Abstract
Background
Lateral compression (LC)-type pelvic fractures encompass a wide spectrum of injuries. Current classification systems are poorly suited to help guide treatment and do not adequately describe the wide range of injuries seen in clinical practice.
Questions/purposes
We therefore (1) defined the spectrum of injuries that compose LC fractures with respect to both anterior and posterior ring injuries, with particular focus on the morphology of sacral fractures, and (2) identified fracture patterns associated with displacement at presentation.
Methods
We retrospectively reviewed 318 LC pelvic fractures. Displacement of the anterior pelvic ring was identified and measured on plain radiographs and posterior displacement was identified by CT.
Results
All 318 patients had an anterior injury and all but 13 (4%) had a posterior injury; 263 of the 318 fractures (87%) included a sacral fracture, with 162 of 318 (51%) having an anterior incomplete sacral fracture, 53 (17%) a complete simple fracture, and 48 (15%) a complete comminuted fracture. Forty-two of 318 (13%) had a crescent fracture. One hundred six of 318 (33%) were displaced at presentation. There was a higher incidence of initial displacement observed in fractures including bilateral rami fractures, a comminuted sacral fracture, or a crescent fracture.
Conclusions
LC pelvic fractures represent a heterogeneous group of injuries with a wide range of associated fracture patterns. In particular, there is a wide range of fracture types represented by injuries classified as LC1 (involving any sacral fracture). Fractures with more complex sacral fractures, crescent fractures, or bilateral pubic rami fractures tend to have higher degrees of initial displacement.
Level of Evidence
Level IV, diagnostic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
Lateral compression (LC)-type pelvic fractures are the most common type of pelvic fracture, accounting for 57% of the injuries reported by Young et al. [13, 14]. Despite their relatively common occurrence, our understanding of LC fracture patterns and their treatment are still evolving. Treatment of LC pelvic fractures depends on fracture stability. Stable fractures should withstand normal physiologic loading without substantial displacement over time, while unstable fractures will tend to displace [6, 9]. Fractures thought to be stable are generally treated nonoperatively while fractures thought to be unstable or initially displaced are usually reduced and surgically stabilized [2, 6, 8, 9]. Current classification systems provide little information regarding the stability of a substantial number of these injuries, particularly those that involve a sacral fracture.
Young and Burgess [13] grouped LC injuries into three types. The LC1 group includes any fracture of the sacrum, the LC2 group includes only crescent fractures, and the LC3 group includes only a very specific pattern in which the pelvis compresses on one side and opens on the other (a so-called “windswept pelvis” [2]). Crescent fractures are defined as a vertical posterior iliac wing fracture leaving the posterior superior iliac spine and posterior sacroiliac ligaments attached to the sacrum, resulting in a rotationally unstable hemipelvis [12]. The wide variety of sacral fractures, either displaced or nondisplaced, seen in clinical practice makes this classification poorly suited to help understand stability.
The AO classification of pelvic fractures is primarily based on stability [11]. Type A fractures do not affect the pelvic ring and are considered stable. Type B fractures are considered partially unstable and include fractures with no more than a partially disrupted posterior arch. The Type C fractures include fractures where the posterior arch has been completely disrupted.
It is generally accepted that unstable fractures require stabilization to prevent displacement [12]. The decision as to whether to surgically manage many LC-type fractures is difficult in practice. Both commonly used classification systems do not provide surgeons with enough information to determine treatment. Buckle fractures [14] and many complete but nondisplaced fractures of the sacrum are considered stable and most surgeons believe they do not require fixation [10]. However, according to the AO classification, these factures would have to be classified as partially unstable. If the fracture completely transverses the sacrum but is not displaced, is it a stable, partially unstable, or completely unstable fracture? Moreover, to classify the fracture according to the AO classification, it is necessary to identify stability, but currently there is little information that tells us how various fracture patterns affect stability.
CT has given us a better understanding of variety of LC injuries, particularly injuries of the sacrum, which are poorly visualized on plain films [3]. The sacral injuries associated with LC injuries are varied and range from incomplete buckle fractures to complete, comminuted fractures [5]. These fractures are currently poorly described in current classification schemes. As our understanding of LC fractures has evolved, it has become clear the anterior injury pattern, posterior injury pattern, and initial displacement are important variables in predicting fracture stability [1, 10, 12]. A more thorough understanding of displacement of both the anterior and posterior ring will hopefully identify fracture patterns that could be at higher risk for displacement or who may be candidates of examination under anesthesia (EUA).
We therefore addressed the following questions: (1) What is the anatomic spectrum of injuries seen with LC-type pelvic fractures? (2) How often are LC-type pelvic fractures displaced, and are specific injury patterns more likely to be displaced? And (3) is there a correlation between the severity of the anterior ring injury (bilateral versus unilateral pubic rami fractures) and the posterior ring injury?
Patients and Methods
We retrospectively reviewed all patients treated with a pelvic fracture at two Level 1 trauma centers from January 1, 2003, through December 31, 2009. Patients were identified through query of our prospectively collected trauma database. Patients were included in the study if they were at least 18 years old at the time of their injury and had at least an AP pelvic film and a CT scan of their injury. Of the 348 patients with confirmed LC pelvic fractures treated during this period, 318 had radiographs of adequate quality in terms of penetration and rotation to allow for classification and measurement of displacement and were included in this study. Of the patients included in the study, 195 were women and 123 were men. Median age was 55 years (range, 18–96 years). The mechanism of injury was a fall in 45% of the patients, a multivehicle crash in 39%, and different factors in 16% (Table 1). No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. Approval was obtained from the institutional research board before completing this study.
Table 1.
Patient demographic data (n = 318)
| Variable | Value |
|---|---|
| Sex | |
| Female | 195 (61%) |
| Male | 123 (39%) |
| Age (years)* | 54 (18–96) |
| Mechanism | |
| Fall | 144 (45%) |
| Motor vehicle collision | 123 (39%) |
| Direct blow | 10 (3%) |
| Crush | 6 (2%) |
| Other | 35 (11%) |
| Closed versus open | |
| Closed | 314 (99%) |
| Open (Type IIIA) | 4 (1%) |
| Young and Burgess class | |
| LC1 | 276 (87%) |
| LC2 | 39 (12%) |
| LC3 | 3 (1%) |
* Values are expressed as median, with range in parentheses; the remaining values are expressed as number of patients, with percentage in parentheses.
A trauma fellowship-trained surgeon (MJW) evaluated all films. The AP radiograph was used to confirm the diagnosis of an LC-type injury. The plain films and CT scan were used to classify fractures according to the Young and Burgess system [13]. The kappa value for interobserver variability in diagnosing fracture patterns according to this system based on plain radiography has been reported as 0.72 [4]. CT was used to define the posterior injury. We defined posterior injuries as having no fracture, an incomplete anterior sacral fracture, a complete but simple sacral fracture, a complete, comminuted sacral fracture, or a crescent fracture (Fig. 1). We defined anterior injuries as having ipsilateral pubic rami fractures, contralateral pubic rami fractures, bilateral pubic rami fractures, or some other injury. A single surgeon (WB) measured the injury radiographs for displacement (Fig. 2). There is no clear consensus on the definition of displacement in LC pelvic fractures. We used criteria similar to those used by Bruce et al. [1]. Pubic rami fractures were considered displaced if the superior ramus fracture was displaced by 100% or more. On the AP and inlet views, the position of the femoral head was assessed with respect to the midline in comparison to the contralateral femoral head. A fracture was considered displaced if the femoral head was medially translated 10 mm or more with respect to the contralateral side. On the AP and outlet views, the difference in height between the iliac spines, the femoral heads, and the ischial tuberosities was measured using lines perpendicular to the midline. The mean height was calculated and the fracture was considered displaced vertically if there was a difference of 10 mm or more with respect to the contralateral side. The anterior pelvic ring was considered to be displaced if the rami were displaced 100% or if the femoral head was migrated medially or vertically 10 mm or more on the AP, inlet, or outlet view. CT scans were used to assess displacement of the posterior elements. Posterior injuries were considered displaced if either the sacral injury or the iliac crescent fracture was translated or gapped 5 mm or more.
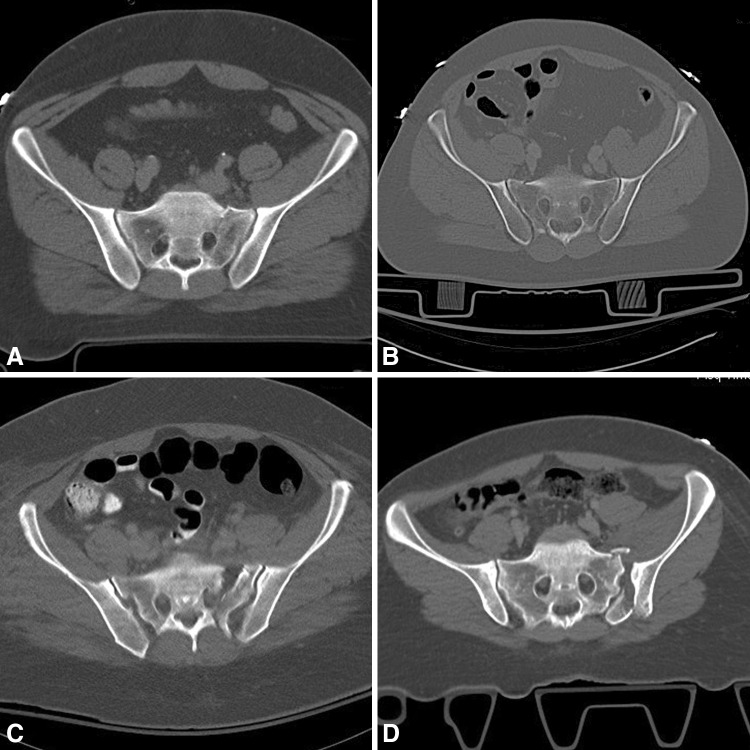
Fig. 1A–D.
CT scans show examples of posterior injury patterns: (A) an incomplete anterior sacral fracture, (B) a complete (simple) sacral fracture, (C) a complete (comminuted) sacral fracture, and (D) a crescent fracture.
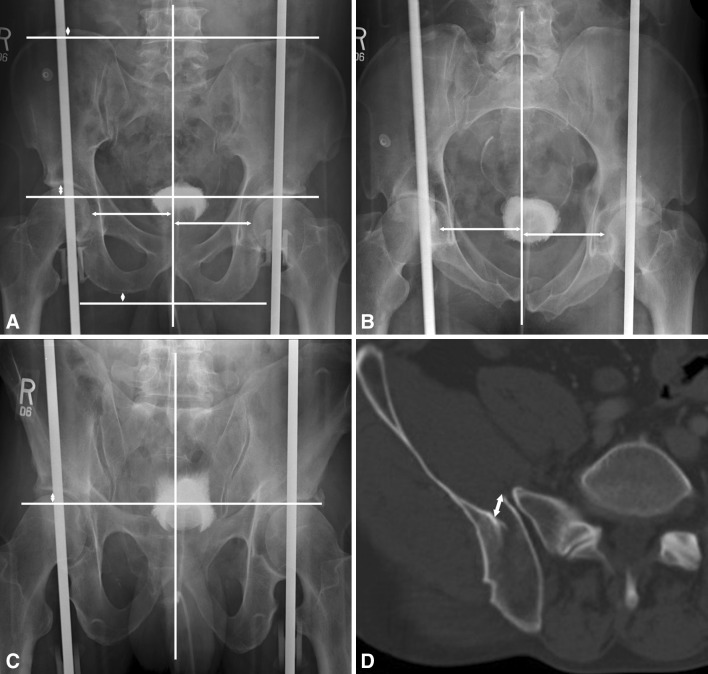
Fig. 2A–D.
Measurements of displacement (arrows) are demonstrated on different radiographic views. (A) On the AP view, the displacement of the superior ramus and the vertical and medical displacement of the femoral head are measured. (B) On the inlet radiograph, the medial displacement of the femoral head is measured. (C) On the outlet radiograph, the vertical displacement of the femoral head is measured. (D) Posterior displacement is measured by CT scan.
We gathered and stored data on Excel® (Microsoft Corp, Redmond, WA, USA). Analysis was performed with SPSS® (SPSS Inc, Chicago, IL, USA). To evaluate the correlation between posterior and anterior injury patterns, patients were grouped by posterior pattern. The proportion of patients with bilateral rami fractures was then compared between groups using the chi-square test. To assess patterns of displacement, we grouped patients into those who had posterior displacement and those who did not. The rate of anterior displacement between groups was compared with the chi-square test. To correlate specific fracture patterns with displacement, fractures were considered displaced if they had either anterior or posterior displacement or both. The rate of displacement was compared between patient groups for both anterior and posterior injuries.
Results
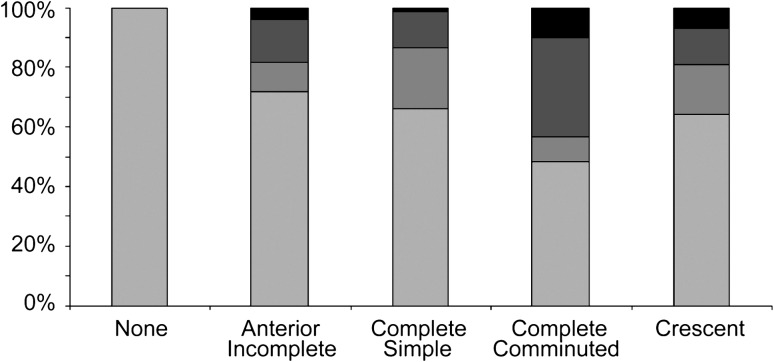
Fractures classified as Young-Burgess LC1 patterns were most common, representing 87% of fractures. The sacral injuries in this group ranged from nondisplaced incomplete anterior buckle fractures to highly comminuted and displaced complete fractures (Table 2). Similarly, there was a wide range of anterior injuries. While most anterior ring fractures occurred ipsilateral to the posterior injury (67%), others occurred on the contralateral side (12%) or were bilateral (16%). Patients with complete comminuted sacral injuries were more likely to have bilateral rami fractures compared to those patients with incomplete (p = 0.001) or simple (p = 0.008) fracture patterns (Fig. 3).
Table 2.
Fracture characteristics
| Characteristic | Number of patients |
|---|---|
| Anterior injuries | |
| Ipsilateral rami fractures | 214 (67%) |
| Contralateral rami fractures | 38 (12%) |
| Bilateral rami fractures | 50 (16%) |
| Other | 16 (5%) |
| Total | 318 (100%) |
| Posterior injuries | |
| None | 13 (4%) |
| Anterior incomplete sacral fractures | 162 (51%) |
| Complete (simple) sacral fractures | 53 (17%) |
| Complete (comminuted) sacral fractures | 48 (15%) |
| Crescent fractures | 42 (13%) |
| Total | 318 (100%) |
Fig. 3.
A graph shows the distribution of anterior pelvic ring injury based on posterior injury pattern. In cases of no posterior injury, the anterior injury was considered to be ipsilateral. There were no instances of bilateral rami fractures in the setting of no identified sacral fracture.
Fractures that demonstrated anterior displacement were three times more likely (p < 0.001) to have posterior displacement than injuries without anterior displacement (34% versus 11%). One hundred six patients (33%) had either anterior or posterior displacement of their pelvic fracture at presentation. Eighty (25%) had displacement of the anterior pelvic ring while 54 (17%) had displacement of the posterior injury (Table 3).
Table 3.
Fracture displacement
| Displacement type | Number of patients |
|---|---|
| Anterior displacement* (≥ 10 mm, n = 318) | 80 (25%) |
| AP (n = 318) | |
| Displaced rami (≥ 100%) | 47 (14%) |
| Medial femoral head displacement | 49 (15%) |
| Vertical femoral head displacement | 55 (17%) |
| Inlet (n = 65) | |
| Medial femoral head displacement | 9 (14%) |
| Outlet (n = 106) | |
| Vertical femoral head displacement | 29 (27%) |
| Posterior displacement† (≥ 5 mm, n = 318) | 53 (17%) |
| Overall displacement‡ (n = 318) | 106 (33%) |
* Based on plain radiography; †either sacral fracture or crescent fracture, based on CT; ‡having anterior displacement (≥ 10 mm) and/or posterior displacement (≥ 5 mm).
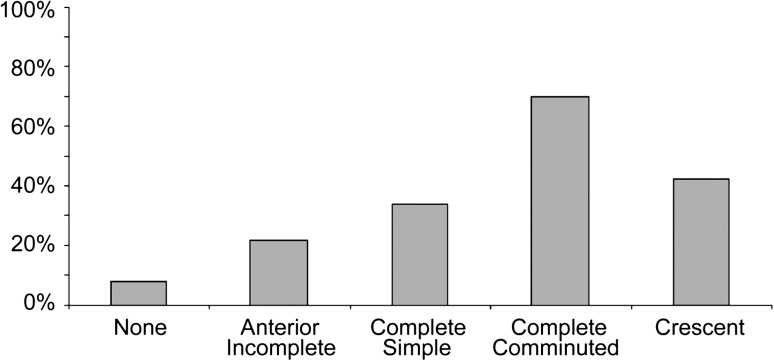
The degree of displacement correlated with the posterior injury (Fig. 4). Patients with complete comminuted sacral injuries were more likely to be displaced compared to those patients with incomplete (p < 0.001) or simple (p < 0.001) sacral fractures or crescent fractures (p = 0.01). Crescent fractures were associated with a higher rate of initial displacement when compared to incomplete anterior sacral fractures (p = 0.007) but not complete simple sacral fractures (p = 0.37). Further, displacement correlated with the anterior pelvic ring injury. Patients with bilateral rami fractures were more likely (p = 0.01) to be displaced, regardless of posterior injury, than patients with ipsilateral rami fractures (29% versus 48%).
Fig. 4.
A graph shows the percentage of fractures displaced at presentation grouped by posterior injury. Patients with complete comminuted sacral fracture were more likely (p < 0.001) to be displaced than all other sacral injury patterns.
Discussion
LC-type pelvic fractures encompass a wide spectrum of injuries. Current classification systems are poorly suited to help guide treatment. The Young and Burgess system is based on a combination of mechanism of injury and anatomic fracture characteristics [14]. All injuries that involve a sacral fracture are grouped together into the LC1 pattern. Clinically, this group of fractures is heterogeneous, with some injuries clearly representing stable injuries that will heal with no intervention and others that are displaced, unstable fractures that are typically treated with reduction and fixation [1, 12]. The AO classification is based primarily on stability [11] and is difficult to apply to this category of injuries. Our purposes were to (1) better define the spectrum of injuries that compose LC fractures with respect to both the anterior and posterior ring injuries, with particular focus of the morphology of sacral fractures, and (2) identify fracture patterns associated with displacement at presentation.
Our study is associated with certain limitations. First, it is a retrospective review describing the anatomic patterns of fractures and the incidence of displacement. Patients were not followed and we do not present information on treatment or eventual outcome. The strength of this study lies in describing the patterns of injury seen in a large cohort of patients with LC-type pelvic fractures and the incidence of initial displacement. Second, to our knowledge, there is no standardized definition of displacement. While the interobserver reliability of classifying fractures as LC is good [4], there are no published data on the interobserver reliability of detecting displacement of LC fracture. We used criteria similar to those of a recent study evaluating risk factors for late displacement of LC1 fractures [1]. These criteria (either vertical or horizontal displacement of the femoral head by 1 cm, 100% translation of a rami fracture or posterior displacement of 5 mm) seem to correlate with clinical experience and are easy to quantify.
The morphology of the fractures seen in our series is varied. The majority of injuries (87%) had a sacral fracture and fit within the category of LC1 injuries as defined by Young and Burgess [2, 13]. Anterior injury patterns included ipsilateral, contralateral, and bilateral rami fractures. Posterior ring injuries included anterior incomplete sacral fractures, complete simple sacral fractures, complete comminuted sacral fractures, and crescent fractures. This range of injuries is similar to previously published series and highlights the variation seen in LC injuries (Table 4).
Table 4.
Literature review
| Variable | Burgess et al. [2] | Lefaivre et al. [5] | Bruce et al. [1] | Current study |
|---|---|---|---|---|
| Patients | 106 | 100 | 117 | 318 |
| Age (years)* | 31 (14–87) | 38 (13–87) | 39 (17–90) | 54 (18–96) |
| Male | 55 (52%) | 46 (46%) | 123 (39%) | |
| Female | 51 (48%) | 54 (54%) | 195 (61%) | |
| Young and Burgess classification | ||||
| LC1 | 79 (75%) | 100 (100%) | 117 (100%) | 276 (87%) |
| LC2 | 12 (11%) | 39 (12%) | ||
| LC3 | 15 (14%) | 3 (1%) | ||
| Anterior injury | 97 (97%) | 112 (96%) | 318 (100%) | |
| Unilateral rami fracture | 68 (58%) | 252 (79%) | ||
| Ipsilateral | 214 (68%) | |||
| Contralateral | 38 (12%) | |||
| Bilateral | 44 (38%) | 50 (16%) | ||
| Other | 3 (3%) | 5 (4%) | 16 (5%) | |
| Posterior injury | 98 (98%) | 117 (100%) | 305 (96%) | |
| None | 2 (2%) | 0 (0%) | 13 (4%) | |
| Anterior incomplete sacral fracture | 51 (51%) | 78 (67%) | 162 (51%) | |
| Complete sacral fracture | 47 (47%) | 39 (33%) | 101 (31%) | |
| Simple | 13 (13%) | 53 (17%) | ||
| Comminuted | 34 (34%) | 48 (15%) | ||
| Crescent fracture | 42 (13%) | |||
| Displacement | ||||
| Anterior | 80 (25%) | |||
| Posterior | 53 (17%) | |||
| Overall | 106 (33%) |
* Values are expressed as median, with range in parentheses; the remaining values are expressed as number of patients, with percentage in parentheses.
Fifty patients (16%) in our series had bilateral rami fractures. This anterior ring pattern was more prevalent in patients with comminuted sacral fractures (33%) compared to those with an incomplete sacral fracture (3%) or a complete simple sacral fracture (11%). Bruce et al. [1] recently published a study that correlated bilateral pubic rami fractures and complete sacral fractures with late displacement in a series of nonoperatively managed minimally displaced LC fractures. In our series, bilateral rami fractures were associated with a higher incidence of initial displacement. Given bilateral rami fractures are linked to both initial displacement and displacement at healing, this particular fracture pattern is likely a marker of a higher-energy injury and instability.
In our cohort of 318 patients, 106 (33%) presented with either anterior or posterior displacement. Characteristics associated with initial displacement included the presence of bilateral pubic rami fractures, complete comminuted fractures of the sacrum, and crescent fractures. We suspect fracture patterns associated with a higher rate of initial displacement are higher-energy injuries and may be prone to late displacement even if they are only minimally displaced at presentation. Sagi et al. [7] recently reported on a series of patients with initially minimally displaced pelvic fractures who underwent EUA. Of 20 patients initially classified as LC1 injuries based on plain film and CT, seven were unstable when examined under fluoroscopy and had internal fixation. Specifics of the sacral fractures of these patients were not reported. As our understanding of LC injuries has evolved, it is now our practice to examine patients with bilateral rami fractures or complete sacral fractures under anesthesia for consideration of fixation or to follow them more closely to look for signs of late displacement.
Crescent fractures represent a group of fractures thought to be unstable [10, 12]. In our series, 43% of crescent fractures were displaced at presentation. Many of the nondisplaced injuries likely represent stable injuries that will not go on to secondary displacement. It is our practice to reduce and fix displaced crescent fractures. However, many nondisplaced fractures can be managed with either a EUA or close observation.
To be useful, a fracture classification needs to provide prognostic information to help guide treatment. The LC injuries as described by Young and Burgess are too broadly grouped to provide useful information for the treating surgeon. Further study is required to define fracture groups that better correlate with fracture stability and hence the need for surgical reduction and fixation or potentially examination under anesthesia. It appears many fracture characteristics are associated with instability, including bilateral rami fractures, complete comminuted sacral fractures, and crescent fractures. This initial evaluation of the spectrum of LC injuries will provide background for developing a system for predicting pelvic instability.
Acknowledgments
We thank our research coordinator Jordan Morgan and our research interns Philip Johnson and Katrina Hacker for gathering and organizing the radiographic data for our review.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Brigham and Women’s Hospital and Massachusetts General Hospital, affiliated with Harvard Medical School, in Boston, MA, USA.
References
- 1.Bruce B, Reilly M, Sims S. Predicting future displacement of non-operatively managed lateral compression sacral fractures: can it be done? J Orthop Trauma. 2011;25:523–527. doi: 10.1097/BOT.0b013e3181f8be33. [DOI] [PubMed] [Google Scholar]
- 2.Burgess AR, Eastridge BJ, Young JW, Ellison TS, Ellison PS, Jr, Poka A, Bathon GH, Brumback RJ. Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma. 1990;30:848–856. doi: 10.1097/00005373-199007000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988;227:67–81. [PubMed] [Google Scholar]
- 4.Koo H, Leveridge M, Thompson C, Zdero R, Bhandari M, Kreder H, Stephen D, McKee MD, Schemitsch EH. Interobserver reliability of the Young-Burgess and Tile classification systems for fractures of the pelvic ring. J Orthop Trauma. 2008;22:379–384. doi: 10.1097/BOT.0b013e31817440cf. [DOI] [PubMed] [Google Scholar]
- 5.Lefaivre KA, Padalecki JR, Starr AJ. What constitutes a Young and Burgess lateral compression-I (OTA 61-B2) pelvic ring disruption? A description of computed tomography-based fracture anatomy and associated injuries. J Orthop Trauma. 2009;23:16–21. doi: 10.1097/BOT.0b013e31818f8a81. [DOI] [PubMed] [Google Scholar]
- 6.Routt ML, Simonian PT, Ballmer F. A rational approach to pelvic trauma. Clin Orthop Relat Res. 1995;318:64–74. [PubMed] [Google Scholar]
- 7.Sagi HC, Coniglione FM, Stanford JH. Examination under anesthetic for occult pelvic ring instability. J Orthop Trauma. 2011;25:529–536. doi: 10.1097/BOT.0b013e31822b02ae. [DOI] [PubMed] [Google Scholar]
- 8.Tile M. Pelvic fractures: operative versus non-operative treatment. Orthop Clin North Am. 1980;11:423–464. [PubMed] [Google Scholar]
- 9.Tile M. Acute pelvic fractures. II. Principles of management. J Am Acad Orthop Surg. 1986;4:152–161. doi: 10.5435/00124635-199605000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surg Br. 1988;70:1–12. doi: 10.1302/0301-620X.70B1.3276697. [DOI] [PubMed] [Google Scholar]
- 11.Tile M. Acute pelvic fractures. I. Causation and classification. J Am Acad Orthop Surg. 1996;4:143–151. doi: 10.5435/00124635-199605000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Tile M, Helfet D, Kellam J. Fractures of the Pelvis and Acetabulum. Philadelphia, PA: Lippincott Williams & Wilkins; 2003. [Google Scholar]
- 13.Young JW, Burgess AR. Radiologic Management of Pelvic Ring Fractures: Systematic Radiographic Diagnosis. Baltimore, MD: Urban & Schwarzenberg; 1987. [Google Scholar]
- 14.Young JW, Burgess AR, Brumback RJ, Poka A. Pelvic fractures: value of plain radiography in early assessment and management. Radiology. 1986;160:445–451. doi: 10.1148/radiology.160.2.3726125. [DOI] [PubMed] [Google Scholar]