Abstract
Background
Plate fixation is a recognized treatment for pelvic ring injuries involving disruption of the pubic symphysis. Although fixation failure is well known, it is unclear whether early or late fixation failure is clinically important.
Questions/purposes
We therefore determined (1) the incidence and mode of failure of anterior plate fixation for traumatic pubic symphysis disruption; (2) whether failure of fixation was associated with the types of pelvic ring injury or pelvic fixation used; (3) the complications, including the requirement for reoperation or hardware removal; and (4) whether radiographic followup of greater than 1 year alters subsequent management.
Methods
We retrospectively reviewed 148 of 178 (83%) patients with traumatic symphysis pubis diastasis treated by plate fixation between 1994 and 2008. Routine radiographic review, pelvic fracture classification, method of fixation, incidence of fixation failure, timing and mode of failure, and the complications were recorded after a minimum followup of 12 months (mean, 45 months; range, 1–14 years).
Results
Hardware breakage occurred in 63 patients (43%), of which 61 were asymptomatic. Breakage was not related to type of plate, fracture classification, or posterior pelvic fixation. Five patients (3%) required revision surgery for failure of fixation or symptomatic instability of the symphysis pubis, and seven patients (5%) had removal of hardware for other reasons, including late deep infection in three (2%). Routine radiographic screening as part of annual followup after 1 year did not alter management.
Conclusions
Our observations suggest the high rate of late fixation failure after plate fixation of the symphysis pubis is not clinically important.
Introduction
Pelvic ring disruption often results from high-energy trauma. Initial management involves immediate resuscitation and the detection of associated injuries. Pelvic fractures may lead to life-threatening hemorrhage [2, 14] and, in the absence of another bleeding source, current management options include the use of a pelvic binder, emergency angiography and embolization, application of an external fixator, pelvic packing, early internal fixation, or a combination of these [1, 6, 21]. For definitive stabilization, a substantially displaced anterior fracture or symphysis pubis diastasis (when the symphysis is disrupted) has a better outcome if reduced anatomically [8, 12].
A variety of methods of achieving anterior ring reduction and fixation have been described in the literature; these include anterior external fixation, plate fixation, tension band wiring, and absorbable sutures [24, 25]. Whereas the use of an anterior external fixator can stabilize the pelvic ring [23], there is a high rate of complications. Pin site infection occurs in 13% to 50% [9, 11] and pin site placement may be inconsistent [22]. Aseptic loosening of the pins may also lead to loss of reduction and necessitate revision fixation [11]. Loss of reduction may also occur in the presence of a posterior ring injury, which is often not stabilized sufficiently by an anterior external fixator [8, 9, 19]. Biomechanical studies have demonstrated that symphyseal plating is effective in restoring anterior ring stability [4, 20] and efficacious outcomes have been confirmed in published case series (Fig. 1) [5, 12, 13, 15]. Plate fixation has a lower rate of complications [11, 17] and has become the preferred method of fixation. Several authors have described rates of hardware failure of 12% to 31%, loss of reduction of 7% to 24%, and revision rates of 3% to 9% [5, 7, 12, 15, 18, 26]. However, the timing and clinical consequences of implant failure are unclear.
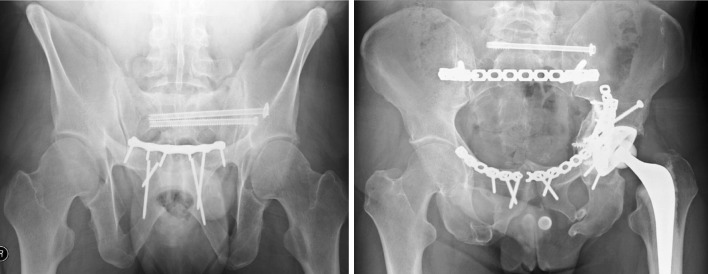
Fig. 1.
An example of an open-book pelvic ring injury treated with symphysis pubis plating.
The aims of this study were to determine: (1) the incidence and mode of failure of anterior plate fixation for traumatic pubic symphysis disruption; (2) whether failure of fixation was associated with the types of pelvic ring injury or pelvic fixation used; (3) the complications, including the requirement for reoperation or hardware removal; and (4) whether radiographic followup of greater than 1 year alters subsequent management.
Patients and Methods
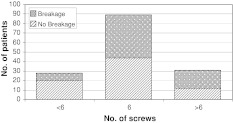
Between January 1994 and August 2008, we treated 178 patients with anterior pelvic ring injuries, involving pubic symphysis disruption, with anterior plate fixation. Our indication for anterior plate fixation was complete pubic symphysis disruption. This may be associated with concominant pubic rami fractures. The contraindication was active infection in the anterior pelvis. One patient died within 1 month of surgery from associated injuries, 18 patients were lost to followup, and 11 patients were followed up for less than 1 year. The remaining 148 patients (83%) were followed a minimum of 12 months (mean, 45 months; range, 12 months to 14 years; median, 36 months). There were 112 males and 36 females with a mean age of 39 years (range, 9–80 years). There were 99 AO/OTA Type B injuries and 49 Type C injuries treated using three different plating systems (Table 1). The majority of injuries were treated using a six-hole 3.5-mm plate (Fig. 2). Supplementary posterior ring fixation was performed in 96 patients (47 of 99 AO/OTA Type B and all 49 Type C). It was the department policy to stabilize posterior injuries, including Type B injuries, with displaced or comminuted sacral fractures and sacroiliac joint fracture subluxations. Initial reduction of the symphysis pubis was anatomical in 134 (91%) patients. The study was approved by the ethical committe for the hospital.
Table 1.
Types of pubic symphysis plates
| Plate type | Total number | Number broken |
|---|---|---|
| DCP | 2 | 0 |
| Recon plate | 62 | 11 |
| Matta plate | 84 | 11 |
| Dual plating | 3 | 0 |
Fig. 2.
The number of screws used for anterior fixation.
Patient details were extracted from the unit’s prospective database and a retrospective review of medical records and radiographic imaging was performed to determine clinical and radiographic outcomes. Fractures were classified according to AO/OTA [10] from the preoperative AP, inlet, and outlet radiographs.
All operations were performed through a midline vertical rectus-splitting anterior approach with the skin incision either being transverse or vertical when associated with an abdominal operation. Where there was an associated pelvic ring or acetabular fracture, alternative approaches were used, including the ilioinguinal, Stoppa, and combined approaches. In vertically unstable fractures and AP compression fractures with considerable posterior instability, posterior fixation was performed before anterior fixation (Fig. 3). Anterior fixation was achieved using a dynamic compression plate (DCP; Synthes, Welwyn Garden City, UK), 3.5-mm reconstruction plate (either Synthes or Stryker Trauma, Newbury, UK), or Matta pelvic symphyseal plate (Stryker Trauma) with the aim of reducing all symphysis pubis diastases anatomically. Typically, we used a single six-hole 3.5-mm reconstruction or the specialized pubic symphysis plate but actual fixation was dependent on injury pattern; fewer than six screws were occasionally used in patients with good bone quality (those without risk factors for osteoporosis). If the injury involved the pubic rami, then the plate length was extended.
Fig. 3.
An example of a pelvic ring injury with disruption of the symphysis pubis, both rami, and both sacroiliac joints stabilized using anterior and posterior fixation using a plate extended across the rami.
Patients were mobilized with toe-touch weightbearing on the side of the hemipelvic injury for 6 weeks. If both sides were involved, patients were restricted to bed-to-chair transfer and a wheelchair. At 6 weeks, mobilization was increased to 50% partial weightbearing and full weightbearing was started at 12 weeks. All mobilization was supervised by a physiotherapist, initially on a daily basis while an inpatient and then subsequently as an outpatient depending on availability of resources and other comorbidities.
Postoperative followup occurred at 6 weeks, 3 months, 6 months, 12 months, and then annually for 5 years in line with department policy at the time. Routine radiographic views taken at these appointments included AP pelvis, inlet, and outlet views. We reviewed the medical case notes to record complications, including deep infection, revision surgery, and hardware removal. Postoperative radiographs were used to assess symphysis pubis reduction and method of pelvic ring fixation, whereas radiographs taken at followup appointments were examined for loss of reduction (defined as displacement greater than 1 cm) and fixation failure.
Data analysis was undertaken using SPSS Version 17.0 (Chicago, IL, USA). We assessed differences in incidence rates of fixation failure between types of plate implanted using Pearson chi square test with Yates correction. We assessed differences in incidence rates of fixation failure between pelvic fracture types (AO/OTA B and C), the presence or absence of posterior fixation, and symphyseal reduction (less than 10 mm) with Fisher’s exact test. The relationship between the presence or absence of screw breakage within 12 months of fixation and further implant failure later was assessed using Pearson’s chi square test.
Results
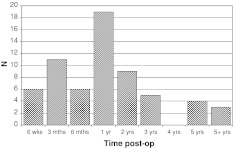
Anterior fixation failure resulting from hardware breakage occurred in 63 patients (43%) at a median of 12 months (Fig. 4). This involved plate breakage only in 14 patients, plate and screws in nine patients (Table 1), and the screws only in 40 patients. Sixty-one of 63 of these patients were asymptomatic. In two patients the screws pulled out of the bone causing a recurrent diastasis without hardware breakage.
Fig. 4.
The timing of initial hardware breakage.
The rate of anterior fixation failure was not related to the type of plate used (p = 0.8), the type of pelvic ring injury (p = 0.9), the presence or absence of posterior fixation (p = 1), and symphyseal reduction (less than or greater than 10 mm) (p = 0.1). If hardware breakage occurred within the first 12 months, there was an increased risk of further breakage in subsequent years (p = 0.009). Typically this was individual screw breakage rather than plate breakage and was asymptomatic.
Revision of the anterior fixation was performed in five patients (3%) (Table 2). All patients underwent uneventful revision of fixation with successful healing and persisting stabilization of the symphysis. Loss of initial postoperative reduction of the symphysis pubis occurred in six patients (4%). In four patients, diastasis occurred after hardware breakage within the first 6 months; two were related to plate breakage and two were related to screw breakage. The other two patients had recurrent diastasis as a result of the screws pulling out of the bone with no hardware breakage; one of these patients only had one screw on each side of the symphysis. Two of the six patients with loss of reduction required early revision of fixation of the symphyseal diastasis as a result of one case of screw breakage and one of screw pullout without breakage. In the remaining four patients, the degree of diastasis (less than 2.5 cm) was not considered clinically important, because the patients were asymptomatic, no progression of displacement occurred, and no revision surgery was performed. Seven patients had removal of the hardware (5%) (Table 3). Three patients developed a late deep infection, one patient at 1 year and two patients at 3 years. They recovered fully after removal of the hardware, wound management, and antibiotic therapy with no evidence of persisting infection or recurrent symphyseal diastasis. No patients presented with an early deep infection and none required revision fixation after deep infection and plate removal. The majority of the 38 females treated with symphyseal plating were of childbearing age (median, 36 years old). Only three of these patients had plates removed electively after discussion regarding future pregnancy and vaginal delivery.
Table 2.
Reason for revision procedure
| Reason for revision fixation (5 patients) | Time postoperatively |
|---|---|
| Plate with 2 screws displaced immediately postoperatively; revised to 6-hole plate | 3 days |
| Screw breakage with subsequent displacement | 6 months |
| Recurrent injury (horse-riding) | 12 months |
| Posterior nonunion and loose symphyseal plates (2 patients) | 12 + 18 months |
Table 3.
Reason for metalwork removal
| Reason for removal of metalwork (7 patients) | Time postoperatively |
|---|---|
| Screw backing out, single screw removed | 6 weeks |
| Female of childbearing age (3 patients) | 2, 3, 5 years |
| Retropubic abscess (2 patients) | 1 and 3 years |
| Deep iliac abscess (1 patient) | 3 years |
Findings on routine annual radiographic screening after 1 year did not alter patient management or outcome.
Discussion
Although anterior plating is the recommended treatment for pubic symphysis disruption, the incidence and consequences of fixation failure have remained a concern. Plating of the symphysis pubis is an effective method of treating displaced anterior pelvic ring injuries and, in the largest series we could identify, our results demonstrate efficacious radiographic results. The aims of this study were to determine the incidence and mode of failure of anterior plate fixation; whether failure of fixation is associated with the type of pelvic ring injury or pelvic fixation used; the complications, including the requirement for reoperation or hardware removal; and whether late fixation failure is clinically important or if longer-term radiographic followup of greater than 1 year is justified.
Our study is subject to a number of limitations. First, the minimum length of followup was 1 year, which may have meant we failed to detect a few additional cases of later fixation failure. Second, we had no measures of patient function. Our aim was to report on the radiographic success of the fixation technique and acknowledge this may not correlate with function. Third, this was a retrospective study in which the complications were recorded from the medical case notes and this may have led to minor complications being underreported although we suspect major complications would have been detected.
The striking finding from this series is the high rate of hardware breakage (Fig. 5). This is higher than previously reported in the literature, which ranged from 12% to 31% [5, 7, 12, 15, 18, 26]. However, it does not appear to often affect the clinical outcome because only three patients (2%) required revision after failure of fixation, two as a result of hardware breakage and one as a result of screw pullout. In two additional patients the anterior fixation failed late as a result of nonunion of the posterior pelvic injury. Other potential causes for the high rate of hardware breakage have been examined in this study. This was not related to the type of pelvic ring injury or to the use of posterior fixation, which may be the result of all potentially unstable posterior ring injuries having undergone fixation, thus achieving similar relative stability to the partially stable injuries that underwent only anterior fixation. Theoretically this is supported by cadaveric and clinical studies [7, 17, 23].
Fig. 5.
An example of hardware breakage of symphysis pubis screws (left) and plate (right) with no subsequent displacement.
The overall revision rate of 3% compares well with the reported literature (Table 4). A systematic review in 2005 found implant failure in 16 of 277 patients, an overall prevelance of 6% [16], and revision rates may be up to 16% in certain patient groups [12, 13, 18]. No revision of fixation was required after infection but three patients (2%) developed a late deep infection at 1 year, 3 years, and 3 years and underwent hardware removal. Interestingly, none of these three patients had experienced initial postoperative wound problems and all were closed injuries. Furthermore, the outcomes compare well with results achieved using definitive external fixation in which revision rates may be as high as 17% and pin site infection rates up to 50% [11, 22]. Lindahl et al. [9] found that loss of reduction can occur in up to 57% of patients with external fixators, including the majority of open-book and Type C fractures, and concluded that internal fixation of these fractures may produce better results.
Table 4.
Comparison of studies examining fixation of traumatic symphysis pubis diastasis
| Author | Study type | Patients | Mean followup (months) | Anterior fixation failure | Loss of reduction | Revision anterior fixation | Deep infection |
|---|---|---|---|---|---|---|---|
| Giannoudis et al. [5] | Case series | 74 | 42 | 9 (12%) | 5 (7%) | 0 | 1 (1%) |
| Lange and Hansen [7] | Case series | 19 | 24 | 4 (21%) | ND | ND | 1 (5%) |
| Matta [12] | Case series | 69 | 36 | ND | ND | 2 (3%) | 1 (1%) |
| Putnis et al. [15] | Case series | 49 | > 12 | 15 (31%) | 6 (12%) | 4 (8%) | 0 |
| Sagi and Papp [18] | Retrospective cohort | 92 | ND | 25 (27%) | 22 (24%) | 8 (9%) | ND |
| Webb et al. [26] | Case series | 14 | 20 | 0 | ND | 0 | 0 |
| Current study | Case series | 148 | 45 | 63 (43%) | 6 (4%) | 5 (3%) | 3 (2%) |
ND = no data available.
Our institution currently reviews all patients for 5 years with annual plain pelvic radiographs. The results from this study suggest that radiographic changes of implant failure at the symphysis pubis after 1 year do not affect future clinical outcome or management. It is proposed that, in the event of an uncomplicated postoperative recovery, it may be prudent to obtain plain radiographs up to 1 year postoperatively and, after this, either restrict routine imaging to an AP pelvic radiograph alone or only perform further radiologic imaging if the patient is symptomatic.
The role of symphysis pubis plate removal has been debated in the literature, although there remains a lack of evidence to guide clinicians [17]. There are arguments for routine removal in women of childbearing age [3] to facilitate pregnancy and vaginal delivery, but some authors suggest this may not be necessary [5]. Only three of the patients in this study had elective removal of their plate for this reason, but the incidence of pregnancy after symphysis pubis fixation in the remaining patients was not specifically examined.
Symphysis pubis plating can be performed in cases of traumatic pubic symphyseal disruptions, particularly in the presence of posterior ring instability requiring fixation [8, 12, 23]. The current study confirms the efficacious radiographic results for symphysis pubis plate fixation of pelvic ring injuries and the low rate of associated complications. Hardware breakage occurs frequently but only clinically affects a small number of patients in the early postoperative period. Routine radiographic screening for up to 5 years did not alter clinical management after 1 year. The role of hardware removal, particularly in young women, is still to be resolved.
Acknowledgments
We thank Alex Torrie and Richard Baker for all their help in collecting data for this study and Ruth Halliday for help with statistical analysis.
Footnotes
One of the authors (TJSC) has or may receive payments, in any one year, an amount in excess of $10,000 from Stryker Trauma GmbH (Schönkirchen, Germany). The institutution of one or more of the authors (TJSC, AJW, JL, SACM) received funding from Stryker UK Ltd (Newbury, UK).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his institution approved the human protocol for this investigation, which occurred at North Bristol NHS Trust, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Pelvic and Acetabular Reconstruction Unit, Frenchay Hospital, North Bristol NHS Trust, Bristol, UK.
References
- 1.Bassam D, Cephas GA, Ferguson KA, Beard LN, Young JS. A protocol for the initial management of unstable pelvic fractures. Am Surg. 1998;64:862–867. [PubMed] [Google Scholar]
- 2.Blackmore CC, Cummings P, Jurkovich GJ, Linnau KF, Hoffer EK, Rivara FP. Predicting major hemorrhage in patients with pelvic fracture. J Trauma. 2006;61:346–352. doi: 10.1097/01.ta.0000226151.88369.c9. [DOI] [PubMed] [Google Scholar]
- 3.Cannada LK, Barr J. Pelvic fractures in women of childbearing age. Clin Orthop Relat Res. 2010;468:1781–1789. doi: 10.1007/s11999-010-1289-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garcia JM, Doblare M, Seral B, Seral F, Palanca D, Gracia L. Three-dimensional finite element analysis of several internal and external pelvis fixations. J Biomech Eng. 2000;122:516–522. doi: 10.1115/1.1289995. [DOI] [PubMed] [Google Scholar]
- 5.Giannoudis PV, Chalidis BE, Roberts CS. Internal fixation of traumatic diastasis of pubic symphysis: is plate removal essential? Arch Orthop Trauma Surg. 2008;128:325–331. doi: 10.1007/s00402-007-0429-1. [DOI] [PubMed] [Google Scholar]
- 6.Giannoudis PV, Pape HC. Damage control orthopaedics in unstable pelvic injuries. Injury. 2004;35:671–677. doi: 10.1016/j.injury.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 7.Lange RH, Hansen ST., Jr Pelvic ring disruptions with symphysis pubis diastasis. Indications, technique, and limitations of anterior internal fixation. Clin Orthop Relat Res. 1985;201:130–137. [PubMed] [Google Scholar]
- 8.Lindahl J, Hirvensalo E. Outcome of operatively treated type-C injuries of the pelvic ring. Acta Orthop. 2005;76:667–678. doi: 10.1080/17453670510041754. [DOI] [PubMed] [Google Scholar]
- 9.Lindahl J, Hirvensalo E, Bostman O, Santavirta S. Failure of reduction with an external fixator in the management of injuries of the pelvic ring. Long-term evaluation of 110 patients. J Bone Joint Surg Br. 1999;81:955–962. doi: 10.1302/0301-620X.81B6.8571. [DOI] [PubMed] [Google Scholar]
- 10.Marsh L, Slongo TF, Agel J, Slongo TF, Agel J, Broderick SJ, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henlay B, Audige L. Fracture and dislocation classification compendium—2007: Orthoapedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21(Suppl):S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 11.Mason WT, Khan SN, James CL, Chesser TJ, Ward AJ. Complications of temporary and definitive external fixation of pelvic ring injuries. Injury. 2005;36:599–604. doi: 10.1016/j.injury.2004.11.016. [DOI] [PubMed] [Google Scholar]
- 12.Matta JM. Indications for anterior fixation of pelvic fractures. Clin Orthop Relat Res. 1996;329:88–96. doi: 10.1097/00003086-199608000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Oh CW, Kim PT, Kim JW, Min WK, Kyuung HS, Kim SY, Oh SH, Ihn JC. Anterior plating and percutaneous iliosacral screwing in an unstable pelvic ring injury. J Orthop Sci. 2008;13:107–115. doi: 10.1007/s00776-007-1201-7. [DOI] [PubMed] [Google Scholar]
- 14.O’Neill PA, Riina J, Sclafani S, Tornetta P., 3rd Angiographic findings in pelvic fractures. Clin Orthop Relat Res. 1996;329:60–67. doi: 10.1097/00003086-199608000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Putnis SE, Pearce R, Wali UJ, Bircher MD, Rickman MS. Open reduction and internal fixation of a traumatic diastasis of the pubic symphysis. J Bone Joint Surg Br. 2011;93:78–84. doi: 10.1302/0301-620X.93B1.23941. [DOI] [PubMed] [Google Scholar]
- 16.Raman R, Roberts CS, Pape HC, Giannoudis PV. Implant retention and removal after internal fixation of the symphysis pubis. Injury. 2005;36:827–831. doi: 10.1016/j.injury.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 17.Rommens PM, Vanderschot PM, Boodt P, Broos PL. Surgical management of pelvic ring disruptions. Indications, techniques and functional results. Unfallchirurg. 1992;95:455–462. [PubMed] [Google Scholar]
- 18.Sagi HC, Papp S. Comparative radiographic and clinical outcome of two-hole and multi-hole symphyseal plating. J Orthop Trauma. 2008;22:373–378. doi: 10.1097/BOT.0b013e31817e49ee. [DOI] [PubMed] [Google Scholar]
- 19.Simonian PT, Routt ML., Jr Harrington RM, Tencer AF. Anterior versus posterior provisional fixation in the unstable pelvis. A biomechanical comparison. Clin Orthop Relat Res. 1995;310:245–251. [PubMed] [Google Scholar]
- 20.Simonian PT, Schwappach JR, Routt ML, Jr, Agnew SG, Harrington RM, Tencer AF. Evaluation of new plate designs for symphysis pubis internal fixation. J Trauma. 1996;41:498–502. doi: 10.1097/00005373-199609000-00019. [DOI] [PubMed] [Google Scholar]
- 21.Tile M. Acute pelvic fractures: II. Principles of management. J Am Acad Orthop Surg. 1996;4:152–161. doi: 10.5435/00124635-199605000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Tucker MC, Nork SE, Simonian PT, Routt ML., Jr Simple anterior pelvic external fixation. J Trauma. 2000;49:989–994. doi: 10.1097/00005373-200012000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Bosch EW, Kleyn R, Hogervorst M, Vugt AB. Functional outcome of internal fixation for pelvis ring fractures. J Trauma. 1999;47:365–371. doi: 10.1097/00005373-199908000-00026. [DOI] [PubMed] [Google Scholar]
- 24.Varga E, Hearn T, Powell J, Tile M. Effects of method of internal fixation of symphyseal disruptions on stability of the pelvic ring. Injury. 1995;26:75–80. doi: 10.1016/0020-1383(95)92180-I. [DOI] [PubMed] [Google Scholar]
- 25.Waikakul S, Soparat K, Harnroongroj T. Anterior stabilization in the pubic symphysis separation: a mechanical testing. J Med Assoc Thai. 1999;82:72–79. [PubMed] [Google Scholar]
- 26.Webb LX, Gristina AG, Wilson JR, Rhyne AL, Meredith JH, Hansen ST., Jr Two-hole plate fixation for traumatic symphysis pubis diastasis. J Trauma. 1988;28:813–817. doi: 10.1097/00005373-198806000-00016. [DOI] [PubMed] [Google Scholar]