Abstract
Background
Diversity among health professionals is believed to be an important step toward improving patient communication and addressing health disparities. Orthopaedic surgery traditionally has been overly represented by Caucasian males, and it remains one of the least racially and gender-diversified surgical subspecialties. As the US population becomes increasingly diverse, a concomitant increase in ethnic diversity and gender diversity is needed to ensure that all Americans receive high-quality, culturally competent health care.
Questions/purposes
We asked whether (1) representation of female orthopaedic residents and clinical faculty and (2) representation of ethnic minority orthopaedic residents, clinical faculty, and basic science faculty increased during the past 15 years since our original study.
Methods
A questionnaire, created on SurveyMonkey®, was distributed by email to the coordinators of all 152 orthopaedic residency training programs in the United States.
Results
Eighty (53%) responses were received. The percentage of female orthopaedic surgery residents and female clinical faculty has nearly doubled since 1995. The percentages of African American, Asian/Pacific Islander, and Hispanic orthopaedic residents, and of clinical faculty have increased. Orthopaedic basic science research faculty is 83% male and is comprised primarily of Caucasians (62%) and Asian/Pacific Islanders (24%).
Conclusions
Despite the increase in diversity in the orthopaedic workforce during the past 15 years, ethnic and gender disparities persist among orthopaedic residency programs regarding residents, clinical faculty, and basic research faculty. To increase diversity in orthopaedic residency programs, an emphasis on recruiting ethnic and gender minority candidates needs to become a priority in the orthopaedic academic community.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-012-2259-x) contains supplementary material, which is available to authorized users.
Introduction
According to the Council on Graduate Medical Education, the ethnic composition of the physician workforce does not reflect the diverse populations in the United States, which contributes to healthcare access problems for underrepresented minorities seeking medical care [12]. Historically, African American and Native Americans have trailed Caucasian Americans in almost every healthcare index, including mortality and compromised average life expectancy [19]. No specialty in the discipline of surgery is devoid of documented evidence of racial disparities [3, 8, 15, 22, 34, 36]. Disparities in minority patient access to appropriate surgical management remain a major problem in the United States [2, 16, 20, 23]. With respect to disparities in orthopaedic care, the rates of total hip arthroplasty and total knee arthroplasty among African American and Hispanic patients are substantially lower than those among non-Hispanic Caucasian patients [24]. Hispanic patients presenting to the emergency department with long-bone fractures are half as likely as non-Hispanic Caucasians to receive pain medication, and they wait nearly twice as long as non-Hispanic Caucasians to receive pain medication [31, 32].
Diversity among health professionals is believed to be an important step toward improving patient communication and addressing healthcare disparities [27]. The profession of orthopaedic surgery traditionally has been overrepresented by Caucasian males, and it remains one of the least racially and gender-diversified surgical subspecialties [4, 5, 17].
The composition of the patients served by orthopaedic surgeons in the United States is changing. Thirty-nine percent of the 2050 population will be comprised of African Americans, Hispanic Americans, American Indians, Alaska Natives, and Pacific Islanders—groups that are underrepresented in the medical profession [32, 33]. As minorities become a larger percentage of the total US population, healthcare access problems and disparities will progressively worsen unless meeting the healthcare needs for this emerging majority becomes a priority.
One of the ways in which underrepresented minority communities can be better served is greater representation from their own minority group serving as their health professionals [21]. Patient-physician race-concordant visits are characterized by higher patient ratings of satisfaction and more positive judgments of physicians’ participatory decision-making style [10, 11, 28]. Minority healthcare professionals are more likely than their Caucasian peers to treat patients of color and to practice in medically underserved communities [7]. As the US population becomes increasingly diverse, a concomitant increase in ethnic diversity among orthopaedic surgeons is needed to ensure that all American citizens receive high-quality, culturally competent health care.
Our previous study, which was conducted in 1995 and based on the most current US Census data at that time, surveyed 159 orthopaedic residency programs and showed that African Americans comprised 12.6% of the population but only 3.6% of the orthopaedic residents; Hispanics comprised 10.2% of the population but only 3% of orthopaedic residents [18]. It is unclear whether any progress has been made to enhance diversity.
Utilizing our previously distributed questionnaire, we reexamined the ethnic and gender workforce in current orthopaedic educational programs across the United States to determine if representation of (1) female orthopaedic residents and clinical faculty and (2) ethnic minority orthopaedic residents, clinical faculty, and basic science faculty has increased during the past 15 years.
Materials and Methods
The pilot questionnaire originally was developed in 1994. It was reviewed by three orthopaedic chairpersons and four orthopaedic clinical faculty members. Based on their comments, a second pilot survey was developed and reviewed by 20 orthopaedic residents. The pilot survey then was revised, finalized, and distributed to 159 orthopaedic residency chairpersons in 1995. This same questionnaire was modified only slightly based on comments from responses received in 1995. The final version of the survey was uploaded onto on SurveyMonkey® (1999–2011 www.SurveyMonkey.com, LLC, Palo Alto, CA, USA) and distributed by email between January 3, 2011, and May 6, 2011, to the coordinators of all 152 Accreditation Council for Graduate Medical Education (ACGME)-accredited orthopaedic educational programs in the United States, which has decreased in number from 159 in 1995 to 152 as of 2010. The coordinators’ email addresses were obtained from the American Medical Association’s Fellowship and Residency Electronic Interactive Database (FREIDA). FREIDA Online has contact information for 9000 graduate medical education programs accredited by the ACGME and for greater than 200 combined specialty programs. Residency coordinators with an active email address were contacted by email and provided a letter that described the purpose of our study and identified the principal investigator. The announcement informed participants that the computerized survey would take approximately 30 minutes to complete and contained a unique, self-identifying link to the survey. Each questionnaire contained 15 questions addressing the ethnicity of the institution’s orthopaedic residents, orthopaedic clinical faculty, and orthopaedic basic science research faculty (supplemental materials are available with the online version of CORR). We categorized ethnicity in the following manner: Caucasian, African-American, Asian/Pacific Islander, Native American/Alaskan Native, Hispanic, and Other. The questionnaire also requested identification of residents’ gender, the proportion of residency graduates who continued in orthopaedic fellowships, and the type of fellowship secured. Participants were informed that survey participation was voluntary and were given the option to decline with no consequence.
No incentives were offered for survey completion. Consent was implied if participants completed and submitted the survey. Followup emails with an attached survey link were sent to nonresponders 3 weeks after initial survey distribution. After the second email wave distribution, 93 typewritten letters were sent to program directors of nonresponding programs. After the third email wave distribution, 10 typewritten letters were sent to nonresponding program chairpersons. Response rates for individual waves were as follows: Wave 1: n = 34 (22%); Wave 2: n = 16 (14%); Wave 3: n = 15 (15%); and Wave 4: n = 10 (11%). We received one letter from a chairperson declining participation. Eighty (53%) responses were received (Table 1).
Table 1.
Geographic distribution of responding and nonresponding programs
| Region | Number (%) of responding programs | Number (%) of nonresponding programs |
|---|---|---|
| New England | 5 (6) | 4 (5) |
| Middle Atlantic | 16 (20) | 16 (22) |
| East North Central | 17 (21) | 9 (13) |
| West North Central | 5 (6) | 5 (7) |
| South Atlantic | 11 (14) | 17 (24) |
| East South Central | 4 (5) | 4 (6) |
| West South Central | 8 (10) | 8 (11) |
| Mountain | 2 (3) | 3 (4) |
| Pacific | 11 (14) | 6 (8) |
| Puerto Rico | 1 (1) | 0 (0) |
| Total | 80 (100) | 72 (100) |
Results
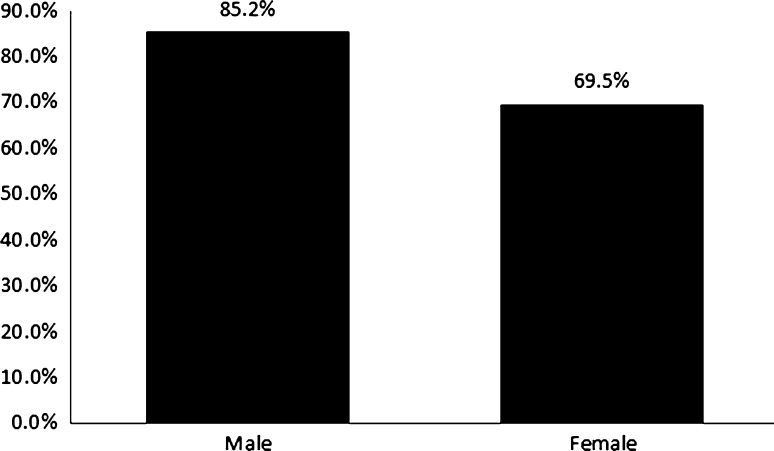
The percentage of female orthopaedic surgery residents and clinical faculty has increased since 1995 (Table 2). A higher percentage of male postgraduate year (PGY)-5 orthopaedic surgery residents secured postgraduate fellowships than female PGY-5 orthopaedic surgery residents (Fig. 1). Only 17% of basic science research faculty is comprised of female researchers (Table 2).
Table 2.
Year percentage comparisons of the gender and ethnic composition of orthopaedic residents, clinical faculty, and research faculty
| Demographic | Residents | Clinical faculty | Research faculty | |||
|---|---|---|---|---|---|---|
| 1995 | 2010 | 1995 | 2010 | 1995 | 2010 | |
| N = 1500 | N = 1877 | N = 1780 | N = 2289 | N = 225 | N = 335 | |
| (%) | (%) | (%) | (%) | (%) | (%) | |
| Female sex | 92 (6.1) | 272 (14.5) | 87 (4.9) | 185 (8.1) | Unknown | 56 (16.7) |
| Ethnicity | ||||||
| Caucasian | 1263 (84.2) | 1447 (77.1) | 1622 (91.1) | 1966 (85.9) | 151 (67.2) | 206 (61.5) |
| African American | 54 (3.6) | 101 (5.4) | 37 (2.1) | 71 (3.1) | 29 (12.9) | 9 (2.7) |
| Asian/Pacific Islander | 99 (6.6) | 221 (11.8) | 45 (2.5) | 179 (7.8) | 20 (9.0) | 82 (24.4) |
| Native American/Alaskan Native | 33 (2.2) | 4 (0.2) | 34 (1.9) | 5 (0.2) | 17 (7.5) | 0 (0) |
| Hispanic | 45 (3.0) | 65 (3.5) | 25 (1.4) | 52 (2.3) | 8 (3.4) | 23 (6.8) |
| Other | 6 (0.4) | 39 (2.1) | 0 (0) | 16 (0.7) | 0 (0) | 15 (4.5) |
Fig. 1.
Of 2009 orthopaedic residency graduates (PGY-5+), men are securing postresidency orthopaedic fellowships at a greater percentage than females.
The percentages of African American, Asian/Pacific Islander, and Hispanic orthopaedic residents and clinical faculty have increased during the past 15 years, whereas the percentages of Caucasian and Native American/Alaskan Native orthopaedic residents have decreased (Table 2). Regarding basic science research faculty, the percentages of African American and Native American researchers have decreased, whereas the percentages of Hispanic and Asian/Pacific Islander researchers have increased (Table 2).
Discussion
As the population treated by orthopaedic surgeons becomes increasingly diverse, there is a need to increase the diversity in the orthopaedic workforce to enhance patient satisfaction and provide high-quality, culturally competent orthopaedic health care. The purpose of our study is to determine if representation of (1) female orthopaedic residents and clinical faculty and (2) ethnic minority orthopaedic residents, clinical faculty, and basic science faculty increased during the past 15 years.
We acknowledge limitations to our study. First, our response rate is 53%. To increase our response rate, we initially contacted the Association of Residency Coordinators in Orthopaedic Surgery to request the listserv of all the orthopaedic residency coordinator members; however, our request was denied owing to privacy issues. We sent typewritten letters to the orthopaedic program directors and chairpersons after the second and third waves of survey distributions. Seventy-two programs did not respond to our survey after four attempts. It is unclear how the metrics of participating programs differed from those of nonparticipating programs. One residency coordinator informed us that the information requested at her institution was not readily available, especially the demographic information of the basic science research faculty. Additionally, we did not mail a hard copy of the survey to orthopaedic residency coordinators who did not respond to our survey. Security firewalls also limited respondents’ access to our emailed surveys. Even though our response rate is 53%, which is similar to the rate in our previous study (56%) [18], this is a respectable response rate for a survey administered by email and does not jeopardize the quality of our findings. Second, the residency coordinators completed the questionnaire. Despite the questionnaire asking questions regarding ethnicity of residents, clinical faculty, and basic science researchers, the residency coordinators were able to obtain this information, although we cannot ensure errors from recall bias.
Compared with the 1995 results [18], our current findings show gender diversity in the orthopaedic workforce has increased during the past 15 years. The percentage of female orthopaedic surgery residents has increased from 6.1% to 14.5%, whereas the percentage of female clinical faculty has increased from 4.9% to 8.1%. Since 1980, women have steadily increased their numbers among medical school graduates. In 2007, women comprised nearly 50% of the 16,142 US medical school graduates [1]. Our data confirm that the number of female orthopaedists likewise has increased during the past 15 years. However, women continue to be underrepresented in orthopaedic surgery residencies. Interestingly, gender underrepresentation in orthopaedics does not reflect a failure of surgical subspecialties as a whole to recruit women; surgical subspecialties other than orthopaedics have been considerably more successful in increasing the numbers of women entering their ranks during the past 35 years [14]. There are several possible explanations for the persistent gender discrepancy in orthopaedic surgery. In the past, women were discouraged from entering orthopaedics given its reputation as a specialty for which women were not physically suited [30]. The orthopaedic profession may lose more than half of the traditional top-tier residency applicant pool unless orthopaedic educational programs increase efforts and effectiveness in recruiting more female applicants [17]. To decrease this gender discrepancy, female medical students should be encouraged to apply to orthopaedic programs and have the opportunity to develop mentoring opportunities with women orthopaedic surgeons or other appropriate mentors to help dispel false stereotypes of the orthopaedic profession.
Our findings also show that ethnic diversity has increased during the past 15 years. African American, Asian/Pacific Islander, and Hispanic orthopaedic residents have increased by 1.8%, 5.2%, and 0.5%, respectively. Similar trends are seen for African Americans, Asian/Pacific Islanders, and Hispanics regarding clinical faculty. Orthopaedic basic science research faculty is comprised primarily of Caucasians and Asian/Pacific Islanders. Despite the increase in diversity in the orthopaedic workforce, ethnic disparities remain among orthopaedic residency educational programs for residents, clinical faculty, and basic science research faculty. In 1995, African Americans and Hispanics comprised 5.8% and 5.7% of US medical school graduates, compared with 6.8% and 6.7% in 2007 [1]. This disparity stems from barriers underrepresented minorities encounter when pursuing an education [21, 35]. These obstacles begin as early as the primary school years and may continue through medical school [21, 26]. Increasing the number of underrepresented minority students who successfully advance through the elementary, secondary, and postsecondary academic pipeline is the first step toward increasing the number of underrepresented minority students eligible to enter medical school and pursue orthopaedics as a career. If underrepresented minorities remain in the academic pipeline, the proportions of underrepresented minority college graduates who apply to medical school are similar to, or even greater than, the proportions of white college graduates applying to medical school [9]. Underrepresented minority college graduates in 2000–2001 applied to medical school at a rate of 28 per 1000 graduates compared with a rate of 25 per 1000 white college graduates applying to medical school that year [13]. Since orthopaedic residency programs are limited to the medical school applicant pool, there is a need for pipeline programs during the elementary and middle school years to subsequently increase the number of underrepresented minorities who enroll in college and medical school [29]. Underrepresented minority medical students interested in orthopaedics should seek out mentors and role models who are able to define and show the requisite academic and research pathways needed to achieve acceptance into an orthopaedic residency.
There have been few studies investigating diversity changes in orthopaedics during the past decade (Table 3). Blakemore et al. [5] reported that the percentage of female orthopaedic residents increased from 0.6% in 1970 to 8.9% in 2001, however, statistical comparison of the fields indicated that the increases in the proportion of women in general surgery, ophthalmology, obstetrics and gynecology, otolaryngology, and urology were greater than the proportion of women in orthopaedic surgery during this 30-year period. Day et al. [14] reported that in 2007, the ethnic composition of orthopaedic residents was lower than for several other specialties including general surgery, neurosurgery, internal medicine, family medicine, and pediatrics. They also stated that African-Americans, Hispanics, and Asian-Americans were underrepresented among orthopaedic faculty compared with their representation in orthopaedic residency programs [14]. Okike et al. [25] reported that from 2001 to 2008, orthopaedic surgery was less diverse than 11 other residencies examined [25]. In addition, temporal analysis conducted by Okike et al. showed that this situation has existed for decades, with no suggestion of change in the near future [25]. Our study showed similar discrepancies in diversity in the orthopaedic workforce. Although there have been improvements in diversity in orthopaedic surgery residencies during the past 15 years, gender and ethnic disparities continue to exist. Therefore, much more needs to be done to encourage women and underrepresented minorities to enter the profession of orthopaedic surgery. It remains unclear why diversity in orthopaedics remains low. The problem may be attributable to a lack of interest, lack of exposure, or lack of support; however, women and underrepresented minorities more often are channeled toward nonsurgical specialties such as internal medicine, pediatrics, and primary care [6]. As minority physicians are more likely to treat patients of color and patients lacking health insurance, and practice in underserved communities, there is evidently a need for more minority orthopaedic surgeons as the population of the United States becomes more diverse.
Table 3.
Comparison of studies investigating diversity in orthopaedics during the past 10 years
| Study | Year of data analysis | Residents | Clinical faculty | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Female | Caucasian | African-American | Hispanic | Female | Caucasian | African-American | Hispanic | ||
| Number (%) | Number (%) | Number (%) | Number (%) | Number (%) | Number (%) | Number (%) | Number (%) | ||
| Blakemore et al. [5] | 2001 | (8.9)# | * | * | * | * | * | * | * |
| Day et al. [14] | 2007 | 399 (12.4) | 2193 (68.3) | 127 (4.0) | 123 (3.8) | 327 (13.4) | 1860 (76.0) | 61 (2.5) | 59 (2.4) |
| Okike et al. [25] | 2008 | * | * | 149 (4.5) | 150 (4.5) | * | * | * | * |
| Current study | 2010 | 272 (14.5) | 1447 (77.1) | 101 (5.4) | 65 (3.5) | 185 (8.1) | 1966 (85.9) | 71 (3.1) | 52 (2.3) |
#Study did not mention raw numbers; * study did not investigate the specified variable.
Electronic supplementary material
Acknowledgments
We thank all of the orthopaedic residency coordinators who participated in our survey especially Ellen Greenberger and Cindy Thompson for their assistance with encouraging participation from members of the Association of Residency Coordinators in Orthopaedic Surgery. We also thank our copyeditor, Linda Harteker, for her comments, suggestions, and reviews. Each of us acknowledges the Timothy L. Stephens Jr MD Orthopaedic Fellowship Program.
Footnotes
This work was performed within the Department of Orthopaedic Surgery, University Hospitals Case Medical Center, Case Western Reserve University School of Medicine, Cleveland, OH, USA. The institution has received funding from St Luke’s Foundation.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
References
- 1.Division of Diversity Policy and Programs. Diversity in Medical Education: Facts and Figures 2008. Washington, DC: Association of American Medical Colleges, Division of Diversity Policy and Programs; 2008. [Google Scholar]
- 2.Ayanian JZ, Cleary PD, Weismann JS, Epstein AM. The effect of patients’ preferences on racial differences in access to renal transplantation. N Engl J Med. 1999;341:1661–1669. doi: 10.1056/NEJM199911253412206. [DOI] [PubMed] [Google Scholar]
- 3.Ball JK, Elixhauser A. Treatment differences between blacks and whites in colorectal cancer. Med Care. 1996;34:970–984. doi: 10.1097/00005650-199609000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Biermann J. Women in orthopaedic surgery residencies in the United States. Acad Med. 1998;73:708–709. doi: 10.1097/00001888-199806000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Blakemore LC, Hall JM, Biermann JS. Women in surgical residency training programs. J Bone Joint Surg Am. 2003;85:2477–2480. doi: 10.2106/00004623-200312000-00031. [DOI] [PubMed] [Google Scholar]
- 6.Boylan M, Grant RE. Diversity and professional excellence. J Natl Med Assoc. 2004;96:1354–1362. [PMC free article] [PubMed] [Google Scholar]
- 7.Butler PD, Longaker MT, Britt LD. Major deficit in the number of underrepresented minority academic surgeons persists. Ann Surg. 2008;248:704–711. doi: 10.1097/SLA.0b013e31817f2c30. [DOI] [PubMed] [Google Scholar]
- 8.Cooper GS, Yuan Z, Landefeld CS, Rimm AA. Surgery for colorectal cancer: race-related differences in rates and survival among Medicare beneficiaries. Am J Public Health. 1996;86:582–586. doi: 10.2105/AJPH.86.4.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139:907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- 10.Cooper RA. Impact of trends in primary, secondary, and postsecondary education on applications to medical school. II: considerations of race, ethnicity, and income. Acad Med. 2003;78:864–876. doi: 10.1097/00001888-200309000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, Ford DE. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282:583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 12.Council on Graduate Medical Education. Third ReportImproving Access to Health Care Through Physician Workforce Reform. Directions for the 21st Century. Rockville, MD: Health Resources and Services Administration; 1992. [PubMed]
- 13.Seventeenth Report Minorities in Medicine: An Ethnic and Cultural Challenge for Physician Training an update. Rockville, MD: Health Resources and Services Administration; 2005. [Google Scholar]
- 14.Day CS, Lage DE, Ahn CS. Diversity based on race, ethnicity, and sex between academic orthopaedic surgery and other specialties: a comparative study. J Bone Joint Surg Am. 2010;92:2328–2335. doi: 10.2106/JBJS.I.01482. [DOI] [PubMed] [Google Scholar]
- 15.Eggers PW. Racial differences in access to kidney transplantation. Health Care Financ Rev. 1995;17:89–103. [PMC free article] [PubMed] [Google Scholar]
- 16.Escarce JJ, Epstein KR, Colby DC, Schwartz JC. Racial differences in the elderly’s use of medical procedures and diagnostic tests. Am J Public Health. 1993;83:948–954. doi: 10.2105/AJPH.83.7.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gebhardt MC. Improving diversity in orthopaedic residency programs. J Am Acad Orthop Surg. 2007;15(suppl 1):S49–S50. doi: 10.5435/00124635-200700001-00012. [DOI] [PubMed] [Google Scholar]
- 18.Grant RE, Banks WJ, Jr, Alleyne KR. A survey of the ethnic and racial distribution in orthopedic residency programs in the United States. J Natl Med Assoc. 1999;91:509–512. [PMC free article] [PubMed] [Google Scholar]
- 19.Groman R. American College of Physicians. Racial and ethnic disparities in health care: a position paper of the American College of Physicians. Ann Intern Med. 2004;141:226–232. doi: 10.7326/0003-4819-141-3-200408030-00015. [DOI] [PubMed] [Google Scholar]
- 20.Harris DR, Andrews R, Elixhauser A. Racial and gender differences in use of procedures for black and white hospitalized adults. Ethn Dis. 1997;7:91–105. [PubMed] [Google Scholar]
- 21.Jiménez RL. Barriers to minorities in the orthopaedic profession. Clin Orthop Relat Res. 1999;362:44–50. [PubMed] [Google Scholar]
- 22.Kokoska ER, Bird TM, Robbins JM, Smith SD, Corsi JM, Campbell BT. Racial disparities in the management of pediatric appendicitis. J Surg Res. 2007;137:83–88. doi: 10.1016/j.jss.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 23.Mort EA, Weissman JS, Epstein AM. Physician discretion and racial variation in the use of surgical procedures. Arch Intern Med. 1994;154:761–767. doi: 10.1001/archinte.1994.00420070077009. [DOI] [PubMed] [Google Scholar]
- 24.Nelson CL. Disparities in orthopaedic surgical intervention. J Am Acad Orthop Surg. 2007;15(suppl 1):S13–S17. doi: 10.5435/00124635-200700001-00005. [DOI] [PubMed] [Google Scholar]
- 25.Okike K, Utuk ME, White AA. Racial and ethnic diversity in orthopaedic surgery residency programs. J Bone Joint Surg Am. 2011;93:e107. doi: 10.2106/JBJS.K.00108. [DOI] [PubMed] [Google Scholar]
- 26.Phillips PJ. Barriers to minority participation in the orthopaedic profession: personal perspectives. Clin Orthop Relat Res. 1999;362:51–54. doi: 10.1097/00003086-199905000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Reede JY. A recurring theme: the need for minority physicians. Health Aff (Millwood). 2003;22:91–93. doi: 10.1377/hlthaff.22.4.91. [DOI] [PubMed] [Google Scholar]
- 28.Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Arch Intern Med. 1999;159:997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- 29.Thomas CL. African Americans and women in orthopaedic residency: the Johns Hopkins experience. Clin Orthop Relat Res. 1999;362:65–71. doi: 10.1097/00003086-199905000-00011. [DOI] [PubMed] [Google Scholar]
- 30.Smith SG, Nsiah-Kumi PA, Jones PR, Pamies RJ. Pipeline programs in the health professions, part 1: preserving diversity and reducing health disparities. J Natl Med Assoc. 2009;101:836–840, 845–851. [DOI] [PubMed]
- 31.Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. JAMA. 1993;269:1537–1539. doi: 10.1001/jama.1993.03500120075029. [DOI] [PubMed] [Google Scholar]
- 32.Minorities in Medicine. Rockville, MD: Department of Health and Human Services; 1998. pp. 3–4. [Google Scholar]
- 33.US Census Bureau. Population Projections of the United States by Age, Sex, Race, and Hispanic Origin: 1995–2050. Available at: www.census.gov/prod/1/pop/p25-1130. Accessed May 15, 2011.
- 34.Wenneker MB, Epstein AM. Racial inequalities in the use of procedures for patients with ischemic heart disease in Massachusetts. JAMA. 1989;261:253–257. doi: 10.1001/jama.1989.03420020107039. [DOI] [PubMed] [Google Scholar]
- 35.White AA., III Resident selection: are we putting the cart before the horse? Clin Orthop Relat Res. 2002;399:255–259. doi: 10.1097/00003086-200206000-00032. [DOI] [PubMed] [Google Scholar]
- 36.Wilson MG, May DS, Kelly JJ. Racial differences in the use of total knee arthroplasty for osteoarthritis among older Americans. Ethn Dis. 1994;4:57–67. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.