Abstract
The objective of the present study was to determine the status of extended high frequencies in subjects with secretory otitis media. The study evaluated 30 ears of 20 subjects with secretory otitis media in the age group of 15–30 years. This data was compared with 20 ears of 10 volunteers of the same age group with clinically normal hearing. Pure tone air conduction thresholds were analyzed in three frequency groups: low frequency (LF: 0.25, 0.5, and 1 kHz), high frequency (HF: 2, 4, and 8 kHz) and extended high frequency (EHF: 10, 12, and 16 kHz). The results showed elevated extended high frequency thresholds (EHFG) as compared to control group and comparatively better thresholds at high frequencies(HFG)s as compared to low (LFG)and extended high frequencies(EHFG) in the study group. This validates the importance of including an extended high frequency audiometry in the test battery of patients with secretory otitis media.
Keywords: Extended high frequency, Secretory otitis media, Pure tone audiometry
Introduction
Secretory otitis media (SOM) is one of the most common disease affecting up to 80% of children who experience at least one episode of middle ear effusion [1]. It is characterized by presence of non suppurative (i.e. non infectious) effusion in the middle ear cleft [2]. The most common feature is hearing loss, which may vary from negligible to 50–60 dB [3, 4]. The magnitude of loss is determined by the extent to which the disease interferes with the ossicular chain, not the severity of the disease [5].
In the past, studies have been restricted to pure tone audiometric evaluation of conventional frequencies (0.25–8 kHz) mainly in chronic suppurative otitis media (CSOM). A number of studies have suggested that sensorineural hearing loss (SNHL) may be a sequela of otitis media [6]. Various studies have demonstrated an association between chronic suppurative otitis media and SNHL [7, 8]. Studies have demonstrated other auditory findings that suggest the presence of inner ear hearing loss due to CSOM [9, 10]. Laboratory studies have shown various histopathologic and electrophysiologic abnormalities in animals that suggest inner ear damage secondary to otitis media [11].
Interest in the extra high frequency (EHF) audiometry with determination of air conduction thresholds in the frequency range of 8–20 kHz has become more wide spread since 1960 with the advent of commercial extra high frequency audiometers. Inter-laboratory comparisons were impossible earlier as custom built instruments were employed but the introduction of commercial EHF audiometer has remedied the situation. There are very few studies to evaluate the auditory status of extra high frequencies in SOM. SOM related SNHL has been reported in 1–9% of cases [12]. In the Finnish cohort study of about 12,000 children, SOM was associated with high frequency loss (6–8 kHz) at the age of 15 years [13]. Dicroff [14] found permanent high frequency loss in few cases of SOM patient’s. Mc Dermott [15] found permanent high frequency loss in frequencies greater than 8 kHz in the patients with cleft and prolonged middle ear disease. SOM may be temporary, but is often recurrent or fluctuating, and may be asymmetric. To the best of our knowledge no studies have been found regarding the auditory status (conventional as well as extra high frequencies) of SOM of several years duration.
Anatomic and physiologic knowledge of the auditory mechanism reveals, frequency coding along the basilar membrane progress from high to low frequencies with distance from the basal end of the cochlea. Therefore, hearing loss produced by the diffusion of otitis media-related toxins across round window membrane would be expected to preferentially affect high frequency hearing first. Therefore this investigation was undertaken to determine the status of extra high frequencies in cases of secretory otitis media of several years duration.
Materials and Methods
The study was conducted in Speech and Hearing Unit, Department of Otolaryngology and Head and Neck Surgery, Post Graduate Institute of Medical Education and Research, Chandigarh, India. The Control group comprised of 20 subjects selected among volunteers using following selection criteria. (1) No documented episode of otitis media. (2) No significant medical history/surgery for any disease (3) Normal hearing in conventional audiometry. The study group included 20 subjects in the age range of 15–30 years who were diagnosed as having unilateral or bilateral SOM by otolaryngologist. All the patients had middle ear effusion persisting continuously for at least 5 years interrupted only by treatment from local practitioners. Previous treatment records of only 12 patients were available during the study. Out of 12, two patients had received only medical treatment while rest of the patients had undergone myringotomy more than twice and five had history of grommet insertion during childhood. The incidence of tympanic membrane (TM) pathology (myringosclerosis, retraction) was high in SOM group. At the time of study, all the patients were being treated for SOM. Ten subjects had unilateral SOM and 10 had bilateral SOM therefore in total 30 ears were taken for the analyses. All the individuals having any other significant medical history, long term use of medication, family history of hearing loss or any other syndrome associated with hearing loss were excluded. Each subject went through the following procedures—detailed case history, air conduction and bone conduction audiometry, tympanometry and EHF audiometry.
The tests were conducted in the centrally air conditioned sound treated rooms. Conventional audiometry was performed with a clinical audiometer ORBITER 922 (calibrated as per ANSI 1992) equipped with the standard and bone conduction transducers (Telephonic TDH 39 supra aural with RADIO EAR MX-41 noise excluding head set and Radio ear respectively). EHF was performed with the same audiometer with the headphones designed for high frequency (Sennheiser HDA 200 circum aural). Tympanometry was performed with Siemens SD30 tympanometer.
The three frequency groups were compared: low frequency (LF: 0.25, 0.5 and 1 kHz), high frequency (2, 4 and 8 kHz) and extended high frequency (10, 12, and 16 kHz). The mean and standard deviation of the air and bone conduction thresholds were calculated for each grouped frequency. The comparison of different frequency averages were made between the study and the control group. The comparison was also made between the differences of low-high and high-extended high frequency averages within the group and between the groups (study and control). Statistically significant estimates were made by using student t test.
Results
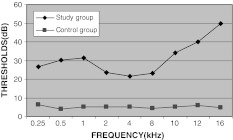
Mean hearing thresholds of SOM group and controls are presented in Fig. 1 and Table 1 The SOM group exhibited significantly higher thresholds as compared to the controls at all the frequencies studied, in the range 0.25–16 kHz (P < 0.001). Figure 2 shows the mean values for all the three frequency groups (low, high, extended high) of both the control and the study group.
Fig. 1.
Mean hearing thresholds in SOM subjects and controls at frequencies of 0.25–16 kHz
Table 1.
Comparison of mean thresholds and standard deviation (SD) in the study and the control group
| Frequency (kHz) | Study group | Control group | t value |
|---|---|---|---|
| 0.25 K | |||
| Mean (dB) | 26.67 | 17.00 | 4.567*** |
| SD | 6.21 | 4.22 | |
| 0.5 K | |||
| Mean (dB) | 30.33 | 15.50 | 10.496*** |
| SD | 3.92 | 3.69 | |
| 1 K | |||
| Mean (dB) | 31.50 | 15.50 | 8.857*** |
| SD | 5.11 | 4.39 | |
| 2 K | |||
| Mean (dB) | 23.50 | 15.00 | 4.900*** |
| SD | 4.94 | 4.08 | |
| 4 K | |||
| Mean (dB) | 21.50 | 14.50 | 3.875*** |
| SD | 5.28 | 3.69 | |
| 8 K | |||
| Mean (dB) | 23.17 | 15.50 | 5.090*** |
| SD | 4.25 | 3.69 | |
| 10 K | |||
| Mean (dB) | 34.00 | 16.00 | 10.073*** |
| SD | 4.98 | 4.59 | |
| 12 K | |||
| Mean (dB) | 40.00 | 17.50 | 10.908*** |
| SD | 5.87 | 4.86 | |
| 16 K | |||
| Mean (dB) | 49.67 | 19.50 | 19.687*** |
| SD | 4.54 | 2.84 | |
kHz kilo Hertz, dB decibel, SD standard deviation
* P < 0.05, ** P < 0.01, *** P < 0.001
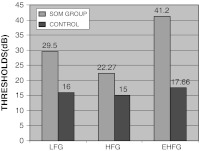
Fig. 2.
Mean thresholds of three frequency groups in study and control group
On applying ANOVA it could be seen in Table 2 that there is no significant difference across the three frequency groups revealing equal hearing sensitivity. However, it could be seen in Table 3 that in the study group there is significant difference among three frequency groups (LFG vs. HFG and HFG vs. EHFG) which reveals that the hearing sensitivity is more affected at certain frequencies. The threshold values show that the hearing is least affected in the HFG with average threshold (TH) value of 22.27 dB as compared to LFG with TH value 29.5 dB and EHF with TH value 41.2 dB which concludes that High frequencies are least affected.
Table 2.
Comparison between three frequency averages (LFG, HFG and EHFG) and standard deviation (SD) in the control group
| Groups | LFG | HFG | EHFG | F value |
|---|---|---|---|---|
| Control group | ||||
| Mean | 16.00 | 15.00 | 17.66 | 2.13 |
| SD | 0.86 | 0.50 | 1.75 | |
| Study group | ||||
| Mean | 29.50 | 22.72 | 41.22 | 44.49*** |
| SD | 3.22 | 3.40 | 3.27 |
SD standard deviation, LFG low frequency average group, HFG high frequency average group, EHFG extended high frequency average group
* P < 0.05, ** P < 0.01, *** P < 0.001
Table 3.
Multiple comparison of three frequency averages LFG–HFG, HFG–EHFG and EHFG–EHFG
| Groups | Mean difference | SE | P |
|---|---|---|---|
| LFG–HFG | 6.777 | 0.8521 | 0.0001 |
| HFG–EHFG | 11.72 | 0.8521 | 0.0001 |
| EHFG–EHFG | 18.52 | 0.8521 | 0.0001 |
LFG low frequency average group, HFG high frequency average group, EHFG extended high frequency average group, SE standard error
* P < 0.05, ** P < 0.01, *** P < 0.001
Discussion
The complete conventional and extra high frequency range contain six and one octave respectively. The former was therefore subdivided into LF and HF ranges in order to reduce this discrepancy to some extent. The main finding in the study is the elevated extended high frequency thresholds in individuals with history of SOM.
An explanation for these results is difficult to find in the light of the present knowledge of the middle ear transmission at extra high frequencies. The following factors may however be relevant. By combination of the pressure amplification and lever action, the middle ear acts as impedance transformer to optimize the flow of energy from air to fluids of the inner ear. As far as the processes of the middle ear are concerned, the concept of the mechanical resonance is fundamental [16]. In such mechanical system two reactive elements, mass and stiffness interact. When reactance of these are equal and opposite, they cancel out each other and resonance occurs. At frequencies below resonance the response is determined by stiffness of the system and at frequencies above resonance the response is determined by the mass of the system. The middle ear ossicles have mass and the stiffness is provided inter alia, by the supporting ligaments and tympanic membrane. In our study, there was a high incidence of pathologic findings in SOM group therefore it can be supposed that these changes in the TM and middle ear space affect the mass characteristics of the middle ear system and cause extra high frequency loss.
Permanent damage to basal cochlear duct has been postulated to occur as a result of leakage of toxins from the middle ear through the round window, reduction of the blood flow to the cochlea,interference with the efferent innervation of the outer hair cells by histamine binding to acetylcholine receptors during the cell mediated immune response at the early stages of effusion and/or local hypoxia (blockage of normal diffusion of oxygen from the tympanic cavity to the perilymph), since perilymphatic oxygen tension in the basal coil is partly dependent on gas diffusion from a ventilated tympanic cavity. Therefore, the obstruction due to fluid accumulation may lead to hypoxia resulting in the permanent cell damage at the basal coil. The contribution of following factors have also been documented regarding extended high frequency loss, lymphatic circulation (blockage of the lymphatic vessels at the sub epithelial layer of round window) and acceleration of atrophic changes that normally occur in the supporting tissues of the cochlear duct with the possible alterations of mass, stiffness and friction of the spiral lamina or the basilar membrane [17]. Another explanation could be that surgical trauma at tube insertion and the suction noise created during aspiration of middle ear fluid may damage hearing. Although suction noise may be excessively loud but, it is short and is concentrated in (1.7–6 kHz) [18]. Our study also shows that the hearing loss is very limited in certain frequencies (2, 4, and 8 kHz) with is also supported by various studies done in the past [19, 20].
The present investigation has employed only the air conduction audiometers at extended high frequencies and therefore the question had remained open whether high frequency hearing loss is related to structural changes in the middle ear space or in cochlea or in both. Another limitation with the study was that no correlation was made between the number of episodes of SOM, the time interval of each episode and the number of time myringotomy done with, the extent of hearing loss.
Conclusion
The present study and many previous studies reported the pronounced impairment of the extended high frequencies in cases of middle ear pathologies [20, 21]. Thus, even in cases of SOM, extended high frequency audiometry should be performed and patients should be kept at regular follow up to check any high frequency damage. Patients should be provided proper counseling regarding their auditory status and their predisposition to EHF loss which may affect speech intelligibility. Further studies are necessary to elucidate the relative contribution of the middle ear pathologies on extended high frequencies and to see whether the impairment of extended high frequencies in these cases is permanent or temporary. The introduction of the electric conduction audiometer which permit audiometric assessment of the inner ear function up to around 16 kHz, should provide clarification.
Conflict of interest
None.
References
- 1.Marcos V, Marcelo MH. Definitions and terminology. Otolaryringol Clin N Am. 1991;2:757–771. [Google Scholar]
- 2.Sade J. Inflammatory and non inflammatory factors related to secretory otitis media. Int J Pediatr Otorhinolaryngol. 1979;1:41–59. doi: 10.1016/0165-5876(79)90028-4. [DOI] [PubMed] [Google Scholar]
- 3.Multu C, Odabasi AO, Metin K, Basak S, Erpek G. Sensory neural hearing loss associated with otitis media with effusion in children. Int J Pediatric Otorhinolaryngol. 1998;46(3):179–184. doi: 10.1016/S0165-5876(98)00159-1. [DOI] [PubMed] [Google Scholar]
- 4.Gravel JS, Wallance IF. Effects of otitis media with effusion on hearing in the first 3 years of life. J Speech Lang Hear Res. 2000;3:631–644. doi: 10.1044/jslhr.4303.631. [DOI] [PubMed] [Google Scholar]
- 5.Robert H, Lisal H. Audiologic evaluation of otitis media patients. Otolayringolog Clin N Am. 1991;24:877–899. [PubMed] [Google Scholar]
- 6.Levine BA, Shelton C, Berliner KI, Sheehy JL. Sensorineural hearing loss in chronic otitis media. Is it clinically significant? Arch Otolaryngol Head Neck Surg. 1989;115:814–816. doi: 10.1001/archotol.1989.01860310052021. [DOI] [PubMed] [Google Scholar]
- 7.Paparella MM, Brady DR, Hoel R. Sensorineural hearing loss in otitis media and mastoiditis. Trans Am Acad Ophthalmol Otolayrangol. 1970;74:108–115. [PubMed] [Google Scholar]
- 8.Cusimano F, Cocita VC, D’Amico A. Sensory neural hearing loss in chronic otitis media. J Laryngol Otol. 1989;103:158–163. doi: 10.1017/S0022215100108333. [DOI] [PubMed] [Google Scholar]
- 9.Arnald W, Ganzer U, Kleinman H. Sensorineural hearing loss in mucous otitis. Arch Otorhinolaryngol. 1977;215:91–93. doi: 10.1007/BF00463196. [DOI] [PubMed] [Google Scholar]
- 10.Smyth GDL. Sensory neural hearing loss in chronic ear surgery. Ann Otol Rhinol Laryngol. 1977;86:1–8. doi: 10.1177/000348947708600102. [DOI] [PubMed] [Google Scholar]
- 11.Schachern PA, Pararella MM, Goycoolea MV, Duvall AJ, III, Choo YB. The permeability of round window membrane during otitis media. Arch Otolaryngol Head Neck Surg. 1987;113:625–629. doi: 10.1001/archotol.1987.01860060051014. [DOI] [PubMed] [Google Scholar]
- 12.Harada T, Yamasoba T, Yagi M. Sensorineural hearing loss associated with otitis media with effusion. ORL J Otorhinolaryngol. 1992;54:61–65. doi: 10.1159/000276263. [DOI] [PubMed] [Google Scholar]
- 13.Sorri M, Rantakallio P. Secretory otitis media and hearing loss. Acta Otolyryngol (Stockh) 1989;457(Suppl):94–99. doi: 10.3109/00016488809138891. [DOI] [PubMed] [Google Scholar]
- 14.Dieroff HG, Schuhmann G. High frequency hearing following otitis media with effusion in childhood. Scand Audiol. 1986;15(Suppl 26):83–84. [PubMed] [Google Scholar]
- 15.Mc Dermott JC, Fausti SA, Frey RH. Effects of middle ear disease and cleft palate on high frequency hearing in children. Audiology. 1986;25:136–148. doi: 10.3109/00206098609078380. [DOI] [PubMed] [Google Scholar]
- 16.Wilson JP. Mechanics of middle and inner ear. Br Med Bull. 1987;43:821–837. doi: 10.1093/oxfordjournals.bmb.a072220. [DOI] [PubMed] [Google Scholar]
- 17.Radaelli de Zinis LO, Luca OR, Campovecchi C, Parrinello G, Antonelli AR (2005) Predisposing factors for inner ear hearing loss association with chronic. Int J Audiol 44:593–598 [DOI] [PubMed]
- 18.Wetmore RF, Hennery WJ, Konkle DF. Acoustical factors of noise created by suctioning middle ear fluid. Arch Otolaryngol Head Neck Surg. 1993;119:762–766. doi: 10.1001/archotol.1993.01880190058012. [DOI] [PubMed] [Google Scholar]
- 19.Marie R, Konard K, Peter W. Hearing loss after refractory otitis media. Acta Otolaryngol. 2005;125:250–255. doi: 10.1080/00016480510003183. [DOI] [PubMed] [Google Scholar]
- 20.Tarlow M. Otitis media pathogenesis and medical sequelae. Ear Nose Throat J. 1998;77(Suppl):3–6. [PubMed] [Google Scholar]
- 21.Iain WS, Mair IW, Oddbjorn F, Einar L. Air conduction thresholds and secretory otitis media: a conventional and extra high frequency audiometric comparison. Ann Otol Rhinol Laryngol. 1989;98:767–771. doi: 10.1177/000348948909801003. [DOI] [PubMed] [Google Scholar]