Abstract
The Hub Population Health System enables the creation and distribution of queries for aggregate count information, clinical decision support alerts at the point-of-care for patients who meet specified conditions, and secure messages sent directly to provider electronic health record (EHR) inboxes. Using a metronidazole medication recall, the New York City Department of Health was able to determine the number of affected patients and message providers, and distribute an alert to participating practices. As of September 2011, the system is live in 400 practices and within a year will have over 532 practices with 2500 providers, representing over 2.5 million New Yorkers. The Hub can help public health experts to evaluate population health and quality improvement activities throughout the ambulatory care network. Multiple EHR vendors are building these features in partnership with the department's regional extension center in anticipation of new meaningful use requirements.
Keywords: Decision support systems, clinical, public health informatics, population surveillance, electronic health records, medical informatics, developing/using computerized provider order entry, methods for integration of information from disparate sources, distributed systems, agents, software engineering: architecture, PCIP, ambulatory care, new york city, cardiovascular disease, food environment, population health
Background
Traditionally, public health departments have gathered information concerning infectious disease outbreaks through mandated provider reporting and chronic disease burden through in-depth interviews of afflicted patients. These methods are costly and resource intensive (eg, the Health and Nutrition Examination Surveys) and require years of planning and execution to carry out.1 2 Additionally, reportable disease registries, birth/death statistics, syndromic surveillance, immunization reporting, etc, tend to be stored in specific program areas, making them difficult to use across a health department.3–8 These approaches cannot respond quickly enough to evolving public health priorities and new discoveries in healthcare. They do not provide a ‘real-time’ assessment of the comprehensive needs of a community and are therefore difficult to use for program planning and resource allocation. More innovative approaches are needed that focus on integrating public health priorities directly into the clinical provider's workflow using the electronic health record (EHR).9 10
In order to develop a system that will allow the flexibility to investigate and monitor unanticipated acute events, respond to changing public health needs around chronic disease burdens, and identify causative agents in a timely manner, the New York City Department of Health and Mental Hygiene (DOHMH) has worked to develop a public health-oriented EHR. Combining the EHR with ad hoc query and alert features would allow public health officials to quickly determine disease burden or investigate outbreaks by geographic zip code, comorbidities, race/ethnicity, etc, and give them a clinical action arm to influence chronic disease care services throughout the community. Furthermore, combining clinical information with additional city health data sources could form the basis for a population heath record for monitoring community health as envisioned by the AMIA Board of Directors in 1997 and reiterated by Friedman et al in 2010.11 12
Methods
Setting
The Primary Care Information Project (PCIP) is a bureau within the DOHMH formed in 2005 with the mission to develop and implement a public health-enabled EHR in ambulatory primary care practices serving the medically underserved.13 14 This EHR includes an integrated decision support system based upon standardized clinical quality measure standards, real-time alerts, order sets, quality measure dashboards, ad hoc registry queries, and health information exchange capabilities.
Through a competitive procurement process, eClinicalWorks was chosen as the initial EHR vendor partner to develop these capabilities and deploy them to all participating practices. As of July 2011, PCIP has implemented the EHR in 532 practices whose 2506 providers serve an estimated 2.5 million patients in 4.8 million encounters per year. These practices range in size from solo practitioners to large, multi-site, 100+ provider community health centers. As PCIP has begun expanding its operations to include regional extension center activities, additional EHR vendor partners and their associated practices are also being added to the program.
System overview
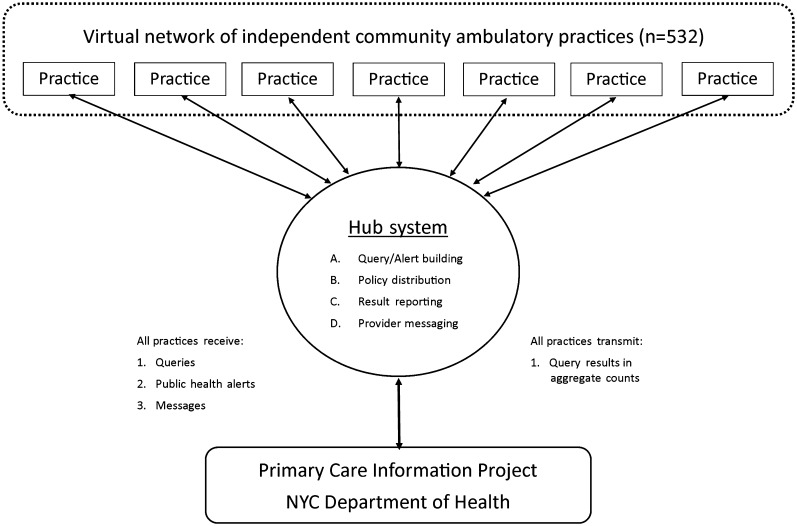
The Hub Population Health System (Hub) was built as a joint collaboration between PCIP and eClinicalWorks beginning in November 2009. Unlike large integrated healthcare delivery systems, PCIP practices are part of a ‘virtual network’ of distributed independent ambulatory practices (see figure 1). Each individual EHR clinical data repository connects on a nightly basis to a central server (the Hub), hosted by the vendor, to receive and transmit information using a secured HTTPS connection. All information is summarized at the aggregate count level before transmission to the Hub. This helps to protect patient privacy by limiting the information shared between institutions, a strategy which has been described in depth by other researchers.15–17 Data from the Hub are downloaded nightly to a secured data warehouse hosted by PCIP. All practices sign data sharing agreements which permit the sharing and use of this aggregate data with PCIP. No aggregate data with practice identifiers are shared with third parties unless specifically authorized to do so by practices.
Figure 1.
Hub system architecture for a virtual network of practices.
The Hub Population Health System provides four primary services to authorized users. First, it permits the distribution of SQL query reports for aggregate count information and EHR point-of-care decision support alerts. Second, it enables the distribution of the reports/alerts to any practice in the network according to defined reporting policies. Third, it provides an interface for viewing and downloading aggregate results reported from the queries run on each of the practices. Fourth, it has the ability to securely message providers directly in their EHR inbox.
As of September 2011, there were 400 Hub-enabled practices, covering 1.6 million patients. A total of 736 unique queries have returned 220 406 results from these practices. The maximum number of queries run by one practice in a single day was 177. A number of error conditions have been reported, including practice installation/configuration issues, MySQL/SQL Server SQL query incompatibilities, and missing transmissions, particularly on weekends/holidays.
Query/alert building
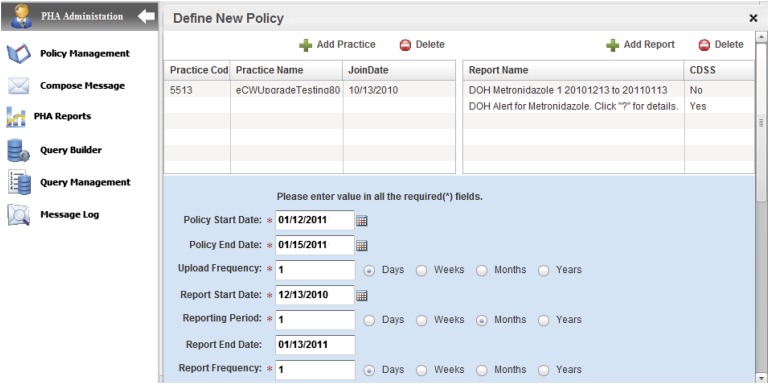
Figure 2 shows the primary navigation panel for the Hub. It illustrates the creation of a new policy with metronidazole reports and a decision support alert. Each report requires a name, description, SQL query code, and decision support flag. The name uniquely identifies each report and serves as the primary alert text (eg, DOH Alert for Metronidazole. Click “?” for details) when the decision support flag is enabled. The description provides additional details to the clinician about the query/alert and an email address for follow-up questions.
Figure 2.
Distribution of a new policy with metronidazole reports and alert (eClinicalWorks).
The SQL query code is generated by public health domain experts leveraging the EHR's Registry reporting tool which has a GUI interface for entering patient characteristics including demographics, medications, diagnoses, etc. The output of this tool is automatically extracted and formatted to be compatible with the Hub using a PCIP-built JAVA plugin called the ‘Phactory’. The combination of these tools creates a process for Hub users to create a wide range of queries with no SQL programming expertise required. More advanced queries are manually written by PCIP analysts; however, future enhancements to the Phactory will automate much of this work.
Policy distribution
Each report is attached to a policy which contains all the reporting metadata. A policy identifies which practices will run the report, the policy start and end dates, the frequency at which the results will be uploaded to the central hub, the report start and end dates, and report frequency. In figure 2, the policy's reports will upload results every day from January 12 to January 15.
On a nightly basis, each practice's EHR system runs a scheduled job that connects over HTTPS to the central Hub server hosted by eClinicalWorks (see figure 1). New policies are downloaded and executed against the local practice's EHR database, and the results are transmitted back to the Hub server. If a policy has expired, it is marked as inactive in the local practice database. Errors in query execution are automatically sent via email to a PCIP administrative account for corrective follow-up action.
All currently active policies for a given practice are displayed in the Registry Reports section of their EHR. A provider can read the report description and email the Hub administrator with any follow-up questions. If an alert has been assigned, it will appear on the right panel of the screen when the provider is documenting in the progress note of a patient meeting the criteria. The alert text can include follow-up links to relevant provider/patient educational material, disease reporting websites, provider surveys, etc, based upon the suggested intervention. The alert will disappear once the appropriate follow-up action is taken (eg, ordering a laboratory test) or the alert's policy expires. Currently the alerts are text-based, but future enhancements will allow direct action through computerized physician order entry.
Result reporting
The Reports section contains all of the results from policies which have been assigned. There are options to filter the data by practice, report name, and reporting date. This information is exported as an Excel file for upload to the PCIP data warehouse for further analytic work. This file contains a unique practice identifier, practice name, report identifier, report name, report run date, report period start and end dates, and the report count. Future enhancements to the system will include automated exporting of the data via web services.
Provider messaging
Finally, the Hub system permits secure messaging of targeted practices using HTML-formatted messages. Messages are delivered to the primary practice provider's inbox used for secure internal practice communication. Each message can be assigned a priority which marks the message as Routine, Urgent, and Emergent. A Message Log page is used to track all messages transmitted to the practices.
Pilot evaluations
Alert campaigns for public health emergencies
Since we can tailor the distribution and timing of the alerts to specific practices for specific times, we can conduct targeted ‘alert campaigns’ that will have optimal clinical impact while minimizing the potential for alert fatigue, which has been studied previously.9 18 We tested such a campaign using a drug recall issued by the CDC for metronidazole, an antibiotic commonly used to treat specific infections in the outpatient setting.
On January 6, 2011, the FDA recalled underweight metronidazole tablets.19 On January 12, the DOHMH Health Alert Network distributed a clinical notification describing the recall.20 Using this recall notification, clinical and public health experts distributed queries to two pilot practices that same evening. The reports returned a count of 62 patients in six stratified time periods who were prescribed metronidazole in the last year.
A secure follow-up message was sent on January 14 to the providers' inboxes embedded in the EHR that included the specifics of the recall, as well as step-by-step instructions on how to use the EHR's Registry function to identify the affected patients for purposes of patient notification. The message also included a hyperlink to the FDA's MedWatch website with detailed information on the recall.
After reviewing the data, a clinical decision support alert entitled ‘DOH Alert for Metronidazole’ was activated from January 19, 2011 to February 19, 2011. For any patient prescribed metronidazole in these two practices in the last 60 days, the alert appeared in the right pane of the progress note documentation screen. The pop-up information window contained the text of the recall, pertinent hyperlinks, and a reminder to review the longer inbox message.
After the message and alert were distributed, we spoke with three providers to understand the caregiver's perspective. Two providers had read the message and used the hyperlinks to read further information about the recall. Also two of the providers saw the progress note alert and agreed that it was useful and informative. The third provider, who had not seen the alert, agreed that receiving these types of interventions would be useful once a week and during an emergency. One provider agreed strongly that the alert changed the way he/she practiced medicine in reacting to this recall. Although this application of queries and alerts was extremely exploratory, it suggests the potential of this interactive technology to improve the way health departments gauge the severity of public health emergencies and connect with providers to deal with them.
Population health analysis
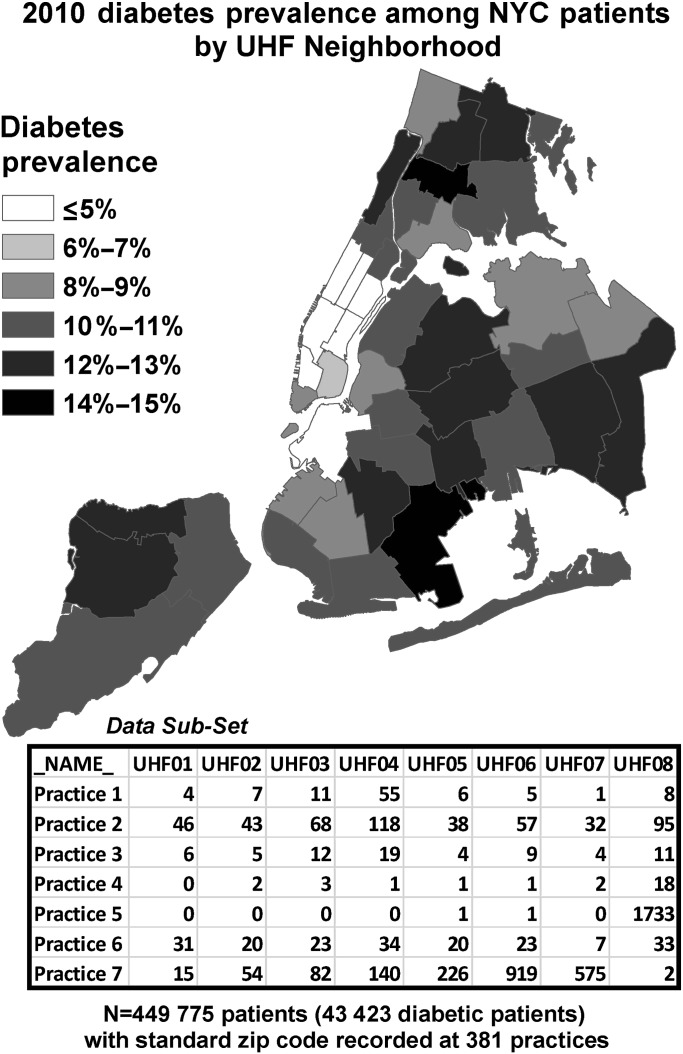
The query feature of the Hub can also be used to examine the distribution of disease on a population level and to inform program planning in real time. As an example, we probed the utility of aggregate count data for public health by looking at neighborhood-level diabetes prevalence among PCIP patients. Our denominator was patients seen in 2010 with a standard NYC zip code, organized into United Hospital Fund (UHF) neighborhoods. Our numerator was the subset of those patients with an ICD-9 code for diabetes on the problem list in 2010.
From August 22 to September 12, 2011, we queried 386 small practices for the numerator and denominator in each UHF neighborhood. These queries returned 28 993 distinct results representing 4 49 775 patients at 381 responder practices, 43 423 of whom had a diagnosis of diabetes. There were an additional 158 error values. To deal with missing values, we allowed only practices with a complete pair of numerator and denominator data for a given neighborhood to contribute to the prevalence estimate for that neighborhood. We transformed the data into numerator/denominator variables, with one observation per practice, aggregating them into neighborhood-level counts and mapping that prevalence (figure 3). While this form of analysis does not achieve the results that more sophisticated multi-level modeling may yield, aggregate geographic information like this is both applicable and essential to health departments trying to target resources where they are most needed.
Figure 3.
Illustration of geographic population health analysis with the Hub.
Discussion
By the first quarter of 2012, the Hub system will cover nearly 2.5 million New Yorkers, or almost 30% of the 8.4 million residents in NYC. PCIP is working to extend the Hub to additional EHR vendor partners, which will enable greater coverage of the NYC ambulatory patient population. This is a significant patient population in which to monitor healthcare outcomes and intervene in near real-time on critical priorities using public health alerts. Through the Hub system, the Health Department can investigate population health issues without clinical or vendor resources. This type of innovation has already had national implications—similar alerts are being considered as a required EHR feature for Meaningful Use Stage 3.21
The datasets we derive from the Hub can currently be used with classic regression techniques to examine quality of care at the practice level. More research is needed to adapt existing multi-level modeling of fixed and random effects to examine patient-level phenomena. Given the geographic component of these queries, these EHR datasets can be linked to other GIS data like air quality and census socioeconomic information to give a more complete picture of health issues and disparities throughout NYC. Eventually these de-identified datasets may even form the basis for an aggregate population health record (popHR) for monitoring health citywide.12 As Hub-like system features, such as ONC's Query Health initiative, penetrate other communities in the nationwide EHR marketplace, they could be used in conjunction with existing public health systems to form a nationwide strategy for population health monitoring and research.10 16 22–26
One important consideration of our approach is that it requires each EHR vendor to provide a separate proprietary interface for creating and sharing public health queries among practices with the same system. The alternative approach would require each EHR vendor to agree to a standardized mapping of their data to a well-defined, uniform subset.24 26 Each approach has its own limitations that should be weighed against the needs and capabilities of local public health and clinical organizations. Other potential limitations in using the Hub system to monitor population health are that the doctor-going population may not be representative of the general population and it has no way to eliminate duplicate patient counts across multiple distinct practices. More in-depth evaluations of the system to compare the Hub data to patient surveys and chart reviews as a formal validation of its quality and reliability are needed.
Acknowledgments
We would like to thank the developers and management of eClinicalWorks for their support of this project.
Footnotes
Funding: This project is funded by the New York City Department of Health and Mental Hygiene.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Thorpe LE, Gwynn RC, Mandel-Ricci J, et al. Study design and participation rates of the New York City Health and Nutrition Examination Survey, 2004. Prev Chronic Dis 2006;3:A94. [PMC free article] [PubMed] [Google Scholar]
- 2.Gwynn RC, Berger M, Garg RK, et al. Measures of adiposity and cardiovascular disease risk factors, New York City Health and Nutrition Examination Survey, 2004. Prev Chronic Dis 2011;8:A56. [PMC free article] [PubMed] [Google Scholar]
- 3.Hopkins RS. Design and operation of state and local infectious disease surveillance systems. J Public Health Manag Pract 2005;11:184–90 [DOI] [PubMed] [Google Scholar]
- 4.Dato V, Wagner MM, Fapohunda A. How outbreaks of infectious disease are detected: a review of surveillance systems and outbreaks. Public Health Rep 2004;119:464–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Loonsk JW. BioSense—a national initiative for early detection and quantification of public health emergencies. MMWR Morb Mortal Wkly Rep 2004;53(Suppl):53–5 [PubMed] [Google Scholar]
- 6.Epiquery. http://www.nyc.gov/health/epiquery (accessed 31 Mar 2011).
- 7.Heffernan R, Mostashari F, Das D, et al. New York City syndromic surveillance systems. MMWR Morb Mortal Wkly Rep 2004;53(Suppl):23–7 [PubMed] [Google Scholar]
- 8.Chamany S, Silver LD, Bassett MD, et al. Tracking diabetes: New York City's A1C Registry. Milbank Q 2009;87:547–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lurio J, Morrison FP, Pichardo M, et al. Using electronic health record alerts to provide public health situational awareness to clinicians. J Am Med Inform Assoc 2010;17:217–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klompas M, Lazarus R, Daniel J, et al. Automated public health reporting-possible with a coalition of the willing. Advances in Disease Surveillance 2007;395:1–2 [Google Scholar]
- 11.Detmer DE. Activating a full architectural model: improving health through robust population health records. J Am Med Inform Assoc 2010;17:367–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Friedman DJ, Parrish RG., 2nd The population health record: concepts, definition, design, and implementation. J Am Med Inform Assoc 2010;17:359–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Primary Care Information Project. http://www.nyc.gov/html/doh/html/pcip/pcip.shtml (accessed 30 Mar 2011).
- 14.New York City Regional Electronic Adoption Center for Health. http://www.nycreach.org (accessed 31 Mar 2011).
- 15.Diamond CC, Mostashari F, Shirky C. Collecting and sharing data for population health: a new paradigm. Health Aff (Millwood) 2009;28:454–66 [DOI] [PubMed] [Google Scholar]
- 16.Maro JC, Platt R, Holmes JH, et al. Design of a national distributed health data network. Ann Intern Med 2009;151:341–4 [DOI] [PubMed] [Google Scholar]
- 17.Lazarus R, Yih K, Platt R. Distributed data processing for public health surveillance. BMC Public Health 2006;6:235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weingart SN, Toth M, Sands DZ, et al. Physicians' decisions to override computerized drug alerts in primary care. Arch Intern Med 2003;163:2625–31 [DOI] [PubMed] [Google Scholar]
- 19.U.S. Food and Drug Administration. http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm239312.htm (accessed 5 Apr 2011).
- 20.New York City's DOHMH Health Alert Network. https://a816-healthpsi.nyc.gov/han/nychan/ (accessed 5 Apr 2011).
- 21.The Office of the National Coordinator for Health Information Technology. http://healthit.hhs.gov/media/faca/MU_RFC%20_2011-01-12_final.pdf (accessed 31 Mar 2011).
- 22.Friedman DJ. Envisioning futures for state Web-based data query systems. J Public Health Manag Pract 2006;12:196–200 [DOI] [PubMed] [Google Scholar]
- 23.Friedman DJ. Assessing the potential of national strategies for electronic health records for population health monitoring and research. National Center for Health Statistics. Vital Health Stat 2 2006;143:1–83 [PubMed] [Google Scholar]
- 24.Miller C. CDC to test actionable alerts with GE Healthcare [press release]. Orlando: GE Healthcare, 2011 [Google Scholar]
- 25.Rajeev D, Staes CJ, Evans RS, et al. Development of an electronic public health case report using HL7 v2.5 to meet public health needs. J Am Med Inform Assoc 2010;17:34–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Standards & Interoperability (S&I) Framework – Query Health. http://wiki.siframework.org/Query+Health (accessed 3 Oct 2011).