Summary
Background:
osteoporosis, depression and other neuro-psychiatric disorders are very common after 50 years of age. Although these conditions recognize several and specific etiologic factors, they however appear to share physiologic, environmental processes and risk factors which may explain their possible association.
Methods:
we have built up a specific research project (the CODE study, Connections between the outcomes of osteoporotic hip fractures and depression, delirium or dementia in elderly patients), and carried out a preliminary survey on 55 hip fractured elderly patients (42 women, mean age 85 years old and 13 men, mean age 82 years old), hospitalized at SS. Annunziata hospital in Florence from July to September 2010.
Results:
there was a significant difference (p=0.010) in the functional recovery after surgery (as measured by Cumulated Ambulation Score, CAS) between depressed and non-depressed subjects (n=38), with a worse recovery and a lower CAS score in depressed patients (n=17). We also observed a higher prevalence of depression in the osteoporotic-fragile elderly people (69,1% of total sample).
Conclusion:
our preliminary survey has validated the suitability of the CODE study protocol in assessing connections between outcomes of osteoporotic hip fractures and depression in elderly patients, fostering the extension of the study (and suggesting also the inclusion of delirium and dementia) within a multicentric prospective study aimed to provide specific information and guidelines for osteoporotic fractured patients with concomitant depression or other neuro-psychiatric disorders.
Keywords: osteoporosis, depression, hip fracture, elderly, neuro-psychiatric disorders, depression
Introduction
It is known that osteoporosis is a condition that enhances the risk of fracture, especially vertebral and hip fractures (1). Each year in Italy, almost 18,000 elderly people become completely disabled as a consequence of hip fractures, resulting in inestimable human suffering and substantial social costs (1). Hip fractures have a 5% acute mortality rate and 15–25% 1-year mortality (1). Furthermore, once hip fracture has occurred, the ability to walk is completely lost in 20% of cases, and only 30–40% of patients recover a degree of autonomy comparable to the period before the fracture (1, 2). Many studies have focused on identifying risk factors for falls and fractures, besides the search for correlations between these risk factors and osteoporosis (2, 3).Particularly in the elderly, recognized risk factors for falls are: muscle weakness, history of falls, impaired balance, visual impairment, arthritis, impaired activities of daily living, depression, cognitive deficits, and age over 80 years (3). Risk factors for osteoporosis-related fractures are: age, osteoarthritis, disability prior to fracture, malnutrition (3). Also depression is considered one of the conditions possibly relating to osteoporotic fractures (3, 4). In a recent review, it is reported the association between low bone mineral density and presence of depression itself. Compared with the normal population, people with depression have higher levels of specific biomarkers such as alkaline phosphatase, parathyroid hormone, pro-inflammatory cytokines (IL-1beta, IL-2, IL-6, TNF-alpha) and low levels of cytokines anti-inflammatory IL-13 (4–7).
Depression is also associated with an increased risk of falling and fracture (8). Depression may increase the risk of fracture due to direct effects on physiology (elevated levels of cortisol, cytokines), or because of the changes of behavior resulting in reduced sun exposure (with a consequent reduction in vitamin D levels) or physical activity (3, 6, 8). Furthermore, depression is thought itself to increase the risk of falls due to somatic symptoms such as fatigue (8). Taking antidepressants, antipsychotics, anticonvulsants and benzodiazepines, often prescribed to depressed patients, additionally increase the risk of falls and fractures in the elderly (8). TCA and SSRI antidepressants, in particular, are recognized for their cardiovascular, anticholinergic and histaminergic effects (8). Some studies suggest that SSRIs have some action in reducing bone mineral density due to their effect on reuptake of serotonin (7). Other studies have looked into the relationship between cognitive impairment and hip fracture in the elderly (9, 10). The presence of cognitive impairment before the fracture is clearly a risk factor for fracture, mainly as it makes more likely the fall.
On these bases, we have built up a specific research protocol (the CODE study, (Connections between outcomes of osteoporotic hip fractures and depression, delirium or dementia in elderly patients), which has started on January 12, 2012 at “Careggi” University Hospital (Florence, Italy), with the approval of the local ethical committee. Through this study, we are aimed to observe and describe as closely as possible the impact, etiology and clinical course of depression and neuropsychiatric disorders occurred as a result of hip fracture in elderly patients or pre-existing to the fracture event. We also would like to improve our knowledge concerning functional outcomes of fractured patients after an appropriate multimodal treatment (surgery/drugs/rehabilitation) addressing concurrent mood disorders. The data collected might be potentially useful for identifying and developing new diagnostic and therapeutic approaches to offer elderly patients with cognitive impairment, delirium and/or depression experiencing a hip fracture, in order to improve the functional outcome and quality of life (10, 11).
Methods
Study Protocol
Primary objectives of the CODE study are to evaluate the relationship between osteoporotic fractures, depression and cognitive impairment in elderly patients through (a) the analysis of the incidence of depression, delirium, cognitive impairment/dementia, including neurodegenerative, Parkinson’s and Parkinson-like diseases, before (correlation with the risk of falls and fractures) and after the femoral fracture’s event of the elderly (correlation with outcomes); (b) prospective analysis of functional outcomes and mortality in patients with hip fracture in the presence of (cases) and without (controls) depression, delirium and/or cognitive impairment/dementia, including neurodegenerative, Parkinson’s and Parkinson-like diseases. Specific secondary objectives are to assess the relationship between osteoporotic fractures, depression and cognitive impairment in elderly patients through: (c) the analysis of the incidence of falls and fractures in patients with these concurrent disorders; (d) the analysis of the prevalence of other minor fractures before and after hip fractures in patients with these concurrent disorders; (d) analysis of the cause of neuropsychiatric disorders observed in hip fractured patients, with particular attention to the role of time between fracture and surgery, postoperative complications, the role of pain (i.e., in determining delirium), and the family/social environment. The study protocol consists in an observational study without pharmacological interventions (non interventional trial). Inclusion criteria implies the enrollment of consecutive patients aged 65 years and older with hip fracture supposed to be a consequence of osteoporosis (fragility fracture determined by low energy trauma) hospitalized at departments of orthopedics/orthogeriatrics. Only after assessments on depressive status, all patients with a diagnosis of previous diagnosis (in history) of cognitive impairment or dementia will be excluded. As major exclusion criteria we have considered all pathological fractures (consequences of cancers), revision of femoral prosthesis, fractures determined by car accidents or accidents occurred at workplace (supposed to result from high-energy trauma) and violence; diagnosis of amiothrophic lateral sclerosis (ALS), muscular dystrophy, Huntington’s disease, multiple sclerosis, tumors with life expectancy < 6 months, concurrent facial trauma fractures, alcohol addiction, serious hearing or vision impairment. The protocol implies that for each enrolled patient with hip fracture it must be recorded, on a specific sheet, all relevant anamnestic data: education level, concurrent conditions, previous fractures events, previous falls (number and circumstances of the fall), presence of stairs, architectural barriers, obstacles or pets in the house, Bone Mineral Density measures, current therapies for osteoporosis, list of medications (with focus on Central Nervous System-active drugs), details about the time elapsed between fracture and surgery, the type and dose of anesthetic used, therapies administered to reduce pain (drug, dosage and time elapsed between fracture and treatment administration). Under the protocol, all data are treated anonymously, by assigning numerical codes. A preliminary survey, limited only to depressed patients, has been carried out from July to September 2010 on 55 hip fractured elderly patients (42 women, mean age 85 years old, and 13 men, mean age 82 years old).
Data Analysis
Functional outcomes and mortality represent the independent variables of multivariate analysis for testing the presence of depression, delirium, cognitive impairment dementia, Parkinson’s disease and Parkinson-like conditions, neurodegenerative diseases, severe postoperative complications, and as a function of time elapsed between fracture and surgery and any pain therapies administered. Functional outcomes and mortality are compared within the population of patients with hip fracture in presence (cases) or absence (controls) of mood/cognitive individual disorders (e.g. depression, delirium, cognitive impairment). Data collected will be subjected to inferential statistical tests, including ANCOVA analysis of covariance.
Scale scores and parameters
The study protocol implies the evaluation of each patient during the first 4 days after surgery by administering the following tests:
– Mini Mental State Examination (MMSE), for the evaluation of the cognitive status;
– Geriatric Depression Scale (GDS), for the evaluation of the Current depressive symptoms;
– Confusion Assessment Method (CAM), to evaluate an acute confusing state (delirium);
– Barthel Index, to assess the ability to perform activities of daily living;
– Modified Blaylock Risk Assessment Score (Brass Index), for social fragility;
– Questionnaire for the assessment of housing and social network of the patient;
– Cumulated Ambulation Score (CAS), for the assessment of functional recovery;
– Verbal and numerical scale (NRS/VRS) for the determination of pre-and post-operative pain;
– 25-OH vitamin D value (subgroup of patient);
– Serum albumin value (subgroup of patients) as an indicator of malnutrition;
– Hemoglobin value (subgroup of patients): anemia as a prognostic factor on the recovery.
Mini Mental State Examination (MMSE)
The MMSE is a tool developed for the assessment of cognitive status and it is definitely one of the most widely used test in clinical practice because of its simplicity, short duration of administration, reproducibility and high sensitivity (12–14). It consists of 11 items that include verbal and nonverbal tests and should evaluate various cognitive areas: orientation in time and space, short-term memory, concentration, long-term memory, language and engineering practice. In each test, when properly performed, are scored for a maximum of 30 points; a score between 30 and 24 is considered normal, 20 to 24 border line, below 20 indicative of cognitive impairment, minor of 14 suggestive of cognitive impairment in older people. The test cannot be performed in patients with severe vision and hearing disease and must be applied some corrective for the normalization of the results by age and educational level of the patient (15).
Geriatric Depression Scale (GDS)
This is a scale for detecting depressive symptoms (12–14), consisting of 30 items that provide an alternative answer (yes/no). The dimensions assessed include: cognitive symptoms, motivation, orientation to past and future, self-image, loss, agitation, obsessive traits, mood. It assigns one point for each answer in the direction of pathology. In general, it is considered normal values up to 10, values from 11 to 17 are considered indicative of mild depression, and above 18 severe depression (15).
Center for Epidemiological Studies - depression scale (CES-d)
This is a questionnaire of 20 questions that, although developed for population studies, is particularly useful in the assessment of depressive symptoms of elderly subjects (12–14). To the examined subject it is asked how often in recent times has experienced the situations listed in the questionnaire. The possible answers are 4, from “never or almost never” (<1 day), to “always or almost always” (5–7 days). The total score is between 0 and 60. The threshold value of 16 is considered to indicate patients with mild depression compared to normal subjects, and the value of 23 or higher indicating clinical depression (15).
Confusion Assessment Method (CAM)
This is a test for assessing the presence of acute confusing state (delirium). It consists of a questionnaire and a treatment algorithm and takes into account 9 evaluation criteria: sudden changes in mental status, impaired attention, disorganized thinking, altered level of consciousness, disorientation, impaired memory, altered perception, psychomotor agitation and retardation, abnormal sleep wake rhythm (16).
Pain assessment scales (NRS e VRS)
Pain is unpleasant sensory and emotional experience associated with tissue potential or perceived (described) damage. Scales of assessment should support an objective and comparable reading of the care phenomena, a uniform and quali-quantitative assessment of patient care, exchange of information between different disciplines. The scales define the intensity of pain (how much pain), quality (what kind of pain) and its location. For this study, the numerical rating scale (VRS) and verbal (VRS) are both useful (17).
Barthel Index
This test is widely used in the assessment of disability; it is characterized by excellent reliability and validity. It consists of 10 items that assess the subject’s autonomy in activities such as eating, bathing, personal hygiene care, sphincter control, move to the bathroom, transferring from bed to chair and vice-versa, ambulate and climb stairs. The total score can range from 0 (totally dependent) to 100 (totally independent) (18).
Blaylock Risk Assessment Screening Score (BRASS Index)
The Brass Index is a tool used to identify patients at risk of prolonged hospitalization and/or difficult discharge. We investigated 10 variables including: age, life situation and social support, functional status, cognitive status, behavioral model, mobility, sensory deficits, number of previous hospitalizations/emergency room access, number of active medical problems and number of drugs taken (19). Through the score obtained, the patients are divided into three groups: low risk (0–10), medium risk (11–19) and high risk (> 20). Patients enrolled in this study were administered the Brass questionnaire only with respect to the size of living conditions, which were further characterized by administering other questions relating to housing and social network.
Cumulated Ambulation Score (CAS)
The Cumulated Ambulation Scores (CAS) is a tool specifically designed to assess physical recovery during the first three days following hip surgery (20, 21). The CAS describes the ability of the patient in the performance of three specific functions: to go in and out of bed, sit and rise from a chair, walking with adequate human support. For each function is assigned a score that is 2 for patients able to perform the function alone, 1 for patients that need help, and 0 for those not able to function despite the assistance of the operator. The test runs for three days and each day the score is made up of individual scores for the three different functions that could vary between 0 and 6. The total score ranging from 0 to 18 is the sum of the individual scores of each day: the higher the score, the better the recovery of post-surgical patient. The reliability and predictive validity of rehabilitation on outcome of the CAS has been established in specific studies on patients with hip fracture (22). This test represents the tool trough which functional outcomes after hip fractures are evaluated.
Results
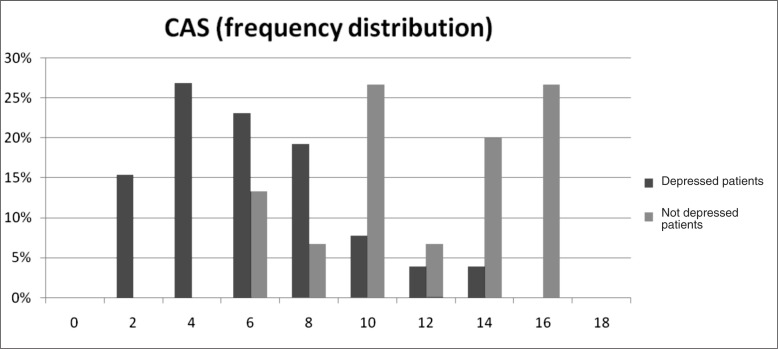
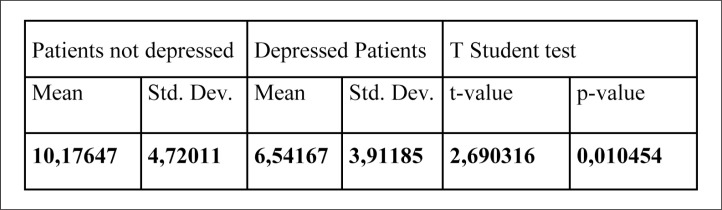
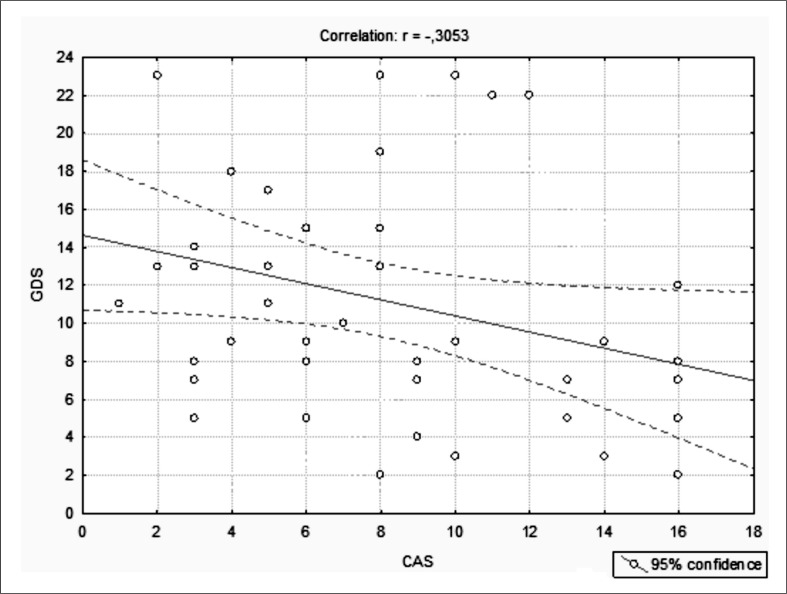
Our preliminary research carried out in 2010 on 55 hip fractured elderly patients (42 women, mean age 85 years old, and 13 men, mean age 82 years old) has shown a high prevalence of depression among hip fractured patients (69,1% of total sample). There was a statistically significant difference (p=0.010) in functional outcomes after surgical intervention – measured by the Cumulated Ambulation Score (CAS) – between depressed patients (n=38) and patients who were not depressed (n=17). Figure 1 and 2 show that depressed subjects had a worse functional recover as measured by CAS (lower scores). Dependence between CAS score and depression has been demonstrated with a high statistical significance (p-value=0.001), as showed in Figure 2. ANCOVA analysis of covariance has demonstrated that depression status investigated as single variable was able to significantly modify the CAS scores, whose values were inversely related to depression status (measured by CES-d scale), with a 95% confidential interval (Figure 3).
Figure 1.
CAS scores and frequency distribution according to depression status.
Figure 2.
Significant difference in terms of functional recover between depressed and not depressed patients (T student test).
Figure 3.
CAS scores (functional recover) and CES-d (depression status) are inversely related.
Discussion
This study represents a first attempt to address the issue of the incidence and course of neuropsychiatric disorders (depression, cognitive impairment, delirium) (12–14) occurring in elderly patients hospitalized because of hip fracture, both before and after the fracture event, taking also into account the possible origin of these disorders and a paying particular attention to functional outcomes after adequate multimodal interventions (surgery, drug treatments and rehabilitation). Givens et al. (23) have recently published a study on the prevalence of depressive symptoms, cognitive impairment and delirium in elderly patients with hip fractures, in order to evaluate how these disorders may affect the healing, the institutionalization probability and the “exitus” after surgery. Among 126 patients aged over 65 years, 22% of them had only one of the three above mentioned neuropsychiatric conditions (depressive symptoms, cognitive impairment or delirium); 30% of fractured patients were affected by two of these conditions, and 7% had all three the diseases. These neuropsychiatric disorders resulted in a significant reduction in functional outcomes, whether present individually or combined together. An early intervention in contrasting these disorders guarantees, according to the authors, a reduction in the risk of adverse outcomes. However, there is still the need to explore the impact of depression, delirium and cognitive impairment on the medium and long-term mortality after hip fracture. Clinical experience also suggests that many elderly patients, after hip fracture, develop a neuropsychological status characterized by cognitive impairment in the absence of pre-existing problems.
Also the presence of cognitive deficits prior to fracture (possibly frequent in elderly patients), also leads to a reduction of functional outcome and quality of life after the fracture has occurred, with an increased risk of subsequent fractures. Most studies focused on the influence of cognitive impairment on functional outcomes in the elderly patients after hip fracture. Other researchers have studied possible effect of simultaneous presence of cognitive impairment and depressive symptoms on functional recovery in elderly patients with hip fractures, but also the impact of depressive symptoms on functional outcomes after hip fracture (degree of physical recovery), an investigation area that still remains largely unexplored. Few authors have focused on neuropsychological changes resulting from hip fractures in the elderly. Bruggemann et al. (5) and Lenze et al. (6) have identified an increased probability of anxiety or mood disorders onset after hip fracture in the elderly. Vibeke et al. (10) have focused on the prevalence of pre-and post-operative delirium after hip fracture in elderly patients, suggesting that fractures may represent a major risk factor for the onset of this disorder. According to these authors, the prevalence of pre-operative delirium was 21.1% with post-operative incidence rising to 36.4%. These figures were confirmed by a recent review that included 1.832 patients with hip fracture, which reported an average incidence of 35%. It seems that a pre-existing cognitive impairment, accidents at home, fever and a prolonged time to the surgical intervention may all re-present risk factors for the onset of pre-operative delirium (5, 6, 10).
Possible risk factors for postoperative delirium have been suggested: low bone density, pre-existing cognitive deficit, home accidents, old age, pre-existing functional impairment and institutionalization. The role of pain and the lack of effective treatments for this symptom needs also to be investigated. Jane et al. evaluated the prevalence of cognitive impairment before hip fracture, the depressive symptoms eventually present immediately after the fracture and delirium diagnosed during hospitalization (3). These authors have analyzed the importance of the effects of these individual or combined disorders on functional outcomes, on probability of post-fracture institutionalization, and mortality after surgery (3). The study showed that 59% of patients with hip fractures had a mood disorder or a cognitive impairment (pre-existing or arising after the event), and that these disorders increased the likelihood of an adverse outcome: a reduced score on activity of daily living (ADL) assessment, a deficit in walking ability, the need for institutionalization, and death (3).
Dementia syndromes are acquired brain diseases causing the decline of intellectual abilities and overall impairment of higher capacities (such as language, praxis, and the ability of abstraction), thus resulting in impairment of social life (12–14). Dementia is divided into: 1) acute, subacute or chronic; 2) regularly or irregularly progressive or non progressive; 3) reversible, partially reversible or irreversible (24). The other condition of particular interest is the depression-related pseudo-dementia, which arises when patients simultaneously fulfill the diagnostic criteria of DSM-IV TR (13) both for major depression (25), and for dementia (24). In these patients it can be detected: impaired memory, impaired concentration ability, reduced cognitive capacity, usually associated with listlessness, apathy, motor slowing, abnormal gait and speech, confusion. Often the neuropsychological tests may be compromised. The CODE study involves both patients positive to the association between cognitive decline and depressive symptom (pseudodementia), and those presenting exclusively depressive symptoms. In the elderly, it must also kept in mind that a depressive episode can arise with dysphoria, agitation, anxiety, somatic complaints and hypochondriacal concerns. From a pathogenetic point of view, depression in the elderly may be determined by stressful events such as retirement (with the loss of professional role), economic difficulties, the death of a spouse or social isolation (25–27). The characteristics of frailty, complexity and instability that are typical of the frail elderly must be also taken into account, because processes of accelerated physical and mental decay that, once triggered, tends to progress in these kind of patients (23).
Conclusions
Based on these positive preliminary results, correlation between the outcomes of osteoporotic hip fractures and depression, delirium and dementia in elderly patients will be further investigated at University of Florence in a specific clinical study (the CODE study), whose results will be available by the end of 2013.
References
- 1.Rizzoli R, et al. Management of osteoporosis in the elderly. Current medical Research and Opinion. 2009;25(10):2373–2387. doi: 10.1185/03007990903169262. [DOI] [PubMed] [Google Scholar]
- 2.Bradley D, et al. Recurrent and Injurious Falls in the Year Following Hip Fracture: A Prospective Study of Incidence and Risk Factors From the Sarcopenia and Hip Fracture Study. Journal of Gerontology: Medical Sciences. 2009;64A(5):599–609. doi: 10.1093/gerona/glp003. [DOI] [PubMed] [Google Scholar]
- 3.Jane L, et al. Functional Recovery After Hip Fracture: The Combined Effects of Depressive Symptoms, Cognitive Impairment, and Delirium. Journal American Geriatrics Society. 2008;56:1075–1079. doi: 10.1111/j.1532-5415.2008.01711.x. [DOI] [PubMed] [Google Scholar]
- 4.Haney EM, et al. Skeletal effects of serotonin (5-hydroxytryptamine) transporter inhibition: Evidence from clinical studies. Review Article, Journal Musculoskelet Neuronal Interact. 2008;8(2):133–145. [PubMed] [Google Scholar]
- 5.Bruggemann L, et al. Predicting acute anxiety and depression following hip fracture. Journal Behavioral Medicine. 2007;30:97–105. doi: 10.1007/s10865-006-9088-x. [DOI] [PubMed] [Google Scholar]
- 6.Lenze EJ, et al. Onset of depression in elderly persons after hip fracture: implications for prevention and early intervention of late-life depression. Journal American Geriatrics Society. 2007;55:81–86. doi: 10.1111/j.1532-5415.2006.01017.x. [DOI] [PubMed] [Google Scholar]
- 7.Gijsbertus Z, et al. Selective Serotonin Reuptake Inhibiting Antide-pressants Are Associated With an Increased Risk of Nonvertebral Fractures. Journal of clinical psychopharmacology. 2008 Aug;28(4):411–417. doi: 10.1097/JCP.0b013e31817e0ecb. [DOI] [PubMed] [Google Scholar]
- 8.Cizza G, et al. Depression as a risk factor for osteoporosis. Trend in Endocrinology and Metabolism. 30(10) doi: 10.1016/j.tem.2009.05.003. article in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laekeman G, et al. Osteoporosis after combined use of a neuroleptic and antidepressants. Pharm World Sci. 2008;30:613–616. doi: 10.1007/s11096-008-9231-6. [DOI] [PubMed] [Google Scholar]
- 10.Vibeke J, et al. Risk Factors for Preoperative and Postoperative Delirium in Elderly Patients with Hip Fracture. Journal American Geriatrics Society. 2009;57:1354–1361. doi: 10.1111/j.1532-5415.2009.02377.x. [DOI] [PubMed] [Google Scholar]
- 11.Bitsch M, et al. Pathogenesis and management strategies for postoperative delirium after hip fracture: a review. Acta Orthop Scand. 2004 Aug;75(4):375–7. doi: 10.1080/00016470410001123. [DOI] [PubMed] [Google Scholar]
- 12.Trattato Italiano di Psichiatria, a cura di P. Pancheri e G.B. Cassano, Seconda Edizione 2002, Masson Ed.
- 13.DSM-IV-TR, Criteri Diagnostici, Quarta Edizione Italiana a cura di V. Andreoli, G.B. Cassano, R. Rossi, 2002, Masson Ed. [Google Scholar]
- 14.Cassano GB, Tundo A. 2006. Psicopatologia e clinica psichiatrica, Utet ed.
- 15.Conti L. Repertorio delle Scale di Valutazione in Psichiatria, collana “Progressi in Psichiatria”, ed. SEE, Firenze.
- 16.Inouye SK, et al. Clarifying confusion: The Confusion Assessment Method. A new method for detection of delirium. Ann. Intern. Med. 1990;113:941–8. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 17.Turk DC, et al. Chronic pain and depression: role of perceived impact control in different age cohorts. Pain. 1995;61:93–101. doi: 10.1016/0304-3959(94)00167-D. [DOI] [PubMed] [Google Scholar]
- 18.Mahoney FI, Barthel D. Functional evaluation: the Barthel Index. Maryland State Med. J. 1965;14:56–61. [PubMed] [Google Scholar]
- 19.Mistiaen P, et al. Predictive validity of the BRASS index in screening patients with post-discharge problems. Blaylock Risk Assessment Screening Score. J. Adv. Nurs. 1999 Nov;30(5):1050–6. doi: 10.1046/j.1365-2648.1999.01203.x. [DOI] [PubMed] [Google Scholar]
- 20.Foss NB, et al. Prediction of postoperative morbidity, mortality and rehabilitation in hip fracture patients: the cumulated ambulation score. Clin Rehabil. 2006 Aug;20(8):701–8. doi: 10.1191/0269215506cre987oa. [DOI] [PubMed] [Google Scholar]
- 21.Kristensen MT, et al. High intertester reliability of the cumulated ambulation score for the evaluation of basic mobility in patients with hip fracture. Clin Rehabil. 2009 Dec;23(12):1116–23. doi: 10.1177/0269215509342330. [DOI] [PubMed] [Google Scholar]
- 22.Kristensen MT, et al. High intertester reliability of the cumulated ambulation score for the evaluation of basic mobility in patients with hip fracture. Clin Rehabil. 2009 Dec;23(12):1116–23. doi: 10.1177/0269215509342330. [DOI] [PubMed] [Google Scholar]
- 23.Givens JL, et al. Functional recovery after hip fracture: the combined effects of depressive symptoms, cognitive impairment, and delirium. J Am Geriatr Soc. 2008 Jun;56(6):1075–9. doi: 10.1111/j.1532-5415.2008.01711.x. Epub 2008 Apr 18. [DOI] [PubMed] [Google Scholar]
- 24.Bellelli G, et al. Dementia, Delirium, and Depression in Patients with Hip Fracture: 1 + 1 doesn’t always make 2. Journal American Geriatrics Society. 2009;57:179–180. doi: 10.1111/j.1532-5415.2009.02068.x. [DOI] [PubMed] [Google Scholar]
- 25.Bellelli G, et al. Depressive symptoms combined with dementia affect 12-months survival in elderly patients after rehabilitation post-hip fracture surgery. International Journal of Geriatric Psychiatry. 2008;23:1073–1077. doi: 10.1002/gps.2035. [DOI] [PubMed] [Google Scholar]
- 26.Shyu Y-IL, et al. Severity of depression risk predicts health outcomes and recovery following surgery for hip-fractured elders. Osteoporos Int. 2008;19:1541–1547. doi: 10.1007/s00198-008-0592-4. [DOI] [PubMed] [Google Scholar]
- 27.Whitson HE, et al. Depressive symptomatology and fracture risk in community-dwelling older men and women. Aging Clin Exp Res. 2008 Dec;20(6):585–592. doi: 10.1007/bf03324888. [DOI] [PMC free article] [PubMed] [Google Scholar]