Abstract
Background
Persons with Parkinson disease (PD) experience turning difficulty, often leading to freezing of gait and falls. Visual information plays a significant role in locomotion and turning, and while the effects of deep brain stimulation (DBS) on oculomotor function have been well documented, the effects of DBS on oculomotor function during turning and on turning itself have yet to be fully elucidated.
Objective
To determine the effects of STN DBS on turning performance and related oculomotor performance in PD.
Methods
Eleven subjects with PD and DBS of the subthalamic nucleus performed a seated voluntary saccade task and standing 180° turns in DBS OFF and DBS ON conditions. Oculomotor data were captured using an infrared eye tracking system while segment rotations were measured using 3-D motion capture.
Results
During the seated saccade task, DBS did not improve saccade amplitude or latency. DBS also did not improve gait velocity and stride length during forward walking. During turning, DBS improved turn performance (turn duration), reduced the number of saccades performed during the turns, and increased the amplitude and velocity of the saccade initiating the turn. DBS decreased the intersegmental latencies (eye-head, eye-foot, and head-trunk) but this effect was lost for eye-head and eye-foot after controlling for the duration of the first gait cycle.
Conclusions
DBS significantly improves turn performance and related oculomotor performance. These findings add to the growing list of therapeutic benefits offered by DBS.
Keywords: Parkinson Disease, Deep Brain Stimulation, Saccades, Oculomotor Dysfunction, Turning
INTRODUCTION
Turning during gait is common and required during normal ambulation and activities of daily living. Individuals with Parkinson disease (PD), however, experience difficulty turning, leading to freezing of gait (FOG), falls, and fear of falling (Bloem et al., 2001; Bloem et al., 2004; Giladi et al., 1992). Falls during turns are eight times more likely to result in hip fracture than falls during straight line walking, and individuals with PD have a 3.2 fold greater risk of hip fracture than age-matched individuals without PD (Melton et al., 2006).
Recent studies have attempted to elucidate the cause of turning difficulty in PD in order to develop strategies to overcome the issue. Such studies have noted that persons with PD require more steps and take longer to complete a turn than healthy controls (Hong et al., 2009; Lohnes and Earhart, 2011; Morris et al., 2001; Stack and Ashburn, 2008) Additionally, individuals with PD show altered timing of segmental rotations during turn initiation, such that their turning strategy is more “en bloc” than healthy controls (Crenna et al., 2007; Hong et al., 2009; Huxham et al., 2008; Visser et al., 2007), although this finding may not be observed in early PD stages (Anastasopoulos et al., 2011).
It is also clear that visual information plays an integral role in this turning sequence. In healthy controls, the eyes participate in the top-down rotation sequence such that they eyes precede the sequential rotations of the head, trunk, and feet (Anastasopoulos et al., 2009). The initial saccade during a turn, in combination with subsequent head movements, provides a shift of gaze to a position aligned with the direction of travel. Gaze shifts precede shifts in center of mass (COM) trajectory during turning, and unexpected perturbations of gaze cause delays in COM movement to steer the body along the desired trajectory (Vallis, 2001). In subjects with PD, however, the amplitude of the initial saccade is smaller than in healthy controls, a greater number of smaller saccades are performed during the turn, and the timing of the initial saccade relative to the first step is altered. During standing turns, Anastasopoulos et al. (2011) found that patients with PD more frequently performed multiple saccades to reach a lateral target and expressed altered eye-head-trunk gaze shifts as compared with healthy controls. Lohnes and Earhart (2011) measured saccades during 180 degree turns and found that patients with PD had a longer delay between initiation of eye movement and start of the first step of the turn, and that first saccades were smaller and slower than controls. Further, measures of saccade function were correlated with turn performance. These oculomotor deficits are consistent with a large body of literature supporting voluntary saccade dysfunction in PD. Prolonged fixation times, bradykinesia, and akinesia during rapid alternating gaze shifts have been observed in PD, and voluntary saccades are widely described as being smaller and slower in PD (Briand et al., 1999). In gaze re-orienting tasks where the eyes rotate in concert with the head to fixate on a lateral target, eye-head coordination is found to be abnormal such that both saccades (White, et al., 1988) and head rotations (Hansen et al., 1990, White et al., 1988) are delayed, hypometric, and slow.
Few studies have been done to determine the effects of therapeutic interventions on turning in PD. While levodopa therapy is largely effective in improving MDS-UPDRS III scores and gait performance (O’Sullivan et al., 1998), the effect on turning dysfunction (turn duration, steps to turn, and the timing of body segment rotations) appears to be minimal (Hong and Earhart, 2010). Similarly, the effects of anti-Parkinson medications on saccade function are mixed. While the amplitude of voluntary saccades appears to be resistant to levodopa therapy (Crevits et al., 2000; Gibson and Kennard, 1987), levodopa may have a beneficial effect on voluntary saccade latencies (Hood et al., 2007; Vermersch et al., 1994), but a negative effect on reflexive saccade latencies (Hood et al., 2007; Michell et al., 2006). In contrast, the effects of subthalamic nucleus (STN) deep brain stimulation (DBS) on oculomotor performance are more robust and in line with evidence showing that DBS improves gait velocity and stride length in PD (Faist et al., 2001; Ferrarin et al., 2005). Rivaud-Pechoux et al. (2000) found a positive effect of STN DBS on saccade gain during a memory guided saccade task while Sauleau et al. (2008) reported improvements in gain and latency of saccades and gaze during head fixed and head free reflexive saccade tasks, respectively, with STN DBS. Finally, Temel et al. (2008; 2009) found a marked improvement in saccade latency distributions with STN-DBS In summary, the effects of DBS on oculomotor function have been well documented and DBS appears to provide more robust improvements in oculomotor control. However, only one study has tested the effects of DBS on turning in PD (Naushahi, 2012) and no studies have examined the effects of DBS on oculomotor control during turning. Therefore, the purpose of this study was to determine the effects of STN DBS on turning performance and related oculomotor performance in PD. Based on evidence that DBS improves both gait and oculomotor performance in PD, we hypothesized that turning performance would be improved with DBS, including an increase in initial saccade amplitude and alterations in the timing of the first saccade relative to turn onset.
METHODS
Participants
Eleven individuals with idiopathic PD participated in this investigation. Participants were recruited from a database of patients from Washington University School of Medicine’s (WUSM) Movement Disorders Center. All participants met the following inclusion criteria: aged 30 years or older, bilateral STN DBS and a minimum of 3 months post implantation surgery, currently taking levodopa medication for a minimum of 3 months (levodopa equivalent daily dose, LEDD = 840.8 ± 345.4 mg), normal central (except for PD in the PD group) and peripheral neurological function, able to stand independently for at least 30 minutes and walk independently without an assistive device, no history of vestibular disease and no evidence or history of dementia. Exclusionary criteria included: any serious medical condition other than PD, use of neuroleptic or other dopamine-blocking drug, use of drug that might affect balance such as benzodiazepines, evidence of abnormality on brain imaging (previously done for clinical evaluations-not part of this research), history or evidence of other neurological deficit, such as previous stroke or muscle disease, and history or evidence of orthopedic, muscular, or psychological problem that may affect task performance during the study. Idiopathic PD was based on a diagnosis of “definite PD” by a board certified neurologist, as previously described by Racette et al. (1999) based upon established criteria (Calne et al., 1992; Hughes et al., 1992). All participants gave written informed consent to perform experimental procedures approved by the Human Research Protection Office at WUSM.
Experimental Procedures
All study procedures were performed in the Locomotor Control Laboratory at WUSM. Participants were tested in the “OFF” state of their anti-Parkinson medication (i.e. after a 12-hour withdrawal of all anti-Parkinson medications). The experimental protocol was performed twice; once with DBS stimulators turned on using clinical settings, and once with DBS stimulators turned off, with the order of the conditions counterbalanced. Testing procedures began a minimum of 45 minutes after DBS settings were changed as it has been shown that 90% of changes in motor performance (MDS-UPDRS-III) occur within 45 minutes of DBS being turned off, and changes after DBS is turned on occur more quickly, with 90% of changes in motor performance occurring in 15–30 minutes (Temperli et. al., 2003). Prior to commencing each round of the experimental protocol, the Movement Disorder Society Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) Motor Subscale III was administered according to Goetz et al. (2008) by a trained rater. The MDS-UPDRS-III is a measure of severity of PD motor symptoms, as well as physical disability, and includes measures of rigidity, gait, tremor, hand/arm and leg movements (bradykinesia), speech, and facial expressions. The modified Hoehn and Yahr scale also was used to evaluate disease severity in PD (Goetz et al., 2004) and the FOG questionnaire (FOG-Q) was assessed to categorize freezers and non-freezers (Giladi et al., 2000).
Saccade Task
To evaluate simple voluntary saccade function during an eyes only task, participants performed saccades to targets positioned 20° to the left and right of a center target. The task was performed in a seated position with the participant’s head positioned in a chin-rest to minimize head movement and rotation, and the square targets (2.5 cm X 2.5 cm) were located at eye level on a white wall in front of the subject. Upon hearing an auditory tone, subjects were instructed to react as quickly as possible by performing a saccade to one of the lateral targets. Within each block of trials, the order of left and right movements was randomized. Five trials were performed for each target.
Turning Protocol
Following the seated saccade task, participants completed in-place turns of 180° amplitude. Instructions were given to perform the turns in a comfortable and normal fashion. No specific auditory or visual cues were provided to cue turn onset or completion other than directing subjects to “turn 180 degrees to face the wall behind you.” Participants were instructed to begin the movement anytime after receiving the turn direction instruction of left or right for the given trial. Turns were completed to both the right and left in randomized order. Participants completed a minimum of 5 turns in each direction. Data quality was visually monitored in real time and additional turns were completed as needed to ensure an adequate number of quality trials for analysis.
Full body kinematic data were captured using an eight camera, passive marker, 3-dimensional, high–resolution motion capture system (Motion Analysis Corporation, Santa Rosa, CA) sampling at 100 Hz in Cortex software (Motion Analysis Corporation, Santa Rosa, CA). Thirty-four retro-reflective markers were positioned on the head (top of head, back of head, left ear, right ear), trunk (left and right acromion, right scapula, sternal notch, xyphoid process, 7th cervical vertebra, 12th thoracic vertebra), pelvis (left and right anterior superior iliac spine, left and right posterior superior iliac spine, sacrum), both legs (greater trochanter, anterior thigh, lateral femoral condyle, tibial tuberosity, front of shank, lateral malleolus) and both feet (calcaneus, navicular, distal 2nd metatarsal). Ocuolmotor data were captured using a head-mounted infrared binocular eye tracking system (Applied Sciences Laboratory, Bedford, MA) and electrooculography (EOG). Oculomotor data were captured synchronously at 1000Hz on the same PC workstation with kinematic data in Cortex software.
Walking Task
To confirm the clinical benefit of DBS, subjects performed 3 trials of forward walking at a comfortable, self-selected pace across a 5 m instrumented, computerized GAITRite walkway (CIR Systems, Inc., Havertown, PA). Gait velocity and stride length were used as measures of gait function.
Data Processing
Individual kinematic marker data and analog data were filtered using 4th order low-pass Butterworth filters. Marker data were filtered in Cortex with a cut-off frequency of 6 Hz while analog data were filtered in MotionMonitor (Innsport, Chicago, IL) with a cut-off frequency of 20 Hz. Global and segment coordinate systems were defined in MotionMonitor with the positive X-axis pointing anteriorly, positive Y-axis pointing to the left, and positive Z-axis pointing upward vertically. For the turning task, rotations of the head, trunk, pelvis, and feet about global Z were extracted using a Z-X-Y Euler sequence. Subsequently, kinematic angle data and filtered analog data were exported for further processing in custom written MATLAB software (The Mathworks, Inc., Natick, MA).
For the turning task, we characterized the timing of the rotation sequence by identifying the time of onset of each segment yaw rotation (relative to the global coordinate system). This was determined by identifying the first frame at which the yaw rotation reached five degrees above baseline. Similar criteria were used to identify turn offset, defined as the frame at which the yaw rotation came within five degrees of maximal, final position. Eye tracker and EOG data were used to identify and measure saccades occurring just prior to and during turn performance. Saccades were identified visually and later confirmed to be true saccades if the maximum velocity of the eye movement exceeded 30 degrees/sec (Chan et al., 2005; Versino et al., 2005). Onsets and offsets of the first saccade associated with each turn were identified visually. Using these time points, saccade amplitude, peak velocity, and timing of the first saccade relative to head and foot rotations were calculated. Our primary variables of interest for the turning task were the amplitude and velocity of the saccade initiating the turn, the total number of saccades performed during the turn, turn duration, and the timing of the first saccade relative to the onset of the first step. Secondary variables of interest included the timing of the turning sequence, i.e. the timing of each body segment (head, trunk, pelvis) relative to the first step of the turn and the relationship between peak saccade velocity and amplitude, or main-sequence-slope, calculated as saccade peak velocity/ saccade peak amplitude.
For the seated task, the first saccade following the auditory cue was measured in a similar manner. Variables of interest were the latency of saccade onset with respect to the auditory cue and saccade amplitude.
Individual trials were excluded from analysis if eye position or body segment rotations about the global Z-axis (during the turn task) were not static for at least 1000ms prior to turn onset. Trials were also excluded if artifacts in oculomotor data due to blinks, prolonged closure of eyelids, or other factors precluded measurement of the initial saccade. Remaining trials were averaged to obtain a single data point for each combination of medication and DBS state within each subject. For the turning and seated tasks, left and right trials were combined for analysis as performance did not differ between leftward and rightward trials.
Data Analysis
Prior to performing statistical tests, all variables were tested for normality and each variable was examined visually for outliers, for which none were identified. To compare between DBS-OFF and DBS-ON, variables that were normally distributed were tested using parametric paired t-tests, while variables found to violate the normality assumption were tested using the Related-Samples Wilcoxon Signed Rank Test. Pearson’s correlations coefficient was employed to examine correlations between clinical measures and turn performance data. All statistical tests were two tailed with criterion for statistical significance set at p<0.05.
RESULTS
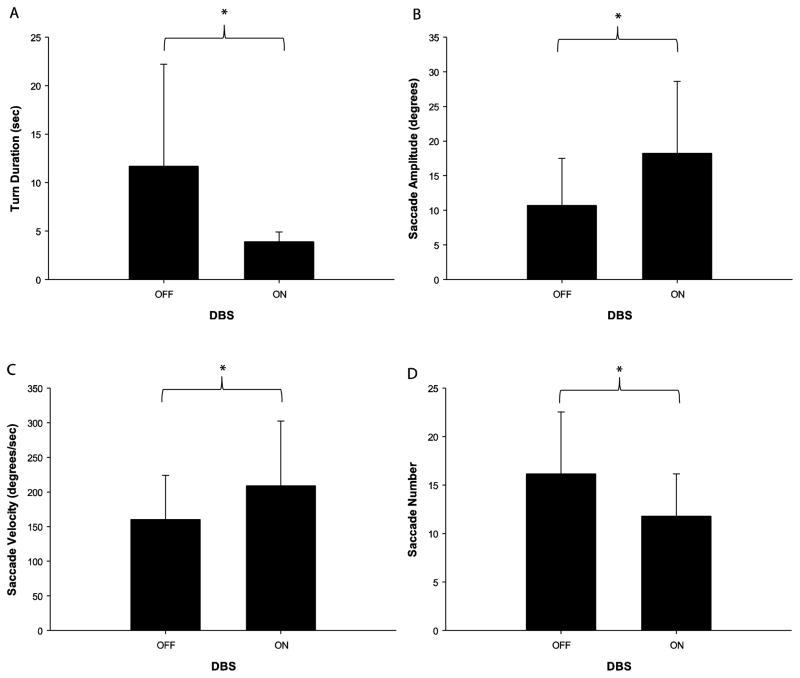
Demographic data are displayed in Table 1; performance data are displayed in Tables 2 and 3. MDS-UPDRS III scores improved significantly with DBS (t=4.04, p=0.002) while gait velocity and stride length did not (t=1.59, p=0.143; t=1.37, p=0.202, respectively). DBS significantly decreased turn duration (t=2.59, p=0.027) and the number of saccades performed during turns (t=5.133, p<0.001) and increased the amplitude and velocity of the first saccade performed during the turn (t=4.96, p=0.001; t=3.82, p=0.003, respectively). The main-sequence-slope was also decreased with DBS (DBS OFF=17.78 ± 8.3, DBS ON = 13.02 ± 5.6; t=3.72, p=0.004).
Table 1.
Subject Demographics
| Subject | Age (years) | Gender | MDS-UPDRS-III DBS-OFF |
Disease Duration (years) | Hoehn & Yahr Stage |
LEDD (mg) | DBS settings Voltage/Pulse Width(μs)/Freq (Hz) |
|---|---|---|---|---|---|---|---|
| 1 | 56 | M | 34 | 16 | 2.5 | 400 | 2.8/ 60/ 185 |
| 2* | 67 | M | 45 | 22 | 2.5 | 1271 | 3.0/ 60/ 185 |
| 3 | 58 | M | 41 | 13 | 2.5 | 1436 | 3.3/ 60/ 185 |
| 4* | 67 | M | 45 | 20 | 2.5 | 1170 | 3.3/ 60/ 185 |
| 5 | 75 | M | 50 | 10 | 2.5 | 1719 | 3.0/ 60/ 185 |
| 6 | 80 | M | 39 | 11 | 2 | 1000 | 2.8/ 60/ 185 |
| 7 | 67 | F | 59 | 27 | 3 | 640 | 2.9/ 60/ 185 |
| 8* | 72 | F | 49 | 10 | 4 | X | 3.0/ 60/ 185 |
| 9 | 64 | F | 36 | 14 | 2.5 | 700 | 3.2/ 60/ 185 |
| 10 | 65 | M | 67 | 23 | 3 | 1750 | 3.1/ 90/ 185 |
| 11 | 63 | M | 39 | 6 | 2 | 1200 | 2.4/ 60/ 185 |
| 66.6 ±7.1 | 45.8 ± 10.0 | 15.6 ± 6.6 | 1128.68 ± 450.5 |
Values are means ± standard deviations. x = Data not recorded.
Freezer - Reported freezing at least once/week on item 3 of the FOG-Q.
Table 2.
GAITRite and Seated Saccade Task Data
| DBS OFF | DBS ON | |
|---|---|---|
| GAITRite Data | ||
| Gait Velocity (cm/s) | 94.9 ± 30.1 | 106.8 ± 20.5 |
| Stride Length (cm) | 103.8 ± 25.2 | 113.4 ± 17.9 |
| Seated Saccade Task | ||
| Saccade Latency (ms) | 335.8 ± 98.0 | 335.0 ± 104.0 |
| Saccade Amplitude (°) | 15.0 ± 2.1 | 16.0 ± 1.3 |
Values are means ± standard deviations.
Significant difference (p<0.05)
Table 3.
Kinematic Performance Data
| DBS OFF | DBS ON | |
|---|---|---|
| Eye-Head Latency (ms) | 320.3 ± 275.6* | 168.9 ± 133.6 |
| Head-Trunk Latency (ms) | 71.5 ± 115.1* | 11.8 ± 48.2 |
| Eye-Foot Latency (ms) | 667.2 ± 438.1* | 334.5 ± 289.8 |
| N. Eye-Head Latency | 306.8 ± 179.4 | 247.4 ± 277.4 |
| N. Eye-Foot Latency (% First Gait cycle) | 48.8 ± 33.5 | 59.9 ± 76.7 |
| N. Head-Trunk Latency (% First Gait cycle) | 7.5 ± 12.1 | 2.7 ± 6.6 |
| N. Head-Foot Latency (% First Gait cycle) | 18.2 ± 29.2 | 35.1 ± 49.9 |
Values are means ± standard deviations.
Significant difference (p<0.05)
In correlating clinical measures with kinematic measures, baseline MDS-UPDRS-III scores (DBS-OFF) correlated with the percentage of improvement in saccade amplitude (r=0.759, p=0.007). Baseline MDS-UPDRS-III scores were not significantly correlated with improvements in turn duration (r=−0.366, p=0.268), saccade velocity (r=0.260, p=0.440), or the number of saccade performed during the turn (r=−0.584, p=0.059). Baseline postural instability and gait (PIGD, items 3.15 – 3.19 from MDS-UPDRS-III) correlated with improvements in saccade amplitude (r=0.623, p=0.40), velocity (r=0.631, p=0.37), and number (r=−0.731, p=0.011), while the baseline PIGD correlation with improvements in turn duration approximated significance (r=0.585, p=0.059).
In characterizing the timing of the rotation sequence, DBS decreased the eye-head (t=2.18, p=0.055), eye-foot (t=4.21, p=0.002), and head-trunk (t=2.40, p=0.037) latencies. When dividing the latencies by the duration of the first gait cycle to obtain normalized latencies in order to control for turning speed, each of the above effects of DBS were removed (t=0.78, p=0.455; t=0.612, p=0.554; t=1.54, p=0.154, respectively). Finally, during the seated tasks, there were no significant effects of DBS (t=0.059, p=0.954; t=1.45, p=.182) in regards to saccade latency or amplitude, respectively.
DISCUSSION
The purpose of this study was to determine the effects of DBS on measures of turning performance and related oculomotor performance in PD. In summary, DBS had a profound effect on turning duration and the number of saccades performed during the turn. DBS also increased the amplitude, velocity, and main-sequence-slope of the first saccade performed during the turn. Finally, the intersegmental latencies between the eyes, head, trunk, and feet were decreased by DBS, however this effect was eliminated when we controlled for turning speed.
To the best of our knowledge, this is the first study to address the therapeutic effects of DBS on turning in PD as well as the first to measure the effects of DBS on oculomotor function during a functionally relevant task. Our findings are consistent with previous research that shows an improvement in motor symptoms (MDS-UPDRS III) with DBS. DBS was also effective in increasing gait velocity by approximately 13% and stride length by approximately 10% in our study, although these differences did not reach statistical significance. Our findings of improved turning duration and concomitant improvements in oculomotor performance during turns are novel yet anticipated based on the efficacy of DBS in improving saccade function and gait in previous studies. Previous work in our lab (Lohnes and Earhart, 2011) showed that persons with PD turn slower and with more steps than healthy, age-matched controls, and that turn performance is correlated with oculomotor function such that individuals who perform later, larger, faster, and fewer saccades turn better. Similarly, data herein suggest that improved oculomotor performance associated with DBS is correlated with improved turn performance. Neither of these studies, however, address a cause-and-effect relationship between oculomotor and turn performance. Since the oculomotor system initiates the turning sequence, we hypothesize that saccades occurring before and early in the turn sequence may affect subsequent turning kinematics, but it is also plausible that improvements in oculomotor function (as measured herein) are driven by improved turn performance. For example, a decrease in the number of saccades performed during the turn may be an effect of shortened turn duration and increased turn speed. Beyond the role of the oculomotor system, other factors are also likely to contribute to the improved turn performance noted with DBS. DBS improved overall MDS-UPDRS-III scores as well as bradykinesia, rigidity, and PIGD, measures that are all independent from saccade function but could affect turn performance. DBS also produced a shortening of intersegmental latencies (eye-head, eye-foot, head-trunk). Again, while DBS-related improvements in saccade function could have contributed to this, the decreased intersegmental latencies are most likely due to the increased speed with which subjects were able to complete the turns during DBS stimulation, hence shortening all aspects of the turn sequence. This hypothesis is supported by the fact that intersegmental latencies were similar when we controlled for the duration of the first gait cycle.
Subjects in this study displayed a top-down rotation sequence in regards to the timing of rotation onset of the various segments (eye-head, head-trunk, trunk-foot). This is in contrast to Hong & Earhart (2010) and Hong et al. (2009) which reported en bloc timing in a group of non-DBS PD patients, but in line with Anastasopoulos et al.(2011) who observed a top-down rotation sequence in a sample of mild PD patients. It is possible that the turning sequence used herein is still more “en bloc” than the pattern utilized by healthy controls, and perhaps falls somewhere between that observed by Hong et al. and Anastasopoulos.
While DBS improved walking and turning performance, it did not improve saccade performance during the seated saccade task, which is contrary to previous research showing beneficial effects of DBS on saccade performance. There were, however, some methodological differences between ours and previous studies. Previous studies examined the effects of DBS on both voluntary (memory guided saccades, anti-saccades) and reflexive saccades using protocols where the saccade was cued visually (either the appearance of a lateral target or the disappearance of the central target). In our study, we used an auditory cue to initiate the saccade. Furthermore, our targets were static in that they remained in view for the duration of the test. In contrast to memory-guided or anti-saccade paradigms where the subjects perform saccades to a target-less location, our subjects made saccades toward a static visual target which may have served as an external cue that facilitated performance.
Limitations
There are a few limitations related to this study. First, we did not consider specific electrode placement within the STN when selecting participants, resulting in some likely heterogeneity among subjects in regards to stimulation localization within the STN. While saccade-related neurons are clustered in the ventral STN (Fawcett et al., 2005; Matsumura et al., 1992), PD motor symptoms such as gait and balance appear to respond similarly to dorsal and ventral STN DBS (McNeely et al., 2011). As such, functional tasks that significantly involve the oculomotor system (e.g. turning) may be best ameliorated by DBS in the ventral STN. Selecting sub-groups of patients based on electrode placement (ie: dorsal vs. ventral STN) may offer further understanding of the effect of STN DBS on oculomotor function during turning, but cognitive function must be considered in such studies as response inhibition has been shown to decrease with ventral STN DBS (Hershey et al., 2010). Second, during the seated saccade task, we used a novel paradigm with static targets and an auditory cue. This may explain the lack of effect of DBS on saccade amplitude and latency. Finally, our relatively small sample size may have contributed to the lack of statistical significance observed in gait parameters.
Conclusions/Implications
In conclusion, STN DBS is largely effective in improving both straight walking and turning performance in PD, including increases in saccade amplitude and a decreased number of saccades required to complete the turn. These results add to the growing number of known benefits offered by DBS, and add to the functional applicability of previous research that has found beneficial effects of DBS on saccades and gaze during seated tasks. Future work may aim to define optimal DBS electrode placement for patients whose primary motor complications include freezing during turning, or a history of falls during turns.
Supplementary Material
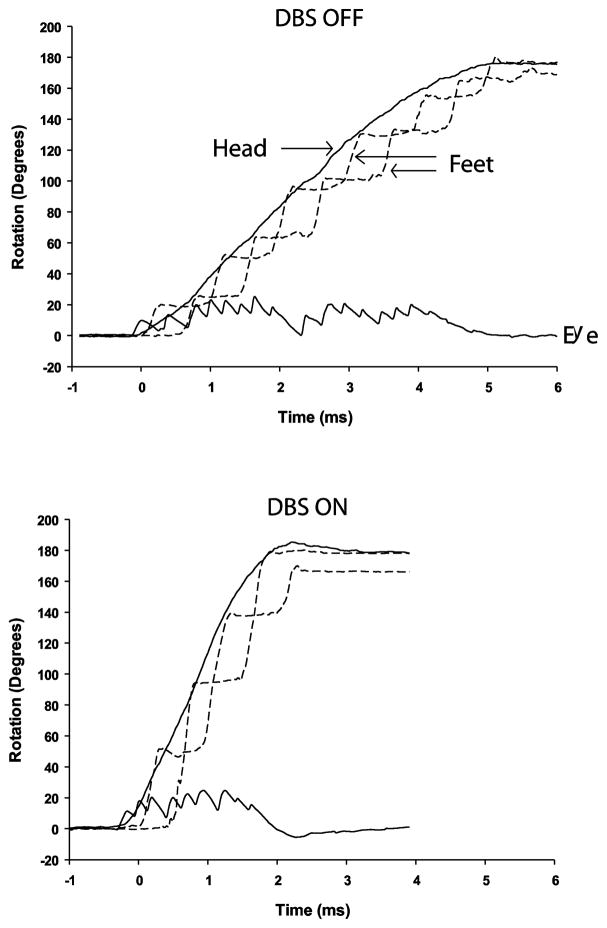
Figure 1.
Representative data from individual turn trials showing eye-in-head, head-overground, and foot-over-ground rotations about the z (vertical) axis. Top = DBS OFF, Bottom = DBS ON. All turns are to the right and are initiated with the right foot. DBS improves turn duration and reduce the number of saccades required to complete the turn.
Figure 2.
Effects of DBS on oculomotor performance during turns. *Significant difference between conditions (p<0.05).
Highlights.
Tested oculomotor function during in-place turning in patients with PD and DBS
Quantified the effect of DBS on turn performance
DBS improved turning performance and reduced number of saccades
DBS improved saccade amplitude and velocity, decreased intersegmental latencies
Acknowledgments
We thank Marie McNeely for assistance with data collection, Brian Morrell for assistance with data processing, and Dr. Richard Abrams for assistance with project design and pilot testing. This publication was made possible by R01 HD056015, the Barnes Jewish Hospital Foundation, and Grant Number UL1 RR024992 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Additional support came from the St. Louis Chapter of the American Parkinson Disease Association (APDA) and the APDA Advanced Center for PD Research at Washington University in St. Louis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anastasopoulos D, Ziavra N, Hollands M, Bronstein A. Gaze displacement and inter-segmental coordination during large whole body voluntary rotations. Exp Brain Res. 2009;193:323–336. doi: 10.1007/s00221-008-1627-y. [DOI] [PubMed] [Google Scholar]
- Anastasopoulos D, Ziavra N, Savvidou E, Bain P, Bronstein AM. Altered eye-to-foot coordination in standing parkinsonian patients during large gaze and whole-body reorientations. Mov Disord. 2011;26:2201–2211. doi: 10.1002/mds.23798. [DOI] [PubMed] [Google Scholar]
- Bacon WE. Secular trends in hip fracture occurrence and survival: age and sex differences. J Aging Health. 1996;8:538–553. doi: 10.1177/089826439600800404. [DOI] [PubMed] [Google Scholar]
- Bloem BR, Grimbergen YA, Cramer M, Willemsen M, Zwinderman AH. Prospective assessment of falls in Parkinson’s disease. J Neurol. 2001;248:950–958. doi: 10.1007/s004150170047. [DOI] [PubMed] [Google Scholar]
- Bloem BR, Hausdorff JM, Visser JE, Giladi N. Falls and freezing of gait in Parkinson’s disease: a review of two interconnected, episodic phenomena. Mov Disord. 2004;19:871–884. doi: 10.1002/mds.20115. [DOI] [PubMed] [Google Scholar]
- Briand KA, Strallow D, Hening W, Poizner H, Sereno AB. Control of voluntary and reflexive saccades in Parkinson’s disease. Exp Brain Res. 1999;129:38–48. doi: 10.1007/s002210050934. [DOI] [PubMed] [Google Scholar]
- Calne DB, Snow BJ, Lee C. Criteria for diagnosing Parkinson’s disease. Ann Neurol. 1992;32(Suppl):S125–127. doi: 10.1002/ana.410320721. [DOI] [PubMed] [Google Scholar]
- Chan F, Armstrong IT, Pari G, Riopelle RJ, Munoz DP. Deficits in saccadic eye-movement control in Parkinson’s disease. Neuropsychologia. 2005;43:784–796. doi: 10.1016/j.neuropsychologia.2004.06.026. [DOI] [PubMed] [Google Scholar]
- Crenna P, Carpinella I, Rabuffetti M, Calabrese E, Mazzoleni P, Nemni R, Ferrarin M. The association between impaired turning and normal straight walking in Parkinson’s disease. Gait Posture. 2007;26:172–178. doi: 10.1016/j.gaitpost.2007.04.010. [DOI] [PubMed] [Google Scholar]
- Crevits L, Versijpt J, Hanse M, De Ridder K. Antisaccadic effects of a dopamine agonist as add-on therapy in advanced Parkinson’s patients. Neuropsychobiology. 2000;42:202–206. doi: 10.1159/000026694. [DOI] [PubMed] [Google Scholar]
- Faist M, Xie J, Kurz D, Berger W, Maurer C, Pollak P, Lucking CH. Effect of bilateral subthalamic nucleus stimulation on gait in Parkinson’s disease. Brain. 2001;124:1590–1600. doi: 10.1093/brain/124.8.1590. [DOI] [PubMed] [Google Scholar]
- Fawcett AP, Dostrovsky JO, Lozano AM, Hutchison WD. Eye movement-related responses of neurons in human subthalamic nucleus. Exp Brain Res. 2005;162:357–365. doi: 10.1007/s00221-004-2184-7. [DOI] [PubMed] [Google Scholar]
- Ferrarin M, Rizzone M, Bergamasco B, Lanotte M, Recalcati M, Pedotti A, Lopiano L. Effects of bilateral subthalamic stimulation on gait kinematics and kinetics in Parkinson’s disease. Exp Brain Res. 2005;160:517–527. doi: 10.1007/s00221-004-2036-5. [DOI] [PubMed] [Google Scholar]
- Gibson JM, Kennard C. Quantitative study of “on-off” fluctuations in the ocular motor system in Parkinson’s disease. Adv Neurol. 1987;45:329–333. [PubMed] [Google Scholar]
- Giladi N, McMahon D, Przedborski S, Flaster E, Guillory S, Kostic V, Fahn S. Motor blocks in Parkinson’s disease. Neurology. 1992;42:333–339. doi: 10.1212/wnl.42.2.333. [DOI] [PubMed] [Google Scholar]
- Giladi N, Shabtai H, Simon ES, Biran S, Tal J, Korczyn AD. Construction of freezing of gait questionnaire for patients with Parkinsonism. Parkinsonism Relat Disord. 2000;6:165–170. doi: 10.1016/s1353-8020(99)00062-0. [DOI] [PubMed] [Google Scholar]
- Goetz CG, Poewe W, Rascol O, Sampaio C, Stebbins GT, Counsell C, Giladi N, Holloway RG, Moore CG, Wenning GK, Yahr MD, Seidl L. Movement Disorder Society Task Force report on the Hoehn and Yahr staging scale: status and recommendations. Mov Disord. 2004;19:1020–1028. doi: 10.1002/mds.20213. [DOI] [PubMed] [Google Scholar]
- Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, Poewe W, Sampaio C, Stern MB, Dodel R, Dubois B, Holloway R, Jankovic J, Kulisevsky J, Lang AE, Lees A, Leurgans S, LeWitt PA, Nyenhuis D, Olanow CW, Rascol O, Schrag A, Teresi JA, van Hilten JJ, LaPelle N. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord. 2008;23:2129–2170. doi: 10.1002/mds.22340. [DOI] [PubMed] [Google Scholar]
- Hansen HC, Gibson JM, Zangemeister WH, Kennard C. The effect of treatment on eye-head coordination in Parkinson’s disease. J Vestib Res. 1990;1:181–186. [PubMed] [Google Scholar]
- Hershey T, Campbell MC, Videen TO, Lugar HM, Weaver PM, Hartlein J, Karimi M, Tabbal SD, Perlmutter JS. Mapping Go-No-Go performance within the subthalamic nucleus region. Brain. 2010;133:3625–3634. doi: 10.1093/brain/awq256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong M, Earhart GM. Effects of medication on turning deficits in individuals with Parkinson’s disease. J Neurol Phys Ther. 2010;34:11–16. doi: 10.1097/NPT.0b013e3181d070fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong M, Perlmutter JS, Earhart GM. A kinematic and electromyographic analysis of turning in people with Parkinson disease. Neurorehabil Neural Repair. 2009;23:166–176. doi: 10.1177/1545968308320639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood AJ, Amador SC, Cain AE, Briand KA, Al-Refai AH, Schiess MC, Sereno AB. Levodopa slows prosaccades and improves antisaccades: an eye movement study in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2007;78:565–570. doi: 10.1136/jnnp.2006.099754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry. 1992;55:181–184. doi: 10.1136/jnnp.55.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huxham F, Baker R, Morris ME, Iansek R. Head and trunk rotation during walking turns in Parkinson’s disease. Mov Disord. 2008;23:1391–1397. doi: 10.1002/mds.21943. [DOI] [PubMed] [Google Scholar]
- Lohnes CA, Earhart GM. Saccadic Eye Movements Are Related to Turning Performance in Parkinson Disease. J Parkinsons Dis. 2011;1:109–118. doi: 10.3233/JPD-2011-11019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsumura M, Kojima J, Gardiner TW, Hikosaka O. Visual and oculomotor functions of monkey subthalamic nucleus. J Neurophysiol. 1992;67:1615–1632. doi: 10.1152/jn.1992.67.6.1615. [DOI] [PubMed] [Google Scholar]
- McNeely ME, Hershey T, Campbell MC, Tabbal SD, Karimi M, Hartlein JM, Lugar HM, Revilla FJ, Perlmutter JS, Earhart GM. Effects of deep brain stimulation of dorsal versus ventral subthalamic nucleus regions on gait and balance in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2011;82:1250–1255. doi: 10.1136/jnnp.2010.232900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melton LJ, 3rd, Leibson CL, Achenbach SJ, Bower JH, Maraganore DM, Oberg AL, Rocca WA. Fracture risk after the diagnosis of Parkinson’s disease: Influence of concomitant dementia. Mov Disord. 2006;21:1361–1367. doi: 10.1002/mds.20946. [DOI] [PubMed] [Google Scholar]
- Michell AW, Xu Z, Fritz D, Lewis SJ, Foltynie T, Williams-Gray CH, Robbins TW, Carpenter RH, Barker RA. Saccadic latency distributions in Parkinson’s disease and the effects of L-dopa. Exp Brain Res. 2006;174:7–18. doi: 10.1007/s00221-006-0412-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris ME, Huxham F, McGinley J, Dodd K, Iansek R. The biomechanics and motor control of gait in Parkinson disease. Clin Biomech (Bristol, Avon) 2001;16:459–470. doi: 10.1016/s0268-0033(01)00035-3. [DOI] [PubMed] [Google Scholar]
- Naushahi MJ, AKL, Lee PY, Anastasopoulos D, Pavese N, Bain PG, Bronstein AM, Nandi D. Efficacy of chronic bilateral STN-DBS on alteren eye-to-foot co-ordination in standing advanced Parkinsonian patients during large gaze and whole-body reorientations. Parkinsonism Relat Disord. 2012;18:S148. [Google Scholar]
- O’Sullivan JD, Said CM, Dillon LC, Hoffman M, Hughes AJ. Gait analysis in patients with Parkinson’s disease and motor fluctuations: Influence of levodopa and comparison with other measures of motor function. Movement Disorders. 1998;13:900–906. doi: 10.1002/mds.870130607. [DOI] [PubMed] [Google Scholar]
- Racette BA, Rundle M, Parsian A, Perlmutter JS. Evaluation of a screening questionnaire for genetic studies of Parkinson’s disease. Am J Med Genet. 1999;88:539–543. [PubMed] [Google Scholar]
- Rivaud-Pechoux S, Vermersch AI, Gaymard B, Ploner CJ, Bejjani BP, Damier P, Demeret S, Agid Y, Pierrot-Deseilligny C. Improvement of memory guided saccades in parkinsonian patients by high frequency subthalamic nucleus stimulation. J Neurol Neurosurg Psychiatry. 2000;68:381–384. doi: 10.1136/jnnp.68.3.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sauleau P, Pollak P, Krack P, Courjon JH, Vighetto A, Benabid AL, Pelisson D, Tilikete C. Subthalamic stimulation improves orienting gaze movements in Parkinson’s disease. Clin Neurophysiol. 2008;119:1857–1863. doi: 10.1016/j.clinph.2008.04.013. [DOI] [PubMed] [Google Scholar]
- Stack E, Ashburn A. Dysfunctional turning in Parkinson’s disease. Disabil Rehabil. 2008;30:1222–1229. doi: 10.1080/09638280701829938. [DOI] [PubMed] [Google Scholar]
- Temel Y, Visser-Vandewalle V, Carpenter RH. Saccadic latency during electrical stimulation of the human subthalamic nucleus. Curr Biol. 2008;18:R412–414. doi: 10.1016/j.cub.2008.03.008. [DOI] [PubMed] [Google Scholar]
- Temel Y, Visser-Vandewalle V, Carpenter RH. Saccadometry: a novel clinical tool for quantification of the motor effects of subthalamic nucleus stimulation in Parkinson’s disease. Exp Neurol. 2009;216:481–489. doi: 10.1016/j.expneurol.2009.01.007. [DOI] [PubMed] [Google Scholar]
- Temperli P, Ghika J, Villemure JG, Burkhard PR, Bogousslavsky J, Vingerhoets FJG. How Parkinsonian signs return after discontinuation of subthalamic DBS? Neurology. 2003;60:78–81. doi: 10.1212/wnl.60.1.78. [DOI] [PubMed] [Google Scholar]
- Vallis LA, Patla AE, Adkin AL. Control of steering in the presence of unexpected head yaw movements. Influence on sequencing of subtasks. Exp Brain Res. 2001;138:128–134. doi: 10.1007/s002210100680. [DOI] [PubMed] [Google Scholar]
- Vermersch AI, Rivaud S, Vidailhet M, Bonnet AM, Gaymard B, Agid Y, Pierrot-Deseilligny C. Sequences of memory-guided saccades in Parkinson’s disease. Ann Neurol. 1994;35:487–490. doi: 10.1002/ana.410350419. [DOI] [PubMed] [Google Scholar]
- Versino M, Zavanone C, Colnaghi S, Beltrami G, Pacchetti C, Zangaglia R, Cosi V. Binocular control of saccades in idiopathic Parkinson’s disease. Ann N Y Acad Sci. 2005;1039:588–592. doi: 10.1196/annals.1325.074. [DOI] [PubMed] [Google Scholar]
- Visser JE, Voermans NC, Oude Nijhuis LB, van der Eijk M, Nijk R, Munneke M, Bloem BR. Quantification of trunk rotations during turning and walking in Parkinson’s disease. Clin Neurophysiol. 2007;118:1602–1606. doi: 10.1016/j.clinph.2007.03.010. [DOI] [PubMed] [Google Scholar]
- White OB, Saint-Cyr JA, Tomlinson RD, Sharpe JA. Ocular motor deficits in Parkinson’s disease. III. Coordination of eye and head movements. Brain. 1988;111 (Pt 1):115–129. doi: 10.1093/brain/111.1.115. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.