Abstract
Endoscopic repair of anterior cranial base has been widely reported. However there is still no uniformity in the technique of endoscopic repair of lateral sphenoid cerebrospinal fluid (CSF) leaks. To highlight the management of CSF leak or encephalocele in the lateral sphenoid recess and relate our experiences. We retrospectively reviewed the medical records of all our patients who underwent an endoscopic repair of CSF leaks in the lateral sphenoid recess during the period from September 2003 to January 2010 at our tertiary hospital. Fifteen cases with CSF leaks/encephalocele that were repaired by the endoscopic approach were included. The majority of our cases were spontaneous leaks. In all our cases we approached the site of defect by an end on approach. All our patients were successfully treated in the first attempt. Endoscopic repair of lateral sphenoid recess has shown better surgical outcome with reduced morbidity.
Keywords: Para nasal sinus, Sphenoid sinus, Rhinorrhoea, Cerebrospinal fluid rhinorrhoea, Spontaneous cerebrospinal fluid rhinorrhoea, Surgical procedure, Endoscopic
Introduction
Transnasal endoscopic repair of anterior skull base defect has been in vogue for quite sometime, and it is a natural progression that the same technique can be used to repair other parts of the skull base.
Initially, transcranial approaches were used to repair all CSF leaks. Subsequently extra cranial approaches were developed and popularized [1]. Most of the literature is limited to the anterior cranial fossa leak. Reports of middle cranial fossa leak into the lateral sphenoid are few. A microscopic transseptal approach will not give adequate visualization of the lateral wall and, an underlay placement of graft may not be possible because of the adjacent neurovascular structures. These patients present with profuse watery discharge on bending forward, salty taste in the mouth and nocturnal coughing. Few do present with meningitis and a history of watery nasal discharge can usually be elicited in them.
We present our experiences in managing CSF leaks and encephalocele in this region.
Methods
We retrospectively reviewed the clinical data of all patients who underwent endoscopic sinus surgery for lesions of the lateral recess of the sphenoid sinus with either an encephalocele or a CSF leak. The inpatient notes for the patients identified in the search of primary measure were collected, and each patient’s data set thoroughly evaluated for history of previous trauma, previous sinus surgery, diagnostic work up including CT and MRI studies and postoperative course. Exemplary images from different imaging studies and intraoperative sites were gathered as well. Also data pertaining to perioperative management, including use of nasal packing, and the use of perioperative prophylactic antibiotics were analyzed (Figs. 1, 2 and 3).
Fig. 1.
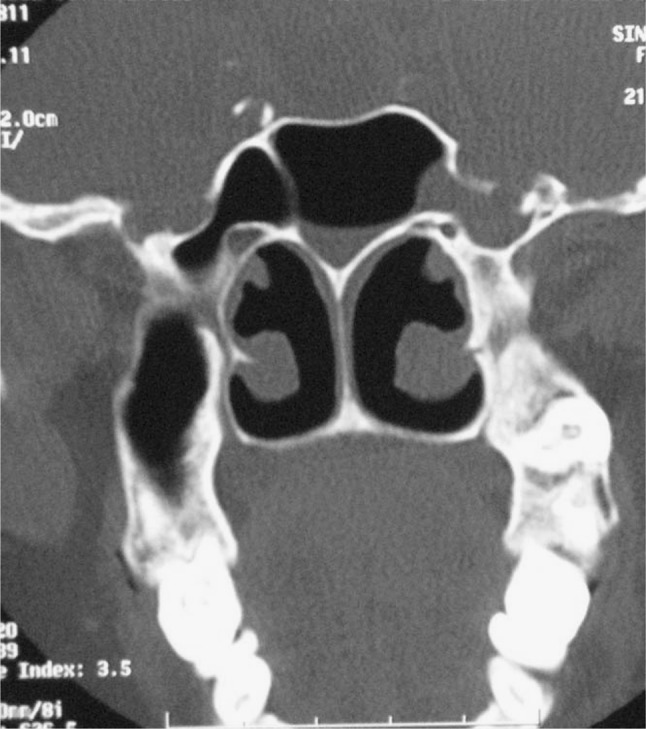
Coronal CT showing the defect in the lateral sphenoid wall
Fig. 2.
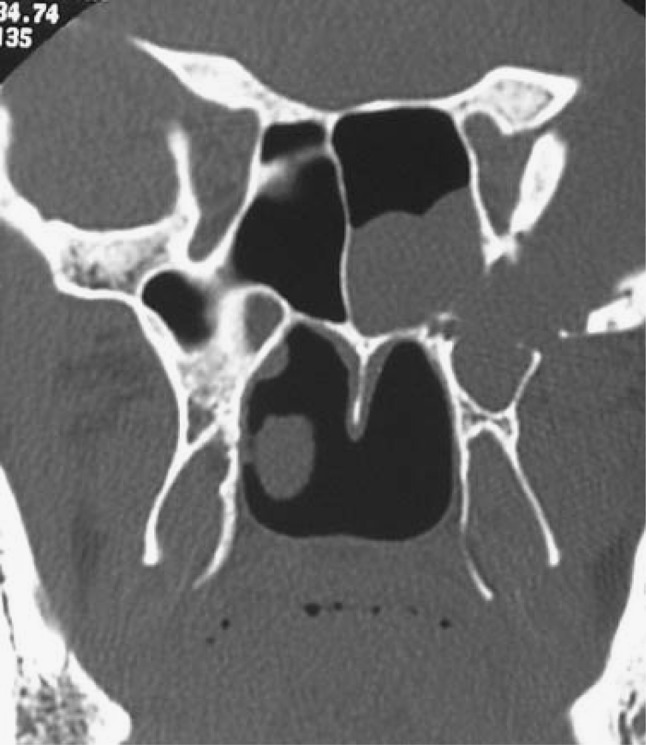
Coronal CT of another patient showing the defect in the lateral sphenoid wall
Fig. 3.
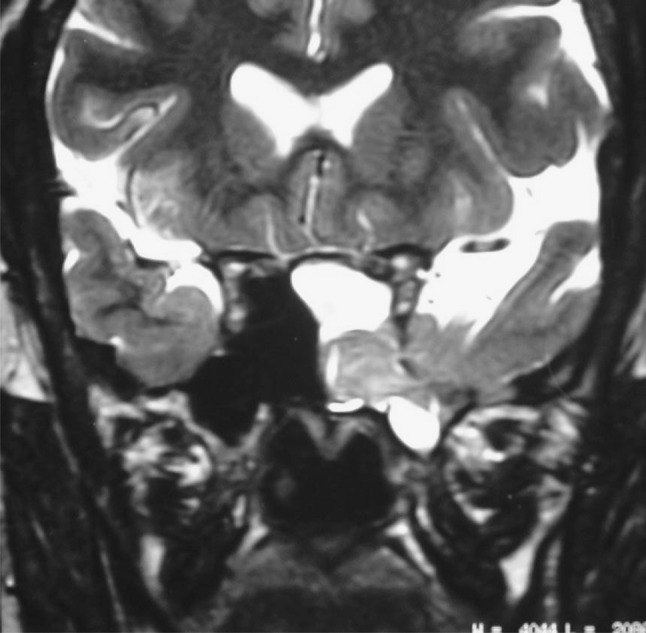
T2 coronal MRI of the same patient as Fig. 2
Results
Between September 2003 and January 2010, 15 patients presented with a CSF leak in the lateral recess of the sphenoid sinus. Our study population was composed of seven male subjects and eight female subjects; their age ranged from 15 to 67 years (mean 45.80). 13 of our patients had spontaneous leaks and one each were following trauma and surgery. Follow up ranged from 6 to 40 months. Complication associated with the CSF leak, before repair, included meningitis in five patients (Table 1).
Table 1.
Patients with lateral sphenoid recess CSF leak
| Patient | Age (years) | Sex | Clinical presentation | Etiology | Side of defect | Type of defect (focal/multiple) | Encephalocoele | Method of repair | Co-morbid conditions |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 40 | F | Rhinorrhoea | Spontaneous | Right | Focal | Absent | AF + RS + TG | Nil |
| 2 | 40 | F | Rhinorrhoea | Spontaneous | Left | Focal | Absent | AF + RS + TG | Nil |
| 3 | 45 | F | Rhinorrhoea | Spontaneous | Left | Focal | Absent | AF + RS + TG | Nil |
| 4 | 67 | M | Rhinorrhoea | Spontaneous | Right | Focal | Absent | AF + RS + TG | Nil |
| 5 | 52 | M | Rhinorrhoea | Spontaneous | Right | Focal | Absent | AF + RS + TG | Nil |
| 6 | 41 | M | Rhinorrhoea | Spontaneous | Right | Focal | Absent | AF + RS + TG | Nil |
| 7 | 15 | F | Rhinorrhoea | Spontaneous | Left | Focal | Absent | AF + RS + TG | Nil |
| 8 | 49 | F | Rhinorrhoea | Spontaneous | Right | Single focal defect with multiple small openings in lateral wall | Present | AF + pedicled nasal septal mucosal flap + TG | Hypertension |
| 9 | 42 | F | Rhinorrhoea | Spontaneous | Left | Focal | Present | AF + RS + TG | Nil |
| 10 | 51 | F | Rhinorrhoea; H/O meningitis | Spontaneous | Left | Focal | Absent | AF + pedicled nasal septal mucosal flap + TG | Nil |
| 11 | 43 | M | Rhinorrhoea; H/O meningitis | Spontaneous | Right | Focal | Absent | AF + RSL + TG | Nil |
| 12 | 29 | F | Rhinorrhoea | H/O Head injury; H/O embolization of dural AV malformation; H/O LP shunt surgery | Left | Focal | Absent | TF + FL + TG + Pedicled nasal septal mucosal flap | Nil |
| 13 | 55 | M | Rhinorrhoea; H/O meningitis | Spontaneous | Right | Focal | Present | TF + FL + TG | Nil |
| 14 | 56 | M | Rhinorrhoea; H/O meningitis | Endoscopic trans-sphenoidal excision of pituitary adenoma done twice; H/O radiation; Gamma knife excision for recurrence | Left | Focal | Absent | AF + RS + TG | Nil |
| 15 | 62 | M | Rhinorrhoea H/o meningitis | Spontaneous | Left | Focal | Absent | TF + FL + inferiorly based nasal mucosal flap | Nil |
Characteristics of the Endoscopic Repair
All our patients presented with watery nasal discharge. Intraoperative endoscopic visualization and its correlation with CT cisternography was used to identify the site of leak. The grafting material used was fascia lata or rectus sheath and thigh fat or abdominal fat. Their order of placement was fat followed by fascia graft followed by fat, which was then supported by an absorbable gelatin sponge and tissue glue. Perioperative management included pre and postoperative antibiotics.
Operative Technique
The initial steps of our approach were the same as in any other endoscopic sinus surgery. An uncinotomy was done, anterior and posterior ethmoids were removed. The posterior end of the middle turbinate was the trimmed and the sphenoid ostium was identified. The same was widened laterally till the lateral end of the recess was reached. The defect was clearly visualized and identified in all its margins. The defect was then packed with fat. The bath plug technique [2] was used to pack the fat in such a way that part of the fat was intracranial and part extracranial. This was then supported by fascia, tissue glue, gelfoam and merocel.
Occasionally we have had cases where there were multiple small openings and the entire sphenoid wall thinned out. In such cases the entire sinus mucosa was denuded and packed with fat, which was supported by a septal mucosal flap based on the splenopalatine artery. The flap is similar to the Hadad flap [3] but smaller as the dissection was limited to the posterior end of the septum.
An angled scope [4] can be used to visualize the defect without drilling the anterior sphenoid sinus wall and an angled bipolar can then be used to burn the gliotic tissue and then plug it with fat, fascia and tissue glue. However we found it more convenient to expose the entire recess. Drilling the anterior wall of the sphenoid sinus does not require much time and is very safe.
The merocel pack was removed on the 5th postoperative morning and the thigh wound sutures were removed on the 10th day.
Discussion
The sphenoid sinus is a developmental outgrowth of the sphenoid bone with variable pneumatization. It may involve a portion or the entire sphenoid bone. Pneumatization of even the pterygoid plates have been reported [5, 6].
Another anatomical variant which needs a mention here is Sternberg’s canal. Originally described by Maximilian Sternberg in 1888, it is a canal extending from junction of the body of sphenoid bone and posterior root of the lesser sphenoid wing just medial to the superior orbital fissure inferiorly to connect with the pharynx at the processes vaginalis or when sufficient pneumatization has occurred into the lateral wall of the sphenoid sinus [7]. Authors have attributed the Sternberg’s canal, as a common site of CSF leak in the lateral recess [7].
CSF leaks in the lateral recess may be due to a culmination of both the factors like anatomical variations mentioned in the previous paragraph and obesity.
Confirmation of the diagnosis is important before starting the treatment. A CSF related rhinorrhoea should be suspected in the presence of a unilateral, watery, clear, nonsticky nasal discharge that is commonly associated with a headache. A sphenoid sinus defect may be suspected with fluid gush on forward tilt of head [8].
We have used beta-2 transferrin to confirm presence of leak in all our cases. A high resolution CT cisternography helps to further confirm and identify the site of the defect. A diagnostic nasal endoscopy helps to further corroborate the site of leak.
MRI cisternography [9] is also becoming increasingly popular as non invasive technique which does not require intrathecal injection and is particularly useful in patients with meningitis.
A number of approaches have been described for the lateral recess of the sphenoid sinus. Historically, transcranial approaches have been used for the surgical management of encephaloceles of the lateral recess of the sphenoid sinus [1, 8, 10]. There have been reports of external approach to reach the lateral recess of the sphenoid sinus [11]. Rivierez and Valsant [12] used a frontotemporal approach with zygomatic osteotomies for accessing a meningoencephalocele in the right lateral sphenoid recess. External approaches however, have a number of disadvantages and the endoscopic approach has firmly found its place as a standard of care [13, 14].
Even within the realm of endoscopy, a number of approaches have been described. Mehandale et al. [14] reported successful repair of three cases of CSF fistula involving the lateral recess using an endoscopic assisted sublabial transseptal approach. They also had their share of failures, which they attributed to lack of availability of instruments which allow manipulation of lesions at the lateral aspect of the sphenoid sinus and freedom to create only a small sphenoidotomy in order to preserve the rostrum to support the graft.
There have been reports of transpterygoid and transethmoidal pterygoidal sphenoidal approach to the lateral recess of the sphenoid sinus [1, 5].
Our approach has evolved from our own past experiences, whereas initially we used to pack the entire sphenoid sinus, we now believe in drillout out the anterior sphenoid wall as far laterally as required to expose the site of defect and close that site only.
Conclusion
Although a number of endoscopic approaches have been described for the lateral recess of the sphenoid sinus, our technique provides a simple direct approach and an orientation to all corners of the defect.
Footnotes
Work done at Department of ENT, P. D. Hinduja National Hospital and Medical Research Centre and Cumballa Hill Hospital, Mumbai.
References
- 1.McCormack B, Cooper PR, Persky M, Rothstein S. Extracranial repair of cerebrospinal fluid fistulas: technique and results in 37 patients. Neurosurgery. 1990;27:412–417. doi: 10.1227/00006123-199009000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Wormald PJ, McDonogh M. The bath plug closure of anterior skull base cerebrospinal fluid leaks. Am J Rhinol. 2003;17:299–305. [PubMed] [Google Scholar]
- 3.Hadad G, Bassagasteguy L, Carru RL, Mataza JC, Kassam A, Synderman CH, Mintz A. A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope. 2006;116:1882–1886. doi: 10.1097/01.mlg.0000234933.37779.e4. [DOI] [PubMed] [Google Scholar]
- 4.Tosum F, Carru RL, Synderman CH, Kassam A, Celin S, Schaitkin B. Endonasal endoscopic repair of cerebrospinal fluid leaks of the sphenoid sinus. Arch Otolaryngol Head Neck Surg. 2003;129:576–580. doi: 10.1001/archotol.129.5.576. [DOI] [PubMed] [Google Scholar]
- 5.Alyea OE. Sphenoid sinus: anatomic study with consideration of the clinical significance of the structural characteristics of the sphenoid sinus. Arch Otolaryngol. 1941;34:225–253. doi: 10.1001/archotol.1941.00660040251002. [DOI] [Google Scholar]
- 6.Earwaker J. Anatomic variants in sphenonasal CT. Radiographics. 1993;3:381–415. doi: 10.1148/radiographics.13.2.8460226. [DOI] [PubMed] [Google Scholar]
- 7.Baranano CF, Cure J, Palmer JN, Woodworth BA. Sternberg’s canal: fact or fiction? Am J Rhinol Allergy. 2009;23:167–171. doi: 10.2500/ajra.2009.23.3290. [DOI] [PubMed] [Google Scholar]
- 8.Schick B, Brors D, Prescher A. Sternberg’s canal—cause of congenital spheniodal meningocele. Eur Arch Otorhinolaryngol. 2000;257:430–432. doi: 10.1007/s004050000235. [DOI] [PubMed] [Google Scholar]
- 9.Shetty PG, Shroff MM, Fatterpekar GM, Sahani DV, Kirtane MV. A retrospective analysis of spontaneous sphenoid sinus fistula: MR and CT findings. AJNR Am J Neuroradiol. 2000;21:337–342. [PMC free article] [PubMed] [Google Scholar]
- 10.Kaufman B, Nulsen FE, Weiss MH, Brodkey JS, White RJ, Sykora GF. Acquired spontaneous, nontraumatic normal pressure cerebrospinal fluid fistulas originating from the middle cranial fossa. Radiology. 1977;122:379–387. doi: 10.1148/122.2.379. [DOI] [PubMed] [Google Scholar]
- 11.Reynolds JM, Tomkinson A, Grigg RG, Perry CFA. Lefort 1 osteotomy approach to the lateral sphenoid sinus encephalocele. J Laryngol Otol. 1998;112:679–681. doi: 10.1017/S0022215100141672. [DOI] [PubMed] [Google Scholar]
- 12.Rivierez M, Valsant P. Spontaneous temporosphenoidal encephalocele. A case report. Neurochirurgie. 2000;46:383–386. [PubMed] [Google Scholar]
- 13.Pasquini E, Sciarretta V, Farneti G, et al. Endoscopic treatment of encephalocele of the lateral wall of sphenoid sinus. Minim Invasive Neurosurg. 2004;47:209–213. doi: 10.1055/s-2004-818522. [DOI] [PubMed] [Google Scholar]
- 14.Mehandale N, Marple BF, Nussenbaum B. Management of sphenoid sinus cerebrospinal fluid rhinorrhoea: making of an extended approach to the sphenoid sinus. Otolaryngol Head Neck Surg. 2002;126:147–153. doi: 10.1067/mhn.2002.122183. [DOI] [PubMed] [Google Scholar]


