Abstract
Ingestion of variety of foreign bodies causing respiratory distress and/or dysphagia is worldwide among all age groups. Securing airway by tracheostomy is important and direct laryngoscopy provides immediate diagnosis. The importance of contributory history and its visualization is emphasized in the diagnosis and early management in the described six cases.
Keywords: Ant, Ballpoint pen, Fish bone, Foreign bodies, Metallic beads, Removable complete denture, Stridor, Toothbrush head, Tracheostomy
Introduction
Ingestion of a foreign body is a common problem among all age groups and particularly in infants and children as they have a tendency to put any thing in the mouth which may be ingested accidentally. These may get lodged in tonsil, base of tongue, piriform fossae, and oesophagus or sometimes in the larynx or lower down in the respiratory tract leading to medical/surgical emergencies which are often challenging to an otorhinolaryngologist. Most of the foreign bodies in pharynx usually get stuck at the level of cricopharynx or down in the right bronchus or lower lobe when the larynx is small. Occasionally the foreign bodies in the larynx may end fatally. The diagnosis is based on history, clinical and radiological examination. Depending upon the age a vast variety of foreign bodies like coins, marbles, buttons, batteries, bottle tops, peas, beans, grains and seeds in infants and children, and bones, dentures and metallic pins/wires have been reported more often in adults [1]. While fish bone is perhaps the commonest foreign body in the pharynx in adult population, live fish impacted in throat too has been documented [2, 3]. The described six patients, both children and adults, had variety of foreign bodies impacted at various levels of oro-pharyngo-larynx each with different clinical presentation.
Case Presentation
Case 1
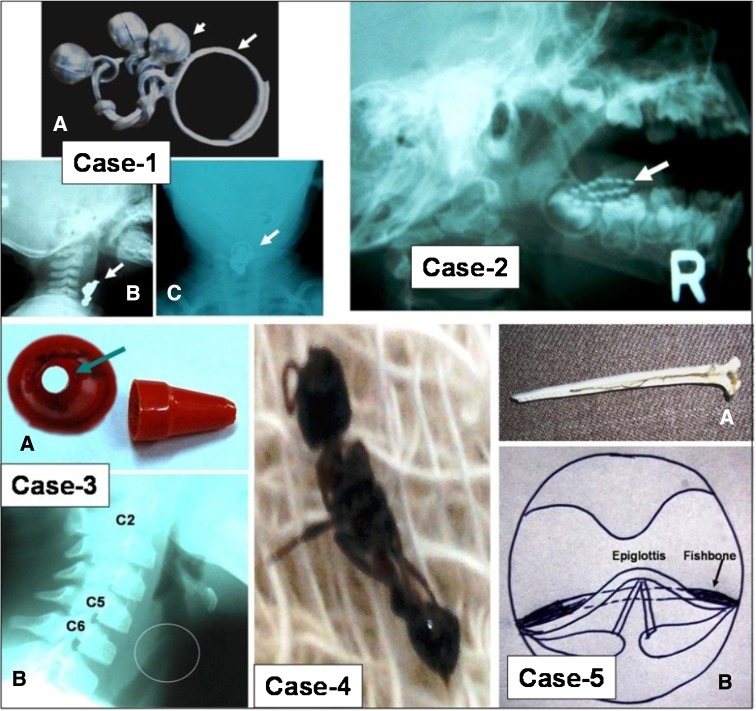
This 6-month-old female child was brought immediately after accidental swallowing of a metal trinket (Fig. 1). Historically the child did not have any episode of apnoea or dyspnoea. The child was comfortable, playful and showed no signs or symptoms suggestive of foreign body ingestion. Examination of the oral cavity was normal. An X-rays soft tissue neck showed foreign body at the level of C4-5 vertebrae (Fig. 1; Case 1). Direct laryngoscopy under general anaesthesia showed round ring lying just above the laryngeal inlet and other ring with metallic beads over the false vocal cord. The foreign body was removed with the help of laryngeal forceps and the child was discharged next day.
Fig. 1.
Case 1. The bigger of the two rings (large arrow) of this metallic trinket was overlying the laryngeal inlet and the other one (small arrow) with beads was lying over the false vocal cord (a). X-rays soft tissue neck (AP and Lateral views) show position of the foreign body (b and c). Case 2. Tooth brush’s head with bristles (arrow) in the right cheek as seen in the X-ray film (lateral view). Case 3. Two views of plastic part of ball point pen (a). The patient was able to breath through the hole (arrow). X-rays soft tissue neck (Lateral view) shows the foreign body (encircled) in trachea in front of C5-6 (b). Case 4. The thief ant (Solenopsis sp.) after removal. Case 5. Fish bone after removal (a) and graphic representation of its position at the base of epiglottis (b)
Case 2
This 2-year-old male child presented in emergency with bleeding from mouth and part of toothbrush lodged in the oral cavity. History revealed that he had tripped and fell over his face while brushing teeth. The child was in pain and crying, and had normal vital signs. Examination showed swelling over right cheek, bleeding and laceration in the right gingivo-buccal fold, and oedema of oral mucosa. The right tonsil showed slight bulging and normal anterior and posterior tonsillar pillars. On bimanual examination a foreign body could be palpated on the right cheek up to the posterior tonsillar pillar. An X-ray head and neck revealed bristled part of toothbrush in lateral view (Fig. 1; Case 2). The part of toothbrush was removed through the laceration with the help of forceps under general anaesthesia and the wound repaired. Subsequent recovery was uneventful.
Case 3
This 10-year-old female child was referred from a peripheral hospital with severe stridor and respiratory distress following accidental ingestion of a small part of ballpoint pen (Fig. 1; Case 3) 2 days earlier. Parents and the child were under great distress as the child was having severe difficulty in breathing and stridor was loud enough to be heard from a distance. X-ray soft tissue neck showed foreign body in the trachea at the level of C5-6. Emergency tracheostomy was performed to secure airway and to prevent the slipping of foreign body further down. The foreign body lying at the upper end of trachea below the vocal cords was removed by direct laryngoscopy under general anaesthesia. Interestingly the patients could breathe through the hole in the foreign body. Tracheostomy tube was removed after 5 days. Further recovery was uneventful.
Case 4
A 20-year-old female presented in the emergency with history of foreign body sensation and irritation in the throat immediately after drinking a glass of water. She was not sure whether the water had any kind of foreign body as she had taken the water while it was dark inside the room. She was uncomfortable but vital signs were normal. Examination of the oropharynx was normal and indirect laryngoscopy showed oedema over the left arytenoid extending to left pyriform fossa. However, no foreign body could be visualized. An X-ray soft tissue neck too was normal. The patient was managed conservatively and repeat indirect laryngoscopy on next morning showed decreased arytenoid edema but she had no improvement in her symptoms. On direct laryngoscopic examination under general anaesthesia there was oedema of the left arytenoid and a live ant (thief ant, Fig. 1; Case 4) was found embedded in the mucosa of left pyriform fossa which was removed. The patient became asymptomatic and discharged.
Case 5
A 25-year-old male was hospitalized with respiratory discomfort, pain and difficulty in swallowing for both liquid and solid foods. He was apprehensive and uncomfortable, had no stridor, and other vital signs were normal. He gave history of accidentally ingesting a fish bone while eating roasted fish a day prior to the development of the symptoms. Although the pharyngeal mucosa and valleculae were congested, edematous and showed traumatic abrasions, no foreign body could be visualized on indirect laryngoscopy. An X-rays soft tissue neck and chest showed no evidence of fish bone or other foreign body in the larynx or tracheobronchial tree. He could not afford for CT scan. The patient was managed conservatively for a day for the respiratory discomfort and mucosal inflammation to subside. Next morning direct laryngoscopic examination under general anaesthesia showed no foreign body but slight reflection of light at the base of epiglottis was observed that felt bony hard when touched with forceps. This was a fish bone (rib) embedded in the soft tissue at the base of epiglottis (Fig. 1; Case 5) merging with its surrounding tissues and could be removed with the help of laryngeal forceps. The patient was asymptomatic at the time of discharged 2 days later.
Case 6
A 62-year-old male presented with history of acute dysphagia and difficulty in breathing. History revealed that his upper removable complete denture had slipped accidentally into his throat while he yawned. He had similar episodes in the past on two occasions but had not complied with the advice to get well fitting dentures. Examination of oral cavity with tongue depressor showed the denture lying in the oropharynx. The denture was removed with the help of Magill’s forceps as office procedure. Repeat clinical examination including indirect laryngoscopy revealed no significant oropharyngeal injury. The patient did not follow up further.
Discussion
Accidental swallowing of a foreign body and its impaction in the airway is common in infants and children between 6 months and 3 years of age possibly due to un-coordinated swallowing, absence of molars for proper chewing, and tendency to put any thing in mouth out of curiosity [4]. However, it is not uncommon in adults particularly having loose dentures. Our patients were three children between 6 months and 10 years and three adults aged 20–62 years. Nature of foreign bodies may be vegetative inanimate (seeds, grains, peas, peanuts, etc.), vegetative animate (insects, etc.) or non-vegetative (fish bone, denture plates, beads, coins, safety pins, etc.) [4, 5]. This was also evident in our patients as well. Our case 4 was interesting in a way that she was not very sure of swallowing of foreign body but a live ant was visualized and she became asymptomatic after its removal. Prompt removal of the foreign body is imperative to prevent complications of hoarseness, stridor, dyspnoea, odynophagia, hemoptysis, or respiratory obstruction. Thus history of foreign body ingestion is important in early diagnosis. However, in up to 5–50% cases contributory history may not be forthcoming [5]. This particularly appears true in case of children who do not comprehend the impending consequences and out of fear may not disclose about this until complications develop. Specific nature of symptoms will obviously be helpful in localizing the foreign body [6]. The foreign bodies in the larynx cause dysphagia, dyspnoea, cough, wheezing, stridor or acute respiratory obstruction causing a sort of panic for both parents and the child. On the other hand pharyngo-oesophageal foreign bodies present with dysphagia and sense of something stuck in the throat that may be alarming for the parents but the child remains less confused. More or less these features were present in our patients and were helpful in early diagnosis. While large sized foreign bodies such as a denture plate may be visualized and removed immediately on direct examination of oropharynx as in our case 6, presence of laceration, edema, or ulceration on examination of oropharynx, as in our case 2 having penetrating impaction of toothbrush, or on direct laryngoscopy and esophagoscopy should make one to suspect a perforating foreign body that can be removed with forceps. X-ray of the soft tissues of the neck (antero-posterior and lateral views) is important to diagnose and to locate a foreign body in suspected cases. However, plain radiographs may miss a fine fish bone or foreign bodies which are not radio-opaque [3]. Our case 5 had a fine fish bone (rib) impacted and encircling the base of epiglottis and was missed in radiographs. The whole bone was embedded in the mucosa that made it difficult to visualize on direct laryngoscopy as well. Similar observations were made by Honda et al. [3] and plausible explanation was deep insertion of the fish bone in the narrow postcricoid mucosa where its visualization is difficult owing to overhanging larynx limiting the operative field. CT scan is considered to be diagnostic tool of choice in such cases. However, its cost may be a constraint in resource-limited settings. Chest radiograph is usually normal initially and features of obstructive emphysema or atelectasis develop late in patients who also have tracheobronchial obstruction. Direct laryngoscopic microscopy has been advocated by some workers to visualize and remove a foreign body [7]. Tracheostomy may be needed in patients presenting with stridor due to foreign body in the trachea. This will also prevent slipping of foreign body further into the bronchus. We used direct laryngoscopy under general anaesthesia both for diagnosis and removal of foreign body in our patients except for case 6. Tracheostomy was needed in one patient, case 2, only.
Closing Remarks
Most patients with oropharyngeal or laryngeal foreign bodies require to be managed in a planned manner without panic. A contributing history and detailed clinical examination are imperative for clinical diagnosis in suspected cases. When breathing is hampered securing of airway by tracheostomy is of utmost importance. We feel that direct laryngoscopy under general anaesthesia will provide immediate diagnosis in all suspected cases and foreign body can be removed with ease.
Acknowledgments
Conflict of interest
None.
References
- 1.Sarkar S, Roychoudhury A, Roychoudhury BK. Foreign bodies in ENT in a teaching hospital in eastern India. Indian J Otolaryngol Head Neck Surg. 2010;62:118–120. doi: 10.1007/s12070-010-0040-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Panigrahi R, Sarangi TR, Behera SK, Biswal RN. Unusual foreign body in throat. Indian J Otolaryngol Head Neck Surg. 2007;59:384–385. doi: 10.1007/s12070-007-0110-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Honda K, Tanaka S, Tamura Y, Asato R, Hirano S, Ito J. Vocal cord fixation caused by a impacted fish bone in hypopharynx: report of a rare case. Am J Otolaryngol Head Neck Med Surg. 2007;28:257–259. doi: 10.1016/j.amjoto.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 4.Kansara AH, Shah HV, Patel MA, Manjunatharao SV. Unusual case of laryngeal foreign body. Indian J Otolaryngol Head Neck Surg. 2006;59:63–65. doi: 10.1007/s12070-007-0019-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ellan M. Tracheo-bronchial foreign bodies: Otolaryngologic. Clin North Am. 2000;33:179–185. doi: 10.1016/s0030-6665(05)70214-0. [DOI] [PubMed] [Google Scholar]
- 6.Connolly AA, Birchall M, walsh-Waring GP, Moore-Gillon V. Ingested foreign bodies: patient-guided localization is a useful tool. Clin Otolaryngol Allied Sci. 1992;17:520–524. doi: 10.1111/j.1365-2273.1992.tb01710.x. [DOI] [PubMed] [Google Scholar]
- 7.Shu MT, Leu YS. Microscopic removal of an embedded foreign body from hypopharynx: report of two cases. Ear Nose Throat J. 2001;80:889–890. [PubMed] [Google Scholar]