Abstract
Objective
To explore state patterns in the racial life expectancy gap.
Data Sources
The 1997–2004 Multiple Cause of Death PUF, 2000 U.S. Census.
Study Design
We calculated life expectancy at birth for black and white men and women.
Data Extraction Methods
Data were obtained by the NCHS and U.S. Census Bureau.
Principal Findings
States with small racial differences are due to higher-than-expected life expectancy for blacks or lower-than-expected for whites. States with large disparity are explained by higher-than-average life expectancy among whites or lower-than-average life expectancy among blacks.
Conclusions
Heterogeneous state patterns in racial disparity in life expectancy exist. Eliminating disparity in states with large black populations would make the greatest impact nationally.
Keywords: Life expectancy, disparity, black, United States
Blacks continue to have a shorter life expectancy than whites in the United States (Wong et al. 2002; National Center for Health Statistics 2010). The elimination of this disparity and other racial health inequities is a public health priority (Institute of Medicine of the National Academies 2003; Keppel 2007; Centers for Disease Control and Prevention 2010). Studies have identified contributors to these disparities, such as poverty, psychosocial factors, and health care quality, but the determinants of disparities remain poorly understood.
Previous studies show geographic variation in racial differences in life expectancy (Murray et al. 2006; Ezzati et al. 2008). Investigators typically measure the magnitude of disparity, with the implicit assumption that interventions should target regions with large disparities rather than those with small disparities. We hypothesize that this assumption may not be correct for all states. Specifically, the public health and policy implications for geographic variations in life expectancy should not only account for the relative difference in life expectancy between blacks and whites but also the absolute life expectancy of each group and the population size.
To explore the prevalence and patterns of racial disparities at the state level, we calculated life expectancy by race and sex for 50 states and the District of Columbia (DC). We rank ordered each state by the size of the life expectancy gap between blacks and whites, and we also examined the contribution of each state to the overall disparity in life expectancy.
Methods
Data Sources
We used 1997–2004 death certificate data from the U.S. Multiple Cause of Death public use files, which included information on race/ethnicity, sex, age at death, and state of birth, residence, and death (National Center for Health Statistics 2007a,b,c,d,e). Of the 19,180,667 deaths from 50 states and DC, we excluded 1,275,707 persons (6.7 percent) who were classified as other than non-Hispanic black or white, 69,370 (0.4 percent) whose state of residence was different from the state where their death occurred, and 1,354 persons (<0.01 percent) with missing age at death.
To determine the denominator in estimating mortality risks, we used 2000 U.S. Census data, which included individual-level geographic area of residence, race/ethnicity, sex, and age (Bureau of the Census 2000). From the 281,421,906 persons in the census data, we excluded 53,200,536 persons (18.9 percent) who were classified as other than non-Hispanic black or white.
Estimating All-Cause Mortality Risks
We estimated the 1-year risk of death for each age, race, sex, and state stratum, calculated as the number of deaths divided by the population for each stratum and averaged over the 8 years of data analyzed. Age was categorized in 1-year increments. To interpolate and extrapolate missing risk estimates for some strata and also to calculate confidence intervals, we fitted the 1-year risk estimates using a binomial regression model as a function of age, sex, race, and all two- and three-way interaction terms (Rothman, Greenland, and Lash 2008). We conducted separate regression models for each state/region.
Estimating Life Expectancy
We used the risk estimates in standard, complete life tables to calculate life expectancy for black and white men and women in each state (Preston, Heuveline, and Guillot 2001). A simulation method was used to obtain 95% confidence intervals for life expectancy estimates. Specifically, we used the variance/covariance matrix of the binomial regression model to generate 1,000 realizations of the regression coefficients. For each realization, we estimated the mortality risks for each age/sex/race stratum and calculated life expectancy. The percentile method was used to estimate the 95% confidence interval.
We calculated the racial difference in life expectancy for men and women at the national and state level. Eleven states (Alaska, Hawaii, Idaho, Maine, Montana, New Hampshire, North Dakota, South Dakota, Utah, Vermont, and Wyoming) had small numbers of blacks and as a result had missing mortality risks estimates for 20 percent or more of the race/sex/age strata. These small numbers resulted in unreliable life expectancy estimates. Therefore, we dropped these 11 states from our analysis (Tables S1 and S2). To understand each state's contribution to the disparity at the national level, we first calculated the weighted average life expectancy that took into account the proportion of the population that was black or white. We then eliminated the disparity in each state by making the life expectancy among blacks equal to the life expectancy among whites in that state and then calculating the change in the national disparity. For all analyses, we used STATA version 10 (StataCorp 2007).
Results
Racial Disparity in Every State
White–black differences in life expectancy vary by state and sex (Figures 1 and 2). The national average life expectancy is 74.79 years for white men (95% confidence interval [CI] 74.76, 74.81) and 67.66 years for black men (95% CI: 67.58, 67.74), a difference of 7.13 years (95% CI: 7.02, 7.24). The national average life expectancy is 79.84 years for white women (95% CI: 79.82, 79.86), 74.64 years for black women (95% CI: 72.21, 77.07), with a disparity of 5.20 years (95% CI: 5.09, 5.31). These results are consistent with national life expectancy estimates from the National Vital Statistics Report (Arias 2002). In every state, the racial gap in life expectancy is smaller for women than for men. For both men and women, the racial disparity in life expectancy is smallest for New Mexico (3.76 years for men, 95% CI: 1.03, 6.62; 2.45 years for women, 95% CI: −0.86, 6.06) and largest for DC (13.77 years for men, 95% CI: 13.45, 15.06; 8.55 years for women, 95% CI: 7.32, 9.65).
Figure 1.
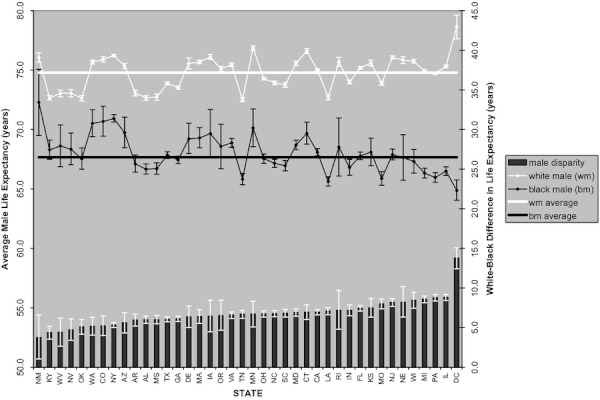
State Variation in Male Life Expectancy. The absolute life expectancy for white (white line) and black (black line) men with 95 percent error bars for the states/region analyzed. The black bars represent the racial disparity or difference in white–black life expectancy. The national average life expectancy for white men is 74.79 years, black men is 67.66 years, and a disparity of 7.13 years
Figure 2.
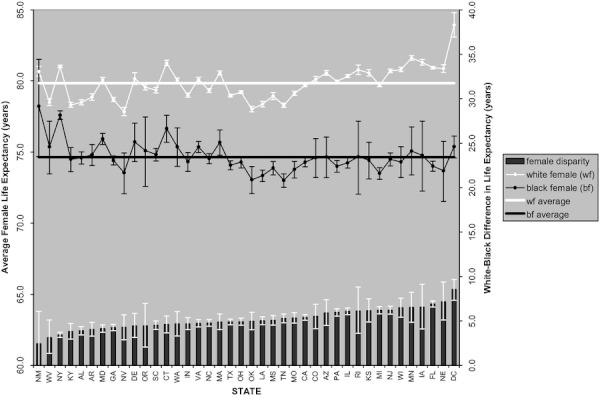
State Variation in Female Life Expectancy. The absolute life expectancy for white (white line) and black (black line) women with 95 percent error bars for the states/region analyzed. The black bars represent the racial disparity or difference in white–black life expectancy. The national average life expectancy for white women is 78.79 years, black women is 73.59 years, and a disparity of 5.20 years
States with the Smallest Racial Disparity
The nine states with the smallest gap in the racial disparity in life expectancy for men (<6 years) are New Mexico (disparity 3.76 years; 95% CI: 1.03, 6.62), Kentucky (4.37 years; 95% CI: 3.53, 5.18), West Virginia (4.42 years; 95% CI: 2.65, 6.20), Nevada (4.72 years; 95% CI: 3.39, 6.10), Oklahoma (5.10 years; 95% CI: 4.17, 6.01), Washington (5.10 years; 95% CI: 4.03, 6.30), Colorado (5.23 years; 95% CI: 3.98, 6.49), New York (5.32 years; 95% CI: 4.99, 5.64), and Arizona (5.60 years; 95% CI: 4.34, 6.89). In four states (KY, WV, NV, OK), the racial disparity is small because white men in these states have lower-than-average life expectancy, while black men have life expectancy close to their national average. In contrast, five states with a small disparity (NM, WA, CO, NY, AZ) have both black and white populations with higher-than-average life expectancy, and black men live substantially longer than the national average for blacks. States with small disparities in life expectancy are the result of two different mechanisms—white men live less than average or black men live substantially more than average. A similar explanation is seen for women. In two of the five states with the smallest racial disparity (<4 years), New Mexico and New York, black women live substantially longer than the national average. In the other three states (WV, KY, AL), white women live fewer years than the national average.
States with the Largest Racial Disparity
The states/region with the largest gap in racial life expectancy for men (>8 years) are NJ, NE, WI, MI, PA, IL, and DC. The gap is large because black men live fewer years than expected, whereas white men live equal to or longer than expected nationally. The states with the largest racial disparity in life expectancy for women are IL, RI, KS, MI, NJ, WI, MN, IA, FL, NE, and DC (>6 years). In these states, white women have higher-than-average life expectancy and black women experience lower-than-average or average life expectancy. Michigan is one exception where the life expectancy is substantially less for black women and similar to the national average for white women (disparity 6.20 years; 95% CI: 5.80, 6.62).
States with the Largest Black Populations
The 10 states with the largest black populations (NY, CA, TX, FL, GA, IL, NC, MD, MI, LA) account for 58 percent of the total black population in the United States (McKinnon 2001). More than one pattern explains the racial disparity in life expectancy in these black populous states. New York has a small gap in racial disparity because both whites and blacks live longer than expected, and blacks have a life expectancy substantially longer than the national average. In contrast, Michigan and Illinois have large disparities explained by a shorter life expectancy among blacks. Florida has a large disparity for women explained by a higher-than-average life expectancy for whites and lower-than-average life expectancy for blacks. Six states with large black populations have racial disparities that are similar to the national disparity in life expectancy (i.e., CA, TX, GA, NC, MD, LA).
When we eliminated the disparity in each state (Figure 3), we found that states with the largest black populations had the greatest impact on the national disparity. Florida has the largest impact on national disparity. The national disparity would fall from 7.13 to 6.63 years for men and from 5.20 to 4.74 years for women if Florida had no white–black disparity in life expectancy. Florida has a racial disparity in life expectancy similar to the national average for men (disparity 7.42 years; 95% CI: 7.08, 7.75) and greater than the national average for women (6.92 years; 95% CI: 6.57, 7.26). Other states that contribute substantially to the national disparity for both men and women are IL, CA, NY, TX, and GA. Among these states, Illinois has a large gap in racial disparity, whereas California, Texas, and Georgia had average gaps for men and women. In contrast, New York has a small difference in life expectancy between black and whites, but elimination of these relatively small disparities would make a comparatively big impact on reducing the national disparity for men (disparity would change from 7.13 to 6.70 years) and women (change from 5.20 to 4.91 years).
Figure 3.
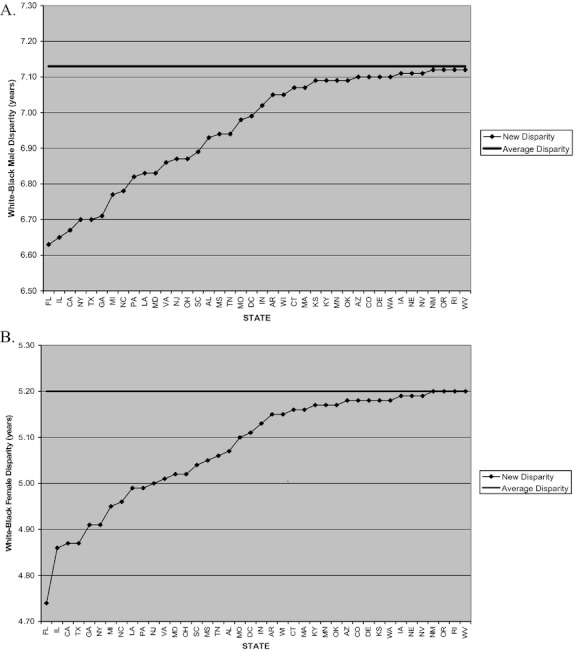
Change in National Disparity by State. The national disparity in life expectancy (LE) of the analyzed states for men is 7.13 years. The national disparity in life expectancy of the analyzed states for women is 5.20 years. The dotted line represents the new national disparity of the 40 analyzed states/regions if there was no disparity in that particular state. For example, the national disparity would drop to 6.63 years for men and 4.74 years for women if there was no racial disparity in LE in Florida. (A) men, (B) women.
Discussion
We found racial disparities in life expectancy across states with a heterogeneous pattern of absolute life expectancy for blacks and whites in each state. Several states with small disparities were not the result of black populations with longer life expectancy, but conversely, due to white populations with shorter life expectancy compared with the national average. We also found that states with large differences, while often driven by black populations living fewer years, may not make a significant contribution to the racial disparity in life expectancy at the national level. Eliminating the disparity in states with large black populations has the greatest impact nationally, even if the racial difference is modest. We argue that federal and state health policies that simply concentrate on the black–white difference in a geographic region may miss important opportunities to improve overall population health or significantly reduce disparity at the national level.
There are several policy implications in understanding the relative and absolute context of racial/ethnic disparities in health. First, federal and state agencies could consider new ways to measure and track health disparities since many disease prevention and health promotion initiatives are identified and monitored by magnitudes in a health disparity. Second, federal initiatives should consider both the relative and absolute differences in life expectancy to fund targets for regional interventions, evaluate health program outcomes, and compare disparities at the local and national levels. Similarly, state minority health offices may consider our findings to set research and funding priorities based on the needs of their local population. In some states, those priorities may be the improvement of health among blacks, while in other states the priority should be the improvement of health for both blacks and whites.
Third, paying attention to state-level differences seems an appropriate focus given that health policy is a growing concern of state governments. For example, control of Medicaid coverage and generosity of public health insurance benefits varies greatly among states. Our results possibly suggest that greater Medicaid coverage for both parents and childless adults might help to reduce health disparities. Specifically, blacks make up a disproportionate percentage of the low-income, Medicaid-eligible population, and we found that Massachusetts and New York, two states where black populations have longer-than-expected life expectancy, are also the states that have expanded Medicaid coverage (The Henry Kaiser Family Foundation 2011). States that have broader Medicaid coverage for parents but not for childless adults (e.g., CA, NJ) are states where the black and white life expectancy is similar to the national level. Interestingly, states with narrow Medicaid eligibility for adults (e.g., AL, TX) have white populations with shorter-than-expected life expectancy. Although Medicaid expansion may improve overall population health at the state level, and even reduce disparities by increasing black life expectancy, low Medicaid eligibility may potentially be contributing to low life expectancy in white populations. We did not model the impact of Medicaid coverage, and a more careful assessment of its expansion on racial/ethnic health disparities is warranted.
Our study has several limitations. We used Census 2000 data for population estimates instead of interpolating population figures using 1990 Census data and assuming a constant growth rate for 1997–1999 or using bridged-race population estimates for years 2001–2004. However, accounting for population changes in the years analyzed is unlikely to alter our results in overall trends in life expectancy and disparity. There may be differential under- or overestimation of race-specific population and mortality due to recording errors that may potentially bias life expectancy in race groups (Hahn and Eberhardt 1995). Life expectancy at birth is a weighted summary of age-specific mortality rates and is sensitive to mortality changes at young ages; analyses using other measures of population health (e.g., disability-adjusted life years) may give different results (Preston, Heuveline, and Guillot 2001). Our results did not account for the tendency of individuals to move throughout their life and mobility may be associated with other health indicators. When we limited our sample to persons whose state of death matched their state of birth and residence, the racial disparities increased, but the small number of observations in individual strata resulted in inconsistent life expectancy estimates. Another concern is that we were not able to use data from 11 states. However, these states had so few black citizens that our estimates would have been unreliable. We chose not to include socioeconomic status (SES) variables, such as education, despite research connecting racial/ethnic disparities to discrepancies in SES. Education and other measures of SES may be along a causal pathway that connects race and health, and by controlling for SES, we may not get a full picture of the extent of the disparity (Hebert, Sisk, and Howell 2008). Additionally, smaller geographic areas, such as cities (i.e., DC), may have different patterns on disparity than states. Future work may include examining the contribution of major causes of death on state-level disparities and understanding patterns and prevalence of disparities in major cities.
Simply focusing on black–white differences may disregard the wide variation in health experience of these respective populations (Morbidity, Mortality Weekly 2002; Baicker et al. 2004; Mechanic 2005; Murray et al. 2006). The most desirable outcome is a decrease in the racial disparity with a concomitant increase in the life expectancy of white and black populations. Policy discussions on racial disparities may need to be based on the needs of each state, or alternatively, on national norms for life expectancy separately for whites and blacks.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors wish to thank Martin Shapiro, M.D., Ph.D., for his help in the interpretation of the data, Patrick Heuveline, Ph.D., for his help in life table methods, and Jenny Kotlerman, Ph.D., for her help in programming codes. Dr. Bharmal was supported by the Robert Wood Johnson Clinical Scholars Program and UCLA National Service Research Award (T32 PE19001).
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Table S1. Racial Differences in Life Expectancy by State—Females.
Table S2. Racial Differences in Life Expectancy by State—Males.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Arias E. United States Life Tables, 2000: National Vital Statistics Reports. Hyattsville, MD: National Center for Health Statistic; 2002. [PubMed] [Google Scholar]
- Baicker K, Chandra A, Skinner JS, Wennberg JE. “Who You Are and Where You Live: How Race and Geography Affect the Treatment of Medicare Beneficiaries.”. Health Affairs. 2004 doi: 10.1377/hlthaff.var.33. hlthaff.var.33. [DOI] [PubMed] [Google Scholar]
- Bureau of the Census. 2000. “PCT.3 Race by Sex by Age by State. Census Summary File 4 (SF 4). American FactFinder” [accessed on October 21, 2000]. Available at http://factfinder.census.gov/servlet/DatasetMainPageServlet?_program=DEC&_submenuId=datasets_1&_lang=en.
- Centers for Disease Control and Prevention. 2010. “Racial and Ethnic Approaches to Community Health (REACH U.S.): Finding Solutions to Health Disparities” [accessed on May 16, 2010]. Available at http://www.cdc.gov/chronicdisease/resources/publications/AAG/reach.htm.
- Ezzati M, Friedman AB, Kulkarni SC, Murray CJL. “The Reversal of Fortunes: Trends in County Mortality and Cross-County Mortality Disparities in the United States”. PLoS Med. 2008;5(4):e66. doi: 10.1371/journal.pmed.0050066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn RA, Eberhardt S. “Life Expectancy in Four US Racial/Ethnic Populations: 1990”. Epidemiology. 1995;6(4):350–5. doi: 10.1097/00001648-199507000-00004. [DOI] [PubMed] [Google Scholar]
- Hebert PL, Sisk JE, Howell EA. “When Does a Difference Become a Disparity? Conceptualizing Racial and Ethnic Disparities in Health”. Health Affairs. 2008;27(2):374–82. doi: 10.1377/hlthaff.27.2.374. [DOI] [PubMed] [Google Scholar]
- The Henry Kaiser Family Foundation. 2011. “statehealthfacts.org: Medicaid & CHIP” [accessed on May 16, 2011]. Available at http://statehealthfacts.org/comparecat.jsp?cat=4&rgn=6&rgn=1.
- Institute of Medicine of the National Academies. Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- Keppel KG. “Ten Largest Racial and Ethnic Health Disparities in the United States Based on Healthy People 2010 Objectives”. American Journal of Epidemiology. 2007;166(1):97–103. doi: 10.1093/aje/kwm044. [DOI] [PubMed] [Google Scholar]
- McKinnon J. The Black Population: 2000, Census 2000 Brief. Washington, DC: U.S. Census Bureau; 2001. [Google Scholar]
- Mechanic D. “Policy Challenges in Addressing Racial Disparities and Improving Population Health”. Health Affairs. 2005;24(2):335–8. doi: 10.1377/hlthaff.24.2.335. [DOI] [PubMed] [Google Scholar]
- Morbidity, Mortality Weekly. “Infant Mortality and Low Birth Weight among Black and White Infants—United States, 1980–2000”. 2002;51(27):589–92. [PubMed] [Google Scholar]
- Murray CJL, Kulkarni SC, Michaud C, Tomijima N, Bulzacchelli MT, Iandiorio TJ, Ezzati M. “Eight Americas: Investigating Mortality Disparities across Races, Counties, and Race-Counties in the United States”. PLoS Med. 2006;3(9):e260. doi: 10.1371/journal.pmed.0030260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. Multiple Cause of Death Public Use Files, 2003. Inter-university Consortium for Political and Social Research (ICPSR); 2007a. [distributor] [Google Scholar]
- National Center for Health Statistics. Multiple Cause of Death Public Use Files, 2004. Inter-university Consortium for Political and Social Research (ICPSR); 2007b. [distributor] [Google Scholar]
- National Center for Health Statistics. Multiple Cause of Death, 1997. Inter-university Consortium for Political and Social Research (ICPSR); 2007c. [distributor] [Google Scholar]
- National Center for Health Statistics. Multiple Cause of Death, 1998. Inter-university Consortium for Political and Social Research (ICPSR); 2007d. [distributor] [Google Scholar]
- National Center for Health Statistics. Multiple Cause of Death, 1999. Inter-university Consortium for Political and Social Research (ICPSR); 2007e. [distributor] [Google Scholar]
- National Center for Health Statistics. Health, United States, 2009: With Special Feature on Medical Technology. Hyattsville, MD: National Center for Health Statistics; 2010. [PubMed] [Google Scholar]
- Preston SH, Heuveline P, Guillot M. Demography: Measuring and Modeling Population Processes. Malden, MA: Blackwell Publishers; 2001. [Google Scholar]
- Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. Philadelphia, PA: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 10. College Station, TX: StataCorp LP; 2007. [Google Scholar]
- Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. “Contribution of Major Diseases to Disparities in Mortality”. New England Journal of Medicine. 2002;347(20):1585–92. doi: 10.1056/NEJMsa012979. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


