Abstract
Background
Implant failure after symphyseal disruption and plating reportedly occurs in 0% to 21% of patients but the actual occurrence may be much more frequent and the characteristics of this failure have not been well described.
Questions/purposes
We therefore determined the incidence and characterized radiographic implant failures in patients undergoing symphyseal plating after disruption of the pubic symphysis.
Methods
We retrospectively reviewed 165 adult patients with Orthopaedic Trauma Association (OTA) 61-B (Tile B) or OTA 61-C (Tile C) pelvic injuries treated with symphyseal plating at two regional Level I and one Level II trauma centers. Immediate postoperative and latest followup anteroposterior radiographs were reviewed for implant loosening or breakage and for recurrent diastasis of the pubic symphysis. The minimum followup was 6 months (average, 12.2 months; range, 6–65 months).
Results
Failure of fixation, including screw loosening or breakage of the symphyseal fixation, occurred in 95 of the 127 patients (75%), which resulted in widening of the pubic symphyseal space in 84 of those cases (88%) when compared with the immediate postoperative radiograph. The mean width of the pubic space measured 4.9 mm (range, 2–10 mm) on immediate postoperative radiographs; however, on the last radiographs, the mean was 8.4 mm (range, 3–21 mm), representing a 71% increase. In seven patients (6%), the symphysis widened 10 mm or more; however, only one of these patients required revision surgery.
Conclusions
Failure of fixation with recurrent widening of the pubic space can be expected after plating of the pubic symphysis for traumatic diastasis. Although widening may represent a benign condition as motion is restored to the pubic symphysis, patients should be counseled regarding a high risk of radiographic failure but a small likelihood of revision surgery.
Level of Evidence
Level IV, case series. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Plate fixation maintains reduction of the disrupted pubic symphysis while the pelvic ligaments heal. This static immobilization may restrict the normal motion of the pubic symphysis, the clinical consequences of which are unknown. Nonetheless, some authors have advocated symphyseal plate removal [3, 10]. However, the restoration of motion to other joints (eg, the syndesmosis and the tarsometatarsal [Lisfranc’s] joint of the foot) after immobilization with orthopaedic implants has been correlated to improved pain, ROM, and validated scores such as the SF-36 [4, 5]. In addition, pelvic hardware has been implicated as a source of pain and several authors have reported a decrease in pain after implant removal [10].
Previous reports have described the rate of fixation failure of the pubic symphysis as ranging between 0% and 21% of cases depending on the method of fixation and the injury pattern [11, 14]. However, failure of fixation was not the focus of these reports. For example, Tornetta et al. [14] found that 21% of rotationally unstable pelvic fractures treated with symphyseal plating had changes on their most recent radiograph compared with postoperative views. Four of their 23 patients had plate breakage with three experiencing recurrent widening of the symphyseal space to 7, 9, and 10 mm. Additionally, the authors noted loss of reduction rarely required revision surgery and was believed to be clinically unimportant. More recently, two small series have briefly discussed symphyseal implant failure after pelvic injury and repair. Similar failure rates were reported by Van Loon et al. [17] who found that 19% of 31 patients with rotationally unstable pelvic ring injuries had asymptomatic loosening of the symphyseal implant. In contrast to previous studies, Collinge et al. [1] reported a much higher occurrence of loosening or breakage of symphyseal hardware. In 20 patients with a saddlehorn pelvic injury (after being bucked from a horse), loosening or breakage of symphyseal hardware was observed in 18 patients (90%) with widening of the pubic space ranging from 1 to 5 mm [1].
Given the disparities reported in the literature regarding symphyseal fixation failure, we therefore determined the incidence and characterized implant failures in a large series of patients undergoing symphyseal plating after disruption of the pubic symphysis. Specifically, we sought to investigate the radiographic changes occurring at the symphyseal repair and in bony alignment at the pubic symphysis.
Materials and Methods
We retrospectively reviewed all 165 patients treated at two regional Level I and one Level II trauma centers with plate fixation for acute disruption of the pubic symphysis between August 2002 and July 2006. We excluded 38 patients for followup less than 6 months, three of whom were known to have died. This left 127 (77%) patients for inclusion in the study (Table 1). The minimum followup was 6 months (average, 12.2 months; range, 6–65 months). No patients were recalled specifically for this study; all data were obtained from prospectively collected trauma databases, medical records, and radiographs. We had prior Institutional Review Board approval for this retrospective study.
Table 1.
Patient and injury characteristics
| Variables | Data |
|---|---|
| Number of patients studied | 127 |
| Mean age | 41 years (range, 18–78 years) |
| Sex | 78% male |
| Mechanism of injury | |
| Automobile crash | 38 |
| Motorcycle/all-terrain vehicle | 36 |
| Horse riding | 22 |
| Fall from height | 17 |
| Industrial | 6 |
| Pedestrian versus motor vehicle | 6 |
| Childbirth | 2 |
| Fracture pattern (Orthopaedic Trauma Association 61-) | |
| B1 | 64 |
| B2 | 11 |
| B3 | 5 |
| C1 | 32 |
| C2 | 8 |
| C3 | 7 |
| Multiple system injuries | 71% |
| Mean pubic diastasis on injury AP radiograph | 37 mm (range, 9–118 mm) |
At the time of injury all patients were evaluated and treated according to Advanced Trauma Life support protocols. This was followed by standardized imaging of the pelvis, including AP, inlet, and outlet plain radiographs and CT. Injury radiographs (AP, inlet, and outlet) were classified by the Tile [13] and the Orthopaedic Trauma Association [18] classifications.
All surgery was performed by one of three surgeons (CC, MTA, BRM). Surgery consisted of either anterior symphyseal plating alone or in combination with posterior fixation when required. Surgery was standardized for all patients with symphyseal disruption and achieved by open reduction and symphyseal plating using a Pfannenstiel approach. Reduction was typically achieved using a pointed reduction clamp carefully applied to the pubic tubercles. Surgical dissection on the anterior aspect of the pubis was avoided. Plating was performed using a four- or six-hole plate and 3.5-mm screws (Matta Pelvic System®; Stryker, Mahwah, NJ, USA, or Synthes’ Reconstruction®, Paoli, PA, USA). This is similar to a contoured stainless steel 3.5-mm reconstruction plate that is reinforced at the middle symphyseal portion with additional material to avoid failure there. This plate accepts 3.5-mm and 4.5-mm screws, although all three reporting surgeons in this study have preferentially used the former unless a screw has stripped requiring revision to a larger screw. No locking screws were used. Seventy-one patients (56%) were treated with posterior fixation applied at the discretion of the surgeon typically based on the injury pattern and the perceived amount of pelvic instability. In 56 of 80 patients, rotationally unstable (B-type) fractures were treated without posterior fixation, whereas all 47 vertically unstable (C-type) injuries were treated with posterior stabilization (iliosacral screws).
Postoperatively, patients were mobilized with physical therapy on the first postoperative day if awake, alert, and they had no other conditions restricting mobility. Patients with multiple injuries were mobilized as soon as was reasonable in the context of their associated trauma. Weightbearing was protected with either toe-touch or nonweightbearing on the side of the posterior injury (at the treating surgeon’s discretion) for a period of 10 to 12 weeks. Patients were allowed to progressively return to full activities after they were fully ambulatory and in relative comfort.
The end point for followup was a clinically healed injury (defined as low pain level and static radiographic findings on sequential followup radiographs > 6 weeks apart at 6 months postinjury), malunion, failure of fixation, or reoperation on the anterior ring. Followup was typically at 4- to 6-week intervals after the perioperative period until discharged from care and included clinical and radiographic assessment (AP pelvis, inlet, and outlet views). From our trauma databases and medical records we extracted patient and injury factors (age, sex, mechanism of injury, other injuries, facture classification, method of treatment, length of followup), treatment methods (fixation pattern), and complications. Major (resulted in death or required surgical or other treatment under anesthesia [Clavien-Dindo III-V]) and minor complications (any deviation from the normal postoperative course without surgical, endoscopic, and radiological interventions [Clavien-Dindo I, II]) were identified [2].
The three treating surgeons (CC, MTA, BRM) independently evaluated radiographs for the following features. We evaluated the last followup AP radiographs for subjective radiographic loss of fixation: screws were considered loosened if there was any interval backout, separation between screw heads and plate, or a distinct radiographic halo (lysis) was noted around the screw threads. Any of these changes on followup radiographs from the immediate postoperative films were noted. We also recorded the occurrence of broken screws or plates. We measured the pubic symphyseal space (defined as the distance between the medial-most aspect of the pubic bone on either side) on injury, postoperative, and last followup AP radiographs [1]. Measurements of the pubic space were standardized in the following manner using electronic radiographic images. On a magnified image of the injury AP pelvis radiograph, we drew a vertical line from the center of the femoral head through the left hip. The distance was measured along this line across the hip from osteochondral line to osteochondral line; we assumed this distance would not change between pre- and postoperative AP pelvis radiographs. On a magnified postoperative AP pelvis radiograph, we used the width of a 3.5-mm screw as a constant from which to measure the symphyseal distance on followup radiographs and to determine radiographic distances across the hip. The latter was then used to estimate the width of the symphyseal space on the preoperative radiographs. All end point data were available for all patients.
The data for continuous variables were presented as means and ranges, whereas for categorical variables, the data were presented as counts and percentages. Differences in proportions such as the presence of failed fixation were compared with Fisher’s exact test. Continuous variables were analyzed using the Student’s t-test for data with two levels of the nominal variable and analysis of variance when there were three or more levels for that variable.
Results
Radiographic changes at the anterior pelvis after symphyseal plating for pubic symphysis disruption were numerous (Table 2). Ninety-five of the 126 patients included for study (75%) had radiographic failure of fixation in the form of screw loosening and/or breakage of their symphyseal fixation by last followup (case example, Figs. 1–3). Sixty-seven patients (71%) had only loose screws, five (5%) had only screws breakage, 16 (17%) had some screws loosen and others that broke, and seven (7%) had a broken plate. Patients with B types had anterior failure at a rate of 74%, whereas in those with C-type injuries, the hardware appeared to fail in 77% (p = 0.19).
Table 2.
Radiographic data
| Variable | Data |
|---|---|
| Mean pubic diastasis on injury AP radiograph | 37 mm (range, 9–118 mm) |
| Mean pubic space on immediate postoperative radiograph | *4.9 mm (range, 2–10 mm) |
| Mean pubic space on final followup radiograph | †8.4 mm (range, 3–23 mm) |
| Patients with fixation failure and pubic space widening of 2–9 mm | 72 (59%) |
| Patients with fixation failure and pubic space widening of ≥ 10 mm | 7 (5.5%) |
| Changes in plate-screw construct associated with symphyseal widening | |
| Screws loosened only | 67 (71%) |
| Broken screws only | 5 (5%) |
| Combination of loosened and broken screws | 16 (17%) |
| Plate breakage | 7 (7%) |
| Patients reoperated for failed fixation | 1 (1%) |
* Statistically different from the injury radiograph (p < 0.05); †statistically different from the immediate postoperative radiograph (p < 0.05).
Fig. 1A–C.
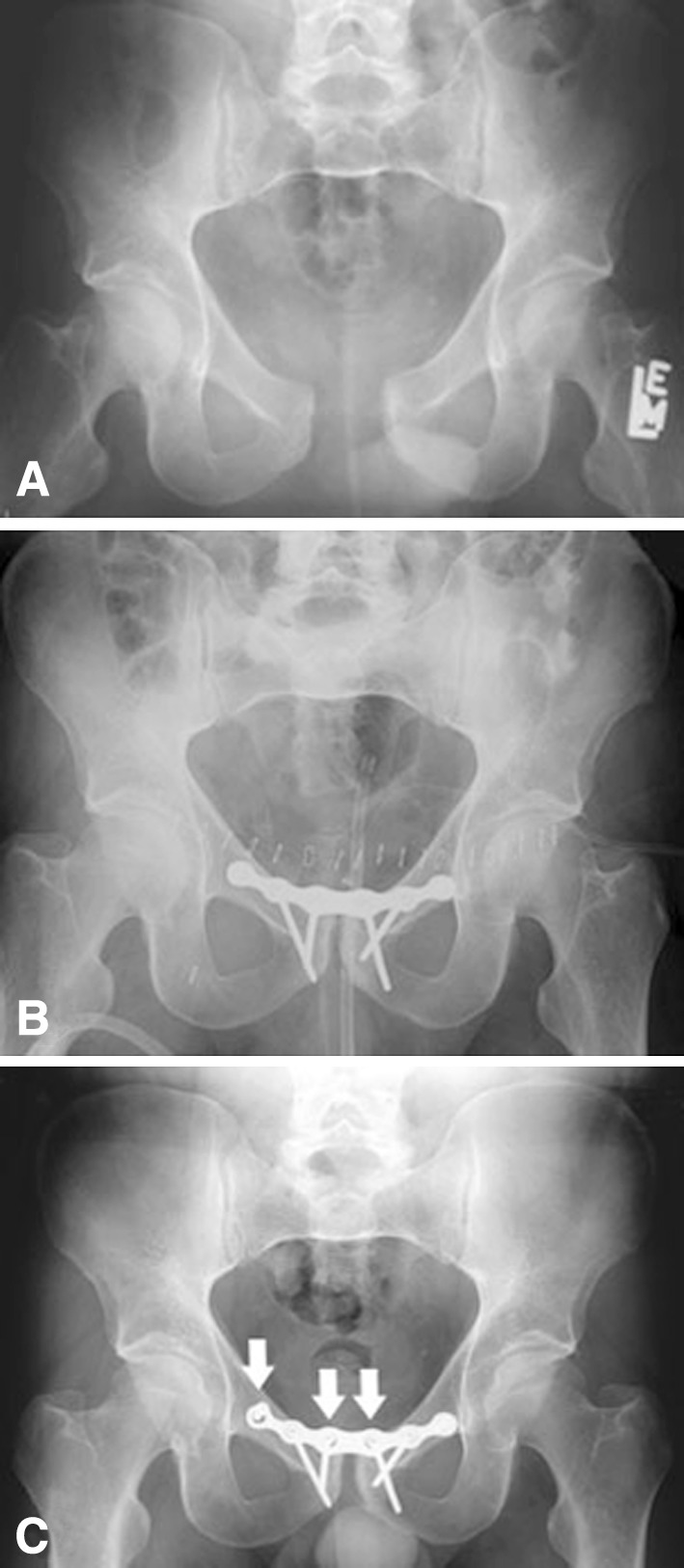
Illustrative case of a 44-year-old man injured in a motorcycle crash. The injury AP radiograph (A) shows a rotationally unstable Orthopaedic Trauma Association 61 pelvic ring injury with pubic diastasis of 38 mm. After standard open reduction and internal fixation using a symphyseal plate (B), the pubic space is measured at 4.5 mm. At last 26-month followup, the AP radiograph (C) demonstrates a loss fixation by means of separation of the screw heads and the plate (seen best at arrows) and widening of the pubic space to 7.6 mm.
The mean pubic symphyseal space was greater (p < 0.001) on the last followup films than on the immediate postoperative radiographs: 8.5 mm (range, 2–24 mm; 95% confidence interval for mean, 7.6–9.3) versus 4.9 mm (range, 2–10 mm; 95% confidence interval for mean, 4.7–5.5), respectively; the mean increase in pubic symphyseal width was 3.4 mm (range, 0–14 mm; 95% confidence interval for mean, 2.7–4.2). Eighty-four of the 95 patients (93%) who had radiographic loosening or breakage of their symphyseal hardware also had widening of their pubic symphyseal space between the immediate postoperative radiographs and those at last followup. Patients without radiographic failure of symphyseal fixation had less widening (p < 0.001) of the pubic symphyseal space than those in whom the hardware had failed (loosened or broken): an average of 1.2 mm (range, 0–4 mm) versus 4.4 mm (range, 0–20 mm), respectively. Patients with fixation failure had a mean widening of the pubic symphyseal space of 3.5 mm, representing a 71% increase in the symphyseal space at an average 10.5 months.
Complications relating to symphysis injury and repair included reoperation on one patient after failure of fixation with recurrent widening of the pubic symphysis to 20 mm. One patient had an acute postoperative wound infection and one an early wound dehiscence, both treated with surgical irrigation and débridement, retention of implants, and secondary wound closure. The patient with infection was treated with 6 weeks of intravenous antibiotics. Both patients’ wounds healed with no further problems. Two patients had implants electively removed. One was a young woman who desired plate removal with the rationale that it might avert potential problems with childbirth, and the other was a man who had a single, loose symptomatic screw and an additional screw that had backed out several centimeters.
Discussion
Plate fixation maintains reduction of the disrupted pubic symphysis while the pelvic ligaments heal. This static immobilization may restrict the normal motion of the pubic symphysis, the clinical consequences of which are unknown. Nonetheless, some authors have advocated symphyseal plate removal [3, 10]. However, the restoration of motion to other joints after immobilization with orthopaedic implants (eg, the syndesmosis and the tarsometatarsal [Lisfranc’s] joint of the foot) has been noted to improve joint motion and pain [4, 5]. In addition, pelvic hardware has been implicated as a source of pain, and some authors have reported improvement in symptoms after implant removal [10]. Previous reports have described the rate of fixation failure of the pubic symphysis as ranging between 0% and 21% of cases, depending on the method of fixation and the injury pattern [1, 11, 14, 17]. Failure of fixation, however, was not the focus of this report, and patients in this study with fixation failure had notable recurrent widening of the symphyseal space. However, patients with the observed symphyseal widening rarely required or underwent revision pelvic fixation because it was believed to be clinically unimportant [14]. In a report describing the outcomes of 20 patients with a saddlehorn pelvic injury after being bucked from a horse, a much higher rate of symphyseal hardware loosening or breakage was reported. In this study, 18 patients (90%) were noted to have radiographic hardware loosening or failure with widening of the pubic space ranging from 1 to 5 mm [1]. Despite this very high rate of radiographic failure, most patients returned to their previous level of activities with similar pain scores to others in the cohort [16]. We therefore determined the incidence and characterized radiographic implant failures in patients undergoing symphyseal plating after disruption of the pubic symphysis.
We recognize limitations to our study. First, this is a radiographic study that includes no clinical correlations or outcomes evaluation. This is, however, important new information regarding the high rate and characteristic pattern of radiographic implant failure after symphyseal plating. Further study regarding the clinical implications of these findings is warranted. Second, the required followup was relatively short at only 6 months. Although this is short in terms of clinical studies, the true incidence of fixation failure and pubic symphyseal widening after anterior plating is most likely underestimated by this study. Third, we had a loss to followup of 24% of patients, which is substantial but compares well with other large series of trauma patients. Fourth, although variations in treatment might have occurred, the operative strategies for the treating surgeons are nearly identical.
We found a high incidence of fixation failure (74%), typically resulting in recurrent widening after plating of a pubic symphyseal disruption. Earlier studies reported failure rates of 0% to 21% after symphyseal plating using similar techniques [14, 17]. These studies have concentrated on factors other than the symphyseal plating, including posterior alignment and fixation, or have had very small patient numbers and have inadequately defined what constitutes fixation failure or malunion. Tornetta et al. [14] noted that four of 27 patients treated operatively for rotationally unstable pelvic fractures broke a 3.5-mm six-hole reconstruction plate and three patients had widening of the pubic space to 7, 9, and 10 mm at an average 39-month followup. Sagi and Papp [11] found that four of 16 patients with rotationally unstable pelvic fractures treated with open reduction and plating using a multihole plate had a failure of fixation and loss of reduction of 5 mm or more. More recently, two small series have briefly discussed symphyseal implant failure and reported clinical outcomes. Van Loon et al. [17] reported on the management and outcomes of 31 rotationally unstable (B1.1) pelvic ring injuries, finding that 19% of patients had asymptomatic loosening of the symphyseal implant and that all of these patients had a very good outcome by pelvic-specific outcome and pain scores. They described loosening or breakage of symphyseal hardware in 18 patients with widening of the pubic space ranging an average of 3.2 mm. Collinge et al. [1] reported the outcomes of 20 patients with a saddlehorn pelvic injury after being bucked from a horse. Finally, if one ignores the radiographic loosening seen in our studies [1], the overall rate of loss of fixation is much closer to the previous literature.
We found patients with fixation failure had a mean widening of the pubic symphyseal space of 3.5 mm, representing a 71% increase in the symphyseal space at an average 10.5 months. There were seven patients with widening of 10 mm or greater on last followup radiographs, although only one (1%) required revision surgery. These results appear similar to previous published series [1, 6, 8, 9, 15, 16] and are indicative of the radiographic natural history of plate fixation of pubic symphyseal disruption. No consensus has been reached as to what amount of malalignment is acceptable after pelvic ring disruption with or without surgical treatment. The natural history of unstable pelvic fractures treated nonoperatively has demonstrated a high incidence of residual disability, pain, pelvic obliquity, and gait disturbances, although patients with anterior ring injuries have fared better than those with more complex patterns [7, 9, 12].
Failure of symphyseal fixation in many cases may simply represent relaxation of the implants as physiological motion is restored to the articulations of the pelvis. However, its clinical relevance remains undefined. To date, there are no data concerning the natural history of pelvic motion after pelvic ring injury and repair or correlating clinical outcomes with this residual pelvic motion. Therefore, patients should be counseled regarding the possibility of radiographic anterior pelvic plate fixation failure.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Harris Methodist Fort Worth Hospital, Fort Worth, TX, USA; the University of Cincinnati Academic Medical Center, Cincinnati, OH, USA; and St Louis University, St Louis, MO, USA.
References
- 1.Collinge CA, Archdeacon MT, LeBus G. Saddle-horn injury of the pelvis. The injury, its outcomes, and associated male sexual dysfunction. J Bone Joint Surg Am. 2009;91:1630–1636. doi: 10.2106/JBJS.H.00477. [DOI] [PubMed] [Google Scholar]
- 2.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giannoudis PV, Chalidis BE, Roberts CS. Internal fixation of traumatic diastasis of pubic symphysis: is plate removal essential? Arch Orthop Trauma Surg. 2008;128:325–331. doi: 10.1007/s00402-007-0429-1. [DOI] [PubMed] [Google Scholar]
- 4.Kuo RS, Tejwani NC, Digiovanni CW, Holt SK, Benirschke SK, Hansen ST, Jr, Sangeorzan BJ. Outcome after open reduction and internal fixation of Lisfranc joint injuries. J Bone Joint Surg Am. 2000;82:1609–1618. doi: 10.2106/00004623-200011000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Manjoo A, Sanders DW, Tieszer C, MacLeod MD. Functional and radiographic results of patients with systematic screw fixation: implications for screw removal. J Orthop Trauma. 2010;24:2–6. doi: 10.1097/BOT.0b013e3181a9f7a5. [DOI] [PubMed] [Google Scholar]
- 6.Matta JM. Indications for anterior fixation of pelvic fractures. Clin Orthop Relat Res. 1996;329:88–96. doi: 10.1097/00003086-199608000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Nepola JV, Trenhaile SW, Miranda MA, Butterfield SL, Fredericks DC, Riemer BL. Vertical shear injuries: is there a relationship between residual displacement and functional outcome? J Trauma. 1999;46:1024–1029. doi: 10.1097/00005373-199906000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Oh CW, Kim PT, Kim JW, Min WK, Kyuung HS, Kim SY, Oh SH, Ihn JC. Anterior plating and percutaneous iliosacral screwing in an unstable pelvic ring injury. J Orthop Sci. 2008;13:107–115. doi: 10.1007/s00776-007-1201-7. [DOI] [PubMed] [Google Scholar]
- 9.Pohlemann T, Gansslen A, Schellwald O, Culemann U, Tscherne H. Outcome after pelvic ring injuries. Injury. 1996;27(Suppl 2):B31–B38. [PubMed] [Google Scholar]
- 10.Raman R, Roberts CS, Pape HC, Giannoudis PV. Implant retention and removal after internal fixation of the symphysis pubis. Injury. 2005;36:827–831. doi: 10.1016/j.injury.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 11.Sagi HC, Papp S. Comparative radiographic and clinical outcome of two-hole and multi-hole symphyseal plating. J Orthop Trauma. 2008;22:373–378. doi: 10.1097/BOT.0b013e31817e49ee. [DOI] [PubMed] [Google Scholar]
- 12.Smith W, Shurnas P, Morgan S, Agudelo J, Luszko G, Knox EC, Georgopoulos G. Clinical outcomes of unstable pelvic fractures in skeletally immature patients. J Bone Joint Surg Am. 2005;87:2423–2431. doi: 10.2106/JBJS.C.01244v. [DOI] [PubMed] [Google Scholar]
- 13.Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surg Br. 1988;70:1–12. doi: 10.1302/0301-620X.70B1.3276697. [DOI] [PubMed] [Google Scholar]
- 14.Tornetta P, 3rd, Dickson K, Matta JM. Outcome of rotationally unstable pelvic ring injuries treated operatively. Clin Orthop Relat Res. 1996;329:147–151. doi: 10.1097/00003086-199608000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Tornetta P, 3rd, Matta JM. Outcome of operatively treated unstable posterior pelvic ring disruptions. Clin Orthop Relat Res. 1996;329:186–193. doi: 10.1097/00003086-199608000-00022. [DOI] [PubMed] [Google Scholar]
- 16.Tornetta P, 3rd, Templeman DC. Expected outcomes after pelvic ring injury. Instr Course Lect. 2005;54:401–407. [PubMed] [Google Scholar]
- 17.Loon P, Kuhn S, Hofmann A, Hessmann MH, Rommens PM. Radiological analysis, operative management and functional outcome of open book pelvic lesions: a 13-year cohort study. Injury. 2011;42:1012–1019. doi: 10.1016/j.injury.2010.11.057. [DOI] [PubMed] [Google Scholar]
- 18.Young JW, Resnik CS. Fracture of the pelvis: current concepts of classification. AJR Am J Roentgenol. 1990;155:1169–1175. doi: 10.2214/ajr.155.6.2122661. [DOI] [PubMed] [Google Scholar]


