Abstract
Since the first laparoscopic gastrectomy for cancer was reported in 1994, minimally invasive surgery is enjoying its wide acceptance. Numerous procedures of this approach have developed, and many patients have benefited from its effectiveness, which has been recently demonstrated for early gastric cancer. However, since laparoscopic surgery is not exempt from some limitations, the robotic surgery system was introduced as a solution by the late 1990's. Many experienced surgeons have embraced this new emerging method that provides undoubted technical and minimally invasive advantages. To date, several studies have concentrated to this new system, and have compared it with open and laparoscopic approach. Most of them have reported satisfactory results concerning the post-operative short-term outcomes, but almost all believe that the role of robotic gastrectomy is still out of focus, especially because long-term outcomes that can prove robotic oncologic equivalency are lacking, and operative costs and time are higher in comparison to the open and laparoscopic ones. This article is a review about the current status of robotic surgery for the treatment of gastric cancer, especially, focusing on the technical aspects, comparisons to other approaches and future prospects.
Keywords: Stomach neoplasms, Robotic surgery, Laparoscopy
Introduction
Minimally invasive approaches for gastric cancer is gaining worldwide increasing acceptance. Laparoscopic surgery, introduced by the 1980's, is widely accepted and currently mainstreamed as a minimally invasive approach for many general surgery procedures, including gastrectomy especially for early gastric cancer (EGC). Since the first case of a laparoscopic gastrectomy (LG) for cancer was reported in 1994, surgeons with sufficient experience in open gastric surgery adopted this new approach for EGC: it offers not only better early post-operative course but also long-term oncologic outcomes comparable to those achieved with open gastrectomy (OG).(1-3)
However, laparoscopic surgery is not exempt from several disadvantages, such as altered operating view, lack of versatility in surgical instrumentation and an indication to treat advanced gastric cancers still to be defined. In an effort to minimize the limitations of laparoscopy, robotic surgery was introduced by the late 1990's; thought this system provides undoubted technical advantages,(4) its role for gastric cancer is still unclear.(5-7)
Since robotic gastrectomy (RG) has been reported,(4,8) the application of this new approach is increasing in experienced centers but, up to date, a limited number of single case studies and not randomized comparative studies have focused on this new method. The purpose of this article is to review the current status of robotic surgery for gastric cancer, its technical aspects, its comparisons with open and laparoscopic surgery and to suggest future prospects.
Technical Aspects
1. Indications
The indications for RG are the same as those for laparoscopic ones(8-10): minimally invasive surgery (MIS) is indicated for EGC and it is based on the recommendations of the Japanese gastric cancer treatment guidelines and classification(11,12) as well as the fact that the oncological safety of MIS for advanced gastric cancer remains controversial. According to the articles present in literature up to date, we can summarize as follow:
- Indications for RG with limited lymphadenectomy: STAGE IA.
- Indications for RG requiring D2 lymphadenectomy: STAGE IB-IIA.
Mucosal and submucosal tumor, if eligible, is first considered for endoscopic resection. In case of failed attempts or not suitable to this approach, it can be a candidate for a RG with limited lymphadenectomy. Specific exclusion criteria or contraindications for robotic surgery, as for laparoscopic surgery, include intolerance to pneumoperitoneum and oncologically contraindicated pre-operative findings of T4b cancers or distant metastases.
2. Operative strategy
Specific characteristics of robotic surgical system and operating room configuration have been previously described in detail.(4,8-10,13-17) Most of authors share port placement modality, except some minor variations. Briefly, it can be summarized as follow:
- The patient is in a supine position like in conventional laparoscopy;
- The camera port is inserted at the umbilicus;
- Pneumoperitoneum of 12 mmHg is achieved and patient is then placed in the reverse Trendelenburg position about 15 degrees;
- Under direct visualization, two ports (8 mm diameter) are inserted in the bilateral hypochondriac regions and two further ports (respectively, 8 mm and 12 mm diameter) are placed at both sides of the lateral abdomen, exception for minor adjustments for the patient's body habitus, relative locations of the intraabdominal organs and distance to the oesophageal hiatus during total gastrectomies.(17)
The patient-side cart is now moved next to the patient and the robotic arms are connected to the ports (Docking procedure). Surgeon holds the curved bipolar Maryland forceps by the first arm and the ultrasonic shears (or a monopolar device) and the Cadiere forceps by the second and the third arm.
Before proceeding with the main surgical steps, operative field needs to be prepared at least with three manoeuvres:
- Gastric decompression with insertion of nasogastric tube or alternatively with a 9 cm long 19 gauge needle introduced percutaneously, in case of gastric distension.(18)
- Liver retraction, with one of the various methods described up to date,(19-21) is a prerequisite for complete exposure of the anterior surface of the hepatogastric ligament.
- Intra-operative tumor localization in order to determine the resection extent during distal subtotal gastrectomy achieved by dye injection, intra-operative endoscopy,(8) or laparoscopic ultrasound,(9,22) or endoclips placement and then abdominal X-ray evaluation.(23)
The following are the main surgical steps respectively for robotic subtotal gastrectomy and total gastrectomy.
1) D2 lymph node (LN) dissection during distal subtotal gastrectomy (numbers are LN stations according to Japanese Classification(11)):
Partial incomplete omentectomy and left side dissection of the greater curvature: left gastroepiploic vessels.
Right side dissection of the greater curvature and duodenal transection: head of pancreas and rightgastroepiploic vessels (LN #4s, 4sb).
Hepatoduodenal ligament dissection and approach to suprapancreatic area: right gastric artery, proper hepatic artery, portal vein, common hepatic artery and celiac axis (LN #5, 12a, 8a, 9).
Exposure of the root of the left gastric artery and skeletonization of the splenic vessels (LN #7, 11p).
Lesser curvature dissection: oesophageal crus and cardia (LN #1, 3); proximal gastric resection.
2) D2 lymphadenectomy during total gastrectomy
All steps are as same as for distal gastrectomy except followings:
(1) Spleen-preserving total gastrectomy
Dissection of the distal splenic vessels (LN #11d), the splenic hilum (LN #10), and the division of the short gastric vessels (LN #2, 4sa).
(2) Total gastrectomy with splenectomy
Full mobilization of the distal pancreas and the spleen.
Reconstruction of gastrointestinal continuity can be achieved according to resection extent and surgeon's preference as follows:
3. Skill
1) What skills can be improved with robotic technology?
The robotic surgery system facilitates the process of performing laparoscopic surgery and provides:
Three dimensional (3D)- image;
An intuitive translation of the instrument handle to the tip movement, thus eliminating the mirror image effect;
Coaxial alignment of the eyes, hands, and tool tip image;
Motion scaling;
Tremor filtering;
An internal articulated endoscopic wrist, providing an additional three degrees of freedom.
This computer-enhanced surgical system thus allows surgeons to overcome various difficulties during endoscopic surgery.(4,8)
2) Dissection of splenic vessels
The small branches of the splenic vessels are easily identified and preserved allowing a pancreas-spleen-preserving D2 lymph-node dissection thank to image magnification, tremor filtering, fine circumferential robotic arm movements. This approach allows surgeons to drive the vascular dissection around and to completely clear the lymphatic tissue without any vascular injury with minimal intra-operative bleeding.(13,14)
3) Isolation of diaphragmatic crura
It's a fundamental step to an en bloc dissection of cardia lymph-nodes and is greatly facilitated by wristed instruments that allow complete encircling of the distal oesophagus.(13,15) Moreover, the four-arms robotic surgery system will facilitate the insertion of the anvil head into the oesophageal stump that could be not so easy to do in conventional laparoscopy,(15) and oesophagojejunostomy, which is usually performed in the deep and narrow space of the abdominal cavity, is feasible to execute by the robot-sewing technique.(27)
4) Lymphadenectomy include LN #14v, #8a, #9, #11p, #11d, #12a
Relatively difficult areas to access during laparoscopic lymphadenectomy include LN #14v, #8a, #9, and #11. Moreover, the infrapyloric area and the superior mesenteric vein, including stations 6 and 14v, are the most frequent sources of intra-operative bleeding, while the suprapancreatic area including stations 7, 8a, and 9 is the second most frequent source.(13,26) If the dissection along these vessels is easily conducted, the risk of bleeding can be reduced and lymphadenectomy can be better performed. The EndoWrist, tremor filtration, stable operative platform, and three-dimensional vision offered by the robotic surgical system aid the surgeon to perform a more accurate lymph nodes and vessels dissection.(26)
Some authors have recently reported a new integrated robotic approach for suprapancreatic D2 nodal dissection which appears to be safe and feasible, even though the number of patients in the study was small.(28) Actually, the role of No. 14v lymphadenectomy in distal gastric cancer is controversial. Dissection of node No. 14v had been a part of D2 gastrectomy defined by the 2nd edition of the Japanese classification, but it has been excluded from the latestedition.(11) However, D2 (+No. 14v) may be beneficial in tumors with apparent metastasis to the No. 6 nodes.
5) Lymphadenectomy in obese and bleeding control
Lymph node dissection around infrapyloric and suprapancreatic area is very difficult to perform in patients with a high body mass index (BMI). Robotic technology may facilitate laparoscopic extended lymphadenectomy in patients who have higher BMI than their Asian counterparts.(16,26)
The surgeon can more clearly and definitely identify and easily catch the bleeding vessels using this robotic system than in conventional endoscopic surgery without such a robotic system. This is mainly due to the fact that the robotic system provides a three-dimensional view and has few limitations in the movement of the instruments.(8)
Current Status
In recent years, phase III clinical trials provided evidence that LG with lymph node dissection is a safe and effective surgical procedure for the therapy of EGC(6): it produces a better early post-operative course than conventional OG and the long-term outcome of laparoscopy is also similar to that of open surgery. In an effort to minimize the short comings of laparoscopy, especially the technical ones, the robotic surgery system was introduced as a solution. It is actually considered as a new technology that holds significant promises for the treatment of gastric cancer, although scientific evidence is still lacking.
1. Single case studies
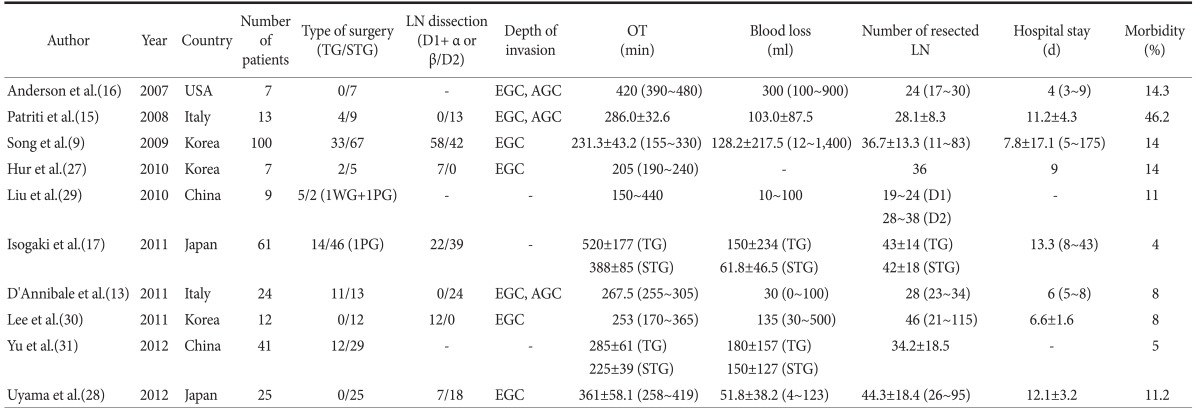
Since 2003 some surgeons started to embrace this new approach. If we consider only caseseries about RG for gastric cancer present in literature, ten reports, with a total of 299 patients, can be collected from 2007 up to date (Table 1).(9,13,15-17,27-31)
Table 1.
Casa series of RG for gastric cancer
RG = robotic gastrectomy; TG = total gastrectomy; STG = subtotal gastrectomy; WG = wedge resection; PG = proximal gastrectomy; LN = lymph node; EGC = early gastric cancer; AGC = advanced gastric cancer; OT = operative time.
The largest study is that of Song et al.(9) published in 2009 about their initial 100 cases of robot-assisted gastrectomy with lymph node dissection followed by another one(17) in 2011 with 61 patients. Total and subtotal robotic gastrectomies were performed with D1+ or/D2 lymphadenectomy according to specific case, on the basis of oncological criteria. Only EGC were included, exception for 2 reports(13,15) that considered also advanced gastric cancer. Three series did not give any information about depth of invasion of the tumor. Each article reports pathologic findings of the enrolled cohort and short-term outcomes including operative details and post-operative course; furthermore, each author describes in details the operative procedure of its own equipe.
In general, all these reports appear to verify the safety and feasibility of this new technology by providing examples of how the robotic surgical system can produce maximum benefits.
RG with D2-lymphadenectomy allows achieving an adequate lymph node harvest and optimal R0-resection rates with low post-operative morbidity and short hospital stays.(13,16,30)
Most common robotic disadvantages shared by most of authors are: longer operative time, higher costs, loss of tactile sensation, indication and lack of oncological results. Obviously, they underline that longer follow-up time and randomized studies are needed to evaluate long-term outcome and clinical advantages.
2. Comparative studies
Several retrospective comparative studies from Europe and Asia have evaluated the use of RG compared with laparoscopic or open ones. In general, they all share the concept that RG with D2 lymph-node dissection is safe, technically feasible for experienced laparoscopic surgeons. On the one hand it's oncologically effective compared to open surgery,(32) associated with less operative blood loss and shorter post-operative hospital stay than laparoscopic and open gastrectomy(33); on the other hand there are still some unresolved issues related to this new technology(5): longer operation time, loss of tactile sensation, higher costs, indications, oncologic equivalency to its counterparts.
1) Robotic vs. open gastrectomy
To date, only two articles compared RG with OG for gastric cancer (Table 2). Pernazza et al.(34), in their preliminary experience, compare for the first time survival, after 26 months of mean follow-up, between these 2 groups and show that robotic surgery may produce some long-term benefits, more evident in patients with advanced disease. At the end of the learning curve, difference in procedure duration is not statistically significant between the 2 groups. Peri-operative morbidity seems to be higher in robotic group, mostly related to the esophagojejunal anastomosis. Post-operative mortality rates are higher in conventional group, mainly in complicated courses with re-operation, probably due to major surgical trauma and immunologic stress, as demonstrated in other studies. Authors believe that robotic D2 lymphadenectomy is convincing, easier than in laparoscopy, and as accurate as in open surgery.
Table 2.
Non-randomized clinical trials robotic vs. open gastrectomy for gastric cancer
R = robotic; O = open; TG = total gastrectomy; STG = subtotal gastrectomy; OT = operative time; LN = lymph node.
In the second study published up to date,(32) based on a strictly matched-case controlled method, no significant difference was shown to exist between the number of lymph nodes obtained during the laparoscopic and open procedures. When a precise lymphadenectomy is needed, robotic system takes advantage of its technologies that makes it possible to perform the dissection with greater ease. In addition, all resected margins in this study were free of tumour in the robotic group, whereas tumour involvement was present in the margin of two specimens in the open group. They furthermore identified less blood loss and a significantly shorter length of hospital stay thus favouring the minimally invasive approach, although surgery took longer for RG than for the OG group. While robotic procedures were associated with longer operative times, there was no difference in 30 day morbidity or mortality between treatment groups. Short-term follow-up evaluation, albeit still in a preliminary setting, showed no difference in survival rates between the two approaches. The conclusion of this trial is that robot-assisted gastric with D2 lymph node dissection is safe, technically feasible and oncologically effective compared to open surgery.
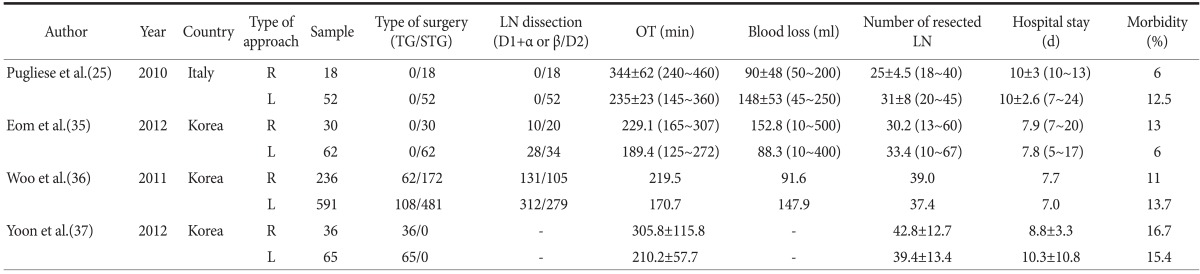
2) Robotic vs. laparoscopic gastrectomy
Only in recent years, some authors published their results about the comparison of RG versus LG (Table 3). Patients enrolled in these studies, are affected by EGC exception for those included in one article(35) that describes encouraging results with a low conversion rate and any intra-operative complications for advanced gastric stages. All these trials evaluate patient characteristics, intra-operative factors, postoperative complications and oncologic parameters.
Table 3.
Non-randomized clinical trials robotic vs. laparoscopic gastrectomy for gastric cancer
R = robotic; L = laparoscopic; TG = total gastrectomy; STG = subtotal gastrectomy; LN = lymph node; OT = operative time.
In terms of intra-operative outcomes, two studies(25,36) find a clinical trend in favour of robotic approach with less blood loss, although the difference is not statistically significant in the first one. In one study,(35) the estimated blood loss difference observed is of minimal clinical significance. Any articles has demonstrated that the hospital stay of the robotic group was statistically lower than the laparoscopic ones, on the contrary, in one report(36) hospital stay appears to be on average longer for the robotic group, although median days to discharge are similar. Morbidity appears to be lower in robotic group for an author,(25) comparable for other ones.(35-37)
Sound oncologic operative outcomes are especially described by two studies.(36,37) The second one, that is also the most numerous, while not randomized, demonstrates that robotic approach permits the experienced surgeon to follow oncologic parameters. None of the specimens shows tumor involvement in the resection line in the robotic group, unlike the laparoscopic ones. More importantly, the number of lymph nodes retrieved for each extent of robotic dissection is sufficient and does not differ by either method.
Moreover, the confirmation of lesions deeper than T2 in the robotic group seems promising for the future use of robotic assistance in treating advanced gastric cancer with D2 lymph node dissection, like Pugliese et al.(25) have already told in advance. Having said that, all these articles lack in long-term oncological outcomes; only one study reports on intermediate survival after RG. Finally, another pitfall of RG is operative time that has been shown to be too long by mostly authors.
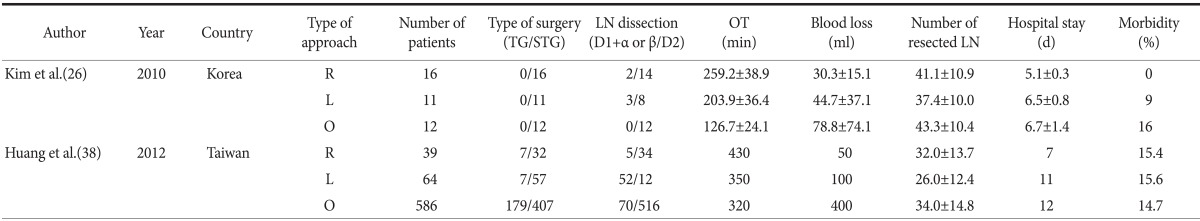
3) Robotic vs. open vs. laparoscopic gastrectomy
While robot-assisted gastrectomy in the setting of gastric cancer has been reported, Kim et al.(26) have been the firsts to compare of this technique with the open and laparoscopic ones, even in a small group of patients (Table 4). According to the authors, RG offers better short-term surgical outcomes than the open and laparoscopic methods in terms of blood loss and hospital stay. The precision of robotic dissection might help to decrease blood loss and transfusion rate and so improve potential survival. Moreover, this new technique might decrease the risk of conversion by overcoming the technical limitations of laparoscopy that lead to conversion.
Table 4.
Non-randomized clinical trials robotic vs. laparoscopic vs. open gastrectomy for gastric cancer
R = robotic; L = laparoscopic; O = open; TG = total gastrectomy; STG = subtotal gastrectomy; LN = lymph node; OT = operative time.
Recently other authors(38) investigated the same aspects in a larger group and reported similar results, with the exception of the post-operative hospital stay that was longer in the present study than other series because the clinical pathway for the laparoscopic group is similar to that used initially with the open ones. They also underline the substantial robotic advantage in facilitating precise lymph node dissection, especially in the infrapyloric and suprapancreatic area due to the stability of the camera, the articulation of the operating arms and the three-dimensional magnified view. Both reports affirm that a longer operation time, as well as higher cost and loss of tactile sense, are considered to be the disadvantages of robotic surgery in comparison to laparoscopic or open conventional surgery.(6)
Future Aspects
1. Operative time and costs
Operating times and cost are at the moment undoubtedly higher than in open and laparoscopic gastric surgery. The first one can be lowered after completion of the learning curve of both surgical and nursing staff as many authors have already published in their trials. With the passing of the time, adequate and better results can be achieved; in addition, a patient should not be denied to undergo a robotic procedure because of this only parameter,(25) provided that the robotic advantages are demonstrated and that it does not entail any risk to the patient.
A prompt reduction of costs in the near future is harder to achieve and it's certainly a big limit. Moreover, a detailed analysis of cost is still lacking, especially in country where a self-pay health care systemis in force. Currently, prospective multicenter studies comparing the cost-effectiveness of open vs. laparoscopic gastrectomy(3) and robotic vs. laparoscopic gastrectomy for gastric cancer are planned as secondary outcomes of more comprehensive study designs (ClinicalTrials.gov. Identifier NCT01309256).
2. Oncological outcomes
Multi-center, randomized, controlled trials are undoubtedly needed to establish the oncological adequacy of RG. The studies performed in Korea are done for EGC only and few trials in Europe have enrolled more advanced gastric cancer stages; the role of robotic surgery in both cases, but especially in the second ones, remains to be delineated, mainly because it is not yet known which is that of laparoscopy.
An interesting aspect that could be investigate in future is in fact regarding the role of minimally invasive approach for the treatment of advanced gastric cancer. Adjuvant chemoradiation and chemotherapy has seemed to increase life expectancy in node-positive gastric cancer patients. In the near future, new approaches to gastric cancer management will provide novel opportunities of treatment, including immunochemotherapy and molecular-targeted therapies.
In this context, minimally invasive surgery could play a key role in improving post-operative course and accelerating times to adjuvant treatments,(15) and especially robotic surgery might be a correct alternative to laparoscopic approach or the first choice for selected cases.
3. Surgeon's skill
It's ostensible that robotic system can improve surgeon dexterity by performing more precise and safer operative technique in a minimally invasive way due to its technologies, even if it is unproven to date. If it will be demonstrated, this skill could improve experienced laparoscopic surgeon performance, but could especially be a turning point for less accomplished ones. As Jayaraman et al.(39) have reported in their article, robotics may allow less experienced surgeons with fundamental knowledges to perform more complex operations without first developing advanced laparoscopic skills.
Another favourable aspect, is regarding the robotic learning curve. In a report comparing the learning curve between conventional laparoscopy and robotic assistance in surgical tasks, some authors(40) demonstrate that laparoscopic surgery showed a steep learning curve, whereas robot-assisted surgery showed better results from the beginning of the initial case with a shallower learning curve, showing the easy adaptability of robot-assisted surgery. Further, the growing application of pre-operative simulator technology in surgical robotics may considerably decrease the learning curve of robot-assisted operations(36) and so accelerate the process of robotic adoption in gastric surgery.
Conclusion
This systematic review is to date the more recent. Robotic surgery is actually endowed with very interesting aspects and promising outcomes that could ultimately offer some benefits for the treatment of gastric cancer. Larger numbers of studies and more specific evaluations are needed to prove it and especially to refute pitfalls and disadvantages that are present as well.
On the other hand, as we observed in laparoscopic surgery, to validate the role of robotic surgery will take many more years.
References
- 1.Kitano S, Shiraishi N, Uyama I, Sugihara K, Tanigawa N Japanese Laparoscopic Surgery Study Group. A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg. 2007;245:68–72. doi: 10.1097/01.sla.0000225364.03133.f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huscher CG, Mingoli A, Sgarzini G, Sansonetti A, Di Paola M, Recher A, et al. Laparoscopic versus open subtotal gastrectomy for distal gastric cancer: five-year results of a randomized prospective trial. Ann Surg. 2005;241:232–237. doi: 10.1097/01.sla.0000151892.35922.f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim HH, Hyung WJ, Cho GS, Kim MC, Han SU, Kim W, et al. Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report--a phase III multicenter, prospective, randomized Trial (KLASS Trial) Ann Surg. 2010;251:417–420. doi: 10.1097/SLA.0b013e3181cc8f6b. [DOI] [PubMed] [Google Scholar]
- 4.Giulianotti PC, Coratti A, Angelini M, Sbrana F, Cecconi S, Balestracci T, et al. Robotics in general surgery: personal experience in a large community hospital. Arch Surg. 2003;138:777–784. doi: 10.1001/archsurg.138.7.777. [DOI] [PubMed] [Google Scholar]
- 5.Hyung WJ. Robotic surgery in gastrointestinal surgery. Korean J Gastroenterol. 2007;50:256–259. [PubMed] [Google Scholar]
- 6.Baek SJ, Lee DW, Park SS, Kim SH. Current status of robot-assisted gastric surgery. World J Gastrointest Oncol. 2011;3:137–143. doi: 10.4251/wjgo.v3.i10.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buchs NC, Bucher P, Pugin F, Morel P. Robot-assisted gastrectomy for cancer. Minerva Gastroenterol Dietol. 2011;57:33–42. [PubMed] [Google Scholar]
- 8.Hashizume M, Sugimachi K. Robot-assisted gastric surgery. Surg Clin North Am. 2003;83:1429–1444. doi: 10.1016/S0039-6109(03)00158-0. [DOI] [PubMed] [Google Scholar]
- 9.Song J, Oh SJ, Kang WH, Hyung WJ, Choi SH, Noh SH. Robot-assisted gastrectomy with lymph node dissection for gastric cancer: lessons learned from an initial 100 consecutive procedures. Ann Surg. 2009;249:927–932. doi: 10.1097/01.sla.0000351688.64999.73. [DOI] [PubMed] [Google Scholar]
- 10.Hyung WJ, Woo YH, Noh SH. Robotic surgery for gastric cancer: a technical review. J Robot Surg. 2011;5:241–249. doi: 10.1007/s11701-011-0263-x. [DOI] [PubMed] [Google Scholar]
- 11.Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–112. doi: 10.1007/s10120-011-0041-5. [DOI] [PubMed] [Google Scholar]
- 12.Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3) Gastric Cancer. 2011;14:113–123. doi: 10.1007/s10120-011-0042-4. [DOI] [PubMed] [Google Scholar]
- 13.D'Annibale A, Pende V, Pernazza G, Monsellato I, Mazzocchi P, Lucandri G, et al. Full robotic gastrectomy with extended (D2) lymphadenectomy for gastric cancer: surgical technique and preliminary results. J Surg Res. 2011;166:e113–e120. doi: 10.1016/j.jss.2010.11.881. [DOI] [PubMed] [Google Scholar]
- 14.Song J, Kang WH, Oh SJ, Hyung WJ, Choi SH, Noh SH. Role of robotic gastrectomy using da Vinci system compared with laparoscopic gastrectomy: initial experience of 20 consecutive cases. Surg Endosc. 2009;23:1204–1211. doi: 10.1007/s00464-009-0351-4. [DOI] [PubMed] [Google Scholar]
- 15.Patriti A, Ceccarelli G, Bellochi R, Bartoli A, Spaziani A, Di Zitti L, et al. Robot-assisted laparoscopic total and partial gastric resection with D2 lymph node dissection for adenocarcinoma. Surg Endosc. 2008;22:2753–2760. doi: 10.1007/s00464-008-0129-0. [DOI] [PubMed] [Google Scholar]
- 16.Anderson C, Ellenhorn J, Hellan M, Pigazzi A. Pilot series of robot-assisted laparoscopic subtotal gastrectomy with extended lymphadenectomy for gastric cancer. Surg Endosc. 2007;21:1662–1666. doi: 10.1007/s00464-007-9266-0. [DOI] [PubMed] [Google Scholar]
- 17.Isogaki J, Haruta S, Man-I M, Suda K, Kawamura Y, Yoshimura F, et al. Robot-assisted surgery for gastric cancer: experience at our institute. Pathobiology. 2011;78:328–333. doi: 10.1159/000330172. [DOI] [PubMed] [Google Scholar]
- 18.Hyung WJ, Song C, Cheong JH, Choi SH, Noh SH. Percutaneous needle decompression during laparoscopic gastric surgery: a simple alternative to nasogastric decompression. Yonsei Med J. 2005;46:648–651. doi: 10.3349/ymj.2005.46.5.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Woo Y, Hyung WJ, Kim HI, Obama K, Son T, Noh SH. Minimizing hepatic trauma with a novel liver retraction method: a simple liver suspension using gauze suture. Surg Endosc. 2011;25:3939–3945. doi: 10.1007/s00464-011-1788-9. [DOI] [PubMed] [Google Scholar]
- 20.Shinohara T, Kanaya S, Yoshimura F, Hiramatsu Y, Haruta S, Kawamura Y, et al. A protective technique for retraction of the liver during laparoscopic gastrectomy for gastric adenocarcinoma: using a Penrose drain. J Gastrointest Surg. 2011;15:1043–1048. doi: 10.1007/s11605-010-1301-0. [DOI] [PubMed] [Google Scholar]
- 21.Shabbir A, Lee JH, Lee MS, Park do J, Kim HH. Combined suture retraction of the falciform ligament and the left lobe of the liver during laparoscopic total gastrectomy. Surg Endosc. 2010;24:3237–3240. doi: 10.1007/s00464-010-1118-7. [DOI] [PubMed] [Google Scholar]
- 22.Hyung WJ, Lim JS, Cheong JH, Kim J, Choi SH, Song SY, et al. Intraoperative tumor localization using laparoscopic ultrasonography in laparoscopic-assisted gastrectomy. Surg Endosc. 2005;19:1353–1357. doi: 10.1007/s00464-004-8196-3. [DOI] [PubMed] [Google Scholar]
- 23.Kim HI, Hyung WJ, Lee CR, Lim JS, An JY, Cheong JH, et al. Intraoperative portable abdominal radiograph for tumor localization: a simple and accurate method for laparoscopic gastrectomy. Surg Endosc. 2011;25:958–963. doi: 10.1007/s00464-010-1288-3. [DOI] [PubMed] [Google Scholar]
- 24.Pugliese R, Maggioni D, Sansonna F, Ferrari GC, Forgione A, Costanzi A, et al. Outcomes and survival after laparoscopic gastrectomy for adenocarcinoma. Analysis on 65 patients operated on by conventional or robot-assisted minimal access procedures. Eur J Surg Oncol. 2009;35:281–288. doi: 10.1016/j.ejso.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 25.Pugliese R, Maggioni D, Sansonna F, Costanzi A, Ferrari GC, Di Lernia S, et al. Subtotal gastrectomy with D2 dissection by minimally invasive surgery for distal adenocarcinoma of the stomach: results and 5-year survival. Surg Endosc. 2010;24:2594–2602. doi: 10.1007/s00464-010-1014-1. [DOI] [PubMed] [Google Scholar]
- 26.Kim MC, Heo GU, Jung GJ. Robotic gastrectomy for gastric cancer: surgical techniques and clinical merits. Surg Endosc. 2010;24:610–615. doi: 10.1007/s00464-009-0618-9. [DOI] [PubMed] [Google Scholar]
- 27.Hur H, Kim JY, Cho YK, Han SU. Technical feasibility of robot-sewn anastomosis in robotic surgery for gastric cancer. J Laparoendosc Adv Surg Tech A. 2010;20:693–697. doi: 10.1089/lap.2010.0246. [DOI] [PubMed] [Google Scholar]
- 28.Uyama I, Kanaya S, Ishida Y, Inaba K, Suda K, Satoh S. Novel integrated robotic approach for suprapancreatic D2 nodal dissection for treating gastric cancer: technique and initial experience. World J Surg. 2012;36:331–337. doi: 10.1007/s00268-011-1352-8. [DOI] [PubMed] [Google Scholar]
- 29.Liu FL, Lv CT, Qin J, Shen KT, Chen WD, Shen ZB, et al. Da Vinci robot-assisted gastrectomy with lymph node dissection for gastric cancer: a case series of 9 patients. Zhonghua Wei Chang Wai Ke Za Zhi. 2010;13:327–329. [PubMed] [Google Scholar]
- 30.Lee HH, Hur H, Jung H, Jeon HM, Park CH, Song KY. Robot-assisted distal gastrectomy for gastric cancer: initial experience. Am J Surg. 2011;201:841–845. doi: 10.1016/j.amjsurg.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 31.Yu PW, Tang B, Zeng DZ, Zhao YL, Shi Y, Hao YX, et al. Robotic-assisted radical gastrectomy using da Vinci robotic system: a report of 41 cases. Zhonghua Wei Chang Wai Ke Za Zhi. 2012;15:121–124. [PubMed] [Google Scholar]
- 32.Caruso S, Patriti A, Marrelli D, Ceccarelli G, Ceribelli C, Roviello F, et al. Open vs robot-assisted laparoscopic gastric resection with D2 lymph node dissection for adenocarcinoma: a case-control study. Int J Med Robot. 2011;7:452–458. doi: 10.1002/rcs.416. [DOI] [PubMed] [Google Scholar]
- 33.Glantzounis G, Ziogas D, Baltogiannis G. Open versus laparoscopic versus robotic gastrectomy for cancer: need for comparative-effectiveness quality. Surg Endosc. 2010;24:1510–1512. doi: 10.1007/s00464-009-0790-y. [DOI] [PubMed] [Google Scholar]
- 34.Pernazza G, Gentile E, Felicioni L, Tumbiolo S, Giulianotti PC. Improved early survival after robotic gastrectomy in advanced gastric cancer. Surg Laparosc Endosc Percutan Tech. 2006;16:286. [Google Scholar]
- 35.Eom BW, Yoon HM, Ryu KW, Lee JH, Cho SJ, Lee JY, et al. Comparison of surgical performance and short-term clinical outcomes between laparoscopic and robotic surgery in distal gastric cancer. Eur J Surg Oncol. 2012;38:57–63. doi: 10.1016/j.ejso.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 36.Woo Y, Hyung WJ, Pak KH, Inaba K, Obama K, Choi SH, et al. Robotic gastrectomy as an oncologically sound alternative to laparoscopic resections for the treatment of early-stage gastric cancers. Arch Surg. 2011;146:1086–1092. doi: 10.1001/archsurg.2011.114. [DOI] [PubMed] [Google Scholar]
- 37.Yoon HM, Kim YW, Lee JH, Ryu KW, Eom BW, Park JY, et al. Robot-assisted total gastrectomy is comparable with laparoscopically assisted total gastrectomy for early gastric cancer. Surg Endosc. 2012;26:1377–1381. doi: 10.1007/s00464-011-2043-0. [DOI] [PubMed] [Google Scholar]
- 38.Huang KH, Lan YT, Fang WL, Chen JH, Lo SS, Hsieh MC, et al. Initial experience of robotic gastrectomy and comparison with open and laparoscopic gastrectomy for gastric cancer. J Gastrointest Surg. 2012 doi: 10.1007/s11605-012-1874-x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 39.Jayaraman S, Quan D, Al-Ghamdi I, El-Deen F, Schlachta CM. Does robotic assistance improve efficiency in performing complex minimally invasive surgical procedures? Surg Endosc. 2010;24:584–588. doi: 10.1007/s00464-009-0621-1. [DOI] [PubMed] [Google Scholar]
- 40.Heemskerk J, van Gemert WG, de Vries J, Greve J, Bouvy ND. Learning curves of robot-assisted laparoscopic surgery compared with conventional laparoscopic surgery: an experimental study evaluating skill acquisition of robot-assisted laparoscopic tasks compared with conventional laparoscopic tasks in inexperienced users. Surg Laparosc Endosc Percutan Tech. 2007;17:171–174. doi: 10.1097/SLE.0b013e31805b8346. [DOI] [PubMed] [Google Scholar]