Summary
In recent decades there has been an increase in upper limb prosthetic surgery, primarily for the shoulder, for osteoarthritis disease and for traumatic pathology. It is occurring in parallel an increase in periprosthetic fractures of the humerus, although with less impact than other anatomical districts such as the hip.
We report a case of humeral periprosthetic refracture in a 66-years-old female patient.
The humerus bone quality is worse than in other districts in patient of the same age.
The fragility humerus fracture are increasing, affecting relatively younger individuals than those with femoral neck fractures and represent an independent risk factor for the occurrence of subsequent fractures.
Actually humeral BMD is underestimated by traditional densitometric evaluation techniques.
Keywords: periprosthetic fracture, shoulder prosthesis, osteoporosis
Introduction
The prosthetic scapular-humeral joint replacement surgery, after the first attempts dating back to the end of the last century, has met with widespread use in recent years, thanks to the improvement of the models used and which are characterized by large modularity, for importance of their adaptation to changes in anatomical and biomechanical characteristics of the particular articulation of this complex. The endoprosthesis is indicated for a vascular necrosis of the humeral head and for fractures of the proximal humerus and nonunion. The total prosthesis is to be reserved for serious gleno-humeral arthropathies, rheumatoid arthritis and failures of a previous endoprostheses, while the mid-eighties has been gradually developing the innovative method of reverse prostheses for which they are valid signs of serious impairment of the components of articular cuff lesions (cuff arthropathy), and in selected cases of fractures of the proximal third of humerus (1). Some studies have shown that the incidence of periprosthetic fracture in the shoulder is 0.6 to 3% (2, 3).
In the literature there are few works on this subject: those we learn that the most significant predisposing factors for these types of fractures are female sex, osteopenia and osteoporosis, advanced age, rheumatoid arthritis and comorbidities (4). Furthermore, it appears that often in periprosthetic fractures, especially of the humeral shaft, complications are intraoperative (5). The incidence of these complications is increasing (6). Periprosthetic fractures represent 25% of all complications of total shoulder arthroplasty, despite an overall decrease (12%) of complications compared to revision multicentric (31%) of the first 5 years (7).
Fractures can be intraoperative (59%) and postoperative (41%) (8).
There are various classification of periprosthetic fractures. The Worland classification is based on the anatomy of the fracture and the inherent stability of the implant: type A fractures occur about the tuberosities, type B fractures occur about the stem and are sub-classified by fracture anatomy and implant stability (B1 fractures are spiral fractures with a stable implant, B2 fractures are transverse or short oblique fractures about the tip of the stem with a stable implant, and B3 fractures are those fractures about the stem with an unstable implant), type C fractures occur well distal to the tip of the stem.
According to Wright and Cofield periprosthetic humeral fractures are classified as type A (around prosthesis tip with proximal extension), type B (around prosthesis tip with no or minimal proximal extension and variable distal extension), and type C (distal to the tip).
Campbell et al. categorized fractures into one of four region: region 1 included the greater or lesser tuberosities, region 2 the proximal metaphysis, region 3 the proximal humeral diaphysis and region 4 the mid and distal diaphysis (9).
Case Report
In this paper the authors present a case of periprosthetic refracture of the humerus.
It is a 66 years old female patient with hypertension, hyperglycemia, concentric shoulder arthritis and overweight; in June 2010 underwent to prosthetic surgery of the right shoulder with resurfacing prosthesis for concentric osteoarthritis of the glenohumeral joint (Durom TM cup).
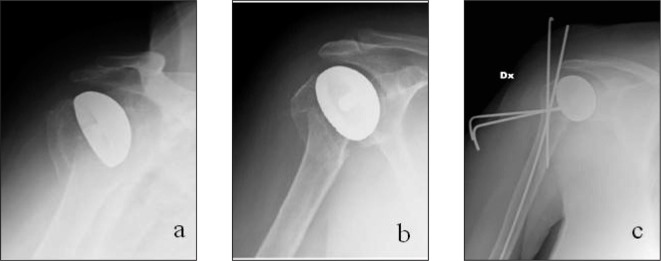
In June 2010, twenty days after the first surgery, the patient fell down causing a periprosthetic fracture (type 2 Campbell) of the humerus (Figure 1a, 1b) treated with osteosynthesis with K-wires (Figure 1c) and immobilization for 30 days followed by a rehabilitation phase. The classification of the periprostethic fracture in this case refers to that Campbell because it is a resurfacing prosthesis without stem.
Figure 1 a, b, c.
Radiograph of periprosthetic fracture and post-operative after synthesis.
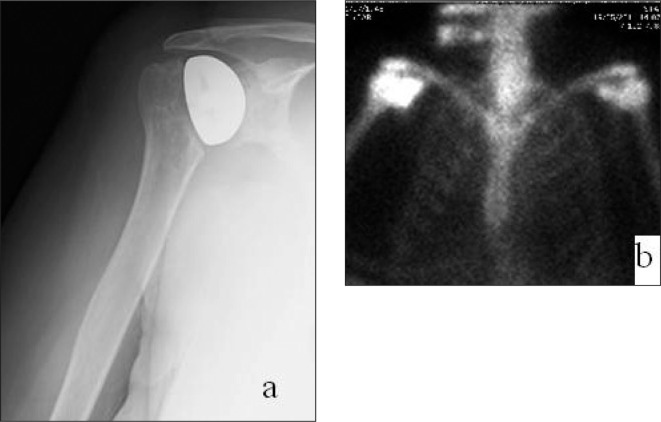
However the patient complained of a worsening of pain for which has been subjected to X-ray studies (Figure 2a), CT scans and scintigraphic investigations (Figure 2b) that showed a mobilization of the implant.
Figure 2 a, b.
a) Radiographic evaluation shows the consolidation of the fracture. b) Scintigraphic image compatible with the mobilization of the implant.
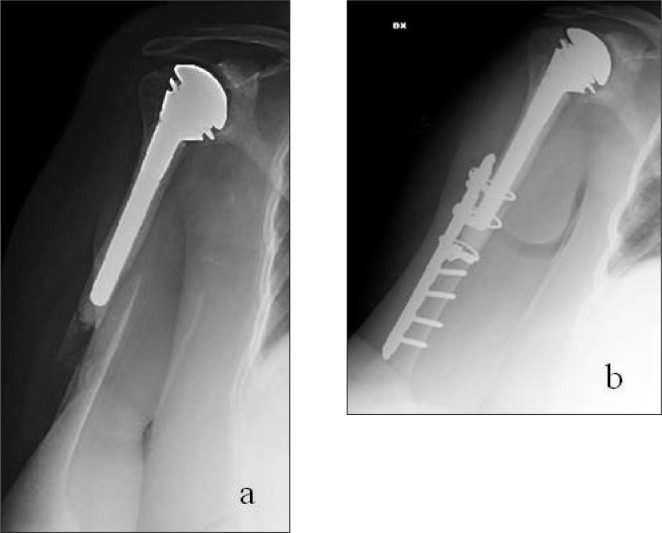
In October 2011 underwent a prosthetic reimplantation of the right shoulder with cemented hemiarthroplasty (Bigliani) (Figure 3). In November 2011, the patient fell down again by getting a new periprosthetic fracture (type B2 Worland) (Figure 4a).
Figure 3.

Radiograph after prosthetic explantation and reimplantation.
Figure 4 a, b.
a) Radiograph after new periprosthetic fracture. b) Postoperative X-Ray after surgical synthesis of the fracture.
We evaluate the radiographic images that show the stability of the prosthesis.
The fracture is treated with reduction and fixation with plate, screws and cerclage (Figure 4b).
During the hospitalization, the patient is being subjected to densitometric investigation (showed that bone density values in the range, the limits osteopenia), evaluation of the humeral cortical index that was decreased and first level blood tests for osteoporosis (which were in the range, except for a hypovitaminosis).
Discussion
The case presented is particular because characterized by two subsequent periprosthetic fractures treated with osteosynthesis in two different types of prosthesis (with and without stem). The clinical case leads us to make some considerations.
The humerus bone quality is worse than in other districts in patient of the same age (10).
The fragility humerus fractures are increasing (20% osteoporosis fractures) (11), affecting relatively younger individuals than those with femoral neck fractures and represent an independent risk factor for the occurrence of subsequent fractures.
Humerus fracture increases by 6 times the risk of the fracture of the femural neck at 12 months (12).
However it is difficult to estimate the humeral bone mineral density and use effective drugs on the humerus.
Actually humeral BMD is underestimated by traditional densitometric evaluation techniques (9). Instead it would be desirable the use of a standardized and easily executable humeral bone densitometric evaluation technique.
The number of periprosthetic fractures in shoulder is steadily increasing. The modularity of the systems is indispensable for the management of the problem. Any doubt on the stability of the prosthesis requires a strategy of revision-reprosthesization.
References
- 1.Pisani A, et al. La chirurgia protesica nelle gravi artropatie gleno omerali degenerative e traumatiche. Acta Orthopaedica Italica. 2009;34 [Google Scholar]
- 2.Boyd AD, Thornhill TS, Barnes CL. Fractures adjacent to humeral prosthesis. J Bone Joint Surg Am. 1992;74:1498–504. [PubMed] [Google Scholar]
- 3.Worland RJ, Kim DY, Arredondo J. Periprosthetic humeral fractures: management and classification. J Shoulder Elbow Surg. 1999;8:590–4. doi: 10.1016/s1058-2746(99)90095-2. [DOI] [PubMed] [Google Scholar]
- 4.Steinmann SP, Cheung EV. Treatment of periprosthetic humerus fractures associated with shoulder arthroplasty. J Am Acad Orthop Surg. 2008 Apr;16(4):199–207. doi: 10.5435/00124635-200804000-00003. [DOI] [PubMed] [Google Scholar]
- 5.McDonough EB, Crosby LA. Periprosthetic fractures of the humerus. Am J Orthop. 2005;34(12):586–591. [PubMed] [Google Scholar]
- 6.Williams GR, Jr, Iannotti JP. Management of periprosthetic fractures: the shoulder. J Arthroplasty. 2002;17(4 suppl 1):14–16. doi: 10.1054/arth.2002.32683. [DOI] [PubMed] [Google Scholar]
- 7.Chin PJ, Sperling JW, Cofield RH, et al. Complications of total arthroplasty: are they fewer or different? J Shoulder Elbow Surgery. 2006;15:19–22. doi: 10.1016/j.jse.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 8.Kumar S, Sperling JW, Haidukewych GH, Cofield RH. Periprosthetic humeral fractures after shoulder arthroplasty. JBJS Am. 2004;86:680–9. doi: 10.2106/00004623-200404000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Bucholz RW, Heckman JD. Rockwood and Green’s fractures in adult. 1:579–583. [Google Scholar]
- 10.Wilson J, Bonner TJ, Head M, Fordham J, Brealey S, Rangan A. Variation in bone mineral density by anatomical site in patients with proximal humeral fractures. J Bone Joint Surg Br. 2009;91:772–775. doi: 10.1302/0301-620X.91B6.22346. [DOI] [PubMed] [Google Scholar]
- 11.Calvo E. Non displaced proximal humeral fractures: high incidence among outpatient-treated osteoporotic fractures and severe impact on upper extremity function and patient subjective health perception. J Shoulder Elbow Surg. 2010 Jul;:795–801. doi: 10.1016/j.jse.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 12.Clinton J, Franta A, Polissar NL, et al. Proximal humeral fracture as a risk factor for subsequent hip fractures. JBJS Am. 2009;91(3):503–511. doi: 10.2106/JBJS.G.01529. [DOI] [PMC free article] [PubMed] [Google Scholar]