Abstract
The use of anticancer drugs in palliative settings is often limited by their severe toxic effects. In gastrointestinal carcinomas the 5-fluorouracil-based palliative regimen FOLFOX-4 is often preferred to the equally effective, but more convenient oral capecitabine-based regimen XELOX. This preference is mainly based on the fact that the highly effective oral agent capecitabine induces hand-foot syndrome (HFS). In this study, we investigated whether the continuous administration of skin prophylaxis (10% urea, panthenol, bisabolol, vitamin A, C and E) is capable of protecting against capecitabine-induced HFS and allowing a more convenient oral therapeutic option. In this retrospective analysis, the toxicity profiles, according to NCI CTCAE 3.0 criteria, of 54 patients with gastrointestinal cancer who received either XELOX (34 patients) or FOLFOX-4 (20 patients) were compared using Fisher tests. The treatment protocols that were compared, herein, did not differ significantly in the majority of the analyzed items, with the exception of increased nausea (XELOX-70), fatigue (XELOX-130) and tumor pain (XELOX-70 and XELOX-130). No significant differences were observed among the various groups with regard to emesis, diarrhea, mucositis, exanthema, alopecia, loss of weight and the incidence of infections. In particular, no significant differences in toxicity levels occurred in terms of dose, and HFS was limited if skin prophylaxis was performed continuously. XELOX-based palliative regimens provide an equally effective and comparably toxic therapeutic alternative to FOLFOX-4 if HFS prophylaxis is performed continuously. Since the oral administration of capecitabine is a more convenient method of application, it provides patients with a quality of life-preserving therapeutic alternative.
Keywords: capecitabine, 5-fluorouracil, hand-foot syndrome, gastrointestinal carcinoma
Introduction
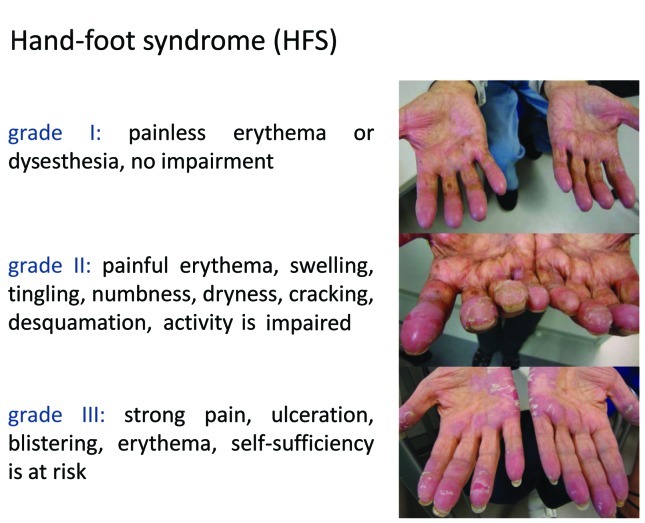
Palmar-plantar erythrodysesthesia, or hand-foot syndrome (HFS), is a common side-effect in patients receiving long-term 5-fluorouracil (5-FU) treatment and is the most frequently reported side effect of oral capecitabine therapy (≥50% of patients), often leading to the disruption of treatment (Fig. 1). Essentially two pathogenic mechanisms of HFS are discussed: The damage of deep capillaries in the soles of the feet and palms of the hands may lead to a COX inflammatory-type reaction. HFS may also be related to enzymes involved in the metabolism of capecitabine, such as thymidine phosphorylase and dihydropyrimidine dehydrogenase (1).
Figure 1.
Hand-foot syndrome (HFS).
In gastrointestinal carcinomas, palliative combination treatments with 5-FU/oxaliplatin (FOLFOX-4) and capecitabine/oxaliplatin (XELOX) are commonly administered. These treatments may improve quality of life and prolong overall survival (2,3). Recent studies have shown an equal efficacy of the two regimens (4–6). However, dose-limiting toxicities are an important factor in treatment choice. FOLFOX-4 is often preferred to the more convenient oral capecitabine-based regimen XELOX due to the quality of life-limiting toxicity induced by the highly effective oral agent capecitabine, particularly HFS (7). Yet, patients developing clinical signs of HFS under administration of capecitabine show an improved overall survival (data provided by Hoffmann-La Roche AG). The administration of infusional FOLFOX-4 regimens can be inefficient, since it requires indwelling catheters, infusion supplies, nursing visits and a significantly higher rate of outpatient treatment contacts and hospitalization (8).
In this retrospective analysis, we compared toxicities according to NCI CTCAE 3.0 criteria in three groups of patients, who received either FOLFOX-4 or XELOX regimens under continuous skin prophylaxis.
Materials and methods
Patient selection
A total of 54 adult patients (>18 years of age) with metastatic or unresectable gastrointestinal cancer were treated with standard combination therapy protocols. Patients with prior surgical intervention were excluded as well as patients with an Eastern Cooperative Oncology Group (ECOG) performance status >2. The patients received treatment over at least six months. Any toxicity during treatment was documented. Patients receiving capecitabine had access to skin prophylaxis, which was performed with a cream consisting of 10% urea, panthenol, bisabolol and vitamin A, C and E. Tumor entities per treatment group are shown in Table I.
Table I.
Tumor entities per treatment group.
| XELOX-70 (Group A) | XELOX-130 (Group B) | FOLFOX-4 (Group C) | |
|---|---|---|---|
| Entity | |||
| Colorectal cancer | 15 | 14 | 12 |
| Cholangiocellular cancer | 0 | 1 | 2 |
| Gastric cancer | 1 | 2 | 3 |
| Esophageal cancer | 1 | 0 | 3 |
Treatment plan
In this study, three groups of patients were compared concerning their toxicity profiles according to NCI CTCAE 3.0 criteria. Group A (17 patients, median age 67, 59% male/41% female) and group B (17 patients, median age 66, 59% male/41% female) received the combination regimen XELOX: Group A received capecitabine 2000 mg/m2 on days 1–14, oxaliplatin 70 mg/m2 on days 1 and 8, q22; group B received capecitabine 2000 mg/m2 on days 1–14, oxaliplatin 130 mg/m2 on day 1, q22. Group C (20 patients, median age 62, 60% male/40% female) received the combination regimen FOLFOX-4 (oxaliplatin 85 mg/m2 day 1, fluorouracil 400 mg/m2 on days 1 and 2 bolus, fluorouracil 600 mg/m2 and folic acid 200mg/m2 infusional on days 1 and 2, q14).
Data mining and statistical methods
The files of the patients matching the inclusion criteria were retrospectively analyzed. The outpatient clinic used a standardized visit protocol containing the relevant adverse events (AEs) graded according to CTCAE 3.0. Thus, AEs are routinely documented at each visit. All graded AEs that occurred during the therapy were transferred into an Excel sheet and analyzed by SPSS 15.0.
The Fisher test was used to compare the treatment groups in terms of significant differences in toxicities. A difference was considered significant when p=0.05.
Results
In total, 54 patients with a stage IV gastrointestinal tumor according to UICC were enrolled in the present study. Of these, 41 patients had a colorectal; three, cholangiocellular; six, gastric and four, esophageal cancer (Table I). None of the patients had a preceding surgical therapy. Patients were either treated with XELOX-70, XELOX-130 or FOLFOX-4 (see Materials and methods). Patients received repeated courses of chemotherapy over a period of at least six months. The different groups were monitored for the occurrence of side effects during the whole period of treatment (>6 months); any toxicity that occurred was documented. Side effects were analysed according to CTCAE 3.0 (Table II) and their significance (Table III) was evaluated using the Fisher test (see Materials and methods).
Table II.
Side effects and toxicities associated with XELOX-70, XELOX-130 and FOLFOX-4.
| XELOX-70 | XELOX-130 | FOLFOX-4 | |
|---|---|---|---|
| n | 17 | 17 | 20 |
| Median age (years) | 66,72 | 67,24 | 61,68 |
| Toxicity according to CTC (%) | |||
| Fatigue (grade) | |||
| 0 | 24 | 0 | 40 |
| 1/2 | 52 | 76 | 40 |
| 3/4 | 24 | 24 | 20 |
| 1–4 | 76 | 100 | 60 |
| Nausea (grade) | |||
| 0 | 18 | 41 | 55 |
| 1/2 | 76 | 41 | 35 |
| 3/4 | 6 | 18 | 10 |
| 1–4 | 82 | 59 | 45 |
| Emesis (grade) | |||
| 0 | 41 | 65 | 65 |
| 1/2 | 41 | 24 | 30 |
| 3/4 | 18 | 11 | 5 |
| 1–4 | 59 | 35 | 35 |
| Diarrhea (grade) | |||
| 0 | 29 | 52 | 55 |
| 1/2 | 65 | 41 | 40 |
| 3/4 | 6 | 6 | 5 |
| 1–4 | 59 | 35 | 35 |
| Mucositis (grade) | |||
| 0 | 48 | 52 | 50 |
| 1/2 | 52 | 48 | 45 |
| 3/4 | 0 | 0 | 5 |
| 1–4 | 52 | 48 | 50 |
| Exanthema (grade) | |||
| 0 | 59 | 70 | 85 |
| 1/2 | 41 | 30 | 10 |
| 3/4 | 0 | 0 | 5 |
| 1–4 | 41 | 30 | 15 |
| HFS (grade) | |||
| 0 | 59 | 48 | 45 |
| 1/2 | 30 | 48 | 50 |
| 3/4 | 11 | 6 | 5 |
| 1–4 | 41 | 54 | 55 |
| Paresthesia (grade) | |||
| 0 | 18 | 6 | 25 |
| 1/2 | 70 | 83 | 65 |
| 3/4 | 11 | 11 | 10 |
| 1–4 | 81 | 94 | 75 |
| 1–4 | 35 | 17 | 30 |
| Pain (grade) | |||
| 0 | 24 | 30 | 60 |
| 1/2 | 70 | 65 | 30 |
| 3/4 | 6 | 6 | 10 |
| 1–4 | 76 | 71 | 40 |
| Alopecia (grade) | |||
| 0 | 59 | 70 | 75 |
| 1/2 | 41 | 30 | 25 |
| 3/4 | 0 | 0 | 0 |
| 1–4 | 41 | 30 | 25 |
| Loss of weight (grade) | |||
| 0 | 65 | 70 | 85 |
| 1/2 | 35 | 30 | 15 |
| 3/4 | 0 | 0 | 0 |
| 1–4 | 35 | 30 | 15 |
| Infections (grade) | |||
| 0 | 65 | 83 | 70 |
| 1/2 | 11 | 11 | 30 |
| 3/4 | 24 | 6 | 0 |
The side effects in percentages observed using the mentioned chemotherapy regimens and their severity according to CTC are shown. HFS, hand-foot syndrome.
Table III.
Comparison of side effects.
| XELOX-70 vs. XELOX-130 | XELOX-130 vs. FOLFOX-4 | XELOX-70 vs. FOLFOX-4 | |
|---|---|---|---|
| Fatigue (grade) | |||
| 1/2 | 0.141 | 0.028 | 0.324 |
| 3/4 | 0.656 | 0.553 | 0.553 |
| 1–4 | 0.404 | 0.003 | 0.239 |
| Nausea (grade) | |||
| 1/2 | 0.040 | 0.481 | 0.013 |
| 3/4 | 0.301 | 0.420 | 0.562 |
| 1–4 | 0.420 | 0.306 | 0.022 |
| Emesis (grade) | |||
| 1/2 | 0.232 | 0.474 | 0.357 |
| 3/4 | 0.500 | 0.438 | 0.242 |
| 1–4 | 0.076 | 0.627 | 0.132 |
| Diarrhea (grade) | |||
| 1/2 | 0.151 | 0.603 | 0.121 |
| 3/4 | 0.758 | 0.715 | 0.715 |
| 1–4 | 0.062 | 0.581 | 0.109 |
| Mucositis (grade) | |||
| 1/2 | 0.500 | 0.581 | 0.440 |
| 3/4 | n.e. | n.e. | n.e. |
| 1–4 | 0.324 | 0.560 | 0.560 |
| Exanthema (grade) | |||
| 1/2 | 0.360 | 0.140 | 0.034 |
| 3/4 | n.e. | n.e. | n.e. |
| 1–4 | 0.243 | 0.254 | 0.350 |
| PPE (grade) | |||
| 1/2 | 0.241 | 0.560 | 0.175 |
| 3/4 | 0.500 | 0.715 | 0.438 |
| 1–4 | 0.540 | 0.581 | 0.524 |
| Paresthesia (grade) | |||
| 1/2 | 0.344 | 0.209 | 0.498 |
| 3/4 | 0.699 | 0.633 | 0.633 |
| 1–4 | 0.596 | 0.130 | 0.447 |
| Pain (grade) | |||
| 1/2 | 0.500 | 0.037 | 0.016 |
| 3/4 | 0.758 | 0.562 | 0.562 |
| 1–4 | 0.239 | 0.062 | 0.028 |
| Alopecia (grade) | |||
| 1/2 | 0.360 | 0.526 | 0.243 |
| 3/4 | n.e. | n.e. | n.e. |
| 1–4 | 0.243 | 0.526 | 0.147 |
| Loss of weight (grade) | |||
| 1/2 | 0.500 | 0.254 | 0.147 |
| 3/4 | n.e. | n.e. | n.e. |
| 1–4 | 0.373 | 0.254 | 0.128 |
| Infections (grade) | |||
| 1/2 | 0.699 | 0.174 | 0.174 |
| 3/4 | 0.147 | n.e. | n.e. |
| 1–4 | 0.147 | 0.315 | 0.502 |
Comparison of side effects among the used chemotherapy regimens XELOX-70, XELOX-130 and FOLFOX-4. Differences in the grade of toxicity were considered significant using the Fisher test when reaching a maximum p value of p<0.05. PPE, palmar-plantar erythrodysesthesia; n.e., not evaluable.
When comparing XELOX-70 with XELOX-130, no significant differences were observed besides a light nausea grade 1/2, which was more frequent in the XELOX-70 group (P=0.04).
When the Xelox-130 group was compared with the FOLFOX-4 group, significantly more fatigue was observed in the XELOX-130 group (grade 1/2 P=0.028, any grade P=0.003), as well as more pain (grade 1/2 P=0.037, any grade P=0.062).
XELOX-70 as compared to FOLFOX-4 resulted in more nausea (grade 1/2 P=0.013; any grade P=0.022) and more pain (grade 1/2 P=0.016, any grade P=0.028).
No significant difference was observed among the different groups with regard to emesis, diarrhea, mucositis, exanthema, HFS, alopecia, loss of weight and the incidence of infections.
Discussion
The ultimate aim of treatment regimens available for patients with advanced tumor diseases in a palliative setting is to attenuate the severity of tumor symptoms without compromising the quality of life immoderately. Therefore, the incidence and severity of side effects associated with different treatment options are the most important criteria for the choice of regimen offered to the patient, as side effects largely affect the patients’ convenience and compliance. The treatment protocols that were compared herein did not differ significantly in their tolerance in the majority of the analyzed items, with the exception of nausea (XELOX-70), fatigue (XELOX-130) and tumor pain (XELOX-70 and XELOX-130). In the study by Cassidy et al these three items did not differ significantly either. The safety data similarly suggest that the profile of adverse events of XELOX and FOLFOX-4 regimens are similar. However, differences in the frequencies at which they occurred were described. XELOX was associated with more grade 3 diarrhea, whereas FOLFOX-4 was associated with more grade 3/4 neutropenia (7).
However, the occurrence of HFS, which often leads to a discontinuation of treatment on the part of patients, showed no significant difference among the three presented groups. This observation is in contrast to larger clinical trials comparing the efficacy of FOLFOX-4 versus XELOX, and thereby also comparing the associated side effects, and may result from the HFS prophylaxis applied in the capecitabine group (9). The XELOX regimen was associated with a higher frequency and severity of diarrhea, thrombocytopenia and HFS, whereas FOLFOX-4 was associated with more grade 3/4 neutropenia. However, as it was shown that the efficacies of the different treatment regimens are equivalent in metastatic gastrointestinal tumors (9–14), the use of an oral chemotherapeutic regimen is certainly more comfortable for outpatients and thus certainly positively influences the compliance of patients.
In conclusion, the oral administration of capecitabine and the application schedule of XELOX is clearly more convenient than that of FOLFOX-4 and equally tolerable concerning HFS if a HFS prophylaxis is applied.
References
- 1.Saif MW. Capecitabine and hand-foot syndrome. Expert Opin Drug Saf. 2011;10:159–169. doi: 10.1517/14740338.2011.546342. [DOI] [PubMed] [Google Scholar]
- 2.Glimelius B, Hoffman K, Graf W, Påhlman L, Sjödén PO. Quality of life during chemotherapy in patients with symptomatic advanced colorectal cancer. Cancer. 1994;73:556–562. doi: 10.1002/1097-0142(19940201)73:3<556::aid-cncr2820730310>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 3.Tournigand C, Andre T, Achille E, et al. FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GERCOR study. J Clin Oncol. 2004;22:229–237. doi: 10.1200/JCO.2004.05.113. [DOI] [PubMed] [Google Scholar]
- 4.Van Cutsem E, Hoff PM, Harper P, et al. Oral capecitabine vs intravenous 5-fluorouracil and leucovorin: integrated efficacy data and novel analyses from two large, randomized, phase III trials. Br J Cancer. 2004;90:1190–1197. doi: 10.1038/sj.bjc.6601676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cao Y, Liao Y, Tan A, Liu L, Mo Z, Gao F. Capecitabine plus oxaliplatin vs fluorouracil plus oxaliplatin as first line treatment for metastatic colorectal cancer – meta-analysis of six randomized trials. Colorectal Disease. 2010;12:16–23. doi: 10.1111/j.1463-1318.2009.01803.x. [DOI] [PubMed] [Google Scholar]
- 6.Ducreux M, Bennouna J, Hebbar M, Ychou M, Lledo G, Conroy T, Adenis A, Faroux R, Rebischung C, Bergougnoux L, Kockler L, Douillard J. For the GI Group of the French Anti-Cancer Centers (FNCLCC): Capecitabine plus oxaliplatin (XELOX) versus 5-fluorouracil/leucovorin plus oxaliplatin (FOLFOX-6) as first-line treatment for metastatic colorectal cancer. Int J Cancer. 2010;128:682–690. doi: 10.1002/ijc.25369. [DOI] [PubMed] [Google Scholar]
- 7.Cassidy J, Tabernero J, Twelves C, et al. XELOX (capecitabine plus oxaliplatin): active first-line therapy for patients with metastatic colorectal cancer. J Clin Oncol. 2004;22:2084–2091. doi: 10.1200/JCO.2004.11.069. [DOI] [PubMed] [Google Scholar]
- 8.Cassidy J, Douillard JY, Twelves C, et al. Pharmacoeconomic analysis of adjuvant oral capecitabine vs intravenous 5-FU/LV in Dukes’ C colon cancer: the X-ACT trial. Br J Cancer. 2006;94:1122–1129. doi: 10.1038/sj.bjc.6603059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arkenau HT, Arnold D, Cassidy J, Diaz-Rubio E, Douillard JY, Hochster H, Martoni A, Grothey A, Hinke A, Schmiegel W, Schmoll HJ, Porschen R. Efficacy of oxaliplatin plus capecitabine or infusional fluorouracil/leucovorin in patients with metastatic colorectal cancer: a pooled analysis of randomized trials. J Clin Oncol. 2008;26:5910–5917. doi: 10.1200/JCO.2008.16.7759. [DOI] [PubMed] [Google Scholar]
- 10.Cassidy J, Clarke S, Diaz-Rubio E, et al. Randomized phase III study of capecitabine plus oxaliplatin as first-line therapy for metastatic colorectal cancer. J Clin Oncol. 2008;26:2006–2012. doi: 10.1200/JCO.2007.14.9898. [DOI] [PubMed] [Google Scholar]
- 11.Van Cutsem E, Twelves C, Cassidy J, et al. Oral capecitabine compared with intravenous fluorouracil plus leucovorin in patients with metastatic colorectal cancer: results of a large phase III study. J Clin Oncol. 2001;19:4097–4106. doi: 10.1200/JCO.2001.19.21.4097. [DOI] [PubMed] [Google Scholar]
- 12.Rothenberg ML, Cox JV, Butts C, Navarro M, Bang YJ, Goel R, Gollins S, Siu LL, Laguerre S, Cunningham D. Capecitabine plus oxaliplatin (XELOX) versus 5-fluorouracil/folinic acid plus oxaliplatin (FOLFOX-4) as second-line therapy in metastatic colorectal cancer: a randomized phase III noninferiority study. Annals of Oncology. 2008;19:1720–1726. doi: 10.1093/annonc/mdn370. [DOI] [PubMed] [Google Scholar]
- 13.Hoff PM, Ansari R, Batist G, et al. Comparison of oral capecitabine versus intravenous fluorouracil plus leucovorin as first-line treatment in 605 patients with metastatic colorectal cancer: results of a randomized phase III study. J Clin Oncol. 2001;19:2282–2292. doi: 10.1200/JCO.2001.19.8.2282. [DOI] [PubMed] [Google Scholar]
- 14.Twelves C, Scheithauer W, McKendrick J, Seitz JF, Van Hazel G, Wong A, Díaz-Rubio E, Gilberg F, Cassidy J. Capecitabine versus 5-fluorouracil/folinic acid as adjuvant therapy for stage III colon cancer: final results from the X-ACT trial with analysis by age and preliminary evidence of a pharmacodynamic marker of efficacy. Ann Oncol. 2011 Sep 6; doi: 10.1093/annonc/mdr366. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]