosmetics 8.52% etc.
It is estimated that 5-10% of cases of contact dermatitis obtained from studies conducted in European clinics are determined by plants. Compositae family contains over 13,000 species, some of them are food, for consumption, other are cultivated as ornamental plants (chrysanthemums) and other (arnica, marigold) are medicinal plants. Schmidt studied allergic contact dermatitis induced by plants from Compositae family. He found that repeated exposure causes often acute contact dermatitis, with frequent relapses and subsequently it becomes chronic, with lichenification. When it is located at the level of the elbow or knee it can simulate an atopic dermatitis. Originally localized lesions at the level of the face, hands and genitals may disseminate and have a bad prognosis, evolving to erythroderma (7). Also, the remaining dust from these plants may induce airborne dermatitis, frequently encountered situations in the regions of desert in the US and Australia.
Most of the drugs applied on tegument may determine sensitizations of different intensities. The list of topical drugs responsible for these sensitizations depends on the constitution of each individual, but also on the pharmaceutical industry to reduce the amount of topically agents capable of sensitization.
In our case study of contact dermatitis from the medicines point of view there were recorded nonsteroid anti-inflammatory agents, antibiotics, topical corticosteroids etc.
The location on hand appears most frequently in professional contact dermatitis at both women and men, in a proportion of 80% to 90%. Also located at the hand level, dermatitis affects 2% of the general population. In 1989, Goh published a clinical study that included more than 2000 patients. When they found that 34% of them had contact dermatitis on the hands (56% men and 44% women) and 30% of cases the cause was likely professional (8). ❑
CONCLUSIONS
Contact dermatitis is a continuing challenge for the dermatologist. Diagnosis is often easy for patients with acute contact dermatitis, and the etiological agent can be mentioned on the basis of the anamnesis. In the case of subacute or chronic dermatitis, repeated anamnesis, in conjunction with the results of the diagnostic test is the main diagnostic methods.
Once you have identified the causative agent or agents, the preventive measures should be imposed (primary, secondary, tertiary), representing the keystone of successful management of contact dermatitis.
Unfavorable prognosis has allergic contact dermatitis due to some agents, particularly nickel and chromium. Once the contact dermatitis appears, it can persist even if the chemical agent was removed (including by changing workplace). This is explained by the destruction of the skin defense barrier, allowing the penetration of another chemical agent. Another potential cause of resistance is the existence of some threatening unknown allergen, in which case the dermatologic and symptomatic treatment is not effective. No matter of professional or domestic involvement, the general and individual measures of prevention and protection are the key to reduce the cases of this disease in the coming years.
References
- 1.Burns T, Breathnach S, Cox N, et al. Rook's Textbook of Dermatology. 7th ed. 2004 [Google Scholar]
- 2.Dubertret L, Aractingi S, Bachelez H, et al. Thérapeutique dermatologique. Flammarion Médecine-Science. 2001 [Google Scholar]
- 3.Johanssen JD, Frosch PJ, Lepoittevin J-P. Springer-Verlag. Berlin Heidelberg; 2011. Contact Dermatitis, 5th Edition. [Google Scholar]
- 4.Petrescu Z, Branisteanu D, Taranu T, et al. Dermatologie si infectii transmise sexual. Ed. Junimea. 2008 [Google Scholar]
- 5.Schäfer T, Bohler E, Ruhdorfer S, et al. Epidemiology of contact allergy in adults. . Allergy . 2001;56:192–196. doi: 10.1034/j.1398-9995.2001.00086.x. [DOI] [PubMed] [Google Scholar]
- 6.Johnson MLT, Roberts J. Skin conditions and related need for medical care among persons 1-74 years. Vital Health Stat. 1978;11:1–72. [PubMed] [Google Scholar]
- 7.Schimdt RJ. Compositae. Clin Dermatol. 1986;4:46–61. doi: 10.1016/0738-081x(86)90063-5. [DOI] [PubMed] [Google Scholar]
- 8.Goh CL. An epidemiological comparison between occupational and non-occupational hand eczema. Br J Dermatol. 1989;120:77–82. doi: 10.1111/j.1365-2133.1989.tb07768.x. [DOI] [PubMed] [Google Scholar]