Abstract
Background
The intraocular pressures and biomechanical parameters measured by the ocular response analyzer make the analyzer a useful tool for the diagnosis and management of anterior segment disease. This observational study was designed to investigate the effect of topical anesthesia on the parameters measured by the ocular response analyzer: corneal hysteresis, corneal resistance factor, Goldmann-correlated intraocular pressure (IOPg), and corneal-compensated intraocular pressure (IOPcc).
Methods
Two sets of measurements were made for 78 eyes of 39 subjects, approximately 1 week apart. In session 1, each eye of each subject was randomized into one of three groups: polyvinyl alcohol (0.5%), tetracaine hydrochloride (0.5%), or oxybuprocaine hydrochloride (0.4%). In session 2, eyes that were in the polyvinyl alcohol group in session 1 were assigned to the tetracaine group, those in the tetracaine group in session 1 were assigned to oxybuprocaine group, and those in the oxybuprocaine group in session 1 were assigned to the polyvinyl alcohol group. For both sessions, each subject first had his or her central corneal thickness assessed with a specular microscope, followed by measurements of intraocular pressure and corneal biomechanical parameters with the Ocular Response Analyzer. All measurements were repeated for 2 minutes and 5 minutes following the instillation of either polyvinyl alcohol, tetracaine, or oxybuprocaine. The level of statistical significance was 0.05.
Results
Polyvinyl alcohol, tetracaine hydrochloride, and oxybuprocaine hydrochloride had no statistically significant (P > 0.05) effect on any of the biomechanical parameters of the cornea. There was no statistically significant effect on either IOPg (P > 0.05) or IOPcc (P > 0.05) 2 minutes after the eye drops were instilled in either session. Five minutes after the eye drops were instilled, polyvinyl alcohol showed no statistically significant effect on either IOPg (P > 0.05) or IOPcc (P > 0.05) in either session. Oxybuprocaine and tetracaine caused statistically significant (P < 0.05) reductions in IOPg in session 1, but only tetracaine had a significant (P < 0.05) effect in session 2. Tetracaine also caused a statistically significant (P < 0.05) reduction in IOPcc in session 1.
Conclusion
The statistically significant effect of topical anesthesia on IOPg varies with the anesthetic used, and while this effect was statistically significant in this study, the small effect is probably not clinically relevant. There was no effect on any of the biomechanical parameters of the cornea.
Keywords: intraocular pressure, ocular response analyzer, corneal biomechanical parameters, corneal hysteresis, corneal resistance factor, topical anesthesia
The influence of central corneal thickness (CCT) on intraocular pressure (IOP) is well documented.1–3 In 2005, Luce4 reported the measurement of corneal resistance factor (CRF) and corneal hysteresis (CH) in vivo. CRF is predominantly a measure of corneal elasticity, and CH is a measure of the viscoelastic parameters of the cornea. Both parameters are measured with the ocular response analyzer (ORA), which fires a precisely metered air pulse that indents the cornea into slight concavity. A brief moment after the cornea is applanated (on its way inward), the air jet is automatically switched off, allowing the cornea to return to its original convex shape. Consequently, the cornea passes through two applanation events – inward and outward. The difference between both applanation pressures is the corneal hysteresis. The corneal resistance factor is defined as a linear function of both applanation pressures.5 In addition to the biomechanical parameters of the cornea, the ORA also measures a corneal-compensated IOP (IOPcc) and a Goldmann-correlated IOP (IOPg). The IOPcc takes the corneal hysteresis into account so that, theoretically at least, it is independent of the viscoelastic parameters of the cornea. The IOPg is the average of both applanation pressures.
Interest in the biomechanical parameters of the cornea stem from the fact that central corneal thickness (CCT) is known to influence the IOP measured with several tonometers, including the clinical gold standard Goldmann applanation tonometer (GAT).2,6–13 Until recently, the only biomechanical parameter that could be assessed in vivo was CCT. Thus, with CH and CRF come two new parameters that could potentially be more influential than CCT on the IOP measured through the cornea.
It is thus important to know if any ORA parameters are influenced by topical anesthetic drops because these are sometimes used before IOP measurements taken with noncontact tonometers (NCTs), especially when the IOPs measured with the NCTs are being compared with devices that make contact with the cornea, thus necessitating topical anesthesia. Such studies usually use topical anesthetics and then randomize the order in which IOP measurements are made.
Ehongo et al14 investigated the effect of topical anesthesia on ORA parameters. Using both eyes of each of 23 healthy volunteers, they found that 0.4% oxybuprocaine caused statistically significant decreases in IOPcc but not in any other ORA parameter. However, the interpretation of the results of their study is limited by a relatively small sample size, the use of only one anesthetic, measurements that were taken only in one visit, and measurements that were taken at only one time point post instillation (at 2 minutes). Also, only IOPcc not IOPg was reduced, in contrast to a study15 in 2007 that reported a small but statistically significant and consistent reduction in the IOP measured with a noncontact tonometer and caused by two different anesthetics.
This study sought to address some of the shortcomings of the Ehongo et al14 study and, in light of the results of AlMubrad and Ogbuehi,15 to address the hypothesis that topical anesthetics will cause a small but statistically significant reduction of the IOPs measured with the ORA.
Methods
Before inclusion in this study, both eyes of each potential subject were subjected to a comprehensive ophthalmological exam, including slit-lamp biomicroscopy, ophthalmoscopy, visual acuity, refraction, and static perimetry, using the central 30-2 configuration on the Humphrey’s automated perimeter. Exclusion criteria were any observable sign or positive history for anterior segment disease or surgery, positive history for intraocular surgery, contact lens wear, prescribed topical medication, or a corneal cylinder ≥4.00DC. Thirty- nine subjects (21 men) completed this study, down from 42 subjects who were selected to participate. In addition to the three subjects lost to follow up, three subjects were excluded from participation (one for contact lens wear and two because of prior laser-assisted in situ keratomileusis (LASIK) surgeries). The ages of the subjects ranged from 20 to 29 years with a mean age (±SD) of 22 (±2) years. Following a detailed explanation of the study and the rights of the subjects who agree to participate, informed consent was obtained from each subject in accordance with the 1975 Helsinki Declaration, as modified in Edinburgh 2000. The study protocol was approved by the research ethics review board of the College of Applied Medical Sciences, King Saud University.
Using a table of random numbers generated on Microsoft Excel, each eye of each subject was randomized into one of three groups in the first measurement session: polyvinyl alcohol (0.5%), tetracaine hydrochloride (0.5%), or oxybuprocaine hydrochloride (0.4%). The groups were not matched for sex or age because, with the narrow age range of the subjects selected for this study, neither age nor sex has been shown to have a significant influence on any of the parameters measured by the ORA. All eye drops were in single dose unit form and were thus preservative free. On the second visit approximately 4 days later, the groups were changed to determine the reproducibility of any observed effects; eyes that were in the polyvinyl alcohol group in session 1 were assigned to the tetracaine group in session 2, those in the tetracaine group in session 1 were assigned to the oxybuprocaine group, and those in the oxybuprocaine group in session 1 were assigned to the polyvinyl alcohol group. In total, 78 eyes of 39 subjects were randomized into three groups, each comprising 26 eyes.
Each subject first had his or her CCT assessed with a Topcon SP3000P specular microscope (Topcon Medical Systems, Paramus, NJ), followed by measurements of IOP and corneal biomechanical parameters with the ORA ( Reichert Ophthalmic Instruments, Depew, NY). In session 2, the order of measurements was the same as in session 1.
Triplicate measurements were made with the specular microscope and averaged to get the mean CCT. Quadruplicate measurements were made with the ORA and averaged to get the mean values for CH and CRF, IOPg, and IOPcc. The four measurements made with the ORA had to be of good quality as described by Luce:4 “a good bell-shaped pressure signal with tall, relatively equal applanation peaks and relatively smooth raw and filtered applanation signals.”
For each subject in each session, the CCT and ORA measurements were repeated twice. The first set of measurements was taken and then one drop of polyvinyl alcohol (0.5%), tetracaine hydrochloride (0.5%), or oxybuprocaine hydrochloride (0.4%) was instilled into the conjunctival sac. The CCT and ORA measurements were repeated 2 minutes and 5 minutes post instillation. Measurements were all made between 12 noon and 2 pm when the IOP is known to be at its lowest and most stable.16
Statistical analyses
Repeated measures analysis of variance (RM-ANOVA) was used to compare the CCT for each eye before instillation, 2 minutes post instillation, and 5 minutes post instillation. The same comparisons were made for CH, CRF, IOPg, and IOPcc.
When a consistent (between sessions) effect on any ORA parameter was noted, a Bland-Altman17 analysis of repeatability for that parameter was assessed before instillation 2 minutes post instillation and 5 minutes post instillation to determine whether or not the effect was, at least in part, mediated by an alteration of the repeatability of the ORA measurements. The level of statistical significance for all comparisons in this study was 5%.
Results
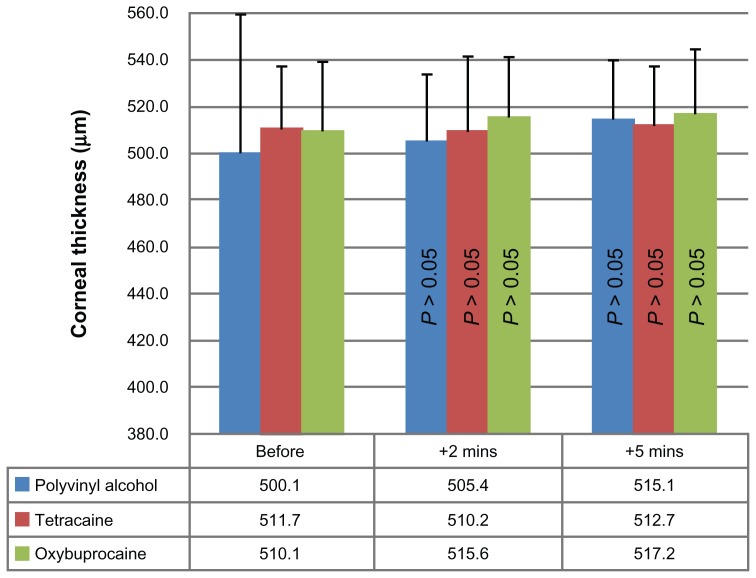
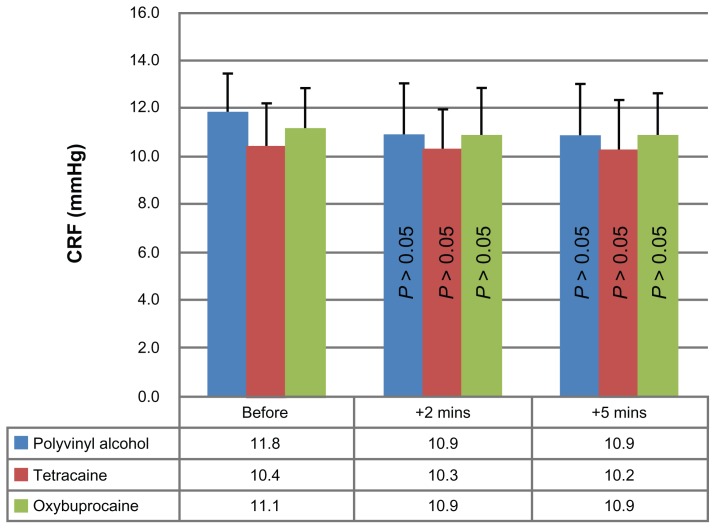
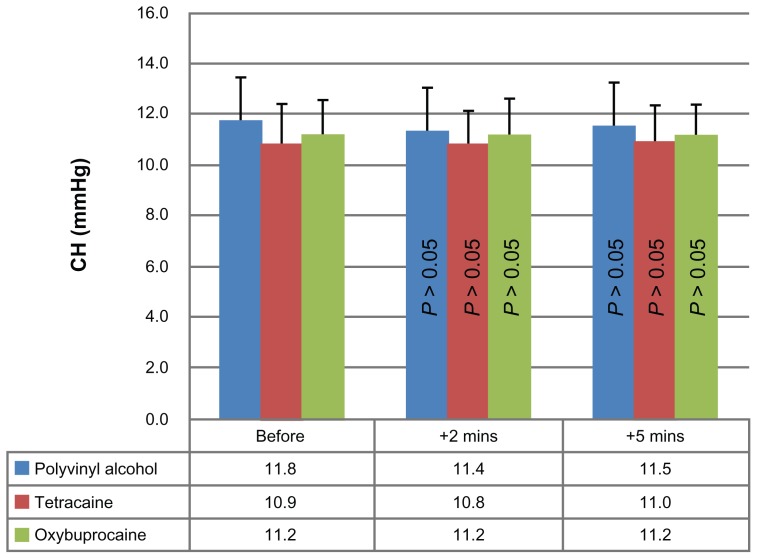
Table 1 shows the age and gender distribution among the groups. The results show that polyvinyl alcohol (control), tetracaine hydrochloride, and oxybuprocaine hydrochloride had no statistically significant effect on any of the biomechanical parameters of the cornea (CCT, CH, and CRF; Figures 1–3, respectively) in either measurement session. The results for the intraocular pressures were less clear.
Table 1.
Demographic Data of the Subjects
| All groups | Polyvinyl alcohol | Tetracaine | Oxybuprocaine | |
|---|---|---|---|---|
| Gender | 42 male eyes (36f) | 14 male eyes (12f) | 15 male eyes (11f) | 13 male eyes (13f) |
| Age (years) | 22.4 ± 2.3 | 22.7 ± 2.2 | 22.3 ± 2.2 | 22.1 ± 2.5 |
Notes: The groups are those for session 1. The ages are reported as mean ± SD Number of female eye are italicized and in brackets.
Figure 1.
Average corneal thickness values for session one before, 2 minutes after, and 5 minutes after the instillations of polyvinyl alcohol (0.5%), tetracaine hydrochloride (0.5%), and oxybuprocaine hydrochloride (0.4%).
Note: The P values are the results of repeated-measures ANOVA comparisons for each eye drop.
Abbreviation: ANOVA, analysis of variance.
Figure 3.
Average corneal resistance factor values for session one before, 2 minutes after, and 5 minutes after the instillations of polyvinyl alcohol (0.5%), tetracaine hydrochloride (0.5%), and oxybuprocaine hydrochloride (0.4%).
Note: The P values are the results of repeated-measures ANOVA comparisons for each eye drop.
Abbreviation: ANOVA, analysis of variance.
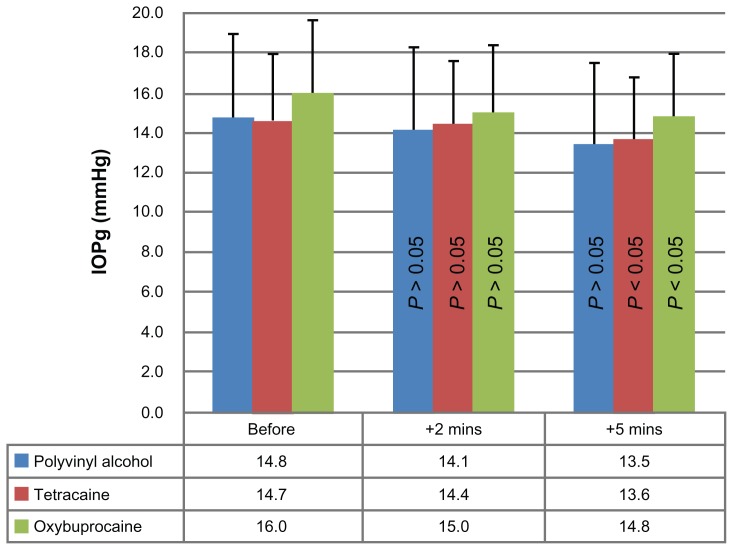
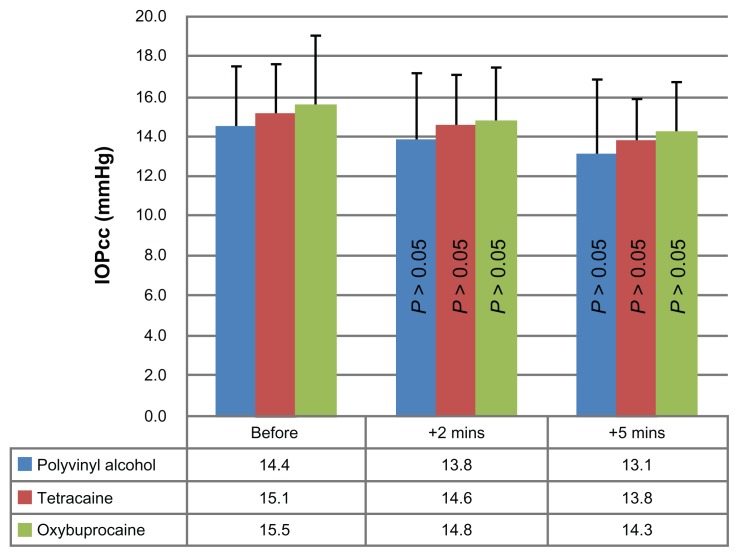
Two minutes after the eye drops were instilled, there was no statistically significant effect on either IOPg (P > 0.05) or IOPcc (P > 0.05) for polyvinyl alcohol, tetracaine hydrochloride, or oxybuprocaine hydrochloride in either session (Figures 4 and 5).
Figure 4.
Average Goldmann-correlated IOP values for session one before, 2 minutes after, and 5 minutes after the instillations of polyvinyl alcohol (0.5%), tetracaine hydrochloride (0.5%), and oxybuprocaine hydrochloride (0.4%).
Note: The P values are the results of repeated-measures ANOVA comparisons for each eye drop.
Abbreviations: ANOVA, analysis of variance; IOP, intraocular pressure.
Figure 5.
Average corneal-compensated IOP values for session one before, 2 minutes after, and 5 minutes after the instillations of polyvinyl alcohol (0.5%), tetracaine hydrochloride (0.5%), and oxybuprocaine hydrochloride (0.4%).
Note: The P values are the results of repeated-measures ANOVA comparisons for each eye drop.
Abbreviations: ANOVA, analysis of variance; IOP, intraocular pressure.
Five minutes after the eye drops were instilled, polyvinyl alcohol showed no statistically significant effect on either IOPg (P > 0.05) or IOPcc (P > 0.05) in either session. Oxybuprocaine hydrochloride caused a statistically significant (P < 0.05) reduction in IOPg in session 1 only. It had no effect on IOPcc in either session 1 or session 2. Tetracaine hydrochloride caused statistically significant reductions in IOPg in both sessions (P < 0.05). Tetracaine hydrochloride also caused a statistically significant (P < 0.05) reduction in IOPcc in session 1 but not in session 2.
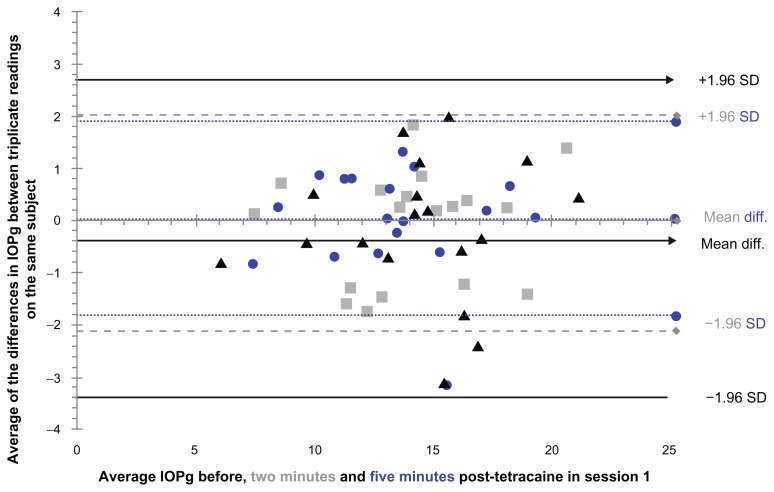
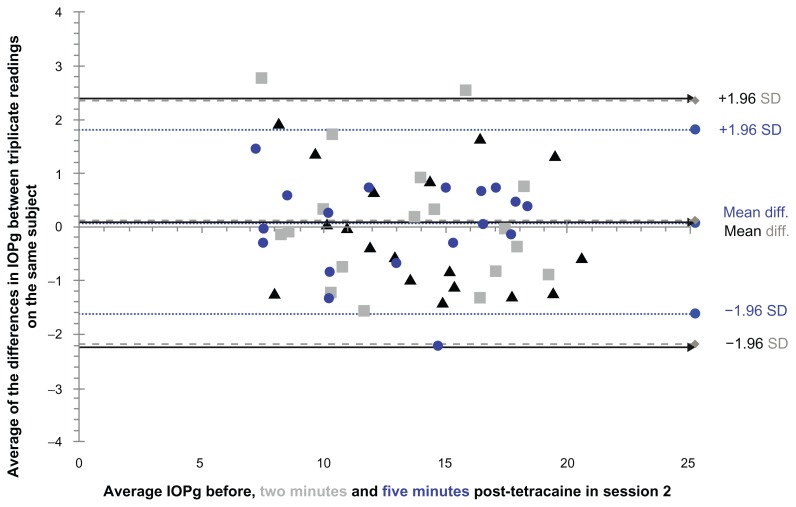
The limits of repeatability (LoR) for IOPg in session 1 (Figure 6) and session 2 (Figure 7) showed that LoR was reduced by tetracaine hydrochloride in both sessions. In session 1, the LoR was reduced at both the 2 minute and 5 minute post-instillation time points, while in session 2 the LoR was reduced by tetracaine hydrochloride only at the 5 minute post-instillation time point.
Figure 6.
Limits of repeatability for the Goldmann-correlated IOP before (solid black lines with arrow heads), 2 minutes post-instillation (dotted gray lines with diamond heads), and 5 minutes post instillation (dotted lines with round heads) of tetracaine hydrochloride (0.5%) in session 1.
Abbreviation: IOP, intraocular pressure.
Figure 7.
Limits of repeatability for the Goldmann-correlated IOP before (solid black lines with arrow heads), 2 minutes post instillation (dotted gray lines with diamond heads), and 5 minutes post instillation (dotted lines with round heads) of tetracaine hydrochloride (0.5%) in session 2.
Abbreviation: IOP, intraocular pressure.
Discussion
The results from this study showed that the topical anesthetics tetracaine hydrochloride (0.5%) and oxybuprocaine hydrochloride (0.4%) did not have any effect on CH, CRF, CCT or IOPcc. However, there were significant effects on IOPg, with tetracaine causing this effect in both measurement sessions but oxybuprocaine causing it only in one session. The results also showed that the effect on IOPg was caused in part by a reduction of the LoR for the IOPg measurements. Polyvinyl alcohol (0.5%) used as control eye drops did not cause any statistically significant change to CCT, CH, CRF, IOPcc, or IOPg.
Topical anesthetics have been reported to cause a significant reduction in the IOP measured with noncontact tonometers. 15 A possible explanation for these effects was that this reduction could have been the result of a tear film destabilization caused by preservatives in the topical anesthetics as theorized by Cho and Brown18 and by Blades et al.19 However, all the drops used in this study were in the form of single dose units and were thus preservative free. It seems unlikely, therefore, that the IOP-reducing effect of topical anesthesia is mediated via tear film destabilization caused by preservatives. It is possible that a decrease in eyelid tension induced by topical anesthesia could explain the reduction in IOPg,14 but that still leaves the questions of why the IOPcc was not affected and why oxybuprocaine hydrochloride caused a decrease in IOPg only in one session. Ehongo et al14 found discrepancies in the way CRF was altered by topical anesthesia in the right eye versus the left eye of the same subjects. Ogbuehi and AlMubrad20 found that IOPcc and IOPg read higher than the Goldmann tonometer in one measurement session, and in another session (about 1 week later), both ORA IOPs read lower than the Goldmann. In addition, those authors reported repeatability coefficients (1.96 SDmean difference) that were much higher for the ORA IOPs than for the Goldmann tonometer and another noncontact tonometer. Also in the same study, the LoR between sessions for the ORA IOPs showed a much greater variation than the LoR for the Goldmann tonometer or the other noncontact tonometer. These findings suggest that the variation in ORA IOP measurements is such that the IOP measured with the ORA may lack short-(repeatability) and long-( reproducibility) term consistency. This would explain the findings of Ehongo et al14 concerning CRF and those in this study concerning the inconsistent effect of tetracaine hydrochloride on IOPcc and the inconsistent effect oxybuprocaine hydrochloride had on IOPg between sessions.
The results from the current study agree well with those of Baudouin and Gastaud21 and AlMubrad and Ogbuehi15 in which the average reductions measured after 2 minutes were 0.76 mmHg and 0.7 mmHg (respectively, for Baudouin and Gastaud21 and for AlMubrad and Ogbuehi15) compared with 0.5 mmHg in this study. At the 5 minute time point, the average reductions in IOP were 1.19 mmHg and 0.9 mmHg, respectively, for Baudouin and Gastaud21 and for AlMubrad and Ogbuehi15 compared to 1 mmHg in this study.
In conclusion, the results from this study show that topical anesthesia affects the Goldmann-correlated IOP measured by the ORA but not the corneal-compensated IOP or the corneal biomechanical parameters. The effect of topical anesthesia varies with the anesthetic used, and while this effect was measured as statistically significant in this study, it is small enough that it is probably not clinically relevant.
The limitations of this study are a relatively small sample size and poor generalizability to the wider population because only young oculovisually normal subjects were selected for this study.
Figure 2.
Average corneal hysteresis values for session one before, 2 minutes after, and 5 minutes after the instillations of polyvinyl alcohol (0.5%), tetracaine hydrochloride (0.5%), and oxybuprocaine hydrochloride (0.4%).
Note: The P values are the results of repeated-measures ANOVA comparisons for each eye drop.
Abbreviation: ANOVA, analysis of variance.
Acknowledgments
The author is grateful to Dr Uchechukwu Osuagwu and Professor Turki AlMubrad for their critical appraisal of this manuscript.
Footnotes
Disclosure
The author reports no conflicts of interest in this work
References
- 1.Whitacre MM, Stein RA, Hassanein K. The effect of corneal thickness on applanation tonometry. Am J Ophthalmol. 1993;115(5):592–596. doi: 10.1016/s0002-9394(14)71455-2. [DOI] [PubMed] [Google Scholar]
- 2.Doughty MJ, Zaman ML. Human corneal thickness and its impact on intraocular pressure measures: a review and meta-analysis approach. Surv Ophthalmol. 2000;44(5):367–408. doi: 10.1016/s0039-6257(00)00110-7. [DOI] [PubMed] [Google Scholar]
- 3.Liu J, Roberts CJ. Influence of corneal biomechanical parameters on intraocular pressure measurement: quantitative analysis. J Cataract Refract Surg. 2005;31(1):146–155. doi: 10.1016/j.jcrs.2004.09.031. [DOI] [PubMed] [Google Scholar]
- 4.Luce DA. Determining in vivo biomechanical parameters of the cornea with an ocular response analyzer. J Cataract Refract Surg. 2005;31(1):156–162. doi: 10.1016/j.jcrs.2004.10.044. [DOI] [PubMed] [Google Scholar]
- 5.Pepose JS, Feigenbaum SK, Qazi MA, Sanderson JP, Roberts CJ. Changes in corneal biomechanics and intraocular pressure following LASIK using static, dynamic and noncontact tonometry. Am J Ophthalmol. 2007;143:39–47. doi: 10.1016/j.ajo.2006.09.036. [DOI] [PubMed] [Google Scholar]
- 6.Foster PJ, Baasanhu J, Alsbirk PH, Munkhbayar D, Uranchimeg D, Johnson GJ. Central corneal thickness and intraocular pressure in a Mongolian population. Ophthalmology. 1998;105(6):969–973. doi: 10.1016/S0161-6420(98)96021-3. [DOI] [PubMed] [Google Scholar]
- 7.Bhan A, Browning AC, Shah S, Hamilton R, Dave D, Dua HS. Effect of corneal thickness on intraocular pressure measurements with the pneumotonometer, Goldmann applanation tonometer, and Tono-Pen. Invest Ophthalmol Vis Sci. 2002;43(5):1389–1392. [PubMed] [Google Scholar]
- 8.Morgan AJ, Harper J, Hosking SL, Gilmartin B. The effect of corneal thickness and corneal curvature on pneumatonometer measurements. Curr Eye Res. 2002;25(2):107–112. doi: 10.1076/ceyr.25.2.107.10162. [DOI] [PubMed] [Google Scholar]
- 9.Aakre BM, Doughty MJ, Dalane OV, Berg A, Aamodt Ø, Gangstad H. Assessment of reproducibility of measures of intraocular pressure and central corneal thickness in young white adults over a 16-h time period. Ophthalmic Physiol Opt. 2003;23(3):271–283. doi: 10.1046/j.1475-1313.2003.00117.x. [DOI] [PubMed] [Google Scholar]
- 10.Li J, Herndon LW, Asrani SG, Stinnett S, Allingham RR. Clinical comparison of the Proview eye pressure monitor with the Goldmann applanation tonometer and the Tonopen. Arch Ophthalmol. 2004;122(8):1117–1121. doi: 10.1001/archopht.122.8.1117. [DOI] [PubMed] [Google Scholar]
- 11.Sullivan-Mee M, Pham F. Correspondence of Tono-Pen intraocular pressure measurements performed at the central cornea and mid-peripheral cornea. Optometry. 2004;75(1):26–32. doi: 10.1016/s1529-1839(04)70008-1. [DOI] [PubMed] [Google Scholar]
- 12.Doughty MJ, Jonuscheit S. Effect of central corneal thickness on Goldmann applanation tonometry measures – a different result with different pachymeters. Graefes Arch Clin Exp Ophthalmol. 2007;245(11):1603–1610. doi: 10.1007/s00417-007-0601-x. [DOI] [PubMed] [Google Scholar]
- 13.Francis BA, Hsieh A, Lai MY, et al. Los Angeles Latino Eye Study Group. Effects of corneal thickness, corneal curvature, and intraocular pressure level on Goldmann applanation tonometry and dynamic contour tonometry. Ophthalmology. 2007;114(1):20–26. doi: 10.1016/j.ophtha.2006.06.047. [DOI] [PubMed] [Google Scholar]
- 14.Ehongo A, De Maertelaer V, Pourjavan S. Effect of topical corneal anaesthesia on ocular response analyzer parameters: pilot study. Int Ophthalmol. 2009;29(5):325–328. doi: 10.1007/s10792-008-9239-x. [DOI] [PubMed] [Google Scholar]
- 15.AlMubrad TM, Ogbuehi KC. Clinical investigation of the effect of topical anaesthesia on intraocular pressure. Clin Ophthalmol. 2007;1(3):305–309. [PMC free article] [PubMed] [Google Scholar]
- 16.Liu JH, Kripke DF, Twa MD, et al. Twenty-four-hour pattern of intraocular pressure in the aging population. Invest Ophthalmol Vis Sci. 1999;40(12):2912–2917. [PubMed] [Google Scholar]
- 17.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8(2):135–160. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- 18.Cho P, Brown B. The effect of benoxinate on the tear stability of Hong Kong-Chinese. Ophthalmic Physiol Opt. 1995;15(4):299–304. [PubMed] [Google Scholar]
- 19.Blades KJ, Murphy PJ, Patel S. Tear thinning time and topical anesthesia as assessed using the HIRCAL grid and the NCCA. Optom Vis Sci. 1999;76(3):164–169. doi: 10.1097/00006324-199903000-00016. [DOI] [PubMed] [Google Scholar]
- 20.Ogbuehi KC, AlMubrad TM. Evaluation of the intraocular pressure measured with the ocular response analyzer. Curr Eye Res. 2010;35(7):587–596. doi: 10.3109/02713681003698871. [DOI] [PubMed] [Google Scholar]
- 21.Baudouin C, Gastaud P. Influence of topical anesthesia on tonometric values of intraocular pressure. Ophthalmologica. 1994;208:309–313. doi: 10.1159/000310527. [DOI] [PubMed] [Google Scholar]