Abstract
Myeloid derived suppressor cells (MDSCs) are primarily recognized for their immunosuppressive properties in malignant disease. However, their interaction with other innate immune cells and their regulation of immune responses such as in parasitic infection necessitate further characterization. We utilized our previously published mouse model of MDSC accumulation to examine the immunoregulatory role of MDSCs in B16 melanoma metastasis and Nippostrongylus brasiliensis (Nb) infection. Here we demonstrate that the activity of MDSCs is dependent on the immune stimuli and subset induced. Monocytic MDSCs predictably suppressed anti-tumor immune responses but granulocytic MDSCs surprisingly enhanced the clearance of Nb infection. Intriguingly, both results were dependent on MDSC interaction with mast cells (MCs) as demonstrated by adoptive transfer studies in MC-deficient (KitWsh/Wsh) mice. These findings were further supported by ex vivo co-cultures of MCs and MDSCs, indicating a synergistic increase in cytokine production. Thus MCs can enhance both immunosuppressive and immunosupportive functions of MDSCs.
INTRODUCTION
Acute inflammatory reactions stimulate the development and recruitment of myeloid lineage cells, including neutrophils and macrophages. Unresolved inflammation increases myelopoiesis, shifting the distribution of myeloid subpopulations. This results in the premature bone marrow release of a heterogeneous population of mononuclear (CD11b+Ly6Chigh) and polymorphonuclear (CD11b+Ly6Ghigh) cells, known as myeloid derived suppressor cells (MDSCs). These cells are widely studied in the context of neoplasia. MDSCs exert their proneoplastic effects through the release of small soluble oxidizers, the depletion of essential amino acids from the local extracellular environment, and the impairment of T-cell/antigen recognition, all ultimately leading to T cell suppression(1). This MDSC mediated immune suppression and impairment of cancer immunotherapy has been extensively investigated(2). However, by limiting immune activation, MDSCs can serve a beneficial role in transplantation, autoimmunity, and sepsis(5). This dual role of MDSCs depends upon nitric oxide production, the cytokine milieu, and the interaction between MDSCs, T cells, and natural killer cells(3-6).
Another interaction that may be physiologically significant is MDSC/mast cell (MC) collaboration. While MCs have been well documented to mediate allergic inflammation, their demonstrated involvement in neoplastic disease is more recent. Mast cells have been shown to accumulate in the tumor microenvironment and correlate with poor prognosis(7). This is largely due to the secretion of various pro-inflammatory cytokines produced by the MCs (8). Additionally, MCs contribute to MDSC recruitment to the tumor site via the production of 5-lipoxygenase and IL-17(9,10). Given that MC deficient mice have weakened tumor growth and that MCs recruit MDSCs to the tumor microenvironment, it is necessary to further examine the contribution of this interaction to tumor metastasis. Furthermore, although several studies indicate the expansion, recruitment, and activity of MDSCs in parasitic infections, they do not clarify the extent to which MDSCs regulate this immune response(11).
Therefore, we analyzed the effect of MDSCs in anti-helminth immunity and B16 metastasis as well as the interaction with MCs during the immune response. We utilized our previously published mouse model of MDSC accumulation in a tumor free environment(12). In these mice, the overexpression of A Distintegrin and Metalloproteinase 10 (ADAM10), promotes the expansion of MDSCs that are analogous to tumor-induced MDSCs. Adoptive transfer (AT) studies using either C57Bl/6 (WT) or MC deficient KitWsh/Wsh mice were performed in parallel. Utilizing two different model systems, we demonstrate that the activity of MDSCs is variable as granulocytic MDSCs enhanced anti-parasite immunity while monocytic MDSCs promoted B16 metastasis. Intriguingly, both activities depend upon the presence of MCs. This intercellular communication leads to augmentation of Th2 polarizing cytokines that are beneficial in the case of parasitic infection but maladaptive in neoplasia. Thus, our findings indicate that MDSCs have an immunomodulatory role that is largely dependent on the type of stimuli, the MDSC population involved and the presence of mast cells.
MATERIALS AND METHODS
Mice
Mice were kept at VCU in line with humane treatment of laboratory animals set forth by NIH and AAALAC. C57BL/6 A10Tgs were generated by VCU Transgenic Mouse Core as previously described(12) and LM were used as controls. Pmel-1 and KitWsh/Wsh mice were purchased from Jackson Laboratories. All mouse protocols were approved by VCU Institutional Animal Care and Use Committee.
Cell Lines
Lewis Lung Carcinoma (LLC) cell line was obtained from the American Type Culture Collection (ATCC). B16-melanoma and GM-CSF-B16 cells were provided by H. Bear and maintained as previously described(13). Mouse bone marrow-derived mast cells (BMMC’s) were generated from mice through isolation and subsequent culture of bone marrow cells in complete RPMI.
Isolation of MDSCs and adoptive transfer
Spleens were harvested from A10Tg or LLC bearing WT mice depending upon experimental protocol. They were then dispersed into single cell suspensions and filtered through 70-μm nylon mesh strainers (Invitrogen). Erythrocytes were lysed using an ammonium chloride potassium (ACK) lysing buffer (Quality Biological). Gr-1+,Ly6G+,o r Ly6C+ cells were purified from A10Tg spleens using the EasySep PE-Selection kit from Stem Cell Technologies according to the manufacturer’s protocol. For AT studies, 5-10 × 106 naïve A10Tg MDSCs were tail vein injected into each experimental group. For T cell depletion, mice were injected with 200ug ip of anti-CD4 (GK1.5) and anti-CD8 (2.43) antibodies on days −3, −2, −1, 0, 5, 10.
ARG and NO detection
MDSC cytoplasmic extracts were prepared from isolated A10Tg and LLC bearing hosts and tested for urea production (DARG-200, BioAssay Systems). Nitric Oxide was measured using Greiss Reagent (Molecular Probes, G7921).
T cell suppression assays
For polyclonal T cell activation, CD90.2+ T cells were sorted from spleen and activated with immobilized anti-CD3 (10μg/mL) and soluble anti-CD28 (1μg/mL) in 96-well plates. Sorted MDSCs (Ly6G+, Gr−1+, and Ly6G−) from A10Tg or LLC tumor bearing mice were then added at increasing T cell:MDSC ratios. For antigen-specific T cell suppression assays, soluble gp100 (1μg/mL) was added to defined ratios of pmel-1 transgenic splenocytes and A10Tg MDSCs. Upon 54hrs of culture, 1μCi of [3H]-thymidine was added to each well for an additional 18 hrs and thymidine incorporation was measured.
BMMC co-culture with A10Tg MDSC
BMMCs were derived from femurs of WT naïve mice cultured in cRMPI containing 20% WEHI-3-conditioned medium over a four week period; and were resuspended at 0.5×106 cells/mL, loaded with 0.5ug/mL of mouse IgE, and cultured with MDSCs at 1:1 ratio in 10ng/mL IL-3 and 10ng/mL GM-CSF overnight. MCs were activated by DNP-HSA (20-100ng/mL) and supernatants were collected 6 or 18 hours after cross-linking for ELISA.
AIT of B16-melanoma
T cells were prepared for AIT as previously described (13). Recipient mice were injected i.v. with 0.25×106 B16 cells. One day prior to AIT, mice were pre-treated i.p. with 2 mg CYP and 1.2 mg of GEM and every five days with GEM only. After 14 days, lung nodules were counted as previously described(13,14) and if too many, were assigned 250.
Nb infection, gemcitabine treatment and adoptive transfer
Nb larvae were generously provided by Joe Urban (Agriculture Research Station, Beltsville, MD) and were maintained as previously described(15). Each experimental group of mice was infected with approximately 650 L3 Nb. Fecal egg burdens were enumerated on days 5-13, serum collected by tail vein nick. For mice injected with GEM, 1.2 mg was injected i.p. starting on Day 0 and repeated every five days throughout the experiment. For AT studies, WT mice were injected with 5-10 × 106 naïve A10Tg MDSCs via tail vein injection starting at day zero of infection and repeated every three days thereafter. Additional groups of animals were sacrificed on Day 7 post infection and the proximal halves of the small intestines were harvested. Adult worms were then purified and enumerated.
Statistical Analysis
P-values were calculated using unpaired two-tailed Student’s t-tests or unpaired Mann-Whitney analysis. Error bars represent the standard error of the mean between samples.
RESULTS AND DISCUSSION
MDSCs from A10Tg mice are phenotypically and functionally analogous to tumor-induced MDSCs
Although MDSC accumulation is a byproduct of ADAM10 overexpression in early hematopoietic progenitors, ADAM10 expression is not altered in these cells(12). To ascertain if A10Tg derived MDSCs are functional, ex vivo T cell suppression assays were performed. A10Tg MDSCs inhibited T cell proliferation of both A10Tg and WT purified T cells under polyclonal (Supplemental Figure S1A,B) and antigen-specific (Supplemental Figure S1C) conditions in a manner parallel to tumor-derived MDSCs (Supplemental Figure S1D). Tumor-derived MDSCs are further divided into granulocytic (CD11b+Ly6Ghigh) and more immunosuppressive monocytic (CD11b+Ly6Chigh) subsets(16). Accordingly, monocytic MDSCs possessed more suppressive potential. Furthermore, similar to T cells from tumor bearing hosts, A10Tg T cells also exhibited reduced levels of L-selectin (CD-62L), a receptor required for homing of naïve T cells to the lymph nodes (Supplemental Figure S1E,F) (17). MDSCs impair the T cell response through the activity of arginase 1 (Arg1) and inducible nitric oxide synthase (iNOS). Accordingly, A10Tg MDSCs had comparable levels of these enzymes to tumor derived MDSCs (Supplemental Figure S1G,H)(2). These ex vivo observations indicate that MDSCs present in tumor-free A10Tg animals behave similarly to tumor-derived MDSCs.
Monocytic MDSCs promote B16 metastasis
To examine in vivo activities of MDSCs from A10Tg mice, we utilized the B16 melanoma model. B16 was injected iv; while not a true metastasis, this allows comparison of tumor colonization into the lung with and without MDSC and is commonly used to assess adoptive immunotherapy (AIT)(13). When challenged with B16, A10Tg animals were more susceptible to metastasis than WT controls (Fig. 1A). The A10Tg animals had tumor nodules that were too numerous to count and were consequently assigned a count of 250. Parallel to the ex vivo assay, the suppressive activity of MDSCs was attributed to the monocytic population. When WT mice were challenged with B16 and AT either monocytic or granulocytic MDSCs, melanoma metastasized more aggressively in mice given the monocytic subset while granulocytic MDSCs had no effect (Supplemental Figure S2A). AIT exerted a minimal effect on A10Tg mice, suggesting that the presence of MDSCs diminished the activity of adoptively transferred T cells. While AIT treatment did not completely abolish metastasis in WT lungs, it nonetheless induced a significant decrease in metastatic lesions. Given that lymphodepleting chemotherapy is known to enhance AIT(18), the protocol was modified to incorporate cyclophosphamide (CYP) and gemcitabine (GEM). CYP lymphodepletes recipient mice, permitting homeostatic proliferation of transferred T cells and GEM preferentially decreases MDSC levels in tumor-bearing mice(19, 20). CYP and GEM alone and in combination in WT mice did not significantly alter metastasis, indicating that they have minimal effects on tumor cells (Supplemental Figure S2C). However, GEM selectively diminished the MDSC population in A10Tg mice without affecting lymphocyte levels (Supplemental Figure S2B). A10Tg mice treated with GEM alone exhibited an anti-tumor response comparable to WT counterparts, demonstrating that T cell function is restored upon MDSC depletion (Fig. 1B,C). Additionally, the combination of GEM,CYP, and AIT (tritherapy) resulted in complete regression of metastasis in both WT and A10Tgs (Fig. 1B,C). Figure 1D illustrates the significant abrogation of metastasis arising from tritherapy. Ideal AIT would utilize tumor-specific T cells and chemotherapy. Thus, the AIT protocol was adjusted to incorporate pmel-1 mice that are T cell receptor transgenic for gp100 melanoma peptide(13). Similar results were observed in that successful AIT required MDSC depletion (Supplemental Figure S2C). Although not shown, A10Tg mice were also more susceptible to Lewis Lung Carcinoma compared to WT controls. Thus, MDSCs in A10Tg mice are functionally analogous to tumor derived MDSCs, promote tumor metastasis, and compromise the efficacy of tumor immunotherapy.
Figure 1. MDSC depletion restores the anti-tumor response and prevents metastatic progression of B16 melanoma in A10Tg mice.
(A) Number of lung metastases in WT and A10Tg animals challenged with B16 melanoma with (filled bar) or without (open bar) adoptive immunotherapy, indicated as (A), as described in Methods. Number of lung metastases of WT (B) or A10Tg (C) mice challenged with B16 and treated as in A with the addition of cyclophosphamide and gemcitabine, represented as (C) and (G), respectively. (D) Representative lungs of WT and A10Tg mice with AIT with and without CYP and GEM. (ND) denotes none detected and (NS), not significant. The data represents five mice per group. *p<0.05 in comparison to respective untreated controls.
Granulocytic MDSCs enhance the immune response against Nb
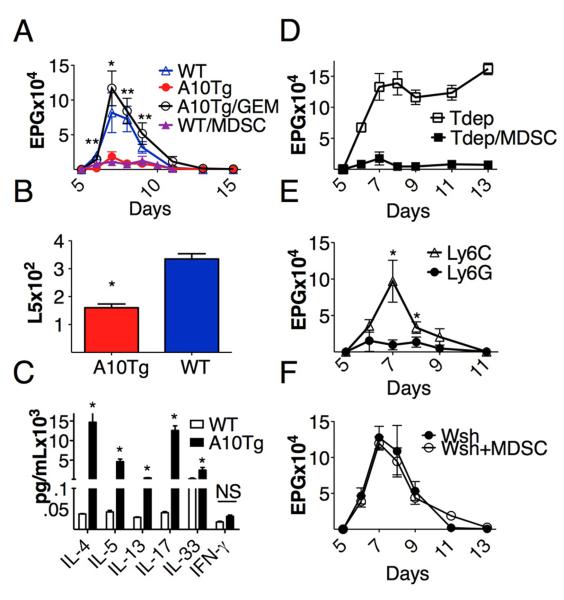
Next, we examined the effect of MDSCs on the immune response in anti-parasite immunity. While MDSC accumulation following Nb infection has been reported(11), the direct immunomodulatory role of MDSCs in anti-Nb responses has not been examined. In Nb infection, a WT response is characterized by production of Th2 associated cytokines that ultimately mediate adult worm (L5) clearance 10-12 days post-inoculation(21). Following Nb challenge, A10Tg animals had significantly reduced fecal egg counts compared to WT controls (Fig. 2A). This is highly correlated with 50 percent reduction in L5 burden in A10Tgs (Fig 2B). This indicated that MDSCs may facilitate parasite clearance. To determine if the increased worm clearance was correlated with an increase in Th2 cytokines, we examined a panel of Th2 cytokines. Analysis of peak infection (day 7) serum levels of IL-4, IL-5 and IL-13 demonstrated significantly enhanced levels in Nb infected A10Tg animals as compared to infected LM (Fig. 2C). Additionally IL-17 and IL-33, which have been reported to recruit MDSCs, were also elevated in serum of A10Tg mice(9, 22). These serum cytokines then decreased as infection began to decline (data not shown).
Figure 2. A10Tg mice are resistant to Nb infection.
(A) Eggs/gram feces were determined at indicated times in WT and A10Tg mice as well as A10Tgs treated with GEM or WT with adoptive transfer (AT) of MDSCs upon infection with 650 Nb L3 worms. (B) WT and A10Tg mice were examined on day seven for adult worm recovery as described in Methods. (C) Serum was collected at day seven and analyzed for the above cytokines using a Milliplex Mouse Cytokine Kit. *p<0.05 in comparison to infected WT controls. (D) Eggs/gram feces of WT mice with MDSC AT or WT controls, both depleted of T cells as described in methods. (E) Enumerated eggs/gram of feces of infected WT with AT of either CD11b+Ly6highLy6Clow or CD11b+Ly6lowLy6Chigh population of MDSCs. (F) Enumerated eggs/gram feces of mast cell deficient KitWsh/Wsh mice with and without MDSCs upon infection with 650 Nb L3 worms. The data represents five mice per group.
To determine whether enhanced Nb clearance is dependent on MDSC-activity, MDSCs were depleted from A10Tg mice. GEM treatment resulted in elevated egg counts in A10Tg mice similar to WT levels (Fig. 2A). Additionally, Nb-infection resulted in a modest 4-5 fold increase in MDSCs in WT spleens from day 0 to day 14. This level of WT MDSCs is sufficient to promote Nb clearance and prevent a chronic infection. However, GEM-mediated MDSC depletion in WT mice significantly exacerbated the peak level of Nb infection. (Data not shown). Taken together, the data indicates that the enhanced immune response in A10Tgs is a consequence of elevated MDSC levels. Next, to eliminate off target effects of GEM, A10Tg MDSCs were purified and adoptively transferred to WT mice over the course of Nb infection. Like the MDSCs that were observed accumulating following Nb-infection, the transferred MDSCs also comprised both Ly-6G+ and Ly6C+ populations. AT of MDSCs resulted in significantly reduced egg counts, comparable to A10Tgs (Fig. 2A). To determine which MDSC subset was responsible for this observation, MDSCs were purified based upon Ly6G and Ly6C expression and AT into WT Nb infected mice. The Ly6Ghigh population had the same effect as total Gr-1+ purified MDSCs while the AT Ly6Chigh had no effect. This indicates that the granulocytic population of MDSCs mediates the anti-Nb immunity (Fig. 2E). The direct of role of MDSCs was further supported in WT mice that were T cell depleted. These mice exhibited the same rapid rate of clearance as WT AT/MDSC experiment (Fig 2A). As expected, Nb clearance was significantly slower in T depleted WT without AT of MDSCs (Fig. 2D).
MCs are required for MDSC mediated Nb clearance
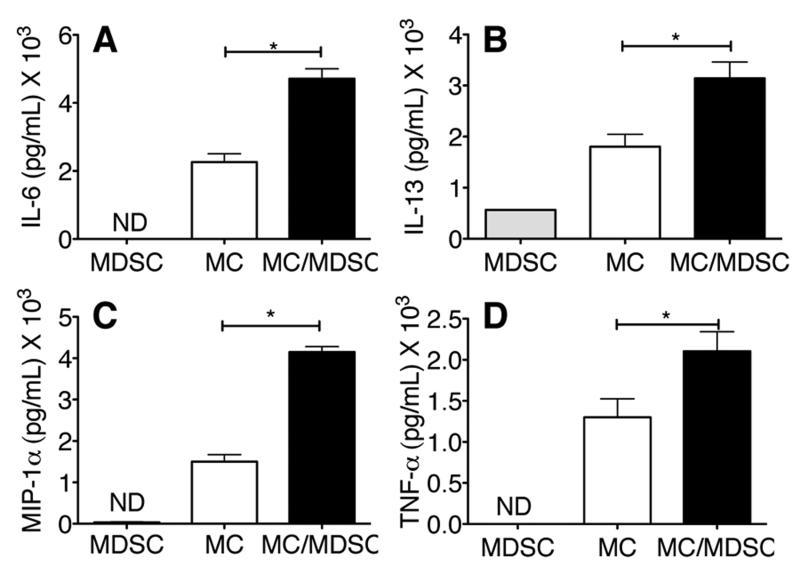
Mucosal MC hyperplasia is a hallmark of gastrointestinal helminth infection which enhances the immune response, leading to parasite clearance(23,24). Mice deficient in MCs exhibit delayed clearance kinetics(25). Given that MCs mainly produce Th2 polarizing and pro-inflammatory cytokines and that MCs chemoattract MDSCs, we examined whether the interaction between the two cell types could be contributing to the enhanced Nb expulsion. Surprisingly, AT of MDSCs into MC deficient mice did not enhance Nb expulsion, indicating that a MDSC/MC interaction is critical for MDSC-mediated anti-Nb responses (Fig. 2F). To assess this interaction ex vivo, MCs were co-cultured with MDSCs. This resulted in synergistic increase of IL-6, IL-13, TNF-μ and MIP-1μ (Fig. 3).
Figure 3. Mast cell/MDSC interaction augments cytokine production.
BMMCs were co-cultured with A10Tg MDSCs as described in Methods. Supernatants were collected and analyzed for the production of (A) IL-6, (B) IL-13, (C) MIP-1μ, and (D) TNF-μ. The data represents pooled spleens of at least three mice per group. *p<0.05 in comparison to mast cells (MCs) alone.
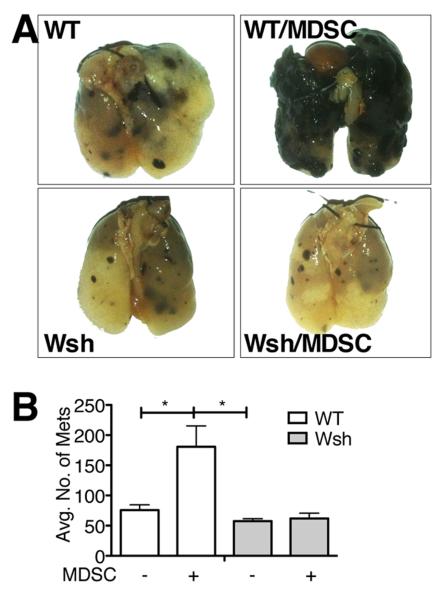
MCs also contribute to MDSC mediated-immune suppression in B16 melanoma
Given that MDSCs require MCs to enhance anti-Nb immunity, the B16 metastasis study was reevaluated in MC deficient mice. Several groups have demonstrated that MCs recruit MDSCs, which accumulate in the tumor microenvironment and correlate with poor prognosis. In addition, MC-deficient mice have decreased rates of tumor growth that increases to WT levels subsequent to MC reconstitution.(26). Therefore, we anticipated that B16 melanoma cells would metastasize slower in KitWsh/Wsh compared to WT controls but would be enhanced with MDSC AT. KitWsh/Wsh and WT mice were injected with B16 with and without AT of MDSCs. WT mice were more susceptible to B16 metastasis compared to KitWsh/Wsh. Upon MDSC AT, WT mice exhibited similar levels of tumor nodules as B16 A10Tgs, indicating the direct contribution of MDSCs to the immune response. However, much to our surprise, adoptive transfer of MDSCs into KitWsh/Wsh mice failed to increase B16 metastasis (Fig. 4A,B). Thus, these results demonstrate that MDSCs promote B16 melanoma metastasis in a MC-dependent manner and indicate that MDSC/MC interactions significantly enhance the MDSC-mediated suppression of antitumor immunity.
Figure 4. MC/MDSC interaction is required for MDSC-mediated immune suppression.
Photographic representation (A) and quantification (B) of B16 lung metastasis in control C57 and KitWsh/Wsh mice with and without the AT of MDSCs. The data is representative of with at least five mice per group. *p<0.05 in comparison to WT alone or KitWsh/Wsh with MDSCs.
The A10Tg mouse affords a unique tool to characterize the immune-modulatory potential of MDSCs in an environment free of established tumor. As the A10Tgs suffer no confounding pathology, this was an ideal system to elucidate the immunomodulatory roles of MDSCs. We used this system to investigate roles for MDSCs in both neoplasia and helminth infection. In B16 metastasis, monocytic MDSCs strongly suppressed the immune response while granulocytic MDSCs failed to promote metastasis. However, in Nb infection, the granulocytic MDSCs enhanced the anti-parasitic immune response and the monocytic MDSCs had no effect. AT studies demonstrated that this differential immune regulation by MDSCs occurs in a MC-dependent manner. The ex vivo co-culture studies indicate that MDSC/MC interactions may modulate immune responses by increasing cytokine production. MDSCs traffic to MCs, affording a synergistic Th2 skewed immune response. While undesirable in the context of neoplasia, the observed response is ideal in helminth infections. Overall our data indicate that inhibition of MC function may serve as a novel target to inhibit MDSC activity.
Supplementary Material
ACKNOWLEDGEMENTS
We thank Natalie Allen, Suzanne Barbour, Madiha Laiq, and Kahley Stanco for technical assistance.
This work was supported by NIH grants RO1AI19697 and U19AI077435, Project 2 to DHC and F31CA159877 to SJS.
REFERENCES
- 1.Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat. Rev. Immunol. 2009;9:162–174. doi: 10.1038/nri2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ostrand-Rosenberg S. Myeloid-derived suppressor cells: more mechanisms for inhibiting antitumor immunity. Cancer Immunol. Immunother. 2010;59:1593–1600. doi: 10.1007/s00262-010-0855-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cuenca AG, Delano MJ, Kelly-Scumpia KM, Moreno C, Scumpia PO, Laface DM, Heyworth PG, Efron PA, Moldawer LL. A paradoxical role for myeloid-derived suppressor cells in sepsis and trauma. Mol. Med. 2011;17:281–292. doi: 10.2119/molmed.2010.00178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bronte V, Apolloni E, Cabrelle A, Ronca R, Serafini P, Zamboni P, Restifo NP, Zanovello P. Identification of a CD11b(+)/Gr-1(+)/CD31(+) myeloid progenitor capable of activating or suppressing CD8(+) T cells. Blood. 2000;96:3838–3846. [PMC free article] [PubMed] [Google Scholar]
- 5.Narita Y, Wakita D, Ohkur T, Chamoto K, Nishimura T. Potential differentiation of tumor bearing mouse CD11b+Gr-1+ immature myeloid cells into both suppressor macrophages and immunostimulatory dendritic cells. Biomed. Res. 2009;30:7–15. doi: 10.2220/biomedres.30.7. [DOI] [PubMed] [Google Scholar]
- 6.Pastuła A, Marcinkiewicz J. Myeloid-derived suppressor cells: a double-edged sword? Int J Exp Pathol. 2011;92:73–78. doi: 10.1111/j.1365-2613.2010.00754.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oldford SA, Haidl ID, Howatt MA, Leiva CA, Johnston B, Marshall JS. A critical role for mast cells and mast cell-derived IL-6 in TLR2-mediated inhibition of tumor growth. J. Immunol. 2010;185:7067–7076. doi: 10.4049/jimmunol.1001137. [DOI] [PubMed] [Google Scholar]
- 8.Huang B, Lei Z, Zhang G-M, Li D, Song C, Li B, Liu Y, Yuan Y, Unkeless J, Xiong H, Feng Z-H. SCF-mediated mast cell infiltration and activation exacerbate the inflammation and immunosuppression in tumor microenvironment. Blood. 2008;112:1269–1279. doi: 10.1182/blood-2008-03-147033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang Z, Zhang B, Li D, Lv M, Huang C, Shen G-X, Huang B. Mast cells mobilize myeloid-derived suppressor cells and Treg cells in tumor microenvironment via IL-17 pathway in murine hepatocarcinoma model. PLoS ONE. 2010;5:e8922. doi: 10.1371/journal.pone.0008922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheon EC, Khazaie K, Khan MW, Strouch MJ, Krantz SB, Phillips J, Blatner NR, Hix LM, Zhang M, Dennis KL, Salabat MR, Heiferman M, Grippo PJ, Munshi HG, Gounaris E, Bentrem DJ. Mast cell 5-lipoxygenase activity promotes intestinal polyposis in APCDelta468 mice. Cancer Res. 2011;71:1627–1636. doi: 10.1158/0008-5472.CAN-10-1923. [DOI] [PubMed] [Google Scholar]
- 11.Van Ginderachter JA, Beschin A, De Baetselier P, Raes G. Myeloid-derived suppressor cells in parasitic infections. Eur. J. Immunol. 2010;40:2976–2985. doi: 10.1002/eji.201040911. [DOI] [PubMed] [Google Scholar]
- 12.Gibb DR, Saleem SJ, Kang D-J, Subler MA, Conrad DH. ADAM10 overexpression shifts lympho- and myelopoiesis by dysregulating site 2/site 3 cleavage products of Notch. J. Immunol. 2011;186:4244–4252. doi: 10.4049/jimmunol.1003318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Le HK, Graham L, Miller CHT, Kmieciak M, Manjili MH, Bear D. Incubation of antigen-sensitized T lymphocytes activated with bryostatin 1 + ionomycin in IL-7 + IL-15 increases yield of cells capable of inducing regression of melanoma metastases compared to culture in IL-2. Cancer Immunol. Immunother. 2009;58:1565–1576. doi: 10.1007/s00262-009-0666-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lipshy KA, Kostuchenko PJ, Hamad GG, Bland CE, Barrett SK, Bear HD. Sensitizing T-lymphocytes for adoptive immunotherapy by vaccination with wild-type or cytokine gene-transduced melanoma. Ann. Surg. Oncol. 1997;4:334–341. doi: 10.1007/BF02303584. [DOI] [PubMed] [Google Scholar]
- 15.Camberis M, Le Gros G, Urban J. Animal model of Nippostrongylus brasiliensis and Heligmosomoides polygyrus. Curr Protoc Immunol. 2003 doi: 10.1002/0471142735.im1912s55. Chapter 19. Unit 19.12. [DOI] [PubMed] [Google Scholar]
- 16.Peranzoni E, Zilio S, Marigo I, Dolcetti L, Zanovello P, Mandruzzato S, Bronte V. Myeloid-derived suppressor cell heterogeneity and subset definition. Curr. Opin. Immunol. 2010;22:238–244. doi: 10.1016/j.coi.2010.01.021. [DOI] [PubMed] [Google Scholar]
- 17.Hanson EM, Clements VK, Sinha P, Ilkovitch D, Ostrand-Rosenberg S. Myeloid-derived suppressor cells down-regulate L-selectin expression on CD4+ and CD8+ T cells. J. Immunol. 2009;183:937–944. doi: 10.4049/jimmunol.0804253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bracci L, Moschella F, Sestili P, La Sorsa V, Valentini M, Canini I, Baccarini S, Maccari S, Ramoni C, Belardelli F, Proietti E. Cyclophosphamide enhances the antitumor efficacy of adoptively transferred immune cells through the induction of cytokine expression, B-cell and T-cell homeostatic proliferation, and specific tumor infiltration. Clin. Cancer Res. 2007;13:644–653. doi: 10.1158/1078-0432.CCR-06-1209. [DOI] [PubMed] [Google Scholar]
- 19.Teitz-Tennenbaum S, Li Q, Davis MA, Wilder-Romans K, Hoff J, Li M, Chang AE. Radiotherapy combined with intratumoral dendritic cell vaccination enhances the therapeutic efficacy of adoptive T-cell transfer. J. Immunother. 2009;32:602–612. doi: 10.1097/CJI.0b013e3181a95165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Le HK, Graham L, Cha E, Morales JK, Manjili MH, Bear HD. Gemcitabine directly inhibits myeloid derived suppressor cells in BALB/c mice bearing 4T1 mammary carcinoma and augments expansion of T cells from tumor-bearing mice. Int. Immunopharmacol. 2009;9:900–909. doi: 10.1016/j.intimp.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 21.Else KJ, Finkelman FD. Intestinal nematode parasites, cytokines and effector mechanisms. Int. J. Parasitol. 1998;28:1145–1158. doi: 10.1016/s0020-7519(98)00087-3. [DOI] [PubMed] [Google Scholar]
- 22.Perrigoue JG, Marshall FA, Artis D. On the hunt for helminths: innate immune cells in the recognition and response to helminth parasites. Cell. Microbiol. 2008;10:1757–1764. doi: 10.1111/j.1462-5822.2008.01174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Turnquist HR, Zhao Z, Rosborough BR, Liu Q, Castellaneta A, Isse K, Wang Z, Lang M, Beer Stolz D, Zheng XX, Demetris AJ, Liew FY, Wood KJ, Thomson AW. IL-33 Expands Suppressive CD11b+ Gr-1int and Regulatory T Cells, including ST2L+ Foxp3+ Cells, and Mediates Regulatory T Cell-Dependent Promotion of Cardiac Allograft Survival. J. Immunol. 2011;187:4598–4610. doi: 10.4049/jimmunol.1100519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miller HR. Mucosal mast cells and the allergic response against nematode parasites. Vet. Immunol. Immunopathol. 1996;54:331–336. doi: 10.1016/s0165-2427(96)05696-6. [DOI] [PubMed] [Google Scholar]
- 25.Mitchell LA, Wescott RB, Perryman LE. Kinetics of expulsion of the nematode, Nippostrongylus brasiliensis, in mast-cell deficient W/WV mice. Parasite Immunol. 1983;5:1–12. doi: 10.1111/j.1365-3024.1983.tb00718.x. [DOI] [PubMed] [Google Scholar]
- 26.Starkey JR, Crowle PK, Taubenberger S. Mast-cell-deficient W/Wv mice exhibit a decreased rate of tumor angiogenesis. Int. J. Cancer. 1988;42:48–52. doi: 10.1002/ijc.2910420110. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.