Abstract
Background
Stabilization after a pelvic fracture can be accomplished with an anterior external fixator. These devices are uncomfortable for patients and are at risk for infection and loosening, especially in obese patients. As an alternative, we recently developed an anterior subcutaneous pelvic internal fixation technique (ASPIF).
Questions/purposes
We asked if the ASPIF (1) allows for definitive anterior pelvic stabilization of unstable pelvic injuries; (2) is well tolerated by patients for mobility and comfort; and (3) has an acceptable complication rate.
Methods
We retrospectively reviewed 91 patients who incurred an unstable pelvic injury treated with an anterior internal fixator and posterior fixation at four Level I trauma centers. We assessed (1) healing by callous formation on radiographs and the ability to weightbear comfortably; (2) patient function by their ability to sit, stand, lie on their sides, and how well they tolerated the implants; and (3) complications during the observation period. The minimum followup was 6 months (mean, 15 months; range, 6–40 months).
Results
All 91 patients were able to sit, stand, and lie on their sides. Injuries healed without loss of reduction in 89 of 91 patients. Complications included six early revisions resulting from technical error and three infections. Irritation of the lateral femoral cutaneous nerve was reported in 27 of 91 patients and resolved in all but one. Heterotopic ossification around the implants, which was asymptomatic in all cases, occurred in 32 of 91 patients.
Conclusions
The anterior internal fixator provided high rates of union for the anterior injury in unstable pelvic fractures. Patients were able to sit, stand and ambulate without difficulty. Infections and aseptic loosening were reduced but heterotopic ossification and irritation of the LFCN are common.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Anterior external fixation is common for initial stabilization and also for definitive treatment in combination with posterior fixation for unstable pelvic fractures. Several groups report its use for treating vertically stable AP compression injuries [2, 8] and lateral compression pelvic fractures [2, 17]. The complications associated with external pelvic frames include pin tract infection in 2.5% to 50% of patients [1, 2, 4, 11–17, 19, 21], osteomyelitis in 0% to 7% [1, 2, 11, 13, 16, 19], aseptic loosening in 0% to 19% [11, 13, 16, 17, 19], and loss of reduction in 0% to 33% [2, 4, 11] of rotationally unstable injuries treated with a standalone anterior external fixator. Loss of reduction in vertically unstable pelvic injuries treated with an isolated anterior external fixator is reported as high as 95% [11, 12, 18] and as low as 0% to 8% when combined with posterior fixation [4, 13, 16]. Compression of the skin and subcutaneous tissues against the fixator frame has been documented in up to 8% [13] and nerve damage in 0% to 7% [2, 4, 11, 16] of these patients. An anterior pelvic external fixator limits patient mobility, especially when sitting and when being rolled from side to side. In obese patients, external fixation is particularly difficult because the distance from the pelvis to the bar clamp can be 10 to 15 cm, which decreases the stability of the construct and makes large, gaping pin tracts [7]. The external fixator is convenient for the surgeon [12] but is unsightly and cumbersome for the patient. Several articles have advocated constructs with a single pin in the dense supraacetabular region of each ilium [2, 3, 6]. One biomechanical study suggests these anteroinferior pins produce more stable constructs than conventional anterosuperior or iliac pins in rotationally and vertically unstable fracture patterns [9]. The pins are then connected to an external bar or a femoral distracter, which can help reduce the anterior pelvic injury [5].
With the aim of improving patient comfort and minimizing the complications associated with an external fixator, we developed a technique using the established principles of anterior external fixation but with internal implants. The technique consists of single supraacetabular pedicle screws placed in each ilium connected with a subcutaneous rod, which we describe as an anterior subcutaneous pelvic internal fixator (ASPIF) [20].
With a multicenter group who have been engaged in the use of this technique, we asked if this technique (1) allows for definitive anterior pelvic stabilization of unstable fractures resulting in healing; (2) is well tolerated by patients allowing them mobility and comfort; and (3) has a complication rate comparable to a historical rate with anterior external fixation.
Patients and Methods
An Institutional Review Board-approved retrospective review was performed at four Level I trauma centers in the United States. The sites were Detroit Receiving Hospital, University of Utah, Parkland Hospital, and Ortho Indy Methodist Hospital. We retrospectively reviewed 96 patients who underwent ASPIF (Fig. 1) from November 2007 to December 2010 after an unstable fracture of the pelvis. The indication for surgery was an unstable pelvic fracture in which the surgeon believed there was a need for anterior fixation (same as external fixation). The contraindications were: hemodynamically unstable patients, patients with soft tissue defects that prevented coverage of the ASPIF, and patients with fractures through the insertion points of supraacetabular screws. There were 56 males and 40 females with an average age of 39.2 years (range, 16–71 years). Five patients were lost to followup before 6 months, which left 91 patients who were studied. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. The minimum followup was 6 months (mean, 15 months; range, 6–40 months); 69 of the 96 patients (72%) had followup greater than 12 months.
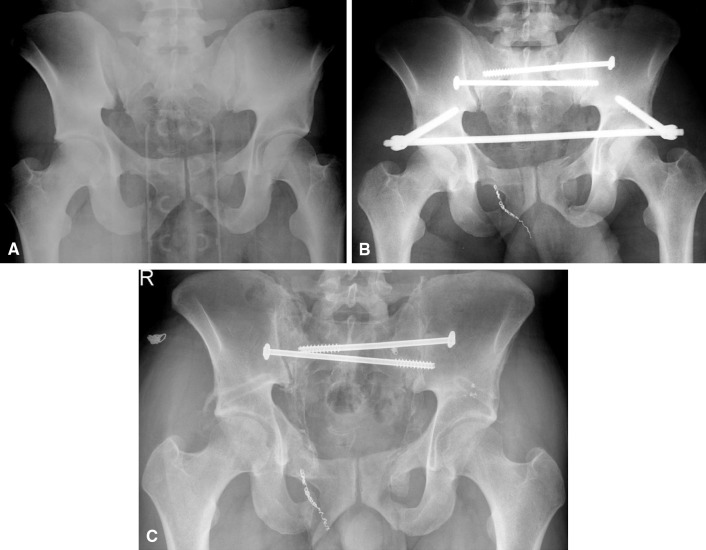
Fig. 1A–C.
(A) An initial AP radiograph showing a patient with an APC3 pelvic injury. (B) The immediate postoperative radiograph after reduction, posterior fixation, and ASPIF. (C) This is a 3-month followup radiograph after removal of the ASPIF, which shows healing and a small amount of heterotopic bone.
All patients had preoperative AP pelvis, inlet and outlet radiographs, pelvic CT scans and were classified according to the Young and Burgess classification of pelvic fractures [22] that is based on the mechanism of injury. It includes lateral compression (LC), AP compression (APC), vertical shear (VS), and a combined mechanism (CM). Lateral compression and APC injuries are further subdivided into three subtypes (Table 1).
Table 1.
Indications for use of anterior subcutaneous pelvic internal fixation in 91 patients
| Pelvic fracture classification Young and Burgess | Pelvic fracture classification AO/OTA | Total |
|---|---|---|
| LC1 | 61-B2.1 | 5 |
| LC2 | 61-B2.2/61-B2.3 | 14 |
| LC3 | 61-B3.2, 61-C2 | 15 |
| APC2 | 61-B1/61-B3.1 | 16 |
| APC3 | 61-C1/61-C3 | 14 |
| VS | 61-C | 20 |
| CM | 61-C | 7 |
| Total | 91 |
LC = lateral compression; APC = AP compression; VS = vertical shear; CM = combined mechanism.
In addition, there were some associated conditions that we believed benefitted from the ASPIF at each site. These conditions included a combination injury of a pelvic fracture and an acetabular fracture (10 patients; Fig. 2), an open pelvic fracture (three patients), a pathologic pelvic fracture (three patients), treatment after failed fixation with other means (three patients), and after a nonhealing osteoporotic fracture (one patient). The ASPIF was used for five cases that were classified as LC1. These were cases that were not able to sit up and be mobile after several days to several weeks. The ASPIF was placed and allowed the patients to sit and get out of bed. It is an unusual indication and we do not recommend this routinely.
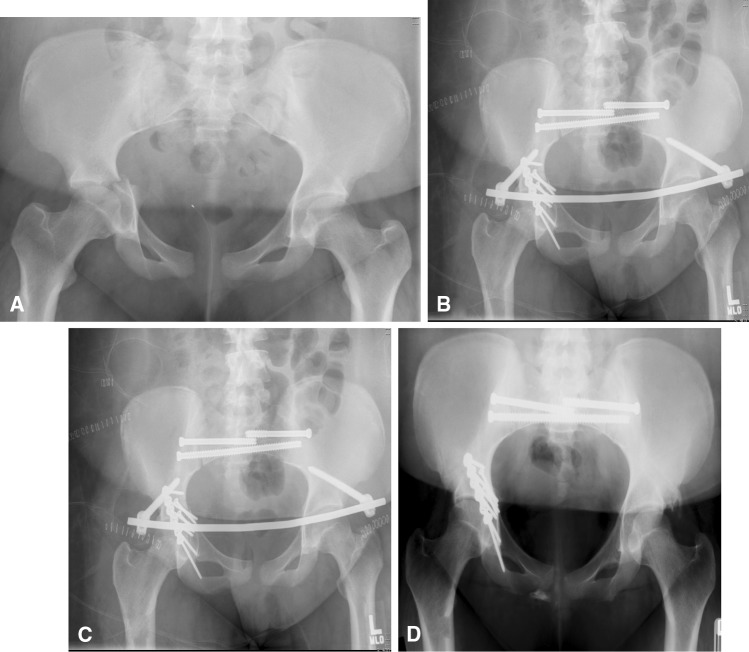
Fig. 2A–D.
(A) A radiograph of a patient with an acetabular fracture associated with an APC2 pelvic injury. (B) The immediate postoperative radiograph after reduction and internal fixation of the posterior injury, the acetabular fracture, and the ASPIF. (C) This is a 3-month postoperative followup film. (D) This is a 10.5-month postoperative film showing healing.
All patients had the appropriate Advanced Trauma Life Support care from trauma surgeons and were brought to the operating room in stable condition. If posterior instability existed, it was addressed first using the standard techniques of reduction and iliosacral screw placement or posterior plating. Two surgeons participating in this study (AJS, DGD) routinely used the Starr Frame to reduce the fracture before fixation [10]. The ASPIF consisted of custom polyaxial pedicle screws used in spinal surgery and a connecting rod. The screws were 7 to 8.5 mm in diameter and 70 to 110 mm in length depending on the size of the patient. These are not normally a part of spinal instrumentation sets so they needed to be specifically requested. The technique for ASPIF insertion, which we used in this group of patients, has been previously described [21].
In the case of APC or VS injuries, the construct is compressed with the standard compression tools found in all spine sets. In the case of LC injuries, the ASPIF was placed without compression or with some distraction if necessary [2]. In the case of a windswept pelvis (LC3), the open posterior injury was fixed first with iliosacral screws to close the posterior component. The ASPIF was applied and the LC component of the injury distracted to reestablish the configuration of the pelvis. Suitable reduction and implant position was confirmed on fluoroscopic AP, inlet, and outlet views.
Postoperative recommendations were toe-touch weightbearing on the side of the posterior injury and weightbearing as tolerated on the side without a posterior injury. Patients with bilateral posterior pelvic injuries remain nonweightbearing. Weightbearing was started at 8 to 12 weeks postinjury depending on radiographs, patient comfort, and surgeon preference and was advanced as tolerated. All sites removed the implant between 3 and 6 months after surgery.
Patients were seen at 2 weeks, 6 weeks, 3 months, 6 months, 1 year, and at latest followup. The patients were asked about their ability to sit, if they had trouble with ambulation because of the implant, if the screw heads bothered them, if the rod bothered them, and if they could lie on their sides. Complications evaluated included loss of fixation or reduction, if the rod was too tight on the abdomen, infection, heterotopic ossification, and lateral femoral cutaneous nerve irritation. Lateral femoral nerve irritation was described as temporary (paresthesias, numbness, or pain that disappeared) or injury (paresthesias, numbness, or pain that was persistent).
The radiographic images at each followup visit included an AP pelvis and inlet and outlet views. These were evaluated by independent observers at three of the four sites (DRH, Parkland, Ortho Indy) and by the surgeon at one site (Utah). Healing was determined by a progression of callus formation until radiographic union and the ability to weightbear without pain. Loss of reduction was determined by failure of the implants to hold the reduction obtained, and failure of fixation was assessed by implant breakage, uncoupling of the ASPIF components, or loosening at the screw-bone interface.
Results
All patients were able to weightbear as tolerated and attained radiographic union. No patient had nonunion at last followup.
All the patients were able to sit and stand with the device in place (91 of 91). Seventy-one of 77 patients who were asked could lie on their sides. Although patients could feel the implants, it did not interfere with their ability to ambulate in any patient (91 of 91).
Early revision surgery was required in a total of six of the 91 patients (7%). Three of these six patients lost reduction (Table 2); in two of these three patients (both APC2), this was attributed to unfamiliarity with the pedicle screw caps. Revision was performed the next day. We believed the caps had been cross-threaded and then had come loose resulting in the loss of fixation. The rod was reinserted on the same screw heads and new caps were placed and were tensioned appropriately. This happened on two occasions and resulted in a successful outcome and maintenance of reduction. In one patient (VS), there was loss of anterior and posterior fixation. A revision was performed of the ASPIF and a second iliosacral screw (S2 screw) was placed after which the reduction was stable. In the other three patients, all of whom were obese, the rod was placed too deep (Fig. 3) leading to patient discomfort, trouble sitting, and a depressed crease in their skin. The patients were brought back to the operating room to place longer and larger diameter screws so that the rod sat much higher above the sartorius muscle and its fascia and they improved. Patients at all four sites noted irritation of the lateral femoral cutaneous nerve: 27 of the 91 patients (30%) had irritation of the nerve, which occurred at the time of insertion of the ASPIF and resolved spontaneously. In one patient, this occurred at the time of removal; the nerve was injured and the patient did not recover. Heterotopic ossification occurred in 32 of the 91 patients (35%) around the implants but did not interfere with function or cause any symptoms. It occurred over the screws, screw caps, and rods in some cases. All hardware was removed between 3 and 6 months in this study population. There were no problems with implant removal at any site. Heterotopic ossification also did not cause any trouble with removal. Three patients sustained infections. One infection was treated by suppressing the infection for 3 months before removing the ASPIF. This patient was also the one with loss reduction, which was revised with revision of the ASPIF and a second iliosacral screw (S2 screw). In two other patients, the infection occurred 4 weeks after fixation. These patients were treated with irrigation, débridement, and removal of the ASPIF. A stress examination was stable so no other fixation was placed. After 6 weeks of antibiotics, the patients held their reduction and did not develop a deep infection (Table 3).
Table 2.
Complications of anterior subcutaneous pelvic internal fixation
| Complication | Total |
|---|---|
| Loss of reduction | 3 |
| Screw bone interface loose | 0 |
| Infection | 3 |
| LFCN irritation | 27 |
| Rod or screw breakage | 0 |
| Rod too tight on the abdomen | 3 |
| Heterotopic ossification | 32 |
LFCN = lateral femoral cutaneous nerve.
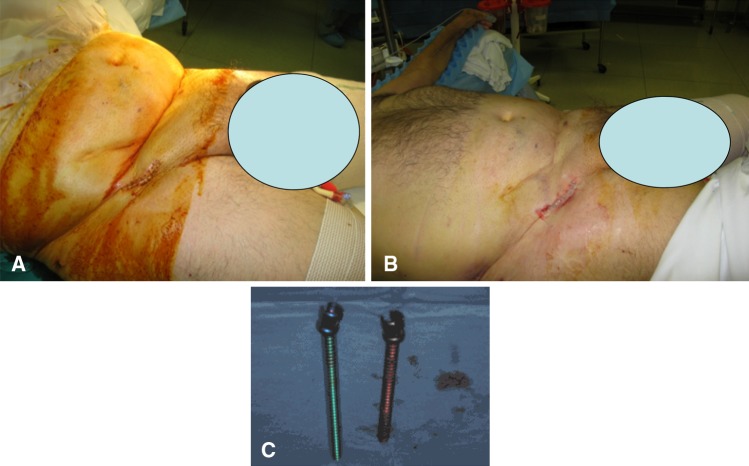
Fig. 3A–B.
(A) This is a photograph of a patient with ASPIF placed with screws sunk too far leading to compression on the abdomen and a skin crease. (B) The photograph after revision with longer screws. (C) A photograph of the new longer versus the old shorter screws.
Table 3.
Clinical results of published studies on definitive external fixation of pelvic fractures
| Author | Number of patients | Pin location | Site infection | Loss of reduction | Aseptic loosening | LFCN injury | Revision surgery | Malunion | Nonunion | HO |
|---|---|---|---|---|---|---|---|---|---|---|
| Scaglione et al. [16], 2010 | 37 | C + S | 35% | 0 | 19% | 0 | 8% | 0 | ||
| Solomon et al. [17], 2009 | 18 | S | 20% | 6% | 0 | 7% | 6% | 0 | ||
| Bellabarba et al. [2], 2006 | 14 | S | 29% | 0 | 0 | 7% | 0 | 0 | ||
| Gänsslen et al. [4], 2005 | 45 | C | 5% | 0 | 0 | 2% | ||||
| Mason et al. [13], 2005 | 52 | C | 50% | 4% | 10% | 17% | 0 | |||
| Arazi et al. [1], 2000 | 41 | C | 19% | 12% | 0 | 0 | 0 | |||
| Tucker et al. [19], 2000 | 40 | C | 2.5% | 7.5% | 7.5% | 10% | 0 | |||
| Lindahl et al. [11], 1999 | 110 | C | 24% | 60% | 2% | 2% | 0 | 58% | 5% | |
| Hupel et al. [7], 1998 | 42 | C | 0% | 17% | 17% | 0 | ||||
| Riemer et al. [15], 1993 | 48 | C | 12% | 0 | ||||||
| Majeed [12], 1990 | 42 | C | 34% | 19% | ||||||
| Wild et al. [21], 1982 | 43 | C | 23% | 28% | 21% | 0 | ||||
| Mears and Fu [14], 1980 | 11 | C | 18% | 0 | ||||||
| Current study | 91 | S | 3% | 2% | 0% | 30%/1% | 6% | 0 | 30% |
LFCN = lateral femoral cutaneous nerve; HO = heterotopic ossification; C = screws placed in the iliac crest; S = subcristal or supraacetabular screws.
Discussion
The role of external fixation in improving outcomes of pelvic fractures has been demonstrated in several studies. However, the complication rates reported have ranged from 12% to 58% [1, 2, 4, 7, 11–17, 19, 21] (Table 3). We devised an internal subcutaneous fixator (ASPIF) and hypothesized that it would stabilize unstable pelvic fractures resulting in healing with decreased complications. Our aim was to corroborate our early results [20] in a larger study with experienced pelvic surgeons and identify feasibility issues for a future prospective study. Specifically we asked if ASPIF (1) allows for definitive anterior pelvic stabilization of unstable fractures resulting in healing; (2) is well tolerated by patients allowing them mobility and comfort; and (3) has a comparable complication rate as that historically reported with anterior external fixation.
There are a number of limitations in the present study. First, this was a retrospective review and the number from each site was small (19–33). Even with these small numbers, we found the approach easy to use and had similar outcomes and similar complications. Second, the study lacked a control group and disallowed direct comparison of results. This is the first study of its kind and serves to assess if ASPIF is a useful technique and if we should pursue its use further. Third, like with every new technique, there is a learning curve and some of the complications in the study may be related to this process so the results here are reported with all surgeons at the learning curve level. However, every surgeon involved in this study has considerable experience with pelvic surgery and the findings might not be generalizable to those who provide such treatment on an occasional basis. Fourth, the ASPIF technique uses FDA-approved implants for spinal fixation in an unapproved method in the pelvis. It is thus an off-label use. All sites used tools and implants that were available from spinal fixation sets but different implants were used at each site. An FDA-approved implant will take time in development. Finally, we had no rigorous approach to assessing radiographic union (eg, strict definitions, multiple blinded observers) and each surgeon evaluated their own radiographs. However, at last followup none of the patients had obvious nonunion.
We found the ASPIF in combination with posterior fixation allowed stabilization of unstable pelvis fractures resulting in predictable healing in all 91 patients. This is not unusual because the healing of unstable pelvic injuries with the use of external fixation has been reported to have low rates of nonunion (0%–4%) [1, 2, 4, 11–17, 19, 21] (Table 3).
It is well known that external fixators are cumbersome for patients as a result of their bulk, external location, and pin tracts. This is more evident in external pelvic fixators that tent across the abdomen. It makes it difficult for patient mobility. In the present study, all sites evaluated patient function by asking them to comment on their ability to sit, stand, lie on their sides, and their ability to tolerate the implants. It was clear from the responses that 91 of 91 patients had the ability to sit, stand, and ambulate with the device in place. The patients did report feeling the subcutaneous rod and several patients could feel the screw heads under their skin, but all patients tolerated the procedure well and none had the ASPIF removed because of discomfort or the inability to mobilize.
Revision surgeries occurred for six of 91 (7%) cases. Loss of reduction occurred in three of 91 cases (4%). Two were the result of unfamiliarity with the implants and failure of both anterior and posterior fixation in a third patient. We believe we could have avoided all three cases because they were attributed to technical error, were subsequently repaired, and led to good outcomes even in the patient with anterior and posterior failure who also had an infection. Loss of reduction has been reported in 7.5% to 60% of cases [7, 11, 19, 21] with anterior fixation as the definitive treatment of the pelvic injury before 2000 but with modern fixation techniques and supplemental posterior fixation, it has fallen to 0% to 6% [4, 13, 16, 17]. Three patients had the screw heads sunk too low resulting in the rod compressing the pelvic muscle and fascia. They were corrected with longer screws reinforcing the importance of keeping the screws off the bone, above the level of the fascia, but also at the level of the subcutaneous rod. In obese patients, there can be up to 5 cm of fat between the sartoris fascia and the skin, which provides a large space for the rod. It is better to leave the screw heads more prominent so the rod has little pressure on the fat and fascia here. Infection of the ASPIF occurred in three instances (4%) despite the device being internal. These infections resolved with eventual removal and antibiotics. This is certainly more troublesome than pin site infections occurring in 4% to 50% of patients with external fixation [1, 2, 4, 11–17, 19, 21] but which often can be treated with local care and antibiotics. Removal of definitive external fixation frames in the treatment for pelvic fractures owing to infection reportedly occurs in 0% to 12% of patients [1, 2, 4, 11, 13–17, 19, 21]. Aseptic loosening of the device was not noted in this series and is likely the result of the larger diameter screws that we use (7–8.5 mm) and the fact that the rod to bone distance is decreased with having an internal rod versus a rod that sits 5 to 10 cm above the skin and another 3 to 5 cm from the skin-to-bone interface. The literature reports an incidence of 0% to 19% [1, 2, 4, 11, 13–17, 19, 21] of this complication with several articles attributing the loosening to loss of fixation.
Temporary irritation of the lateral femoral cutaneous nerve was observed in 30% of patients, being transient in all except one (one of 91). This was diagnosed with altered sensation or pain in its distribution. It is possible to injure the nerve during implantation and removal requiring awareness of this complication. Prior studies using supraacetabular pins [2, 5, 6] have reported injury to the lateral femoral cutaneous nerve in zero of 37 [16], one of 14 (7%) [2], and three of 45 (7%) [4] patients, which is much lower. These studies listed injured nerves and we listed irritation and permanent injury. We postulated that technique may have something to do with this, but it was present at all sites and each surgeon is familiar with supraacetabular placement of Schanz pins. Perhaps the placement and existence of a subcutaneous rod may have had something to do with this occurrence. We believe this requires further study and patients should be warned about the possible injury to the lateral femoral cutaneous nerve when doing the procedure and that it is usually temporary.
Heterotopic ossification was a common finding in our review and was noted in 32 of 91 patients (35%). Although the incidence of this complication is high in the present study, we have not noted any adverse effect of this occurrence to this date and we continue to follow the patients. Previous reports have recommended thorough lavage of the surgical site for prevention of this complication. We believed it was more prominent in patients who had the ASPIF left in longer; however, we were unable to prove that with the current database.
The subcutaneous fixator is intended as a temporary treatment with removal typically performed after 12 weeks. The device requires removal in the operating room, unlike an external fixator that may be removed in an outpatient setting.
Disruptions of the pelvic ring are complex injuries and should be managed on a case-specific basis. The ASPIF technique offers comfort and mobility for patients; it is not difficult to use because it builds on the prior work on external pelvic fixation [1, 2, 4, 7, 11–17, 19, 21], two pin fixators [2, 4, 19], and subcristal pin location [2, 4, 17]. It allows stable anterior fixation when combined with posterior reduction and fixation where indicated. Several complications, including technical errors, can be avoided by adhering to a proper technique and being familiar with the implants. Infection rates (3%) and aseptic loosening (0%) are low but heterotopic ossification and irritation of the lateral femoral cutaneous nerve are common and need to be further evaluated.
Footnotes
One of the authors (RV) is a consultant for Stryker Corporation to develop a commercial product related to the topic of this article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
This work was performed at the Detroit Medical Center, Wayne State University, Detroit Receiving Hospital, Detroit, MI, USA; University of Utah, Salt Lake City, UT, USA; Parkland Memorial Hospital, Dallas, TX, USA; and Ortho Indy Methodist Hospital, Indianapolis, IN, USA.
References
- 1.Arazi M, Kutlu A, Mutlu M, Yel M, Kapiciğlu MI. The pelvic external fixation: the mid-term results of 41 patients treated with a newly designed fixator. Arch Orthop Trauma Surg. 2000;120:584–586. doi: 10.1007/s004020000142. [DOI] [PubMed] [Google Scholar]
- 2.Bellabarba C, Ricci WM, Bolhofner BR. Distraction external fixation in lateral compression pelvic fractures. J Orthop Trauma. 2006;20(Suppl):S7–S14. [PubMed] [Google Scholar]
- 3.Bucholz RW, Heckman JD, Court-Brown C, editors. Rockwood and Green’s Fractures in Adults. 6. Philadelphia, PA, USA: Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 4.Gänsslen A, Pohlemann T, Krettek C. A simple supraacetabular external fixation for pelvic ring fractures] [in German. Oper Orthop Traumatol. 2005;17:296–312. doi: 10.1007/s00064-005-1134-2. [DOI] [PubMed] [Google Scholar]
- 5.Gardner MJ, Nork SE. Stabilization of unstable pelvic fractures with supraacetabular compression external fixation. J Orthop Trauma. 2007;21:269–273. doi: 10.1097/BOT.0b013e318030e3e4. [DOI] [PubMed] [Google Scholar]
- 6.Haidukewych GJ, Kumar S, Prpa B. Placement of half-pins for supra-acetabular external fixation: an anatomic study. Clin Orthop Relat Res. 2003;411:269–273. doi: 10.1097/01.blo.0000069899.31220.d7. [DOI] [PubMed] [Google Scholar]
- 7.Hupel TM, McKee MD, Waddell JP, Schemitsch EH. Primary external fixation of rotationally unstable pelvic fractures in obese patients. J Trauma. 1998;45:111–115. doi: 10.1097/00005373-199807000-00024. [DOI] [PubMed] [Google Scholar]
- 8.Kellam JF. The role of external fixation in pelvic disruptions. Clin Orthop Relat Res. 1989;241:66–82. [PubMed] [Google Scholar]
- 9.Kim WY, Hearn TC, Seleem O, Mahalingam E, Stephen D, Tile M. Effect of pin location on stability of pelvic external fixation. Clin Orthop Relat Res. 1999;361:237–244. doi: 10.1097/00003086-199904000-00030. [DOI] [PubMed] [Google Scholar]
- 10.Lefaivre KA, Starr AJ, Reinert CM. Reduction of displaced pelvic ring disruptions using a pelvic reduction frame. J Orthop Trauma. 2009;23:299–308. doi: 10.1097/BOT.0b013e3181a1407d. [DOI] [PubMed] [Google Scholar]
- 11.Lindahl J, Hirvensalo E, Böstman O, Santavirta S. Failure of reduction with an external fixator in the management of injuries of the pelvic ring. Long-term evaluation of 110 patients. J Bone Joint Surg Br. 1999;81:955–962. doi: 10.1302/0301-620X.81B6.8571. [DOI] [PubMed] [Google Scholar]
- 12.Majeed SA. External fixation of the injured pelvis. The functional outcome. J Bone Joint Surg Br. 1990;72:612–614. doi: 10.1302/0301-620X.72B4.2380212. [DOI] [PubMed] [Google Scholar]
- 13.Mason WT, Khan SN, James CL, Chesser TJ, Ward AJ. Complications of temporary and definitive external fixation of pelvic ring injuries. Injury. 2005;36:599–604. doi: 10.1016/j.injury.2004.11.016. [DOI] [PubMed] [Google Scholar]
- 14.Mears DC, Fu FH. Modern concepts of external skeletal fixation of the pelvis. Clin Orthop Relat Res. 1980;151:65–72. [PubMed] [Google Scholar]
- 15.Riemer BL, Butterfield SL, Diamond DL, Young JC, Raves JJ, Cottington E, Kislan K. Acute mortality associated with injuries to the pelvic ring: the role of early patient mobilization and external fixation. J Trauma. 1993;35:671–677. doi: 10.1097/00005373-199311000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Scaglione M, Parchi P, Digrandi G, Latessa M, Guido G. External fixation in pelvic fractures. Musculoskelet Surg. 2010;94:63–70. doi: 10.1007/s12306-010-0084-5. [DOI] [PubMed] [Google Scholar]
- 17.Solomon LB, Pohl AP, Sukthankar A, Chehade MJ. The subcristal pelvic external fixator: technique, results, and rationale. J Orthop Trauma. 2009;23:365–369. doi: 10.1097/BOT.0b013e3181a2aec3. [DOI] [PubMed] [Google Scholar]
- 18.Tile M. The management of unstable injuries of the pelvic ring. J Bone Joint Surg Br. 1999;81:941–943. doi: 10.1302/0301-620X.81B6.10474. [DOI] [PubMed] [Google Scholar]
- 19.Tucker MC, Nork SE, Simonian PT, Routt ML., Jr Simple anterior pelvic external fixation. J Trauma. 2000;49:989–994. doi: 10.1097/00005373-200012000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Vaidya R, Colen R, Vigdorchik J, Tonnos F, Sethi A. Minimally invasive treatment of unstable pelvic ring injuries with an internal anterior fixator and posterior iliosacral screw. J Orthop Trauma. 2011 Oct 22 [Epub ahead of print]. [DOI] [PubMed]
- 21.Wild JJ, Jr, Hanson GW, Tullos HS. Unstable fractures of the pelvis treated by external fixation. J Bone Joint Surg Am. 1982;64:1010–1020. [PubMed] [Google Scholar]
- 22.Young JW, Burgess AR, Brumback RJ, Poka A. Pelvic fractures: value of plain radiography in early assessment and management. Radiology. 1986;160:445–451. doi: 10.1148/radiology.160.2.3726125. [DOI] [PubMed] [Google Scholar]