Abstract
Study Design
Randomized trial and concurrent observational cohort study
Objective
To compare 4 year outcomes of surgery to non-operative care for spinal stenosis.
Summary of Background Data
Surgery for spinal stenosis has been shown to be more effective compared to non-operative treatment over two years, but longer-term data have not been analyzed.
Methods
Surgical candidates from 13 centers in 11 U.S. states with at least 12 weeks of symptoms and confirmatory imaging were enrolled in a randomized cohort (RC) or observational cohort (OC). Treatment was standard decompressive laminectomy or standard non-operative care. Primary outcomes were SF-36 bodily pain (BP) and physical function (PF) scales and the modified Oswestry Disability index (ODI) assessed at 6 weeks, 3 months, 6 months and yearly up to 4 years.
Results
289 patients enrolled in the RC and 365 patients enrolled in the OC. An as-treated analysis combining the RC and OC and adjusting for potential confounders found that the clinically significant advantages for surgery previously reported were maintained through 4 years, with treatment effects (defined as mean change in surgery group minus mean change in non-op group) for BP 12.6 (95% CI, 8.5 to 16.7); PF 8.6 (95% CI, 4.6 to 12.6); and ODI −9.4 (95% CI, −12.6, to −6.2). Early advantages for surgical treatment for secondary measures such as bothersomeness, satisfaction with symptoms and self-rated progress also were maintained.
Conclusions
Patients with symptomatic spinal stenosis treated surgically compared to those treated non-operatively maintain substantially greater improvement in pain and function through four years.
Keywords: Spinal stenosis, randomized trial, surgery, non-operative, SPORT, outcomes
INTRODUCTION
Spinal stenosis (SpS) patients typically present with radicular leg pain or neurogenic claudication (i.e., pain in the buttocks/legs with walking or standing that resolves with sitting down or lumbar flexion). Lumbar decompression surgery is commonly performed in the United States for patients having back and leg symptoms due to spinal stenosis. 1 Studies have compared surgery to non-operative treatment in SpS; however, these studies typically included a mixed group with and without degenerative spondylolisthesis,2-4 had small sample sizes, limited geographic participation, or lacked non-operative controls and validated outcome measures. 5-7
The special methodological challenges of surgical trials (e.g., compliance with treatment2,5-7) were addressed by SPORT’s trial design, with a randomized cohort (RC) and a concurrent observational cohort (OC) using identical selection criteria and outcomes assessment.8-12 In the SPORT study, as-treated comparisons with careful control for potentially confounding baseline factors showed that patients with spinal stenosis who were treated surgically had substantially greater improvement in pain and function during a period of 2 years than patients treated non-operatively. In this paper, we assess the stability of pain and functional outcomes out to four years for patients with SpS.
MATERIALS AND METHODS
Study Design
SPORT was conducted in 11 states at 13 US medical centers with multidisciplinary spine practices. SPORT included both a randomized cohort and a concurrent observational cohort of patients who declined randomization. 8,9,12-14This design allows for improved generalizability. 15 Additional information is available in previous publications. 2,8,10,11,16,17.
Patient Population
All patients had neurogenic claudication and/or radicular leg symptoms; confirmatory cross-sectional imaging showing lumbar spinal stenosis at one or more levels; and were judged to be surgical candidates. Patients with degenerative spondylolisthesis were studied separately.9,11 Patients with lumbar instability defined as greater than 4mm translation or 10 degrees of angular motion between flexion and extension on upright lateral radiographs were excluded. All patients had ongoing symptoms for a minimum of 12 weeks. The content of pre-enrollment non-operative care was not pre-specified but included: physical therapy (68%); epidural injections (56%); chiropractic (28%); anti-inflammatories, (55%); and opioid analgesics (27%). Enrollment began March 2000 and ended March 2005.
Study Interventions
The protocol surgery consisted of a standard posterior decompressive laminectomy. 8 The non-operative protocol was “usual care” recommended to include at least: active physical therapy, education/counseling with home exercise instruction, and non-steroidal anti-inflammatories if tolerated. 8,18
Study Measures
Primary endpoints were the SF-36 Bodily Pain (BP) and Physical Function (PF) scales, 19-22 and the AAOS/Modems version of the Oswestry Disability Index (ODI) 23 measured at six weeks, three months, six months, and yearly out to four years. If surgery was delayed beyond six weeks, additional follow-up data were obtained six weeks and three months post-operatively. Secondary outcomes included patient self-reported improvement; satisfaction with current symptoms and care;24 stenosis bothersomeness;3,25 and low back pain bothersomeness.3 Treatment effect was defined as the difference in the mean changes from baseline between the surgical and non-operative groups (difference of differences).
The SF-36 scores range from 0 to 100, with higher scores indicating less severe symptoms; the Oswestry Disability Index ranges from 0 to 100, with lower scores indicating less severe symptoms; the Stenosis Bothersomeness Index ranges from 0 to 24, with lower scores indicating less severe symptoms; and the Low Back Pain Bothersomeness Scale ranges from 0 to 6, with lower scores indicating less severe symptoms.
Statistical Considerations
Statistical methods for the analysis of this trial have been reported in previous publications,9-14 and these descriptions are repeated here. Initial analyses compared the baseline characteristics of patients in the randomized cohort with those in the observational cohort and between surgical and non-operative groups in the combined cohorts. The extent of missing data and the percentage of patients undergoing surgery were calculated according to study group for each scheduled follow-up. Baseline predictors of the time until surgical treatment (including treatment crossovers) in both cohorts were determined through a stepwise proportional-hazards regression model with an inclusion criteria of P<0.1 to enter and P>0.05 to exit. Predictors of adherence to treatment and missing follow-up visits at 1, 2, 3 and 4 years were determined through stepwise logistic regression. Primary analyses compared surgical and non-operative treatments with the use of changes from baseline at each follow-up visit, with a mixed effects model of longitudinal regression that included a random individual effect to account for correlation between repeated measurements. The randomized cohort was initially analyzed on an intention-to-treat basis. Because of crossover, subsequent analyses were based on treatments actually received.
In the as-treated analyses, the treatment indicator was a time-varying covariate, allowing for variable times of surgery. For the intention-to-treat analyses, all times are from enrollment. For the as-treated analysis, the times are from the beginning of treatment (i.e., the time of surgery for the surgical group and the time of enrollment for the non operative group). Therefore, all changes from baseline before surgery were included in the estimates of the non-operative treatment effect. After surgery, changes were assigned to the surgical group, with follow-up measured from the date of surgery.
Repeated measures of outcomes were used as the dependent variables, and treatment received was included as a time-varying covariate. Adjustments were made for the time of surgery with respect to the original enrollment date so as to approximate the designated follow-up times. Treatment comparisons were made at designated follow-up time. In addition, a global significance test was based on the time-weighted average/ area under the curve analysis over all time periods.26
As-treated estimates of treatment effect from the RC and OC were compared to establish comparability. Subsequent analyses combined the two cohorts. To adjust for potential confounding, baseline variables that were associated with missing data or treatment received were included as adjusting covariates in longitudinal regression models. Computations were performed with the use of the PROC MIXED procedure for continuous data and the PROC GENMOD procedure for binary and non-normal secondary outcomes in SAS software, version 9.1 (SAS Institute). Statistical significance was defined as p <0.05 on the basis of a two-sided hypothesis test with no adjustments made for multiple comparisons. Data for these analyses were collected through December 8, 2008.
RESULTS
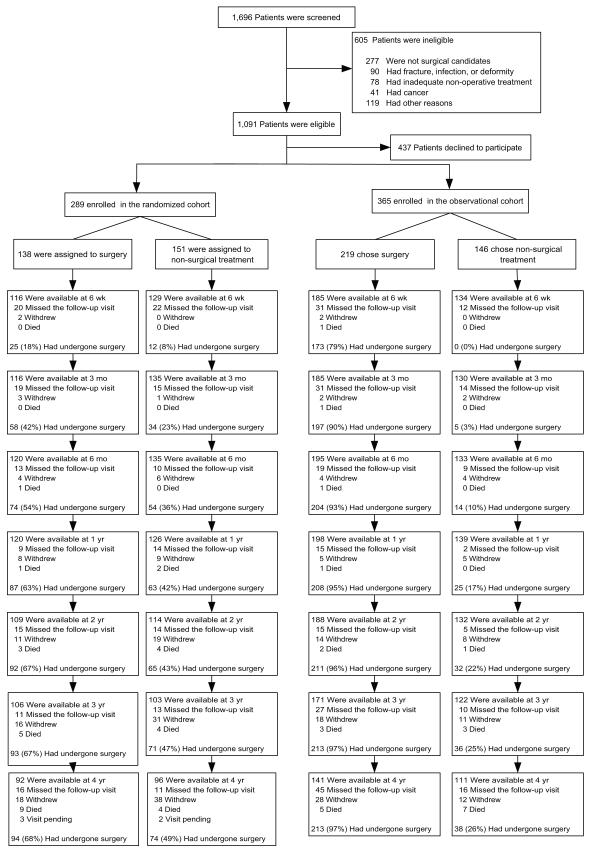
A total of 654 SPORT participants were enrolled out of 1,091 eligible for enrollment (289 in the RC and 365 in the OC) (Figure 1). In the RC, 138 were assigned to surgical treatment and 151 to non-operative treatment. Of those randomized to surgery, 67% received surgery by 2 years, 68% by 4 years. In the group randomized to non-operative care, 43% received surgery by two years, 49% by 4 years (Figure 1). In the OC group, 219 patients initially chose surgery and 146 patients initially chose non-operative care. Of those initially choosing surgery, 96% received surgery by two years and 97% by 4 years. Of those choosing non-operative treatment, 22% had surgery by two years, 26% by 4 years (Figure 1). In both cohorts combined, 419 patients received surgery at some point during the first 4 years; 235 remained non-operative. The proportion of enrollees who supplied data at each follow-up visit interval ranged from 67% to 89% with losses due to dropouts, missed visits, or deaths.
Figure 1.
Patient Characteristics
Table 1 shows the baseline characteristics and clinical findings of participants in the randomized and the observational cohorts. The cohorts were remarkably similar except for their preferences for surgery (p < 0.001), with more RC patients unsure of their preference (34% vs. 7%), and fewer RC patients definitely preferring either surgery (12% vs. 46%) or non-operative treatment (13% vs. 24%).
Table 1.
Patient baseline demographic characteristics, comorbidities, and health status measures according to study cohort and treatment received.
| SPORT Study Cohort | Randomized and Observational Cohorts Combined: Treatment Received* |
|||||
|---|---|---|---|---|---|---|
| Randomized | Observational | Surgery | Non- Operative |
|||
| (n=278) | (n=356) | (n=413) | (n=221) | |||
| Mean Age (stdev) | 65.5 (10.5) | 63.9 (12.5) | 0.098 | 63.8 (12.2) | 66.1 (10.4) | 0.019 |
| Female | 106 (38%) | 143 (40%) | 0.66 | 159 (38%) | 90 (41%) | 0.64 |
| Ethnicity: Not Hispanic† | 259 (93%) | 346 (97%) | 0.027 | 396 (96%) | 209 (95%) | 0.58 |
| Race - White | 238 (86%) | 295 (83%) | 0.41 | 349 (85%) | 184 (83%) | 0.77 |
| Education - At least some college | 176 (63%) | 225 (63%) | 0.96 | 259 (63%) | 142 (64%) | 0.77 |
| Marital Status - Married | 197 (71%) | 249 (70%) | 0.87 | 300 (73%) | 146 (66%) | 0.10 |
| Work Status | 0.12 | 0.32 | ||||
| Full or part time | 88 (32%) | 128 (36%) | 147 (36%) | 69 (31%) | ||
| Disabled | 24 ( 9%) | 36 (10%) | 40 (10%) | 20 ( 9%) | ||
| Retired | 144 (52%) | 152 (43%) | 182 (44%) | 114 (52%) | ||
| Other | 22 ( 8%) | 40 (11%) | 44 (11%) | 18 ( 8%) | ||
| Compensation - Any‡ | 21 (8%) | 27 (8%) | 0.89 | 30 (7%) | 18 (8%) | 0.81 |
| Mean Body Mass Index (BMI), (stdev)§ | 29.8 (5.6) | 29.3 (5.6) | 0.31 | 29.4 (5.3) | 29.8 (6.1) | 0.44 |
| Smoker | 34 (12%) | 28 (8%) | 0.089 | 37 (9%) | 25 (11%) | 0.42 |
| Comorbidities | ||||||
| Hypertension | 134 (48%) | 154 (43%) | 0.25 | 175 (42%) | 113 (51%) | 0.043 |
| Diabetes | 50 (18%) | 46 (13%) | 0.098 | 57 (14%) | 39 (18%) | 0.24 |
| Osteoporosis | 22 (8%) | 38 (11%) | 0.30 | 32 (8%) | 28 (13%) | 0.061 |
| Heart Problem | 80 (29%) | 85 (24%) | 0.19 | 102 (25%) | 63 (29%) | 0.34 |
| Stomach Problem | 60 (22%) | 79 (22%) | 0.93 | 86 (21%) | 53 (24%) | 0.41 |
| Bowel or Intestinal Problem | 36 (13%) | 50 (14%) | 0.78 | 50 (12%) | 36 (16%) | 0.18 |
| Depression | 36 (13%) | 34 (10%) | 0.22 | 46 (11%) | 24 (11%) | 0.98 |
| Joint Problem | 158 (57%) | 188 (53%) | 0.35 | 222 (54%) | 124 (56%) | 0.63 |
| Other¶ | 95 (34%) | 125 (35%) | 0.87 | 143 (35%) | 77 (35%) | 0.97 |
| Time since most recent episode > 6 months | 158 (57%) | 210 (59%) | 0.64 | 245 (59%) | 123 (56%) | 0.42 |
| Bodily Pain (BP) Score∥ | 31.9 (17.5) | 31.4 (17.4) | 0.73 | 28.9 (16.2) | 36.6 (18.6) | <0.001 |
| Physical Functioning (PF) Score | 35.4 (22.6) | 34.3 (23.8) | 0.55 | 31.8 (21.8) | 40.5 (24.8) | <0.001 |
| Mental Component Summary (MCS) Score | 49.8 (12.4) | 49.1 (11.6) | 0.47 | 48.6 (12) | 50.9 (11.7) | 0.023 |
| Oswestry (ODI)** | 42.7 (17.9) | 42.1 (19) | 0.70 | 45.6 (17.9) | 36.3 (18.1) | <0.001 |
| Stenosis Frequency Index (0-24)†† | 13.5 (5.7) | 14.2 (5.8) | 0.13 | 15 (5.5) | 11.8 (5.7) | <0.001 |
| Stenosis Bothersome Index (0-24)‡‡ | 13.9 (5.7) | 14.7 (5.8) | 0.084 | 15.4 (5.4) | 12.4 (5.8) | <0.001 |
| Back Pain Bothersomeness§§ | 4 (1.9) | 4.2 (1.8) | 0.19 | 4.2 (1.8) | 3.8 (1.8) | 0.012 |
| Leg Pain Bothersomeness¶¶ | 4.3 (1.7) | 4.4 (1.7) | 0.44 | 4.5 (1.6) | 3.9 (1.8) | <0.001 |
| Satisfaction with symptoms - very dissatisfied | 183 (66%) | 250 (70%) | 0.27 | 320 (77%) | 113 (51%) | <0.001 |
| Problem getting better or worse | 0.48 | <0.001 | ||||
| Getting better | 18 ( 6%) | 28 ( 8%) | 14 ( 3%) | 32 (14%) | ||
| Staying about the same | 95 (34%) | 108 (30%) | 115 (28%) | 88 (40%) | ||
| Getting worse | 160 (58%) | 218 (61%) | 277 (67%) | 101 (46%) | ||
| Treatment preference | <0.001 | <0.001 | ||||
| Definitely prefer non-surg | 37 (13%) | 86 (24%) | 38 ( 9%) | 85 (38%) | ||
| Probably prefer non-surg | 61 (22%) | 45 (13%) | 43 (10%) | 63 (29%) | ||
| Not sure | 95 (34%) | 26 ( 7%) | 67 (16%) | 54 (24%) | ||
| Probably prefer surgery | 51 (18%) | 36 (10%) | 75 (18%) | 12 ( 5%) | ||
| Definitely prefer surgery | 33 (12%) | 163 (46%) | 190 (46%) | 6 ( 3%) | ||
| Pseudoclaudication - Any | 219 (79%) | 289 (81%) | 0.51 | 334 (81%) | 174 (79%) | 0.59 |
| SLR or Femoral Tension | 41 (15%) | 91 (26%) | 0.001 | 89 (22%) | 43 (19%) | 0.61 |
| Pain radiation - any | 215 (77%) | 284 (80%) | 0.52 | 322 (78%) | 177 (80%) | 0.60 |
| Any Neurological Deficit | 146 (53%) | 203 (57%) | 0.29 | 223 (54%) | 126 (57%) | 0.52 |
| Reflexes - Asymmetric Depressed | 76 (27%) | 92 (26%) | 0.74 | 109 (26%) | 59 (27%) | 0.99 |
| Sensory - Asymmetric Decrease | 68 (24%) | 114 (32%) | 0.046 | 122 (30%) | 60 (27%) | 0.59 |
| Motor - Asymmetric Weakness | 71 (26%) | 106 (30%) | 0.28 | 109 (26%) | 68 (31%) | 0.28 |
| Stenosis Levels | ||||||
| L2-L3 | 77 (28%) | 102 (29%) | 0.86 | 123 (30%) | 56 (25%) | 0.27 |
| L3-L4 | 183 (66%) | 237 (67%) | 0.91 | 278 (67%) | 142 (64%) | 0.49 |
| L4-L5 | 255 (92%) | 324 (91%) | 0.86 | 380 (92%) | 199 (90%) | 0.49 |
| L5-S1 | 72 (26%) | 101 (28%) | 0.55 | 105 (25%) | 68 (31%) | 0.18 |
| Stenotic Levels (Mod/Severe) | 0.45 | 0.15 | ||||
| None | 4 ( 1%) | 11 ( 3%) | - | 6 ( 1%) | 9 ( 4%) | - |
| One | 106 (38%) | 128 (36%) | - | 148 (36%) | 86 (39%) | - |
| Two | 109 (39%) | 132 (37%) | - | 162 (39%) | 79 (36%) | - |
| Three+ | 59 (21%) | 85 (24%) | - | 97 (23%) | 47 (21%) | - |
| Stenosis Locations | ||||||
| Central | 241 (87%) | 302 (85%) | 0.58 | 357 (86%) | 186 (84%) | 0.51 |
| Lateral Recess | 236 (85%) | 267 (75%) | 0.003 | 334 (81%) | 169 (76%) | 0.23 |
| Neuroforamen | 88 (32%) | 119 (33%) | 0.70 | 124 (30%) | 83 (38%) | 0.066 |
| Stenosis Severity | 0.24 | 0.006 | ||||
| Mild | 4 ( 1%) | 11 ( 3%) | - | 6 ( 1%) | 9 ( 4%) | - |
| Moderate | 131 (47%) | 151 (42%) | - | 171 (41%) | 111 (50%) | - |
| Severe | 143 (51%) | 194 (54%) | - | 236 (57%) | 101 (46%) | - |
Patients in the two cohorts combined were classified according to whether they received surgical treatment or only nonsurgical treatment during the first 4 years of enrollment.
Race or ethnic group was self-assessed. Whites and blacks could be either Hispanic or non-Hispanic.
This category includes patients who were receiving or had applications pending for workers compensation, Social Security compensation, or other compensation.
The body-mass index is the weight in kilograms divided by the square of the height in meters.
Other = problems related to stroke, cancer, fibromyalgia, CGS, PTSD, alcohol, drug dependency, lung, liver, kidney, blood vessel, nervous system, migraine or anxiety.
The SF-36 scores range from 0 to 100, with higher score indicating less severe symptoms.
The Oswestry Disability Index ranges from 0 to 100, with lower scores indicating less severe symptoms.
The Stenosis Frequency Index ranges from 0 to 24, with lower scores indicating less severe symptoms.
The Stenosis Bothersomeness Index ranges from 0 to 24, with lower scores indicating less severe symptoms.
The Low Back Pain Bothersomness Scale ranges from 0 to 6, with lower scores indicating less severe symptoms
The Leg Pain Bothersomeness Scale ranges from 0 to 6, with lower scores indicating less severe symptoms.
Summary statistics for the combined cohorts are also shown in Table 1 according to treatment received. At baseline, patients in the group undergoing surgery within 4 years from the combined randomized and observational cohorts were younger than those receiving non-operative treatment. They had worse pain, function, disability, and symptoms than patients in the non-operative group. Patients in the surgery group were more dissatisfied with their symptoms and at enrollment more often rated their symptoms as worsening and definitely preferred surgery. These observations highlight the need to control for baseline differences in the adjusted models. Based on the selection procedure for variables associated with treatment, missing data and outcomes, the final as-treated models controlled for the following covariate: center; age; gender; baseline score (for SF-36, ODI); income; treatment preference; current duration of symptoms; compensation; smoking status; BMI; baseline sciatica bothersomeness; joint; stomach; and bowel (Table 4).
Table 4.
Primary analysis results for years 3 and 4. Intent-to-treat for the randomized cohort and adjusted* analyses according to treatment received for the randomized and observational cohorts combined. ‡‡
| Baseline | 2-Year | 3-Year | 4-Year | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Overall Mean |
Mean Change (SE) or percent |
Mean Change (SE) or percent |
Mean Change (SE) or percent |
|||||||
|
|
|
|
||||||||
| Surgery | Non- Operative |
Treatment Effect (95% CI)† |
Surgery | Non- Operative |
Treatment Effect (95% CI)† |
Surgery | Non- Operative |
Treatment Effect (95% CI)† |
||
|
RCT Intent-to-treat
Primary Outcomes |
(n = 109) | (n = 114) | (n = 106) | (n = 103) | (n = 92) | (n = 96) | ||||
|
| ||||||||||
| SF-36 Bodily Pain (BP) (0-100) (SE)‡ | 31.9 (1.1) | 23.2 (2.3) | 15.4 (2.2) | 7.8 (1.4, 14.1) |
21 (2.4) | 16.6 (2.3) | 4.4 (−2.1, 10.9) |
15.9 (2.4) | 15.7 (2.4) | 0.3 (−6.4, 7) |
|
| ||||||||||
| SF-36 Physical Function (PF) (0-100) (SE)‡ |
35.4 (1.4) | 16.7 (2.4) | 17 (2.3) | −0.3 (−6.7, 6.1) |
17.1 (2.4) | 14.4 (2.3) | 2.6 (−4, 9.2) | 12.7 (2.5) | 15.9 (2.4) | −3.2 (−9.9, 3.6) |
|
| ||||||||||
| Oswestry Disability Index (ODI) (0-100) (SE)§ |
42.7 (1.1) | −16.1 (1.9) | −12.7 (1.8) | −3.4 (−8.5, 1.8) |
−14.7 (2) | −13.3 (1.9) |
−1.4 (−6.8, 3.9) |
−12.2 (2) | −12.4 (1.9) | 0.2 (−5.2, 5.7) |
|
| ||||||||||
| Secondary Outcomes | ||||||||||
|
| ||||||||||
| Sciatica Bothersomeness Index (0-24) (SE)¶ |
13.9 (0.35) | −6 (0.71) | −5.4 (0.69) | −0.5 (−2.5, 1.4) |
−6 (0.73) | −4.9 (0.71) |
−1 (−3.1, 1) | −5.2 (0.75) |
−4.5 (0.73) | −0.7 (−2.8, 1.4) |
|
| ||||||||||
| Leg pain (0-6) (SE)∥ | 4.3 (0.1) | −2 (0.2) | −1.8 (0.2) | −0.2 (−0.8, 0.4) |
−2.2 (0.2) | −1.6 (0.2) | −0.6 (−1.2, 0) | −1.8 (0.2) | −1.8 (0.2) | 0 (−0.7, 0.6) |
|
| ||||||||||
| Low back pain bothersomeness (0-6) (SE)** |
4 (0.1) | −1.2 (0.2) | −1.6 (0.2) | 0.4 (−0.2, 0.9) |
−1.2 (0.2) | −1.3 (0.2) | 0.1 (−0.4, 0.7) | −0.9 (0.2) | −1.3 (0.2) | 0.4 (−0.2, 1) |
|
| ||||||||||
| Very/somewhat satisfied w/ symptoms (%) |
5 (2.2) | 53.1 | 43.3 | 9.8 (−3.3, 22.9) |
56.6 | 45.2 | 11.5 (−2.1, 25.1) |
48.2 | 43.8 | 4.5 (−9.6, 18.6) |
|
| ||||||||||
| Very/somewhat satisfied w/ care(%) | 75.9 | 67.6 | 8.3 (−3.6, 20.2) |
79.6 | 62.8 | 16.8 (4.5, 29.2) |
69.4 | 70.6 | −1.2 (− 14.5, 12.2) |
|
|
| ||||||||||
| Self-rated progress: major improvement (%) |
49.4 | 43.5 | 5.9 (−7.3, 19.2) |
47.2 | 42.7 | 4.5 (−9.1, 18.2) |
42.3 | 33.9 | 8.3 (−5.4, 22.1) |
|
|
RCT/OC As-treated
Primary Outcomes |
(n = 350) | (n = 199) | (n = 326) | (n = 171) | (n = 275) | (n = 144) | ||||
|
| ||||||||||
| SF-36 Bodily Pain (BP) (0-100) (SE)‡ | 31.4 (0.6) | 27 (1.2) | 12.9 (1.5) | 14 (10.5, 17.6) |
26.8 (1.2) | 13.4 (1.6) | 13.4 (9.6, 17.1) |
25.1 (1.3) | 12.5 (1.7) | 12.6 (8.5, 16.7) |
|
| ||||||||||
| SF-36 Physical Function (PF) (0-100) (SE)‡ |
34.9 (0.8) | 22.2 (1.3) | 12.7 (1.5) | 9.5 (6, 13) | 20.9 (1.3) | 10.4 (1.6) | 10.4 (6.7, 14.1) |
20.3 (1.3) | 11.6 (1.7) | 8.6 (4.6, 12.6) |
|
| ||||||||||
| Oswestry Disability Index (ODI) (0-100) (SE)§ |
43.2 (0.6) | −20.3 (0.98) | −9.4 (1.2) | −10.9 (−13.7, -8.1) |
−18.6 (0.98) |
−9.1 (1.2) | −9.4 (−12.4, − 6.5) |
−18.7 (1.1) |
−9.3 (1.3) | −9.4 (−12.6, -6.2) |
|
| ||||||||||
| Secondary Outcomes | ||||||||||
|
| ||||||||||
| Sciatica Bothersomeness Index (0-24) (SE)¶ |
14.5 (0.2) | −8 (0.35) | −4.2 (0.43) | −3.8 (−4.9, − 2.8) |
−7.7 (0.35) | −4.4 (0.46) |
−3.2 (−4.3, − 2.1) |
−7.6 (0.39) |
−4.1 (0.49) | −3.5 (−4.7, − 2.3) |
|
| ||||||||||
| Leg pain (0-6) (SE)∥ | 4.3 (0.1) | −2.6 (0.1) | −1.3 (0.1) | −1.3 (−1.6, − 1) |
−2.5 (0.1) | −1.6 (0.1) | −1 (−1.3, -0.6) | −2.5 (0.1) | −1.4 (0.2) | −1.1 (−1.5, − 0.7) |
|
| ||||||||||
| Low back pain bothersomeness (0-6) (SE)** |
4.1 (0.1) | −2.1 (0.1) | −1 (0.1) | −1.1 (−1.4, − 0.8) |
−1.9 (0.1) | −0.9 (0.1) | −1 (−1.3, -0.7) | −1.8 (0.1) | −0.9 (0.1) | −0.8 (−1.2, − 0.5) |
|
| ||||||||||
| Very/somewhat satisfied w/ symptoms (%) |
5.8 (2.3) | 69.3 | 28.3 | 41 (32.5, 49.5) |
65.5 | 35.8 | 29.7 (20.4, 39.1) |
63.1 | 32.2 | 31 (20.9, 41) |
|
| ||||||||||
| Very/somewhat satisfied w/ care(%) | 82.5 | 66.2 | 16.3 (7.9, 24.6) |
83.6 | 61.8 | 21.9 (12.8, 30.9) |
77.8 | 63.6 | 14.3 (4.1, 24.5) |
|
|
| ||||||||||
| Self-rated progress: major improvement (%) |
63.6 | 27.9 | 35.8 (27.3, 44.2) |
61 | 28.5 | 32.5 (23.6, 41.4) |
52.8 | 23.1 | 29.6 (20.3, 39) |
|
Adjusted for center, age, gender, baseline score, income, treatment preference, duration of symptoms, compensation, smoking status, BMI, baseline Sciatica Bothersomeness, joint, stomach and bowel.
Treatment effect is the difference between the surgical and non-operative mean change from baseline.
The SF-36 scores range from 0 to 100, with higher score indicating less severe symptoms.
The Oswestry Disability Index ranges from 0 to 100, with lower scores indicating less severe symptoms
The Stenosis Bothersomeness Index ranges from 0 to 24, with lower scores indicating less severe symptoms
The Leg Pain Bothersomeness Scale ranges from 0 to 6, with lower scores indicating less severe symptoms
The Low Back Pain Bothersomeness Scale ranges from 0 to 6, with lower scores indicating less severe symptoms
The sample sizes for the as-treated analyses reflect the number of patients contributing to the estimate in a given time-period using the longitudinal modeling strategy explained in the methods section, and may not correspond to the counts provided for each visit time in Figure 1.
The estimates for 1Y and 2Y for IDH RCT ITT differ slightly from those presented in NEJM paper (reference) due to modeling differences.
Non-Operative Treatments
Non-operative treatments used during SPORT included physical therapy (44%); visits to a surgeon (46%); nonsteroidal anti-inflammatory drugs (49%); and opioids (37%); More patients in the randomized cohort reported receiving injections (54% vs. 41%, p=0.02) while more observational patients reported receiving other medications (74% vs. 62%, p=0.02). Pre-enrollment there were no significant differences in non-operative treatments received between the RCT and OBS cohorts.
Surgical Treatment and Complications
The mean surgical time was 129 minutes, with a mean blood loss of 311 ml (Table 2). There was no significant difference between the cohorts in rates of intraoperative blood replacement, or postoperative transfusion rates. The most common surgical complication was dural tear (9%). The 4-year reoperation rate was 13%.
Table 2.
Operative treatments, complications and events.
| Randomized Cohort (n=166*) |
Observational Cohort (n=245) |
p-value | |
|---|---|---|---|
| Procedure | 0.53 | ||
| Decompression only | 142 (88%) | 213 (88%) | |
| Non-instrumented fusion | 7 ( 4%) | 15 ( 6%) | |
| Instrumented fusion | 12 ( 7%) | 13 ( 5%) | |
| Multi-level fusion | 5 (3%) | 11 (4%) 0.62 | |
| LaminectomyLevel | |||
| L2-L3 | 57 (35%) | 90 (37%) | 0.74 |
| L3-L4 | 123 (76%) | 159 (66%) | 0.043 |
| L4-L5 | 149 (92%) | 224 (93%) | 0.86 |
| L5-S1 | 62 (38%) | 91 (38%) | 1 |
| Levels decompresssed | 0.81 | ||
| 0 | 4 ( 2%) | 4 ( 2%) | - |
| 1 | 35 (21%) | 58 (24%) | - |
| 2 | 50 (30%) | 78 (32%) | - |
| 3+ | 77 (46%) | 105 (43%) | - |
| Operation time | 129 (64.1) | 128.6 (67) | 0.96 |
| Blood loss | 333.2 (515.3) | 296.9 (310.4) | 0.38 |
| Blood Replacement | |||
| Intraoperative replacement | 15 (9%) | 24 (10%) | 1 |
| Post-operative transfusion | 7 (4%) | 13 (5%) | 0.82 |
| Lenth of stay | 3.5 (2.6) | 3 (2.2) | 0.023 |
| Post-operative mortality (death within 6 weeks of surgery) |
0 (0%) | 1 (0.4%)‡ | 0.84 |
| Post-operative mortality (death within 3 months of surgery) |
0 (0%) | 1 (0.4%)‡ | 0.84 |
| Intraoperative complications§ | |||
| Dural tear/ spinal fluid leak | 15 (9%) | 23 (9%) | 0.95 |
| Other | 1 (1%) | 2 (1%) | 0.73 |
| None | 149 (90%) | 219 (90%) | 0.99 |
| Postoperative complications/events¶ | |||
| Wound hematoma | 3 (2%) | 1 (0%) | 0.35 |
| Wound infection | 4 (2%) | 5 (2%) | 0.95 |
| Other | 10 (6%) | 14 (6%) | 0.97 |
| None | 141 (87%) | 213 (87%) | 0.94 |
| Additional surgeries (1-year rate)∥ | 7 (4%) | 15 (6%) | 0.41 |
| Additional surgeries (2-year rate)∥ | 11 (7%) | 21 (8%) | 0.48 |
| Additional surgeries (3-year rate)∥ | 17 (10%) | 29 (12%) | 0.64 |
| Additional surgeries (4-year rate)∥ | 22 (13%) | 32 (13%) | 0.94 |
| Recurrent stenosis/progressive spondylolisthesis | 15 (9%) | 9 (4%) | |
| Pseudoarthrosis/fusion exploration | 0 (0%) | 0 (0%) | |
| Complication or Other | 6 (4%) | 12 (5%) | |
| New condition | 1 (NE) | 7 (3%) |
171 RCT and 252 OBS patients had surgery, surgical information was available for 166 RCT patients and 245 observational patients. Specific procedure information was available on 161 RCT and 241 OBS patients.
Patient died 9 days after surgery of a myocardial infarction. The death was juded probably related to treatment by the DHMC review and not related to treatment by the external review.
None of the following were reported: aspiration, nerve root injury, operation at wrong level, vascular injury.
Any reported complications up to 8 weeks post operation. None of the following were reported: bone graft complication, CSF leak, nerve root injury, paralysis, cauda equina injury, wound dehiscence, pseudarthrosis.
One-, two-, three- and four-year post-surgical re-operation rates are Kaplan Meier estimates and p-values are based on the log-rank test. Numbers and percentages are based on the first additional surgery if more than one additional surgery. Surgeries include any additional spine surgery not just re-operation at the same level.
Over four years, there were 12 deaths in the non-operative group within 4 years of enrollment compared to 23 expected based on age-gender specific mortality rates, and 15 deaths in the surgery group within 4 years of surgery, compared to 29 expected. The hazard ratio based on a proportional hazards model adjusted for age was 0.7 (95% CI: 0.32, 1.6); p=0.43. All 27 deaths were independently reviewed and 23 were judged not to be treatment-related. Four deaths were of unknown cause and unknown treatment relation but occurred 1203, 1192, 855, 501 days post-surgery/enrollment. Three of these deaths were in patients who had had surgery and one was in a patient who had not had surgery.
Cross Over
Non-adherence to treatment assignment affected both arms: patients chose to delay or decline surgery in the surgical arm and crossed over to surgery in the non-operative arm (Figure 1). The characteristics of cross over patients that were statistically different from patients who did not cross over are shown in Table 3. Patients who crossed over to non-operative care were: less likely to be white; less bothered by their symptoms; more likely to judge their symptoms as improving at baseline; and had stronger baseline treatment preferences for non-operative care. Patients crossing over to surgery: had lower mental component summary scores, were more disabled and bothered by their symptoms, were less satisfied by their symptoms, and had stronger baseline preference for surgery.
Table 3.
Statistically significant predictors of adherence to treatment among RCT patients.
| Assigned to Surgery | Assigned to Non-operative | |||||
|---|---|---|---|---|---|---|
| Treatment Received within 4 Years |
p-value | Treatment Received within 4 Years |
p-value | |||
| Surgery | Non- operative |
Surgery | Non-operative | |||
| (n=91) | (n=41) | (n=73) | (n=73) | |||
| Race - White | 81 (89%) | 28 (68%) | 0.008 | 67 (92%) | 62 (85%) | 0.30 |
| Comorbidities | ||||||
| Hypertension | 41 (45%) | 27 (66%) | 0.04 | 31 (42%) | 35 (48%) | 0.62 |
| Mental Component Summary (MCS) Score | 50 (12.1) | 50.3 (14.2) | 0.88 | 47.1 (12.7) | 52 (10.9) | 0.012 |
| Oswestry (ODI) | 44.7 (18) | 38.3 (19.1) | 0.07 | 46 (18.3) | 39.3 (15.8) | 0.019 |
| Stenosis Frequency Index (0-24) | 14.6 (5.4) | 11.8 (6.3) | 0.009 | 14.3 (5.5) | 12.1 (5.5) | 0.019 |
| Stenosis Bothersome Index (0-24) | 14.9 (4.9) | 12.1 (6.1) | 0.007 | 15 (5.5) | 12.5 (6.1) | 0.011 |
| Leg Pain Bothersomeness | 4.5 (1.6) | 4 (1.9) | 0.08 | 4.5 (1.5) | 3.9 (1.8) | 0.049 |
| Satisfaction with symptoms - very dissatisfied | 67 (74%) | 23 (56%) | 0.07 | 56 (77%) | 37 (51%) | 0.002 |
| Problem getting better or worse | 0.007 | 0.15 | ||||
| Getting better | 2 ( 2%) | 6 (15%) | 2 ( 3%) | 8 (11%) | ||
| Staying about the same | 28 (31%) | 17 (41%) | 25 (34%) | 25 (34%) | ||
| Getting worse | 58 (64%) | 18 (44%) | 44 (60%) | 40 (55%) | ||
| Treatment preference | 0.02 | <0.001 | ||||
| Definitely prefer non-surg | 9 (10%) | 8 (20%) | 7 (10%) | 13 (18%) | ||
| Probably prefer non-surg | 16 (18%) | 14 (34%) | 12 (16%) | 19 (26%) | ||
| Not sure | 32 (35%) | 12 (29%) | 19 (26%) | 32 (44%) | ||
| Probably prefer surgery | 23 (25%) | 7 (17%) | 17 (23%) | 4 ( 5%) | ||
| Definitely prefer surgery | 11 (12%) | 0 ( 0%) | 18 (25%) | 4 ( 5%) | ||
The SF-36 scores range from 0 to 100, with higher score indicating less severe symptoms.
The Oswestry Disability Index ranges from 0 to 100, with lower scores indicating less severe symptoms.
The Stenosis Frequency Index ranges from 0 to 24, with lower scores indicating less severe symptoms.
The Stenosis Bothersomeness Index ranges from 0 to 24, with lower scores indicating less severe symptoms.
The Leg Pain Bothersomeness Scale ranges from 0 to 6, with lower scores indicating less severe symptoms.
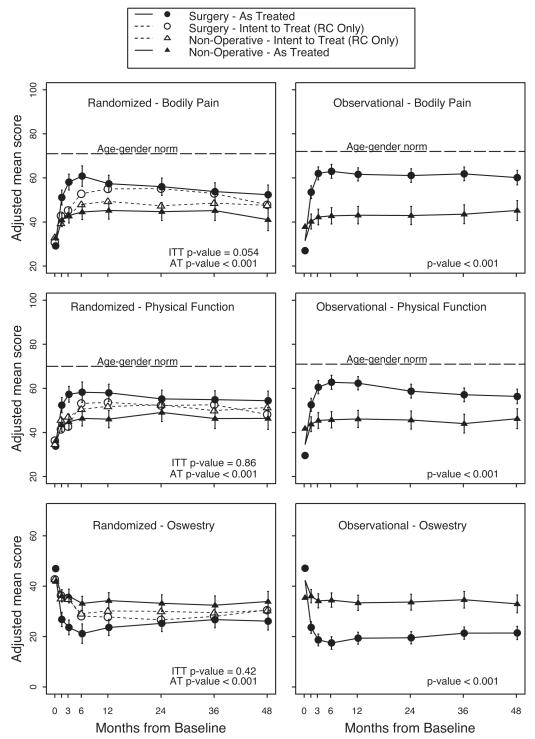
Main Treatment effects
The intent-to-treat analysis of the randomized cohort showed no statistical differences between surgery and non-operative care based on overall global hypothesis tests for differences in mean changes from baseline (Figure 2). The randomized and observational cohorts’ as-treated treatment effects were similar at 4 years (Figure 2):
Bodily Pain: RC 11.4 (95% CI, 5.1 to 17.6) vs. OC 14.9 (95% CI, 9.3 to 20.5);
Physical Function: RC 8.0 (95% CI, 1.7 to 14.3) vs. OC 10.1 (95% CI, 4.7 to 15.5); and
Oswestry Disability Index: RC −7.8 (-12.9, −2.6) vs. OC −11.5 (-15.8, −7.3).
The global hypothesis test comparing the as-treated RC and OC treatment effects over all time periods showed no difference between the cohorts (p = 0.27 for BP; p = 0.56 for PF; and p= 0.25 for ODI).
Figure 2.
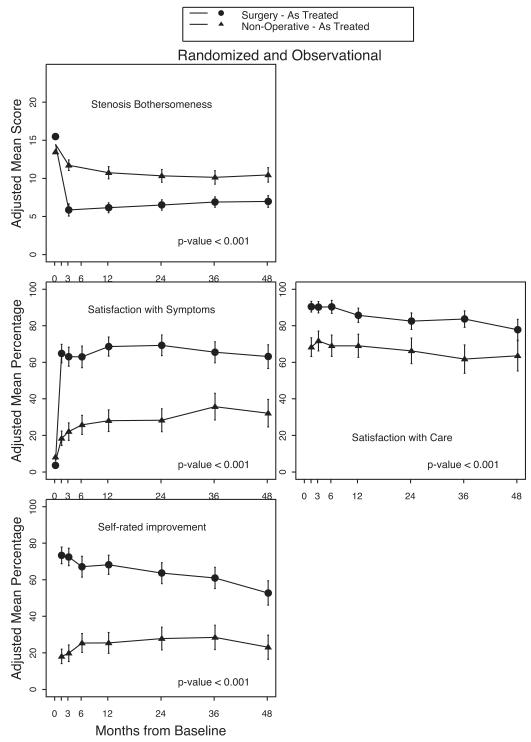
Results from the intent-to-treat and as-treated analyses of the two cohorts are compared in Figure 2. The as-treated treatment effects significantly favored surgery in both cohorts. In the combined analysis, treatment effects were statistically significant in favor of surgery for all primary and secondary outcome measures at each time point out to four years (Table 4). At 4 years the treatment effect for bodily pain was 12.6 (95%CI, 8.5 to 16.7) for physical function was 8.6 (95%CI, 4.6 to 12.6) and for Oswestry Disability Index was −9.4 (95%CI, −12.6 to −6.2).
Table 5 shows the proportion of patients in the as-treated comparison of surgery versus non-operative care who achieved at least a 15-point improvement in the ODI at 1 and 4 years respectively. 23 These proportions at 4 years (61% in surgery group, 32% in non-operative group) are quite similar to the proportions rating themselves as being very/somewhat satisfied with their symptoms (63% in the surgery group, 32% in the non-operative group) and having had a major improvement (53% in surgery group, 23% in non-operative group).
Table 5.
Proportion of patients who had a change of ≥ 15 on the ODI at 1-year and 4-years from baseline. Based on the adjusted as-treated analysis for the randomized and observational cohorts combined, according to treatment received.
| Surgery | Nonoperative | Treatment Effect (95% CI) | p-value | |
|---|---|---|---|---|
| At 1-Year | 64.7% | 30.7% | 33.9% (26.1, 41.7) | <0.001 |
| At 4-Year | 60.6% | 32.4% | 28.2% (18.6, 37.7) | <0.001 |
DISCUSSION
In patients presenting with signs and symptoms of image confirmed spinal stenosis (SpS) persisting for at least twelve weeks, the intention-to-treat analysis found no significant advantage for surgery over non-operative treatment. These results must be viewed in the context of substantial rates of non-adherence to the assigned treatment. This mixing of treatments generally biases treatment effect estimates towards the null.8-14
In the as-treated analysis, the treatment effect in favor of surgery suggests the intention-to-treat analysis underestimates the true effect of surgery. The effect was seen as early as six weeks, appeared maximal by 3-12 months and has persisted over four years. The non-operative treatment group demonstrated only modest improvement over time. The results in both treatment groups were maintained between two and four years.
This study provides an opportunity to compare results involving patients who were willing to participate in a randomized study (randomized cohort) and those who were unwilling to participate in such a study (observational cohort). These two cohorts were remarkably similar at baseline. Other than treatment preference the only significant differences at baseline were small ones: location of stenosis, tension signs and sensory findings. The cohorts also had similar outcomes, with no significant differences between the treatment effects in the as-treated analyses, supporting the validity of the combined analysis. Although these analyses are not based entirely on randomized treatment assignments, the results are strengthened by the use of specific inclusion and exclusion criteria, the sample size, and the adjustment for potentially confounding baseline factors.10-12
Comparisons to Other Studies
SPORT represents the largest study of its kind, and the largest study to isolate spinal stenosis from stenosis secondary to degenerative spondylolisthesis. Its cohort was recruited from 13 centers in 11 states, making it the most heterogeneous study of stenosis, and its inclusion and exclusion criteria were the most rigorous to date. The characteristics of the participants and the short term outcomes of SPORT as previously reported are comparable to studies both of isolated spinal stenosis and of mixed cohorts of patients with and without degenerative spondylolisthesis with stenosis.9, 11, 12
The surgical outcomes in SPORT were generally similar to those in previous surgical series. Herkowitz and Kurz 7 reported absolute improvements of 33% for back pain and 55% for leg pain (6-point scales) at an average of 3 years, similar to the changes of 26% and 36 %, respectively (7-point scales), seen in SPORT at 4 years. The improvement at 4 years in the patients in SPORT who were undergoing surgery for isolated spinal stenosis were also similar to the outcomes of surgery in the Maine Lumbar Spine Study (MLSS) mixed-stenosis (those with and those without degenerative spondylolisthesis) cohort.27 The improvement in the stenosis bothersomeness index, leg pain and low back pain bothersomeness respectively were: −7.6, −2.5 and −1.8 in SPORT vs. −9.4, −3.5 and −1.7 in the MLSS.
There was little evidence of harm from either treatment. In the interval between 2 and 4 years there have not been any cases of paralysis in either the surgical or non-operative group. The 4-year rate of re-operation for recurrent stenosis was 6% and the overall re-operation rate increased from 8% at 2 years to 13% at 4 years; compared to 6.2% at 4 years in the MLSS. The perioperative mortality rate remained unchanged at 0.2%, nearly identical to 0.24% seen in Washington State Commission Hospital Abstract Reporting System patients after surgery.28
The 4-year mortality rate was similar in both treatment groups and was lower than actuarial projections. It should be noted that higher rates of complications have been reported with increasing age and coexisting medical conditions. 29
CONCLUSION
In the as-treated analysis combining the randomized and observational cohorts of patients with spinal stenosis (SpS), those treated surgically showed significantly greater improvement in pain, function, satisfaction, and self-rated progress over four years compared to patients treated non-operatively. Results in both groups were stable between two and four years.
Key Points.
Many previous trials of spinal stenosis surgical treatment have had one or more important limitations: mixed diagnosis, small sample size, no non-operative control or lack of validated outcome measures.
In both cohorts combined, 419 patients received surgery at some point during the first 4 years; 235 remained non-operative. The proportion of enrollees who supplied data at each follow-up visit interval ranged from 67% to 89% with losses due to dropouts, missed visits, or deaths.
An as-treated analysis combining the randomized and observational cohorts and adjusting for potential confounders found that the clinically significant advantages for surgery previously reported were maintained through 4 years.
Figure 3.
Acknowledgments
Funding: The National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01-AR45444) and the Office of Research on Women’s Health, the National Institutes of Health, and the National Institute of Occupational Safety and Health, the Centers for Disease Control and Prevention.
Footnotes
Trial Registration: Spine Patient Outcomes Research Trial (SPORT): Spinal Stenosis; #NCT00000411; http://www.clinicaltrials.gov/
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Weinstein JN, Lurie JD, Olson PR, et al. United States’ trends and regional variations in lumbar spine surgery: 1992-2003. Spine. 2006;31:2707–14. doi: 10.1097/01.brs.0000248132.15231.fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Malmivaara A, Slatis P, Heliovaara M, et al. Surgical or nonoperative treatment for lumbar spinal stenosis?: a randomized controlled trial. Spine. 2007;32:1–8. doi: 10.1097/01.brs.0000251014.81875.6d. [DOI] [PubMed] [Google Scholar]
- 3.Atlas SJ, Deyo RA, Keller RB, et al. The Maine Lumbar Spine Study, Part III. 1-year outcomes of surgical and nonsurgical management of lumbar spinal stenosis. Spine. 1996;21:1787–94. doi: 10.1097/00007632-199608010-00012. discussion 94-5. [DOI] [PubMed] [Google Scholar]
- 4.Arega A, Birkmeyer NJ, Lurie JD, et al. Racial variation in treatment preferences and willingness to randomize in the Spine Patient Outcomes Research Trial (SPORT) Spine. 2006;31:2263–9. doi: 10.1097/01.brs.0000232708.66608.ac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bridwell KH, Sedgewick TA, O’Brien MF, et al. The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disord. 1993;6:461–72. doi: 10.1097/00002517-199306060-00001. [DOI] [PubMed] [Google Scholar]
- 6.Fischgrund JS, Mackay M, Herkowitz HN, et al. 1997 Volvo Award winner in clinical studies. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine. 1997;22:2807–12. doi: 10.1097/00007632-199712150-00003. [DOI] [PubMed] [Google Scholar]
- 7.Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. 1991;73:802–8. [PubMed] [Google Scholar]
- 8.Birkmeyer NJ, Weinstein JN, Tosteson AN, et al. Design of the Spine Patient outcomes Research Trial (SPORT) Spine. 2002;27:1361–72. doi: 10.1097/00007632-200206150-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med. 2007;356:2257–70. doi: 10.1056/NEJMoa070302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT) Spine. 2008;33:2789–800. doi: 10.1097/BRS.0b013e31818ed8f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus Non-Operative Treatment for Lumbar Degenerative Spondylolisthesis: Four-Year Results of the Spine Patient Outcomes Research Trial (SPORT) Randomized and Observational Cohorts. J Bone Joint Surg Am Accepted. 2008 doi: 10.2106/JBJS.H.00913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med. 2008;358:794–810. doi: 10.1056/NEJMoa0707136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. Jama. 2006;296:2451–9. doi: 10.1001/jama.296.20.2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. Jama. 2006;296:2441–50. doi: 10.1001/jama.296.20.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tunis SR, Stryer DB, Clancy CM. Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. Jama. 2003;290:1624–32. doi: 10.1001/jama.290.12.1624. [DOI] [PubMed] [Google Scholar]
- 16.Johnsson KE, Uden A, Rosen I. The effect of decompression on the natural course of spinal stenosis. A comparison of surgically treated and untreated patients. Spine. 1991;16:615–9. doi: 10.1097/00007632-199106000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Malmivaara A, Statis P, Heliovaara M, et al. International Society for Study of the Lumbar Spine (ISSLS) Porto, Portugal: 2004. Surgical treatment for moderate lumbar spinal stenosis: A randomized controlled trial. [Google Scholar]
- 18.Cummins J, Lurie JD, Tosteson TD, et al. Descriptive epidemiology and prior healthcare utilization of patients in The Spine Patient Outcomes Research Trial’s (SPORT) three observational cohorts: disc herniation, spinal stenosis, and degenerative spondylolisthesis. Spine. 2006;31:806–14. doi: 10.1097/01.brs.0000207473.09030.0d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McHorney CA, Ware JE, Jr., Lu JF, et al. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Stewart AL, Greenfield S, Hays RD, et al. Functional status and well-being of patients with chronic conditions. Results from the Medical Outcomes Study. Jama. 1989;262:907–13. [PubMed] [Google Scholar]
- 21.Ware J, Sherbourne D. The MOS 36-item short-form health survey. Medical Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 22.Ware JJ. SF-36 Health Survey: Manual and Interpretation Guide. Nimrod Press; Boston, MA: 1993. [Google Scholar]
- 23.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25:2940–52. doi: 10.1097/00007632-200011150-00017. discussion 52. [DOI] [PubMed] [Google Scholar]
- 24.Deyo RA, Diehl AK. Patient satisfaction with medical care for low-back pain. Spine. 1986;11:28–30. doi: 10.1097/00007632-198601000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Patrick DL, Deyo RA, Atlas SJ, et al. Assessing health-related quality of life in patients with sciatica. Spine. 1995;20:1899–908. doi: 10.1097/00007632-199509000-00011. [DOI] [PubMed] [Google Scholar]
- 26.Fitzmaurice G, Laird N, Ware J. Applied Longitudinal Analysis. John Wiley & Sons; Philadelphia, PA: 2004. [Google Scholar]
- 27.Atlas SJ, Keller RB, Robson D, et al. Surgical and nonsurgical management of lumbar spinal stenosis: four-year outcomes from the maine lumbar spine study. Spine. 2000;25:556–62. doi: 10.1097/00007632-200003010-00005. [DOI] [PubMed] [Google Scholar]
- 28.Deyo RA, Cherkin DC, Loeser JD, et al. Morbidity and mortality in association with operations on the lumbar spine. The influence of age, diagnosis, and procedure. J Bone Joint Surg Am. 1992;74:536–43. [PubMed] [Google Scholar]
- 29.Ciol MA, Deyo RA, Howell E, et al. An assessment of surgery for spinal stenosis: time trends, geographic variations, complications, and reoperations. J Am Geriatr Soc. 1996;44:285–90. doi: 10.1111/j.1532-5415.1996.tb00915.x. [DOI] [PubMed] [Google Scholar]