Abstract
Objective
To develop an algorithm for the discovery of drug treatment patterns for endocrine breast cancer therapy within an electronic medical record and to test the hypothesis that information extracted using it is comparable to the information found by traditional methods.
Materials
The electronic medical charts of 1507 patients diagnosed with histologically confirmed primary invasive breast cancer.
Methods
The automatic drug treatment classification tool consisted of components for: (1) extraction of drug treatment-relevant information from clinical narratives using natural language processing (clinical Text Analysis and Knowledge Extraction System); (2) extraction of drug treatment data from an electronic prescribing system; (3) merging information to create a patient treatment timeline; and (4) final classification logic.
Results
Agreement between results from the algorithm and from a nurse abstractor is measured for categories: (0) no tamoxifen or aromatase inhibitor (AI) treatment; (1) tamoxifen only; (2) AI only; (3) tamoxifen before AI; (4) AI before tamoxifen; (5) multiple AIs and tamoxifen cycles in no specific order; and (6) no specific treatment dates. Specificity (all categories): 96.14%–100%; sensitivity (categories (0)–(4)): 90.27%–99.83%; sensitivity (categories (5)–(6)): 0–23.53%; positive predictive values: 80%–97.38%; negative predictive values: 96.91%–99.93%.
Discussion
Our approach illustrates a secondary use of the electronic medical record. The main challenge is event temporality.
Conclusion
We present an algorithm for automated treatment classification within an electronic medical record to combine information extracted through natural language processing with that extracted from structured databases. The algorithm has high specificity for all categories, high sensitivity for five categories, and low sensitivity for two categories.
Keywords: Clinical natural language processing, electronic medical record, phenotype extraction, endocrine therapy, breast cancer treatment, human-computer interaction and human-centered computing, providing just-in-time access to the biomedical literature and other health information, applications that link biomedical knowledge from diverse primary sources (includes automated indexing), linking the genotype and phenotype, discovery, NLP, asdf d, pet, biostatistics, ontologies, knowledge representations, controlled terminologies and vocabularies, information retrieval, HIT data standards, pharmacogenomics
Background and significance
The electronic medical record (EMR) has traditionally been viewed by medical practitioners as a place to document the medical care of their patients, provide a record of billable services, and protect the legal interests of both patients and healthcare providers. A less appreciated purpose of the EMR is its potential for medical research. A broad EMR implementation will result in the accumulation of vast quantities of patient data that can be mined to improve the quality, safety, efficiency, and efficacy of healthcare, and also advance research and public health. These developments will necessitate exposing enormous computational and analytical tools directly to practitioners and investigators. At the national level, the US Office of the National Coordinator of Health Information Technology (ONC) has emphasized the importance of the use of information technology in healthcare by leading the Strategic Health IT Advanced Research Projects (SHARP)1 initiative. One of the four SHARP projects focuses exclusively on secondary data use of information arising from EMR (SHARPn).2
Several national efforts, supported by the US National Institutes of Health, demonstrate the secondary use of the EMR for research purposes by focusing on ‘developing, disseminating and applying approaches to research that combine DNA biorepositories with the EMR systems for large-scale, high-throughput biomedical research’3 such as the electronic Medical Record and Genomics consortium3 4 and the Pharmacogenomics Research Network (PGRN).5 Wilke and colleagues6 overview the convergence of healthcare and genotyping technologies. In a 2010 JAMA manuscript on the association between CYP2D6 polymorphisms and outcomes among women with early stage breast cancer treated with tamoxifen, Schroth and colleagues7 point out that the results of their study ‘once more underscore the need for high-powered data sets.’ A major bottleneck is patient data abstraction, traditionally a time-consuming, effort intense review of patients' medical records by trained abstractors to find relevant phenotype nuggets.
The EMR offers the computational environment for automated or semi-automated information extraction across data residing in structured databases and in the free-text clinical narratives generated by the practitioners at the point of care. Information extraction from structured databases requires standard querying techniques, while information extraction from the clinical narrative calls for Natural Language Processing (NLP) methods. EMR algorithms for high-throughput phenotyping require merged information extracted from multiple sources, for example, prescribing systems, laboratory results, and clinical notes. Many academic healthcare centers now recognize the secondary uses of the EMR by creating operational EMR mirrors for research purposes as exemplified by the Mayo Clinic Enterprise Data Trust (EDT)8 and Informatics for Integrating Biology and the Bedside (i2b2) datamarts.9 In an August, 2011 JAMA editorial, Jha10 discusses the promises of the EMR, emphasizing the importance of NLP as an enabling tool for accessing the vast information residing in the EMR, and stated that ‘federal government can play a helpful role by funding the basic research needed to launch this field forward.’
Our study contributes to the growing body of research demonstrating the secondary use of the EMR data enabled by NLP methods for mining the clinical narrative and its integration with other types of EMR information. In this study, we used the manually abstracted treatment regimens from a prior breast cancer pharmacogenomic study to test the hypothesis that automatically extracted information from the EMR originally created by the practitioner at the point of care, coupled with computational techniques, is comparable to the information found by traditional manual abstraction methods. Our model study is part of a larger PGRN-supported breast cancer pharmacogenomic study designed to evaluate the role of genetic variation related to endocrine therapy, clinical outcomes, and drug-related side effects. We chose this study as a ‘model system’ because: (1) it is an example of medical research combining large-scale genomic and phenotype data in an attempt to advance breast cancer drug therapy; and (2) it presents technical challenges typical for information extraction from the EMR, specifically mining treatment events and relating them temporally. The study objectives were: (1) to develop an automated EMR endocrine breast cancer treatment classification algorithm; (2) to measure the agreement between the data abstracted by the algorithm and the traditional manual abstraction method; and (3) to perform a detailed error analysis to outline the next steps. The purpose of this study was not to reach conclusions about the ‘pharmacogenetics’ of the endocrine therapy of breast cancer, but rather to test an enabling high-throughput EMR automated tool to obtain endocrine treatment patterns.
Materials and methods
Patient cohort
The Mayo Clinic Breast Cancer study is an on-going cohort study initiated in February 2001 at Mayo Clinic, Rochester, Minnesota. Patients (women aged 18 years or over from Minnesota, Iowa, Wisconsin, Illinois, North Dakota, and South Dakota diagnosed with histologically confirmed primary invasive breast cancer and no prior history of another cancer (excluding non-melanoma skin cancer)) were enrolled within 6 months of diagnosis. Patients' written informed consent was obtained. All aspects of these studies were approved by the Mayo IRB. The cohort used in this analysis consisted of 1507 women with stage I, II, or III breast cancer.
Manual data abstraction
A trained registered nurse abstracted the treatment information for tamoxifen and/or aromatase inhibitor (AI) cycles from the patient's chart. Table 1 lists the relevant treatments. Information for 14 cases was abstracted from paper histories, typically notes from the local physicians who treated patients after the patients returned to their homes. Based on the information in these sources, each patient was assigned to one treatment category:
Table 1.
List of tamoxifen and aromatase inhibitor medications
| Tamoxifen drugs and synonyms (yes/no inclusion in RxNorm) | Aromatase inhibitors (yes/no inclusion in RxNorm) |
| Tamoxifen (yes) | Arimidex (yes) |
| Fentamox (yes) | Anastrozole (yes) |
| Nolvadex (yes) | Aromasin (yes) |
| Emblon (yes) | Exemestane (yes) |
| Tamofen (yes) | Femara (yes) |
| Soltamox (yes) | Letrozole (yes) |
| Oestrifen (yes) | |
| Noltam (yes) | |
| Fentamox (yes) | |
| Tamox (no) | |
| Tam (no) |
Unified Medical Language System (UMLS; http://www.nlm.nih.gov/research/umls/) 2009AB version of the RxNorm drug terminology (http://www.nlm.nih.gov/research/umls/rxnorm/)
Category 0: no tamoxifen or AI
Category 1: Tamoxifen only
Category 2: AI only
Category 3: Tamoxifen then AI
Category 4: AI then tamoxifen
Category 5: multiple AIs and tamoxifen cycles in no specific order
Category 6: no specific dates could be attributed to the AI and tamoxifen treatment/s
Category 7: no confirmation of whether the patient has received either tamoxifen or AI treatment.
Electronic medical record
The Mayo Clinic has utilized a comprehensive EMR since 2002. Some EMR data types are the free-text clinical narrative generated by the practitioners at the point of care, laboratory results, and the electronic prescribing database (Orders97) with fields for drug name, generic drug name, prescription dates, dose, refills, quantity, frequency, route, and duration. We used the research mirror of Mayo's EMR, the EDT.8 Orders97 provides a medication history as part of outpatient clinical notes and is a means to enter prescriptions related to all types of services including ophthalmology (eye glasses) and other general applications (wheel chairs), in addition to medications.
Clinical Text Analysis and Knowledge Extraction System (cTAKES)
cTAKES (http://ohnlp.svn.sourceforge.net/viewvc/ohnlp/trunk/) is an open-source, general purpose, modular, extensible NLP software for processing the clinical narrative.11 cTAKES applications to mining the clinical narrative are presented elsewhere.12–15 cTAKES processes clinical notes and identifies the following clinical named entity mentions (NEs): Drugs, Diseases/Disorders, Signs/Symptoms, Anatomical sites, and Procedures. Each discovered NE is assigned attributes such as text span, ontology mapping code (UMLS,16 SNOMED CT,17 RxNorm18), context (family history of, current, unrelated to patient), and a negation indicator. Version 1.1.0 of the cTAKES platform consists of the following annotators in this specific order:
Sentence boundary detector, a wrapper around OpenNLP's sentence boundary detector,19 but trained on clinical data
Rule-based tokenizer to separate punctuations from words
Normalizer, a wrapper around LVG20 to standardize, for example, morphologically different phrases with the same meaning, for example, ‘infection,’ ‘infecting,’ ‘infects’ normalize to the same form of ‘infect’
Context dependent tokenizer grouping tokens to create Date, Time, Fraction, Range, Measurement, and PersonTitle groupings
Part-of-speech tagger, a wrapper around OpenNLP's but trained on clinical data. The module assigns a part-of-speech label to each word
Phrasal chunker, a wrapper around OpenNLP's but trained on clinical data to detect phrases such as noun phrases, verb phrases, and prepositional phrases
Dictionary lookup annotator which performs a permutational lookup against a dictionary database. The permutations are computed off the components within the user-specified lookup window (usually the noun phrase)
Context annotator based on NegEx21 to link information with the patient or family members
Negation detector based on NegEx to discover whether a concept is negated or not
Dependency parser to detect dependency relationships between words22
Module for the identification of patient smoking status: past smoker, current smoker, non-smoker, smoker, unknown23
Drug mention annotator populating a drug template (described in the section entitled ‘Component one: information extraction from the clinical narrative (document-level treatment extraction)’).
cTAKES is built within the engineering framework of the Apache Unstructured Information Management Architecture (UIMA)24 which facilitates scalability, expandability, and collaborative software development.
Treatment/drug classification algorithm
A multidisciplinary approach was required to develop the algorithm that leveraged the knowledge of epidemiology, oncology, pharmacogenomics, NLP, statistics, and software engineering experts. The clinical notes for each patient from the date of their breast cancer diagnosis (as established by the pathology test) were extracted. The automated tool relied only on information extracted from the EMR and had the four components as listed below to combine information extracted from the free-text part of the EMR using NLP techniques with information extracted from structured databases through traditional queries.
Component one: information extraction from the clinical narrative (document-level treatment extraction)
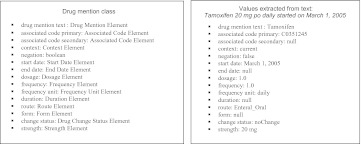
This component processed each electronic free-text clinical note to discover treatment information. cTAKES functionality was extended for the discovery of medication-specific attributes (figure 1). Of note, optical character recognition was not applied to the scanned local medical doctor documentation and paper histories, hence information from them was not included in the automated tool.
Figure 1.
cTAKES expansion for drug-specific attributes at the document level.
To extract information from the clinical narrative, we extended the cTAKES information model with medication-specific attributes such as frequency, route, and dosage and developed a module to extract values from the free-text clinical document. Figure 1 provides an example of values extracted by cTAKES for a typical text string. The values for the drug-specific attributes such as dosage, route, frequency, etc, are discovered by scanning the text within a particular window (defined below) and extracting values from within that window. Windows are defined using two methods. The first method is designed to extract data from a list-type format typically found in the section entitled ‘Current/admission/discharge medications’; thus this first window is delimited by new line characters. The second method is designed to extract data from narrative sections of the EMR and search for sentence boundaries. Each sentence containing a medication mention becomes one window from which the attribute values are extracted. If a sentence contains multiple medication mentions, then the sequencing pattern is taken into account and the closest attributes to the particular drug mention are assigned to that mention. For example, in ‘Aspirin 325 mg PRN, Tylenol 325 mg PRN,’ the sequencing pattern is Drug mention, Strength, Frequency, hence the Strength and Frequency attributes following the Drug mention are assigned to that specific medication.
Extraction of associated code attributes
The associated code primary attribute is reserved for the RxNorm18 code while the associated code secondary attribute represents an additional mapping to medication classes, for example, the National Drug File – Reference Terminology25 class. RxNorm terminology provides normalized names for clinical drugs used in pharmacy management. Each drug links to a unique code, for example, tamoxifen is assigned an RxNorm code of 10324. RxNorm, however, does not provide a list of unofficial abbreviations that practitioners might use in their daily practice and care management documentation, for example, the commonly used in clinical notes abbreviation ‘tam.’ The list of tamoxifen and AI medications consisted of 11 and seven items, respectively (table 1). Two terms (‘tam’ and ‘tamox’) not found in the RxNorm (UMLS26 version 2009AB) were added to the dictionary.
Extraction of date attributes
Date attributes for each drug mention are extracted from the free text through a pattern matching technique. The Date attribute is populated with a spanned text date field which can be associated with either the start or end date.
Extraction of dosage attribute
Dosage refers to how many of each drug the patient is taking. Any numeric text description or a number value adjacent to a Strength or Frequency mention will populate Dosage with its value. For instance, in the phrase ‘Take two 325-mg aspirin tablets’ the ‘two’ would indicate the Dosage attribute and ‘325 mg' would indicate the Strength.
Extraction of frequency attribute
Frequency describes how often the patient needs to take the drug. It consists of a frequency number and frequency unit. Periodic phrases coupled with numeric text values or number values adjacent to Drug named entity, Strength, and Frequency terms are discovered as Frequency. This also includes common Latin terms (eg, ‘b.i.d.,’ ‘p.r.n.,’ and ‘qhs’) and hyphenated phrases (eg, ‘every-other-evening,’ ‘as-needed,’ and ‘once-a-day’).
Extraction of duration attribute
Duration represents how long the patient is expected to take the drug. Phrases starting with terms like ‘for,’ ‘x,’ ‘continued,’ ‘until’ and followed by periodic values, key hyphenated phrases, and/or numeric text or number values are used for this term.
Extraction of route attribute
Route refers to the way that the drug is introduced into the body. Phrases that are equivalent or synonymous of the following are included: topical, oral, gastric, rectal, intravenous, intra-arterial, intramuscular, intracardiac, subcutaneous, intrathecal, intraperitoneal, transdermal, and transmucosal.
Extraction of form attribute
Form describes the physical appearance of a drug. Terms include aerosol, capsule, cream, elixir, emulsion, enema, gel, implant, inhalant, injection, liquid, lotion, lozenge, ointment, patch, pill, powder, shampoo, soap, solution, spray, suppository, syrup, and tablet.
Extraction of change status attribute
Change status refers to whether the medication is currently being taken or not and the change associated with this. Its values are started, stopped, increased, decreased, and no change. For example, the extraction from ‘increased Zoloft from 5 mg to 10 mg’ results in two drug annotations: (1) Drug mention=‘Zoloft,’ context=current, change status=increased, strength=10 mg; and (2) Drug mention=‘Zoloft,’ context=history of, change status=null, strength=5 mg.
Extraction of strength attribute
Strength is a two word text span of, typically, number and unit. It is subdivided into strength number and strength unit, for example in the span ‘325 mg,’ 325 is the number and mg is the unit.
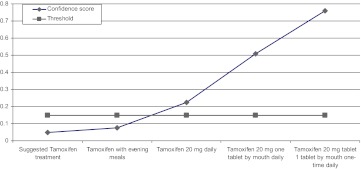
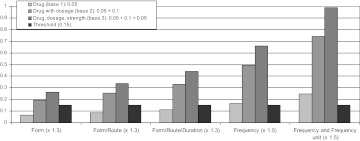
Estimation of confidence in data extracted
A confidence metric that the medication has been prescribed is used for the Impression/Report/Plan (I/R/P) and History of Present Illness (HPI) sections based on the presence of drug-related attributes near the drug mention. For instance, if the I/R/P section contains ‘tamoxifen 20 mg daily,’ the presence of both ‘20 mg’ and ‘daily’ boosts the confidence. Any drug-related named entity will be assigned a base value of 0.05 for the Confidence initially; however, this value will be set to 0.15 if there is an adjacent Strength discovered. Additionally, 0.05 will be added if the presence of the Dosage attribute is determined. This value will increase with the addition of other drug elements if discovered. ‘Confidence’ will increase by a factor of 1.3 if Form, Route, or Duration attributes are found, and it will increase by a factor of 1.5 if Frequency and Frequency Unit are discovered. The maximum confidence would be just under 1.0 (0.989=(0.05+0.15)×1.3×1.3×1.3×1.5×1.5) in the event that all elements of the drug named entity were discovered (see figure 2 for examples). The weights of these attributes are used to reflect the scale of the likelihood that this attribute relates to a drug term, so the presence of Form/Route/Duration is slightly less weighted than Frequency/Frequency Unit. The ‘Confidence’ value threshold that will determine if a mention will be extracted is 0.15 and above. The confidence scaling was determined empirically based on observations of the likelihood that a drug mention was related to the patient and not a hypothetical general discussion. The more detail about the drug mention, the higher the confidence that the mention is related to a present or recent prescription. In the absence of a medication dosage and strength information, at least four other signature elements are required to achieve the desired threshold. Figure 3 represents the resulting scores when different signature elements are discovered and the effect of each element on the final score (1.3 or 1.5 factor). The only combination not represented in the figure would be a drug mention with dosage and no strength, which is atypical.
Figure 2.
Confidence scores for five examples.
Figure 3.
Confidence scores for three base states representing the drug signature elements' relative effect on the confidence score. The first three column groups represent the addition of Form, Route, and Duration attributes. The last two column groups represent the addition of Frequency and Frequency Unit attributes.
Consideration of negation terms
The list of discovered medication mentions was additionally pruned to filter out negated AI and tamoxifen mentions. We extended the list of the negation words incorporated within the generic cTAKES negation detection algorithm.21 Terms signaling non-confirmed treatments included ‘suggest,’ ‘doubt,’ ‘discuss,’ ‘decide,’ ‘recommend,’ ‘talk,’ ‘plan,’ ‘think,’ ‘consider,’ and ‘considers’ along with their variants. For example, in ‘I discussed with the patient tamoxifen treatment,’ ‘tamoxifen’ is flagged as a medication, but filtered out as it was in the context of a discussion only and not a confirmed treatment.
Component two: information extraction from the medication prescribing system
This component extracted prescription information from the electronic prescribing database (Orders97) through standard database queries. The same window used for the clinical notes was applied to obtain all prescription entries starting 2 weeks prior to the diagnosis of breast cancer to allow for slight deviations in the date of diagnosis. The start date for an Orders97 medication was the time the medication was prescribed. As typical for electronic prescription interfaces, Orders97 specifies no end date.
Component three: information merging
This component unified the information from the first two components to create the patient-level medication history. The final patient-level start date for a medication was determined by its first Orders97 entry if there was one, otherwise by the first start date of that medication as discovered from the clinical notes. If a start date existed for both the clinical document and the Orders97 entry, then the Orders97 date was used, unless the Orders97 date was more than 2 weeks earlier than the diagnosis date for this particular patient. In the event that the Orders97 information was earlier than 2 weeks, the clinical document date was used. The final end date for a medication was determined by the last stop date attribute if available, otherwise by the date of the last mention within the clinical notes if there was no 7+ month gap of inactivity. If there was a 7+ month gap, then a new start/end cycle was begun. The 7-month timeframe was considered the most reasonable from a clinical practice standpoint in that 6-month intervals are most commonly used for follow-up.
Component four: automatic treatment classification
This component applied the final logic based on the evidence from the third component. The algorithm collapsed into one category the data points for category 0 and 7 from the manually abstracted data because the distinctions were not entirely clear. Patients with no medication data are classified into category 0.
Evaluation metrics
We report results in terms of sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). Accuracy is the ratio between the total number of system assignments that agree with the abstractor assignments and the total number of cases.
Results
A total of 96 833 clinical notes were identified for the 1507 patients, and 1384 (91.84%) patients had notes with at least one medication mention. The clinical notes of 619 (41.07%) patients contained at least one tamoxifen mention (6338 tamoxifen instances; mean 10.24, median 7). The clinical notes of 539 (35.77%) patients contained at least one aromatase inhibitor (AI) mention (6759 AI instances; mean 12.54, median 8). For patients with any Orders97 orders (1378 patients (91.43%)), there were a total of 20 323 medication orders. Overall, 510 (33.86%) patients had at least one tamoxifen order (1337 tamoxifen orders, mean 2.62, median 2) and 446 (29.54%) patients had at least one AI order (1233 AI orders; mean 2.76, median 2).
Each clinical note document was processed through the enhanced cTAKES to discover medications from the following five sections: Impression/Report/Plan, History of Present Illness, Current medications, Admission medications, and Discharge medications. Processing took approximately 3 h and 15 min (Dual AMD Opteron 248 processors (64 bit) with 16 GB system RAM running the Linux-based Fedora Core 6 (64 bit) OS). Manual data abstraction is estimated to proceed at a rate of 25 charts per week by an experienced registered nurse abstractor, which for this study totals 15 weeks.
The accuracy of overall agreement for the results for treatment classification was 0.925. For categories 0, 1, 2, 3, and 4, the sensitivity and specificity ranged from 90.27% to 99.83%, while the predictive values ranged from 80.00% to 99.93% with lower results for categories 5 and 6 where complex treatment timelines presented a challenge (table 2).
Table 2.
Agreement results between the two methods: (1) traditional manual abstraction (manual abstraction columns) and (2) automated tool combining information extracted from clinical free-text through natural language processing with information extracted from an electronic prescribing system (automated tool, all components rows)
| Manual abstraction | |||||||
| True | False | Total | Sensitivity | Specificity | Positive predictive value | Negative predictive value | |
| Category 0 and 7: no tamoxifen or AI treatment, or no confirmation for tamoxifen or an AI | |||||||
| Automated tool (all components) | |||||||
| True | 573 | 36 | 609 | 99.83% | 96.14% | 94.09% | 99.89% |
| False | 1 | 897 | 898 | ||||
| Total | 574 | 933 | 1507 | ||||
| Category 1: tamoxifen only | |||||||
| Automated tool (all components) | |||||||
| True | 334 | 9 | 343 | 90.27% | 99.21% | 97.38% | 96.91% |
| False | 36 | 1128 | 1164 | ||||
| Total | 370 | 1137 | 1507 | ||||
| Category 2: aromatase inhibitors only | |||||||
| Automated tool (all components) | |||||||
| True | 305 | 25 | 330 | 91.59% | 97.87% | 92.42% | 97.62% |
| False | 28 | 1149 | 1177 | ||||
| Total | 333 | 1174 | 1507 | ||||
| Category 3: tamoxifen followed by aromatase inhibitors | |||||||
| Automated tool (all components) | |||||||
| True | 160 | 34 | 194 | 92.49% | 97.45% | 82.47% | 99.01% |
| False | 13 | 1300 | 1313 | ||||
| Total | 173 | 1334 | 1507 | ||||
| Category 4: aromatase inhibitors followed by tamoxifen | |||||||
| Automated tool (all components) | |||||||
| True | 16 | 4 | 20 | 94.12% | 99.73% | 80% | 99.93% |
| False | 1 | 1486 | 1487 | ||||
| Total | 17 | 1490 | 1507 | ||||
| Category 5: multiple aromatase inhibitors and tamoxifen cycles in no specific order | |||||||
| Automated tool (all components) | |||||||
| True | 4 | 1 | 5 | 23.53% | 99.93% | 80% | 99.13% |
| False | 13 | 1489 | 1502 | ||||
| Total | 17 | 1490 | 1507 | ||||
| Category 6: no specific dates can be attributed to treatment, thus no sequencing timelines | |||||||
| Automated tool (all components) | |||||||
| True | 0 | 0 | 0 | 0% | 100% | NA | 99.73% |
| False | 4 | 1503 | 1507 | ||||
| Total | 4 | 1503 | 1507 | ||||
Due to time limitations, we randomly selected 131 (63.6%) from the total of 206 disagreements between the automated system and the traditional manual abstraction method for review. Table 3 summarizes the disagreements. Some 73% (96 instances) were true algorithmic errors, and 27% (35 instances) were not algorithmic errors, of which 11% (14 instances) were due to the lack of data source access (eg, scanned documents or paper histories), 8% (10 instances) were misses by the abstractor, and 8% (11 instances) were disagreements due to the last manual abstraction date. The algorithmic errors were related to the discovery of complex temporality, medication attributes outside of the window, and confidence metric assignment. The cut-off date disagreements are such that the system abstracted information from documents after the last manual abstraction date.
Table 3.
Distribution of manually reviewed disagreements (a sample of a randomly selected 131 disagreements from a total of 206 disagreements)
| Treatment category | Manually reviewed: algorithm errors | Manually reviewed: errors related to data access | Manually reviewed: manual abstraction misses | Manually reviewed: evidence found after the last abstraction date | Total manually reviewed errors |
| Category 0 and 7 | 25 | 0 | 3 | 9 | 37 |
| Category 1 | 35 | 6 | 0 | 1 | 42 |
| Category 2 | 18 | 2 | 4 | 1 | 25 |
| Category 3 | 5 | 4 | 2 | 0 | 11 |
| Category 4 | 0 | 1 | 1 | 0 | 2 |
| Category 5 | 9 | 1 | 0 | 0 | 10 |
| Category 6 | 4 | 0 | 0 | 0 | 4 |
| Total | 96 | 14 | 10 | 11 | 131 |
Discussion
Within an EMR environment, we built an algorithm for mining endocrine breast cancer treatment patterns that combines NLP and standard database queries. The algorithm has high specificity for all categories, high sensitivity for five of the categories, and low sensitivity for two of the categories. Approaches like ours could assist accrual of large EMR cohorts for research as they are scalable and can be used both retrospectively and prospectively.
The EMR environment we used, EDT,8 is grounded in interoperability principles such as Health Level 7 Standards to ‘improve care delivery, optimize workflow, reduce ambiguity and enhance knowledge transfer among all stakeholders’ (http://www.hl7.org/). A direct implication of that implementation is the clear boundaries of the clinical note sections enabling unambiguous phenotype extraction, for example, limiting medication extraction to Impression/Report/Plan, History of Present Illness, Current Medications, Admission Medications, and Discharge Medications sections. Such an environment allows data sharing and phenotype extraction not only across patients, but across institutions and healthcare providers. Our approach is disease-agnostic and could be applied to other diseases after a modification of the medication dictionary. We also hope to contribute to a shift where each practitioner starts to view the EMR as a valuable data resource with a life that extends beyond purely patient care and administrative tasks.
Our study emphasizes important technical challenges for information extraction from the clinical narrative such as clinical events temporality.27 Another challenge includes incomplete event documentation. If there is insufficient evidence and/or heavy reliance on background knowledge and inference, the current NLP-based system does not have any recovery functionalities.
Conclusion
Our goal in this study was to demonstrate a secondary and meaningful use of the EMR data generated at the point of care, coupled with information technologies for high-throughput phenotyping for clinical translational research. We chose a breast cancer pharmacogenomic study for our model system. We showed that data harvested from the EMR in an automated fashion are comparable to those manually abstracted by a trained registered nurse abstractor. Next steps will include the incorporation of additional modules for chemotherapy, radiation therapy, breast cancer recurrence, and other types of cancer diagnosis extraction as well as drugs that are CYP2D6 inhibitors, which are known to affect tamoxifen metabolism—all these extracted from the EMR using NLP and standard database queries. Our hope is that studies like ours will enable the EMR to achieve its full potential as an indispensible analytical aid for both practitioners and biomedical investigators to improve patient care and accelerate translational research.
Footnotes
Funding: This work was funded by an NCI DCCPS supplement grant (PI Olson), grants UO1 GM61388 (PI Weinshilboum), U01 HG 04599 (PI Chute), R01 CA122340 (PI Couch), Breast SPORE CA 116201 (PI Ingle), and a SHARP award (90TR0002) (PI Chute).
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The data used in the study has been shared within the team. The software code is released open source at the cTAKES website: http://ohnlp.svn.sourceforge.net/viewvc/ohnlp/trunk/cTAKES/
References
- 1.Strategic Health IT Advanced Research Projects (SHARP) Program, Office of the National Coordinator. 2011. http://healthit.hhs.gov/portal/server.pt/community/healthit_hhs_gov__sharp_program/1806 (accessed 31 Jul 2011). [Google Scholar]
- 2.Strategic Health IT Advanced Research Projects: Area 4 (SHARPn): Secondary Data Use and Normalization. http://sharpn.org (accessed 31 Jul 2011).
- 3.eMERGE https://www.mc.vanderbilt.edu/victr/dcc/projects/acc/index.php/Main_Page (accessed 31 2011).
- 4.McCarty C, Chisholm R, Chute C, et al. The eMERGE network: a consortium of biorepositories linked to electronic medical records data for conducting genomic studies. BMC Medical Genomics 4 2011. doi:10.1186/1155-8794-4-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.PGRN http://www.nigms.nih.gov/Initiatives/PGRN (accessed 31 Jul 2011).
- 6.Wilke R, Xu H, Denny J, et al. The emerging role of the electronic medical records in pharmacogenomics. Clin Pharmacol Ther 2011;89:379–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schroth W, Goetz M, Hamann U, et al. Association between CYP2D6 polymorphisms and outcomes among women with early stage breast cancer treated with tamoxifen. JAMA 2009;302:1429–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chute C, Beck S, Fisk T, et al. The enterprise data trust at mayo clinic: a semantically integrated warehouse of biomedical data. J Am Med Inform Assoc 2010;17:131–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murphy S, Weber G, Mendis M, et al. Serving the enterprise and beyond with informatics for integrating biology and the bedside (i2b2). J Am Med Inform Assoc 2010;17:124–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jha A. The promise of electronical records: around the corner or down the road? J Am Med Assoc 2011;306:880–1 [DOI] [PubMed] [Google Scholar]
- 11.Savova G, Masanz J, Ogren P, et al. Mayo clinical Text Analysis and Knowledge Extraction System (cTAKES): architecture, component evaluation and applications. J Am Med Inform Assoc 2010;17:507–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kullo I, Fan J, Pathak J, et al. Leveraging informatics for genetic studies: use of the electronic medical record to enable genome-wide association study of peripheral arterial disease. J Am Med Inform Assoc 2010;17:568–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Savova G, Ogren P, Duffy P, et al. Mayo clinic system for patient smoking status classification. J Am Med Inform Assoc 2008;15:25–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Savova G, Clark C, Zheng J, et al. The mayo/MITRE system for discovery of obesity and its comorbidities. In: 2nd i2b2 Challenge Workshop. Washington, DC: American Medical Informatics Association Annual Symposium, 2008 [Google Scholar]
- 15.Cheng L, Zheng J, Savova G, et al. Discerning tumor status from unstructured MRI reports—completeness of information in existing reports and utility of natural language processing. J Digit Imaging 2010;23:119–32 PMID: 19484309. http://www.ncbi.nlm.nih.gov/pubmed/19484309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Unified Medical Language System (UMLS) http://www.nlm.nih.gov/research/umls/ (accessed 31 Jul 2011).
- 17.SNOMED CT http://www.nlm.nih.gov/research/umls/Snomed/snomed_main.html (accessed 31 Jul 2011).
- 18.RxNorm http://www.nlm.nih.gov/research/umls/rxnorm/ (accessed 31 Jul 2011).
- 19.OpenNLP http://opennlp.sourceforge.net/index.html (accessed 31 Jul 2011).
- 20.LVG http://SPECIALIST.nlm.nih.gov (accessed 31 July 2011).
- 21.Chapman W, Bridewell W, Hanbury P, et al. A simple algorithm for identifying negated findings and diseases in discharge summaries. J Biomed Inform 2001;34:301–10 [DOI] [PubMed] [Google Scholar]
- 22.Choi J, Nicolov N. K-best, transition-based dependency parsing using robust minimization and automatic feature reduction. Collections of multilinguality and interoperability in language processing with emphasis on Romanian. 2010:288–302 http://www.racai.ro/Multilinguality%20and%20Interoperability/14.html [Google Scholar]
- 23.Sohn S, Savova G. Mayo Clinic Smoking Status Classification System. San Francisco, CA: American Medical Informatics Association Annual Symposium, 2009:619–23 [PMC free article] [PubMed] [Google Scholar]
- 24.UIMA http://uima.apache.org (accessed 31 Jul 2011).
- 25.NDF-RT http://www.nlm.nih.gov/research/umls/sourcereleasedocs/2008AB/NDFRT/ (accessed 31 Jul 2011).
- 26.National Library of Medicine Unified Medical Language System. 2010. https://login.nlm.nih.gov/cas/login?service=http://umlsks.nlm.nih.gov/uPortal/Login (accessed 31 Jul 2011). [Google Scholar]
- 27.Savova G, Bethard S, Styler W, et al. Towards Temporal Relation Discovery From The Clinical Narrative. San Francisco, CA: American Medical Informatics Association Annual Symposium, 2009 [PMC free article] [PubMed] [Google Scholar]