Abstract
Background
Most patients with displaced femoral neck fractures are treated by THA and hemiarthroplasty, but it remains uncertain which if either is associated with better function and lower risks of complications.
Questions/purposes
We performed a meta-analysis of randomized controlled trials (RCTs) to determine whether THA was associated with lower rates of reoperations, mortality, complications, and better function compared with hemiarthroplasty.
Methods
We searched the PubMed, Embase, Chinese Biomedicine Literature, and Cochrane Register of Controlled Trials databases and identified 12 RCTs (including a total of 1320 patients) for meta-analysis. Risk ratios (RRs) and weighted mean differences (WMDs) from each trial were pooled using random-effects or fixed-effects models depending on the heterogeneity of the included studies.
Results
THA was associated with a lower risk of subsequent reoperations compared with hemiarthroplasty (RR = 0.53; 95% CI, 0.34–0.84). There was no difference in mortality between patients undergoing THA and hemiarthroplasty (RR = 0.81; 95% CI, 0.60–1.09). For complications, there was a higher risk of dislocation in patients undergoing THA (RR = 1.99; 95% CI, 1.26–3.15), but there were no differences in local infections (RR = 1.60; 95% CI, 0.74–3.46) and general complications (RR = 1.15; 95% CI, 0.91–1.45). Patients with THA had higher Harris hip scores at 1 year (WMD = 3.81; 95% CI, 0.87–6.74) and at 3 or 4 years (WMD = 10.07; 95% CI, 6.92–13.21).
Conclusions
Despite more dislocations, THA can benefit patients with displaced femoral neck fractures with a lower reoperation rate and higher functional scores.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-012-2293-8) contains supplementary material, which is available to authorized users.
Introduction
Hip fracture is an international public health problem, and there are approximately 1.5 million hip fractures worldwide per year [40]. In 2050, there will be an estimated 3.9 million fractures worldwide, with more than 700,000 in the United States [40]. Hip fractures in older patients are associated with impaired mobility, excess morbidity and mortality, and obvious loss of independence [6, 14]. Thus, hip fractures remain a public health concern, especially with the aging population and with the high incidence of osteoporosis [14, 40].
A displaced femoral neck fracture is one of the most common hip fractures and these unstable fractures of the femoral neck generally need surgical intervention [4]. The goals of surgical treatment are immediate pain relief, rapid mobilization, accelerated rehabilitation, and a low risk of surgical complications or subsequent revision [26, 32]. Established surgical options for displaced femoral neck fracture mainly include internal fixation, hemiarthroplasty, and THA [4]. For decades, the optimal treatment choice has been debated, and whether THA is better than hemiarthroplasty for displaced femoral neck fractures is still uncertain [29, 30, 37, 38]. Many RCTs have evaluated the benefits of THA compared with hemiarthroplasty, but there is obvious inconsistency of effects across those studies [2, 3, 5, 11, 16, 22, 23, 27, 28, 34, 36, 39]. Meta-analysis has been recognized as an important tool to more precisely define the effect of clinical interventions and two systematic reviews have been published to compare the benefits of THA compared with hemiarthroplasty [15, 20]. A recent meta-analysis suggested THA was associated with lower reoperation rates compared with hemiarthroplasty for displaced femoral neck fractures [20]. However, this meta-analysis covered only seven eligible RCTs with a total of 769 patients. Furthermore, five new RCTs have been published since 2008 [9, 24, 25, 33, 41]. Therefore, to provide the most comprehensive assessment of THA and hemiarthroplasty for displaced femoral neck fractures, we performed an updated meta-analysis of all available RCTs.
We determined whether THA was associated with lower rates of reoperations, mortality, and complications and better function compared with hemiarthroplasty.
Search Strategy and Criteria
We searched the PubMed, Embase, Chinese Biomedicine Literature, and Cochrane Register of Controlled Trials databases for studies published between January 1980 and June 2011 with the search terms: (“total hip arthroplasty” or “total hip replacement” or “THA”) and (“hemiarthroplasty” or “unipolar” or “bipolar” or “femoral head replacement”). No language restriction was applied. The reference lists of identified studies and key review articles also were searched. The inclusion criteria for this meta-analysis were RCTs comparing THA with hemiarthroplasty for displaced femoral neck fractures and reporting at least one of the following main clinical outcomes: reoperations for any cause, 1-year mortality, hip function (Harris hip score), local infections, general perioperative complications, and dislocations. We excluded case series investigating either THA or hemiarthroplasty for treating displaced femoral neck fractures.
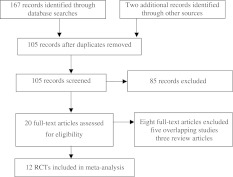
We identified 167 articles through database searching plus two additional articles through other sources (Fig. 1). There were 105 articles after removing duplicates. We excluded 85 of these articles, leaving 20 potentially relevant studies [2, 3, 5, 9, 11, 15, 16, 21–25, 27–29, 33, 34, 36, 39, 41]. We then excluded eight more articles (three review articles [15, 21, 29] and five duplicate articles [3, 5, 23, 27, 39]), leaving 12 RCTs meeting our selection criteria and involving a total of 1320 patients (624 in the THA group and 696 in the hemiarthroplasty group) [2, 9, 11, 16, 22, 24, 25, 27, 28, 32, 36, 41] (Table 1).
Fig. 1.
A flowchart shows the selection of studies for inclusion in the meta-analysis.
Table 1.
Key characteristics and quality of studies included in the meta-analysis.
| Study | Indication | Followup (months) | THA | Hemiarthroplasty | Main outcomes |
|---|---|---|---|---|---|
| Dorr et al. [11] 1986 | Displaced femoral neck fractures Garden III/IV | 24 | 39 cemented THAs | 51 cemented or uncemented hemiarthroplasties | Reoperations, mortality, dislocations, local infections, mortality |
| Ravikumar and Marsh [36] 2000 | Displaced femoral neck fractures Garden III/IV | 156 | 91 cemented THAs | 81 unipolar and uncemented hemiarthroplasties | Reoperations, mortality, dislocations, local infections |
| Keating et al. [22] 2005 | Displaced femoral neck fractures | 24 | 69 cemented THAs | 111 bipolar and cemented hemiarthroplasties | Reoperations, mortality, dislocations, local infections, general complications |
| Avery et al. [2] 2011 | Displaced femoral neck fractures | 108 | 40 cemented THAs | 41 cemented and bipolar hemiarthroplasties | Reoperations, mortality, dislocations, local infections, general complications |
| Hedbeck et al. [16] 2011 | Displaced femoral neck fractures | 48 | 60 cemented THAs | 60 bipolar and cemented hemiarthroplasties | Reoperations, mortality, dislocations, local infections, general complications, function (Harris hip score) |
| Macaulay et al. [28] 2008 | Displaced femoral neck fractures Garden III/IV | 24 | 17 cemented or uncemented THAs | 23 hemiarthroplasties | Reoperations, mortality, dislocations, local infections, general complications, function (Harris hip score) |
| Mouzopoulos et al. [33] 2008 | Displaced femoral neck fractures Garden III/IV | 48 | 43 cemented THAs | 43 bipolar hemiarthroplasties | Reoperations, mortality, function (Harris hip score) |
| Deng et al. [9] 2009 | Displaced femoral neck fractures Garden III/IV | 36 | 28 cemented or uncemented THAs | 28 cemented or uncemented hemiarthroplasties | Reoperations, dislocations, local infections, general complications, function (Harris hip score) |
| van den Bekerom et al. [41] (2010) | Displaced femoral neck fractures | 60 | 115 cemented THAs | 137 cemented hemiarthroplasties | Reoperations, mortality, dislocations, general complications |
| Lai [24] (2010) | Displaced femoral neck fractures Garden III/IV | 34 | 20 uncemented THAs | 22 uncemented hemiarthroplasties | Reoperations, dislocations, local infections, general complications |
| Li et al. [25] (2011) | Displaced femoral neck fractures | 60 | 55 cemented or uncemented THAs | 52 hemiarthroplasties | Dislocations, general complications, function (Harris hip score) |
| Pang [34] (2011) | Displaced femoral neck fractures | 40 | 47 cemented or uncemented THAs | 47 bipolar and cemented hemiarthroplasties | Dislocations, general complications, function (Harris hip score) |
Two of us (LY, JC) assessed the quality of the included RCTs using the scoring system of Jadad et al. [21], which evaluated studies based on randomization, blinding, and a description of withdrawals and dropouts (Table 1). Interobserver variability of assessing quality or inconsistencies were settled by consensus among all three authors. Among these studies, nine RCTs were high-quality studies (scoring 3 points or more), whereas the other three studies were low-quality studies (scoring 1 or 2 points). The Cochrane Risk of Bias Tool was used to assess the risk of bias in the included studies [17]. (Supplemental Table 1; supplemental materials are available with the online version of CORR).
From the full manuscripts, we extracted the following information from each study: year of publication, study design, number of patients, fracture classification, mean patient age, sex distribution, mean length of followup, type of prosthesis, and use of bone cement. To assess efficacy of treatment, we recorded reoperations for any cause, 1-year mortality, and hip function (Harris hip score). To assess complications associated with treatment, we recorded local infections, general perioperative complications (including pneumonia, urinary tract infections, thromboembolic events, and cardiovascular events), and dislocations. Inconsistencies in the extracted data were settled by consensus among all authors.
RRs and WMDs from each trial were pooled using random-effects or fixed-effects models depending on the heterogeneity of the included studies. As RRs were estimated to assess the advantage conferred by THA, an RR less than 1 was taken to indicate THA was superior to hemiarthroplasty. We used random-effects and fixed-effects models to analyze dichotomous data. The random-effects model was conducted using the method of DerSimonian and Laird [10], and the fixed-effects model was conducted using the method of Mantel and Haenszel [31]. To assess the between-study heterogeneity more precisely, we performed heterogeneity testing by calculating the chi-square-based Q statistic test for heterogeneity and the I2 statistic to quantify the proportion of the total variation attributable to heterogeneity [8, 18]. Heterogeneity was considered significant when the PQ statistic was less than 0.10, and the random-effects model was used to pool the relative data; otherwise, the fixed-effects model was used to pool the relative data. To validate the credibility of pooled results in this meta-analysis, we performed sensitivity analysis by sequential omission of individual studies. To better investigate possible sources of heterogeneity that might influence the results, meta-regression analysis also was used in this meta-analysis. Ten studies provided data for reoperations [2, 9, 11, 16, 22, 24, 28, 33, 36, 41]. There was no heterogeneity between trials (I2 = 17%; p = 0.29); therefore, the fixed-effects model was used to pool the relative data (Table 2). Nine studies provided data for mortality [2, 11, 16, 22, 25, 28, 33, 36, 41]. We observed no heterogeneity between trials (I2 = 0%; p = 0.94) and therefore used the fixed-effects model to pool the relative data (Table 2). There were six individual studies (including five studies at 1 year [9, 16, 25, 28, 33] and five studies at 3 or 4 years [9, 16, 25, 33, 34]) providing data for hip function as assessed by the Harris hip score. We found heterogeneity between trials (both p < 0.01), and the random-effects model was used to pool the relative data (Table 2). Eight studies provided data for local infections [2, 9, 11, 16, 22, 24, 28, 36]. There was no heterogeneity between these trials (I2 = 0%; p = 0.79); therefore, the fixed-effects model was used to pool the relative data (Table 2). Nine studies provided data for general complications [2, 9, 16, 22, 24, 25, 28, 34, 41]. We found no heterogeneity between trials (I2 = 24%; p = 0.23) and therefore used the fixed-effects model to pool the relative data (Table 2). Eleven studies provided data for dislocation [2, 9, 11, 16, 22, 24, 25, 28, 34, 36, 41]. Again, there was no heterogeneity between trials (I2 = 5%; p = 0.39), therefore we used the fixed-effects model to pool the relative data (Table 2).
Table 2.
Summary of RRs and WMDs with 95% CIs in the meta-analysis.
| Analysis item | Number of studies included | RR/WMD (95% CI) | p value | Heterogeneity | Model | |
|---|---|---|---|---|---|---|
| I2 (%) | p value | |||||
| Efficacy | ||||||
| Reoperation rates | 10 | 0.53 (0.34, 0.84) | 0.006 | 17 | 0.29 | Fixed-effects |
| Mortality | 9 | 0.81 (0.60, 1.09) | 0.17 | 0 | 0.94 | Fixed-effects |
| Harris hip scores at 1 year | 5 | 3.81 (0.87, 6.74) | 0.03 | 73 | 0.005 | Random-effects |
| Harris hip scores at 3 or 4 years | 5 | 10.07 (6.92, 13.21) | < 0.001 | 85 | < 0.001 | Random-effects |
| Complications | ||||||
| Dislocations | 11 | 1.99 (1.26, 3.15) | 0.003 | 5 | 0.39 | Fixed-effects |
| Local infections | 8 | 1.60 (0.74, 3.46) | 0.23 | 0 | 0.79 | Fixed-effects |
| General complications | 9 | 1.15 (0.91, 1.45) | 0.25 | 0.23 | 0.23 | Fixed-effects |
RR = risk ratio; WMD = weighted mean difference.
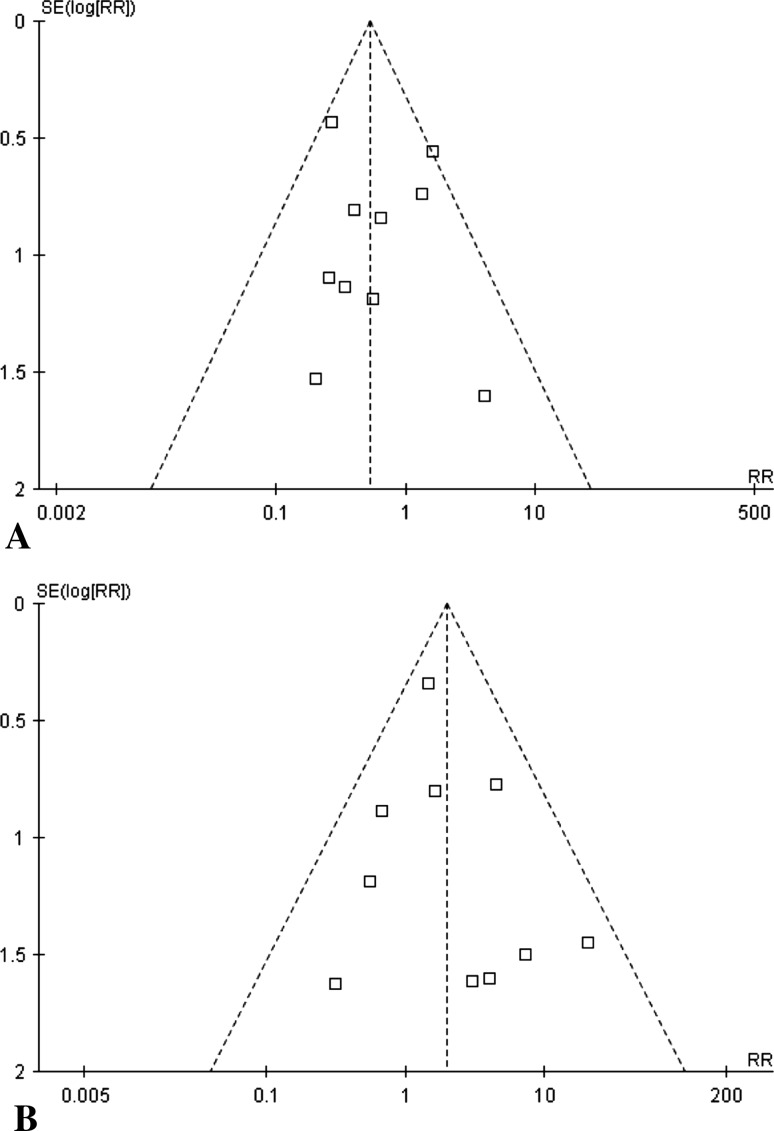
We performed funnel plots, in which the standard error of log [RR] of each study was plotted against its log [RR], and Egger’s linear regression test [12] to assess the publication bias. We first visually evaluated the symmetry of the funnel plots and did not find obvious evidence of asymmetry. In addition, all the p values of the Egger’s tests were greater than 0.05, providing no statistical evidence of asymmetry of the funnel plots (Fig. 2). These results suggested publication bias was not evident in this meta-analysis.
Fig. 2A–B.
The funnel plots assess publication bias of the meta-analysis comparing THA with hemiarthroplasty for displaced intracapsular hip fractures for (A) reoperations (TEgger’s test = −0.62; 95% CI, −1.41 to 2.45; PEgger’s test = 0.55 > 0.05) and (B) mortality (TEgger’s test = −0.60; 95% CI, −1.12 to 0.67; PEgger’s test = 0.57 > 0.05). SE = standard error.
Statistical analyses were performed using Review Manager (Version 5.0.2) (Cochrane Information Management System, http://ims.cochrane.org/revman) and STATA® (Version 12.0) (StataCorp LP, College Station, TX, USA) software programs. All p values were two-sided.
Results
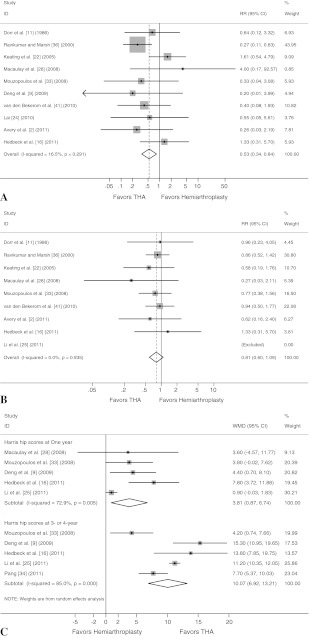
THA was associated with a lower risk (4.6%) of subsequent reoperations compared with hemiarthroplasty (8.6%) (RR = 0.53; 95% CI, 0.34–0.84; p = 0.006) (Fig. 3A). Sensitivity analysis by sequential omission of individual studies showed no change in significance.
Fig. 3A–C.
Meta-analysis results are shown for the comparison of THA with hemiarthroplasty for displaced intracapsular hip fractures regarding efficacy. The forest plot shows pooled RRs with 95% CIs suggesting (A) THA is associated with lower rate of reoperations (analysis of 10 studies; fixed-effects model) and (B) THA is not associated with lower rate of mortality (analysis of nine studies; fixed-effects model). (C) A forest plot shows pooled WMDs with 95% CIs suggesting THA is associated with better hip function (analysis of six individual studies; random-effects model). RR = risk ratio; WMD = weighted mean difference.
We found no difference (RR = 0.81; 95% CI, 0.60–1.09; p = 0.17) in mortality between patients undergoing THA (11.6%) and hemiarthroplasty (13.9%) (Fig. 3B). Sensitivity analysis showed the significance changed by omission of one study [41], which indicated the credibility of these pooled results was unstable and needs additional study.
The mean Harris hip scores at 1 year were higher after THA (WMD = 3.81; 95% CI, 0.87–6.74; p = 0.03), as were the mean Harris hip scores at 3 or 4 years (WMD = 10.07; 95% CI, 6.92–13.21; p < 0.001) (Fig. 3C). Sensitivity analysis by sequential omission of individual studies showed no change in significance. For the meta-analysis of hip function, we found heterogeneity between the trials; univariate analysis of meta-regression suggested the status of cemented or uncemented and surgery indications were important sources of between-study heterogeneity
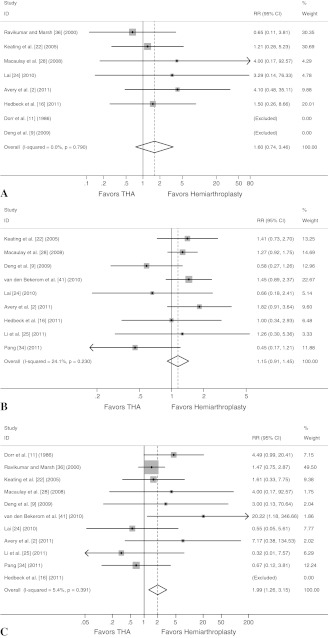
We found no difference (RR = 1.60; 95% CI, 0.74–3.36; p = 0.23) in postoperative infections between patients undergoing THA (3.8%) and hemiarthroplasty (2.4%) (Fig. 4A). Sensitivity analysis by sequential omission of individual studies showed no change in significance. As with infections, we observed no difference (RR = 1.15; 95% CI, 0.91–1.45; p = 0.25) in general complications between patients undergoing THA (21.7%) and hemiarthroplasty (19.4%) (Fig. 4B). Sensitivity analysis by sequential omission of individual studies showed no change in significance. We found a higher risk of dislocation in patients undergoing THA (7.6%) (RR = 1.99; 95% CI, 1.26–3.15; p = 0.003) (Fig. 4C) compared with hemiarthroplasty (3.5%). Sensitivity analysis by sequential omission of individual studies showed no change in significance.
Fig. 4A–C.
Meta-analysis results are shown for the comparison of THA with hemiarthroplasty for displaced intracapsular hip fractures regarding complications. The forest plots show pooled RRs with 95% CIs suggesting (A) THA is not associated with lower rate of local infections (analysis of eight studies; fixed-effects model), (B) THA is not associated with lower rate of general complications (analysis of nine studies; fixed-effects model), and (C) THA is associated with higher rate of dislocations (analysis of 11 studies; random-effects model). RR = risk ratio.
Discussion
Established surgical options for displaced femoral neck fractures mainly include internal fixation, hemiarthroplasty, and THA, but the optimal treatment choice continues to be debated and it is still uncertain whether THA is better than hemiarthroplasty for displaced femoral neck fractures [29, 30, 37, 38]. The latest meta-analysis showed THA might lead to a lower reoperation rate and better function compared with hemiarthroplasty for displaced femoral neck fractures [20]. However, the data available in that meta-analysis did not allow for definitive conclusions regarding the identified treatment effects, owing to varying interactions between subgroups and concerns regarding the random allocation of patients [20]. In addition, that meta-analysis covered only seven eligible RCTs with a total of 769 patients. Furthermore, five new RCTs have been published since 2008 [9, 24, 25, 33, 41]. Therefore, to provide the most comprehensive assessment of THA and hemiarthroplasty for displaced femoral neck fractures, we performed an updated meta-analysis to determine whether THA was associated with lower rates of reoperations, mortality, and complications and better function compared with hemiarthroplasty.
Some possible limitations to this meta-analysis should be acknowledged. First, the eligibility criteria for inclusion of patients with displaced femoral neck fractures differed for each study, which might influence the obvious consistency of effects across the included studies and cause between-study heterogeneity. Although the heterogeneity analyses did not find obvious between-study heterogeneity in this meta-analysis, the various eligibility criteria should be noted. In addition, to ensure uniformity in defining patient characteristics for displaced femoral neck fractures and clinical efficacy measures, a meta-analysis of individual patient data is needed [7]. Second, the clinical outcomes of cemented and uncemented hemiarthroplasties or THA differed [1, 19], and a previous Cochrane review suggested there was good evidence that cementing the prostheses in place would reduce postoperative pain and lead to better mobility [35], however, we did not perform subgroup analyses according to cemented or uncemented status owing to the limited studies reported in the original papers. Therefore, additional studies could compare THA and hemiarthroplasty according to cemented or uncemented status independently. Third, a hemiarthroplasty might use unipolar or bipolar head components [13], and there also is need for an additional meta-analysis comparing unipolar or bipolar hemiarthroplasty with THA for patients with displaced femoral neck fractures independently. Fourth, owing to the lack of relative information, the risk of biases could not be well assessed and the outcomes from this study might be affected by risk of biases from those included studies (Supplemental Table 1; supplemental materials are available with the online version of CORR). Finally, RCTs using longer-term outcome assessments and more patient outcomes are needed to confirm the outcomes from this meta-analysis.
We included 12 RCTs (with a total of 1320 patients) in this meta-analysis. The meta-analysis showed THA was associated with a lower risk of subsequent reoperations compared with hemiarthroplasty and better ratings in the Harris hip scores, but there was no difference in mortality between patients undergoing THA and hemiarthroplasty. However, there was a tendency for a lower risk of mortality at 1 year in patients undergoing THA, and the sensitivity analysis showed the significance was changed by omission of one study [41], which indicated the credibility of this outcome was unstable and requires further studies with larger sample sizes.
Regarding complications, there was a higher risk of dislocation in patients undergoing THA, but there were no differences in local infections and general complications, confirming the findings reported by Hopley et al. [20]. This higher risk for dislocation should be well recognized and noted in clinical applications.
Although hemiarthroplasty is a quick and highly standardized procedure that allows for early weightbearing and recovery [30, 32, 38], we found it was associated with a higher risk of subsequent reoperations and lower mean Harris hip scores compared with THA. In addition, we found a tendency for a higher risk of mortality at 1 year in patients undergoing hemiarthroplasty. Therefore, hemiarthroplasty is inferior to THA for treatment of patients with displaced femoral neck fractures, and THA may have a larger role in the treatment of displaced femoral neck fractures than it has in the past.
In interpreting our results, the clinical and statistical significance of the findings should be considered. In this meta-analysis, THA can reduce the incidence of subsequent reoperations by 4.0% (4.6% with THA versus 8.6% for hemiarthroplasty), which is a relative risk reduction of approximately 50% (RR = 0.53; p = 0.006) and obviously suggests clinical and statistical significance. However, as THA seems to yield a higher risk of dislocation (7.6 % with THA versus 3.5% for hemiarthroplasty), the advantages of lower reoperation rate and higher Harris hip scores for THA must be traded off against the higher risk of dislocation, and THA may be more suitable for patients with more possibility of dislocation risk. Therefore, after weighing the advantages and disadvantages of THA in displaced femoral neck fractures compared with hemiarthroplasty, we recommend THA for displaced femoral neck fractures in patients with less possibility of dislocation risk.
Despite more dislocations, THA can benefit patients with displaced femoral neck fractures with a lower reoperation rate and higher functional scores.
Electronic supplementary material
Acknowledgments
We thank Zhang Guoqiang MD, Department of Orthopedics, Chinese General Hospital of People’s Liberation Army, for valuable statistic advice concerning this study.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
References
- 1.Ahn J, Man LX, Park S, Sodl JF, Esterhai JL. Systematic review of cemented and uncemented hemiarthroplasty outcomes for femoral neck fractures. Clin Orthop Relat Res. 2008;466:2513–2518. doi: 10.1007/s11999-008-0368-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Avery PP, Baker RP, Walton MJ, Rooker JC, Squires B, Gargan MF, Bannister GC. Total hip replacement and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck: a seven- to ten-year follow-up report of a prospective randomised controlled trial. J Bone Joint Surg Br. 2011;93:1045–1048. doi: 10.1302/0301-620X.93B8.27132. [DOI] [PubMed] [Google Scholar]
- 3.Baker RP, Squires B, Gargan MF, Bannister GC. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck: a randomized, controlled trial. J Bone Joint Surg Am. 2006;88:2583–2589. doi: 10.2106/JBJS.E.01373. [DOI] [PubMed] [Google Scholar]
- 4.Bernstein J, Ahn J. In brief: fractures in brief: femoral neck fractures. Clin Orthop Relat Res. 2010;468:1713–1715. doi: 10.1007/s11999-010-1295-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blomfeldt R, Törnkvist H, Eriksson K, Söderqvist A, Ponzer S, Tidermark J. A randomised controlled trial comparing bipolar hemiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in elderly patients. J Bone Joint Surg Br. 2007;89:160–165. doi: 10.1302/0301-620X.89B2.18576. [DOI] [PubMed] [Google Scholar]
- 6.Butler M, Forte M, Kane RL, Joglekar S, Duval SJ, Swiontkowski M, Wilt T. Treatment of common hip fractures. Evid Rep Technol Assess (Full Rep). 2009;184:1–85, v. [PMC free article] [PubMed]
- 7.Cipriani A, Barbui C. What is an individual patient data meta-analysis? Epidemiol Psichiatr Soc. 2007;16:203–204. [PubMed] [Google Scholar]
- 8.Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10:101–129. doi: 10.2307/3001666. [DOI] [Google Scholar]
- 9.Deng R, Zhu J, Hong L, Cui H, Huang Z. [Total hip replacement and femoral head replacement in the treatment of femoral neck fractures in elderly patients] [in Chinese] Chinese Journal of Postgraduates of Medicine. 2009;32(suppl):81–83. [Google Scholar]
- 10.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 11.Dorr LD, Glousman R, Hoy AL, Vanis R, Chandler R. Treatment of femoral neck fractures with total hip replacement versus cemented and noncemented hemiarthroplasty. J Arthroplasty. 1986;1:21–28. doi: 10.1016/S0883-5403(86)80006-7. [DOI] [PubMed] [Google Scholar]
- 12.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Enocson A, Hedbeck CJ, Törnkvist H, Tidermark J, Lapidus LJ. Unipolar versus bipolar Exeter hip hemiarthroplasty: a prospective cohort study on 830 consecutive hips in patients with femoral neck fractures. Int Orthop. 2011 July 26. [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 14.Giannoudis PV, Kontakis G, Christoforakis Z, Akula M, Tosounidis T, Koutras C. Management, complications and clinical results of femoral head fractures. Injury. 2009;40:1245–1251. doi: 10.1016/j.injury.2009.10.024. [DOI] [PubMed] [Google Scholar]
- 15.Goh SK, Samuel M, Su DH, Chan ES, Yeo SJ. Meta-analysis comparing total hip arthroplasty with hemiarthroplasty in the treatment of displaced neck of femur fracture. J Arthroplasty. 2009;24:400–406. doi: 10.1016/j.arth.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 16.Hedbeck CJ, Enocson A, Lapidus G, Blomfeldt R, Törnkvist H, Ponzer S, Tidermark J. Comparison of bipolar hemiarthroplasty with total hip arthroplasty for displaced femoral neck fractures: a concise four-year follow-up of a randomized trial. J Bone Joint Surg Am. 2011;93:445–450. doi: 10.2106/JBJS.J.00474. [DOI] [PubMed] [Google Scholar]
- 17.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA. Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holt G, Hook S, Hubble M. Revision total hip arthroplasty: the femoral side using cemented implants. Int Orthop. 2011;35:267–273. doi: 10.1007/s00264-010-1167-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hopley C, Stengel D, Ekkernkamp A, Wich M. Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: systematic review. BMJ. 2010;340:c2332. doi: 10.1136/bmj.c2332. [DOI] [PubMed] [Google Scholar]
- 21.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 22.Keating JF, Grant A, Masson M, Scott NW, Forbes JF. Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty. Health Technol Assess. 2005;9:iii–iv, ix–x, 1–65. [DOI] [PubMed]
- 23.Keating JF, Grant A, Masson M, Scott NW, Forbes JF. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty: treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg Am. 2006;88:249–260. doi: 10.2106/JBJS.E.00215. [DOI] [PubMed] [Google Scholar]
- 24.Lai M. [Hemiarthroplasty and total hip arthroplasty in the treatment of femoral neck fractures in elderly patients] [in Chinese] Chinese Journal of New Clinical Medicine. 2010;3:41–44. [Google Scholar]
- 25.Li L, Nie Z, Niu J. [Total hip arthroplasty and hemiarthroplasty for treatment of femoral neck fractures in elderly patients] [in Chinese] China Foreign Medical Treatment. 2011;19:52–55. [Google Scholar]
- 26.Lowe JA, Crist BD, Bhandari M, Ferguson TA. Optimal treatment of femoral neck fractures according to patient’s physiologic age: an evidence-based review. Orthop Clin North Am. 2010;41:157–166. doi: 10.1016/j.ocl.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 27.Macaulay W, Nellans KW, Garvin KL, Iorio R, Healy WL, Rosenwasser MP. other members of the DFACTO Consortium. Prospective randomized clinical trial comparing hemiarthroplasty to total hip arthroplasty in the treatment of displaced femoral neck fractures: winner of the Dorr Award. J Arthroplasty. 2008;23(6 suppl 1):2–8. doi: 10.1016/j.arth.2008.05.013. [DOI] [PubMed] [Google Scholar]
- 28.Macaulay W, Nellans KW, Iorio R, Garvin KL, Healy WL, Rosenwasser MP. DFACTO Consortium. Total hip arthroplasty is less painful at 12 months compared with hemiarthroplasty in treatment of displaced femoral neck fracture. HSS J. 2008;4:48–54. doi: 10.1007/s11420-007-9061-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Macaulay W, Pagnotto MR, Iorio R, Mont MA, Saleh KJ. Displaced femoral neck fractures in the elderly: hemiarthroplasty versus total hip arthroplasty. J Am Acad Orthop Surg. 2006;14:287–293. doi: 10.5435/00124635-200605000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Macaulay W, Yoon RS, Parsley B, Nellans KW, Teeny SM. DFACTO Consortium. Displaced femoral neck fractures: is there a standard of care? Orthopedics. 2007;30:748–749. doi: 10.3928/01477447-20070901-08. [DOI] [PubMed] [Google Scholar]
- 31.Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–748. [PubMed] [Google Scholar]
- 32.Miyamoto RG, Kaplan KM, Levine BR, Egol KA, Zuckerman JD. Surgical management of hip fractures: an evidence-based review of the literature. I: femoral neck fractures. J Am Acad Orthop Surg. 2008;16:596–607. doi: 10.5435/00124635-200810000-00005. [DOI] [PubMed] [Google Scholar]
- 33.Mouzopoulos G, Stamatakos M, Arabatzi H, Vasiliadis G, Batanis G, Tsembeli A, Tzurbakis M, Safioleas M. The four-year functional result after a displaced subcapital hip fracture treated with three different surgical options. Int Orthop. 2008;32:367–373. doi: 10.1007/s00264-007-0321-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pang H. [Total hip arthroplasty and bipolar hemiarthroplasty for treatment of femoral neck fractures] [in Chinese] China Prac Med. 2011;6:81–83. [Google Scholar]
- 35.Parker MJ, Gurusamy KS, Azegami S. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev. 2010;6:CD001706. [DOI] [PMC free article] [PubMed]
- 36.Ravikumar KJ, Marsh G. Internal fixation versus hemiarthroplasty versus total hip arthroplasty for displaced subcapital fractures of femur: 13 year results of a prospective randomised study. Injury. 2000;31:793–797. doi: 10.1016/S0020-1383(00)00125-X. [DOI] [PubMed] [Google Scholar]
- 37.Rodríguez-Merchán EC. Displaced intracapsular hip fractures: hemiarthroplasty or total arthroplasty? Clin Orthop Relat Res. 2002;399:72–77. doi: 10.1097/00003086-200206000-00010. [DOI] [PubMed] [Google Scholar]
- 38.Schmidt AH, Leighton R, Parvizi J, Sems A, Berry DJ. Optimal arthroplasty for femoral neck fractures: is total hip arthroplasty the answer? J Orthop Trauma. 2009;23:428–433. doi: 10.1097/BOT.0b013e3181761490. [DOI] [PubMed] [Google Scholar]
- 39.Skinner P, Riley D, Ellery J, Beaumont A, Coumine R, Shafighian B. Displaced subcapital fractures of the femur: a prospective randomized comparison of internal fixation, hemiarthroplasty and total hip replacement. Injury. 1989;20:291–293. doi: 10.1016/0020-1383(89)90171-X. [DOI] [PubMed] [Google Scholar]
- 40.Sterling RS. Gender and race/ethnicity differences in hip fracture incidence, morbidity, mortality, and function. Clin Orthop Relat Res. 2011;469:1913–1918. doi: 10.1007/s11999-010-1736-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bekerom MP, Hilverdink EF, Sierevelt IN, Reuling EM, Schnater JM, Bonke H, Goslings JC, Dijk CN, Raaymakers EL. A comparison of hemiarthroplasty with total hip replacement for displaced intracapsular fracture of the femoral neck: a randomised controlled multicentre trial in patients aged 70 years and over. J Bone Joint Surg Br. 2010;92:1422–1428. doi: 10.1302/0301-620X.92B10.24899. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.