Abstract
Objectives
This study aimed to determine the frequency of dysmenorrhea, as identified by different definitions, in a population of young women, and to investigate factors associated with this complaint.
Materials and methods
A final group of 408 young women completed a self-assessment questionnaire. This was a cross-sectional analytical study.
Results
Menstrual pain was reported by 84.1% of women, with 43.1% reporting that pain occurred during every period, and 41% reporting that pain occurred during some periods. Women with menstrual pain had an earlier menarche (P = 0.0002) and a longer menstrual flow (P = 0.006), and this group was characterized as having a higher prevalence of smokers (P = 0.031) and a lower prevalence of hormonal contraception users (P = 0.015). Pain intensity was correlated (r = 0.302, P < 0.0001) positively with menstrual flow length (CR = 0.336), history of abortions (CR = 3.640), and gynecological pathologies (CR = 0.948), and negatively with age at menarche (CR = −0.225), use of hormonal contraception (CR = −0.787), and history of gynecological surgery (CR = −2.115). Considering the parameters of menstrual pain, a need for medication, and inability to function normally (absenteeism from study or social activities) alone or together, the prevalence of dysmenorrhea is 84.1% when considering only menstrual pain, 55.2% when considering the association between menstrual pain and need for medication, 31.9% when considering the association between menstrual pain and absenteeism, and 25.3% when considering the association between menstrual pain, need for medication, and absenteeism (P < 0.0001). The probability of having more severe dysmenorrhea is directly related to pain intensity as measured by a visual analog scale, but does not coincide with it.
Conclusion
Menstrual pain is a very common problem, but the need for medication and the inability to function normally occurs less frequently. Nevertheless, at least one in four women experiences distressing menstrual pain characterized by a need for medication and absenteeism from study or social activities.
Keywords: menstrual pain, dysmenorrhea, treatment, absenteeism
Introduction
Background
The terms “menstrual pain” and “dysmenorrhea” are commonly considered synonymous in clinical practice and literature. They indicate a cramp-like, dull, throbbing pain that usually emanates from the lower abdomen, and that occurs just before and/or during menstruation.1 Some authors suggest that a type of menstrual pain that is lighter than dysmenorrhea, called normal menstrual cramps, could exist.2,3 Dysmenorrhea seems to be associated with late4–6 or early7,8 menarche, prolonged and heavier than normal menstrual flow,9 low bodyweight and body mass index, inadequate physical exercise,10,11 genetic predisposition,12 active and passive cigarette smoking,9,13–15 low socioeconomic status, diet,5,16,17 stress, and mental illness.18
Dysmenorrhea appears to have an impact on public and occupational health,19,20 but its prevalence is unclear, with studies performed in different populations reporting rates of between 20% and 94%.4,5,21–27 This wide variation may derive from ethnic, sociocultural, or biological factors of the study populations,21–27 and also from the range of definitions of dysmenorrhea.
The proposed distinction between dysmenorrhea and normal menstrual cramps is “the need for medication and the inability to function normally in the latter situation.” A recent large-scale survey demonstrated that the reporting of painful periods was more common than the reporting of problematic periods,3 indicating that pain alone is not sufficient to make a period a clinical problem. Accordingly, categorizing dysmenorrhea on the basis of pain intensity using a visual analog scale (VAS)4,5 fails to consider a woman’s capacity to cope with pain, and so may not directly relate to the need for medication or the ability of a woman to function normally when suffering from dysmenorrhea.
Objectives
The principal aim of this study was to evaluate the prevalence of dysmenorrhea as identified by different definitions, and to demonstrate that rates and impacts of dysmenorrhea can vary significantly depending on the definition used. Factors associated with menstrual pain were also investigated.
The present study is reported according to the STROBE statement for improving the quality of observational studies (http://www.strobe-statement.org).
Materials and methods
Study design and setting
A cross-sectional analytical survey was carried out at the University of Modena and Reggio Emilia in April 2010. The study was approved by the internal review board of the Department of Obstetrics, Gynecology, and Pediatrics, Azienda Ospedaliero Universitaria Policlinico of Modena. Permission to distribute the questionnaires in university classrooms was obtained from the university.
A sample of academic years and the degree courses offered in different disciplinary areas (faculties of medicine, law, economy, and engineering) was randomly selected, and provided a total of 500 female students. Those who agreed to participate in the research were enrolled in the classroom prior to lessons, with participation being voluntary, and written consents gathered before any data was collected. A self-assessment questionnaire was anonymously completed by each participant.
Participants
The eligibility criteria for this study were:
All participants were female students enrolled in a randomly selected academic year of a degree course of the university.
Participants must have been present in the classroom when the researcher visited to collect data.
Informed consent was required for participation.
Data sources
The questionnaire was based on previous studies in the literature and the results of a pilot study.25 It comprised 26 questions investigating each participant’s menstrual pattern and specific personal, family, educational, physical, and gynecological factors.
Women who reported that they had suffered from menstrual pain completed an additional eleven questions regarding the onset of symptoms, length of pain, relation of pain with menstrual flow, pain intensity using a VAS, use and effectiveness of painkillers, and whether menstrual pain interfered with school or social activities.
Statistical methods
The characteristics of women with and without pain were analyzed and compared. Possible features related to menstrual pain were evaluated with independent factors defined by logistic regression analysis for categorical variables (dependent variable: presence/absence of menstrual pain) or multiple regression analysis for continuous variables (dependent variable: intensity of pain by VAS). In the multiple regression analysis, categorical data were entered as dummy variables. Sugar and salt consumption (minimal, moderate, excessive) and breakfast frequency (daily, 2/3 times a week, never) were entered into the analysis as two dummy variables, while the presence of a sentimental relationship, smoking, physical activity, coffee consumption, fish consumption, use of hormonal contraception, gynecological pathology and surgery in the participant’s medical history, and alcohol consumption were entered as a single dummy variable.
Prevalence of dysmenorrhea was calculated according to the association of different features and in accordance with the only definition reported in literature,2 in which dysmenorrhea is considered to be menstrual pain associated with a need for medication and inability to function normally. Accordingly, we evaluated the prevalence of menstrual pain per se, of menstrual pain associated with a need for medication, and of menstrual pain associated with an inability to function at, or absenteeism from, school or social events. Prevalence of a combination of the above parameters was also evaluated. Similarly, menstrual pain was stratified by VAS scores into mild, moderate, and severe categories, and their prevalence was calculated. When necessary, prevalence was compared by contingency tables and the Chi square test.
Statistical analysis was performed using the statistical package StatView (v 5.01.98; SAS Institute Inc, Cary, NC). Correlations were considered to be significant at P < 0.05. The results of continuous data are expressed as mean ± standard deviation (SD).
Results
Participants
Of the 500 women selected, 63 (12.6%) were not present in the classroom when the researcher visited. Twenty-nine (5.8%) of the women who were present declined to participate in the study.
Descriptive data
The final study group consisted of 408 subjects, whose features are reported in Table 1.
Table 1.
Mean (±SD) characteristics of women stratified by presence of menstrual pain
| All women (n = 408) | Women with pain (n = 343) | Women without pain (n = 65) | |
|---|---|---|---|
| Age | 22.90 ± 3.03 | 22.89 ± 2.95 | 22.92 ± 3.44 |
| Height (m) | 1.66 ± 0.06 | 1.66 ± 0.06 | 1.66 ± 0.06 |
| Weight (kg) | 57.88 ± 7.99 | 57.83 ± 8.02 | 58.11 ± 7.88 |
| BMI (kg/m2) | 20.94 ± 2.77 | 20.89 ± 2.81 | 21.17 ± 2.56 |
| Births (n) | 0.03 ± 0.24 | 0.03 ± 0.25 | 0.03 ± 0.17 |
| Miscarriages (n) | 0.01 ± 0.11 | 0.01 ± 0.09 | 0.03 ± 0.17 |
| Abortions (n) | 0.01 ± 0.14 | 0.02 ± 0.15 | 0.00 ± 0.00 |
| Menarche (years) | 12.56 ± 1.32 | 12.45 ± 1.36 | 13.13 ± 1.17* |
| Cycle length (days) | 28.91 ± 4.12 | 28.97 ± 4.40 | 28.62 ± 2.03 |
| Flow length (days) | 4.56 ± 1.19 | 4.63 ± 1.21 | 4.18 ± 1.03** |
Notes:
P = 0.0002;
P = 0.006 versus women with pain, by Student’s t-test.
Sixty-five of these 408 subjects (15.9%) reported that they had never experienced menstrual pain, while 343 (84.1%) reported having experienced menstrual pain, either during every period (176/408, 43.1%) or during some periods (167/408, 41%).
Key results
Presence/absence of pain
Women with menstrual pain had an earlier menarche (P = 0.0002), longer menstrual flow (P = 0.006) (Table 1), were more likely to smoke (P = 0.031), and were less likely to use hormonal contraception (P = 0.015) (Table 2). The major features of menstrual pain are reported in Table 3.
Table 2.
Prevalence of familiar, educational, dietary, physical activity, and obstetrical-gynecological features in women stratified by the presence of menstrual pain
| Women with pain (n = 343) | Women without pain (n = 65) | P-value | |
|---|---|---|---|
| Stable sentimental relationship | 195 (56.85%) | 38 (58.46%) | 0.801 |
| Active smoking | 109 (31.78%) | 12 (18.46%) | 0.031 |
| Physical exercise | 273 (79.59%) | 52 (80%) | 0.940 |
| Coffee consumption | 316 (92.13%) | 57 (87.69%) | 0.242 |
| Attitude to have breakfast | 317 (92.42%) | 60 (92.31%) | 0.975 |
| Alcohol consumption | 275 (80.17%) | 52 (80%) | 0.974 |
| Excessive sugar consumption | 72 (20.99%) | 16 (24.61%) | 0.424 |
| Excessive salt consumption | 29 (8.45%) | 6 (9.23%) | 0.837 |
| Fish consumption | 326 (95.04%) | 62 (95.38%) | 0.907 |
| Gynecological visits | 274 (79.88%) | 53 (81.54%) | 0.759 |
| Contraception users | 96 (27.99%) | 28 (43.08%) | 0.015 |
| Regular cycle | 285 (83.09%) | 54 (83.08%) | 0.998 |
| Past gynecological pathology | 68 (19.82%) | 10 (15.38%) | 0.461 |
| Past gynecological surgery | 11 (3.21%) | 5 (7.69%) | 0.087 |
Table 3.
Major features of menstrual pain
| Pain onset versus menarche | |
| With menarche | 67.4% |
| After 6–12 months | 21% |
| After 1 year | 11.6% |
| Pain onset versus menstrual flow | |
| 2 days before | 18.7% |
| 1 day before | 22.2% |
| With menstrual flow | 50.7% |
| After beginning of menstrual flow | 8.4% |
| Duration of pain during menstrual flow | |
| 1 day | 49.8% |
| 2 days | 38.5% |
| 3 days | 9.6% |
| All flow | 2.1% |
| Associated symptoms | 83.7% |
| Depression | 36.7% |
| Headache | 34.7% |
| Acne | 33.5% |
| Nausea/vomiting | 16.8% |
| Lack of appetite | 10% |
| Use of medicines | 65.6% |
| School performance reduced | 47.8% |
| Social performance reduced | 44.6% |
| Absenteeism | 37.9% |
Menstrual pain influenced quality of life and decreased school performance in 164/343 (47.8%) and social functioning in 153/343 (44.6%) women with menstrual pain. Overall, 130/343 (37.9%) women with menstrual pain reported a certain degree of absenteeism during the last menstrual flow.
The association of menstrual pain and the need for medication was reported in 225/408 (55.2%) subjects. The association of menstrual pain and reduction of school and social performance occurred in 164 (40.2%) and 153 (37.5%) subjects, respectively. Menstrual pain was associated with absenteeism in 130 (31.9%) women. Menstrual pain associated with the need for medication and absenteeism was present in 103 (25.3%) women. These prevalences were significantly different (P < 0.0001).
Pain intensity
Mean pain intensity was 50.2 ± 22.4 mm on a 100 mm VAS scale. Among subjects reporting menstrual pain, pain intensity by VAS was related independently (r = 0.302, P < 0.0001) and directly to menstrual flow length (CR = 0.336), history of abortions (CR = 3.640), and gynecological pathologies (CR = 0.948), and inversely related to age at menarche (CR = −0.225), use of hormonal contraception (CR = −0.787), and history of gynecological surgery (CR = −2.115).
When stratified by menstrual pain VAS score, 82/408 (20.1%) women had mild menstrual pain, 192/408 (47.0%) moderate menstrual pain, and 69/408 (17.0%) severe menstrual pain.
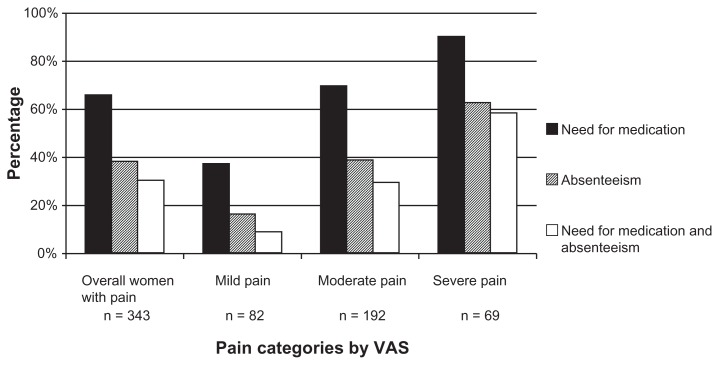
In these three categories the need for medication was 37%, 69.3%, and 89.9%, respectively. Similarly, absenteeism was 16%, 58.5%, and 62.3%, respectively. The need for medication plus absenteeism was 8.6%, 29.2%, and 58%, respectively (Figure 1).
Figure 1.
Prevalence of disturbances associated with menstrual pain in all women and in women stratified by intensity of menstrual pain as evaluated by a visual analogic scale.
Stratification by VAS score was not coincident with the figures representing a need for medication and absenteeism. Indeed, only 58% of individuals with severe menstrual pain had a disorder that concomitantly required treatment and impaired quality of life to the point of inducing absenteeism.
Discussion
Key results
In this survey-based study, the total prevalence of menstrual pain experience was very high with 84.1% of participants reporting pain at some point. Some 43.1% of participants reported having painful menstruation in every menstrual period, and 41% reported pain in some periods. These results are comparable with other data reported in the literature.9,25–27 It was found that the group of women who suffered from menstrual pain were more likely to smoke and less likely to use hormonal contraception. Those with menstrual pain also tended to have a longer menstrual flow and an early menarche.
The association between smoking and menstrual pain has previously been reported,8,13–15 and a dose-response relationship has been observed.15 The observed association with menarche is controversial, and both an early7,8 and late4–6 menarche have been considered risk factors for menstrual pain in women.
Higher pain intensity is associated with longer menstrual flow, a history of abortions or gynecological pathologies, and not being on hormonal contraception, further supporting the protective role exerted by hormonal contraception on this disease.
In some studies,5,7,25 mild to intermediate menstrual pain has been considered sufficient to define dysmenorrhea. Others have considered dysmenorrhea to be menstrual pain associated with “the need for medication and the inability to function normally.”2 These two definitions are quite different, and the current study found that the intensity of menstrual pain does not coincide with a need for medication or the inability to function normally. Approximately 55% of the women in the current study reported menstrual pain and a need for medication, with poor social functioning or absenteeism (features of not functioning normally) as a result of menstrual pain ranging from 32% to 40%. When evaluating the most complete picture of dysmenorrhea characterized by menstrual pain, absenteeism, and a need for medication, prevalence is about 25%. How dysmenorrhea is defined will have an impact on figures regarding its prevalence.
Limitations
There are several limitations to the current research. It was not possible to discriminate between primary and secondary dysmenorrhea, and menstrual pain as a whole was considered. The self-reporting nature of this study may have resulted in recall bias and over-reporting of the condition. Women were randomly selected, but some did not complete the questionnaire. This may have had an impact on the reported prevalence of the disease.
Generalizability
All participants were university students, and thus the educational level of participants was high. However, the Italian Ministry of University and Research reported in 2010 that 71.5% of individuals in the study region who graduate from secondary school go on to study at university. Accordingly, the data may reasonably be expected to apply to most but perhaps not all women. Finally, this study was conducted in only one university, so the results cannot be extended to other regions of Italy or to other countries. Nevertheless, the collected data provide a clear indication that the prevalence of dysmenorrhea may vary depending on how it is defined. It can be concluded that a more concrete definition of dysmenorrhea should be given in order to obtain reliable and comparable results from independent trials.
Acknowledgment
The authors thank all the students that participated in this study.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Harel Z. Dysmenorrhea in adolescents and young adults: etiology and management. J Pediatr Adolesc Gynecol. 2006;19(6):363–371. doi: 10.1016/j.jpag.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 2.Dawood MY. Dysmenorrhea and prostaglandins: pharmacological and therapeutic considerations. Drugs. 1981;22(1):42–56. doi: 10.2165/00003495-198122010-00003. [DOI] [PubMed] [Google Scholar]
- 3.Santer M, Warner P, Wyke S. A Scottish postal survey suggested that the prevailing clinical preoccupation with heavy periods does not reflect the epidemiology of reported symptoms and problems. J Clin Epidemiol. 2005;58(11):1206–1210. doi: 10.1016/j.jclinepi.2005.02.026. [DOI] [PubMed] [Google Scholar]
- 4.Ozerdogan N, Sayiner D, Ayranci U, Unsal A, Giray S. Prevalence and predictors of dysmenorrhea among students at a university in Turkey. Int J Gynecol Obstet. 2007;107(1):39–43. doi: 10.1016/j.ijgo.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 5.Ortiz MI, Rangel-Flores E, Carrillo-Alarcòn LC, Veras-Godoy HA. Prevalence and impact of primary dysmenorrhea among Mexican high school students. Int J Gynecol Obstet. 2009;107(3):240–243. doi: 10.1016/j.ijgo.2009.07.031. [DOI] [PubMed] [Google Scholar]
- 6.Tangchai K, Titapant V, Boriboonhirusarn D. Dysmenorrhea in Thai adolescents: prevalence, impact and knowledge of treatment. J Med Assoc Thai. 2004;87(Suppl 3):S69–S73. [PubMed] [Google Scholar]
- 7.Harlow SD, Park M. A longitudinal study of risk factors for the occurrence, duration and severity of menstrual cramps in a cohort of college women. Br J Obstet Gynecol. 1996;103(11):1134–1142. doi: 10.1111/j.1471-0528.1996.tb09597.x. [DOI] [PubMed] [Google Scholar]
- 8.Svanberg L, Ulmsten U. The incidence of primary dysmenorrhea in teenagers. Arch Gynecol. 1981;230(3):173–177. doi: 10.1007/BF02111800. [DOI] [PubMed] [Google Scholar]
- 9.Balbi C, Musone R, Menditto A, et al. Influence of menstrual factors and dietary habits on menstrual pain in adolescence age. Eur J Obstet Gynecol Reprod Biol. 2000;91(2):143–148. doi: 10.1016/s0301-2115(99)00277-8. [DOI] [PubMed] [Google Scholar]
- 10.Latthe P, Mignini L, Gray R, Hills R, Khan K. Factors predisposing women to chronic pelvic pain: systematic review. BMJ. 2006;332(7544):749–755. doi: 10.1136/bmj.38748.697465.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blakey H, Chisholm C, Dear F, et al. Is exercise associated with primary dysmenorrhea in young women? BJOG. 2010;117(2):222–224. doi: 10.1111/j.1471-0528.2009.02220.x. [DOI] [PubMed] [Google Scholar]
- 12.Hillen TI, Grbavac SL, Johnston PJ, Straton JA, Keogh JM. Primary dysmenorrhea in young Western Australian women: prevalence, impact and knowledge of treatment. J Adolesc Health. 1999;25(1):40–45. doi: 10.1016/s1054-139x(98)00147-5. [DOI] [PubMed] [Google Scholar]
- 13.Hornsby PP, Wilcox AJ, Weinberg CR. Cigarette smoking and disturbance of menstrual function. Epidemiology. 1998;9(2):193–198. [PubMed] [Google Scholar]
- 14.Charlton A, While D. Smoking and menstrual problems in 16-year-olds. J R Soc Med. 1996;89(4):193–195. doi: 10.1177/014107689608900405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen C, Cho SI, Damokosh AI, et al. Prospective study of exposure to environmental tobacco smoke and dysmenorrhea. Environ Health Perspect. 2000;108(11):1019–1022. doi: 10.1289/ehp.001081019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abdul-Razzak KK, Ayoub NM, Abu-Taleb AA, Obeidat BA. Influence of dietary intake of dairy products on dysmenorrhea. J Obstet Gynecol Res. 2010;36(2):377–383. doi: 10.1111/j.1447-0756.2009.01159.x. [DOI] [PubMed] [Google Scholar]
- 17.Fujiwara T, Sato N, Awaji H, Sakamoto H, Nakata R. Skipping breakfast adversely affects menstrual disorders in young college students. Int J Food Sci Nutr. 2009;26:1–9. doi: 10.1080/09637480802260998. [DOI] [PubMed] [Google Scholar]
- 18.Wang L, Wang X, Wang W, et al. Stress and dysmenorrhea: a population based prospective study. Occup Environ Med. 2004;61(12):1021–1026. doi: 10.1136/oem.2003.012302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reddish S. Dysmenorrhea. Aust Fam Physician. 2006;35(11):842–849. [PubMed] [Google Scholar]
- 20.Coco AS. Primary dysmenorrhea. Am Fam Physician. 1999;60(2):489–496. [PubMed] [Google Scholar]
- 21.Jamieson DJ, Steeg JF. The prevalence of dysmenorrhea, dyspaurenia, pelvic pain and irritable bowel syndrome in primary care practices. Obstet Gynecol. 1996;87(1):55–58. doi: 10.1016/0029-7844(95)00360-6. [DOI] [PubMed] [Google Scholar]
- 22.Patel V, Tanksale V, Sahasrabhojanee M, Gupte S, Nevrekar P. The burden and determinants of dysmenorrhea: a population-based survey of 2262 women in Goa, India. BJOG. 2006;113(4):453–463. doi: 10.1111/j.1471-0528.2006.00874.x. [DOI] [PubMed] [Google Scholar]
- 23.Burnett MA, Antao V, Black A, et al. Prevalence of primary dysmenorrhea in Canada. J Obstet Gynecol Can. 2005;27(8):765–770. doi: 10.1016/s1701-2163(16)30728-9. [DOI] [PubMed] [Google Scholar]
- 24.Pitts MK, Ferris JA, Smith AM, Shelley JM, Richters J. Prevalence and correlates of three types of pelvic pain in a nationally representative sample of Australian women. Med J Aust. 2008;189(3):138–143. doi: 10.5694/j.1326-5377.2008.tb01945.x. [DOI] [PubMed] [Google Scholar]
- 25.Polat A, Celik H, Gurates B, et al. Prevalence of primary dysmenorrhea in young adult female university students. Arch Gynecol Obstet. 2009;279(4):527–532. doi: 10.1007/s00404-008-0750-0. [DOI] [PubMed] [Google Scholar]
- 26.Cakir M, Mungan I, Karakas T, Girisken I, Okten A. Menstrual pattern and common menstrual disorders among university students in Turkey. Ped Int. 2007;49(6):938–942. doi: 10.1111/j.1442-200X.2007.02489.x. [DOI] [PubMed] [Google Scholar]
- 27.Al-Kindi R, Al-Bulushi A. Prevalence and impact of dysmenorrhea among Omani high school students. SQU Med J. 2011;11(4):485–491. [PMC free article] [PubMed] [Google Scholar]