Abstract
Objective
To translate a set of evidence-based clinical standards designed to allow paramedics to forgo unnecessary and potentially harmful resuscitation attempts into a feasible new policy.
Data Sources/Setting
Policy documents, meeting minutes, and personal communications between a large urban Emergency Medical Services (EMS) agency serving all of Los Angeles County (LAC) and a research group were reviewed over 12 months.
Study Design
LAC EMS and University of California, Los Angeles (UCLA) formed a partnership (the EMS-UCLA Collaborative) to develop and translate the standards into new EMS protocols. Clinical indicators considered appropriate and feasible by an expert panel were submitted to the agency for inclusion in the new policy.
Findings
The Collaborative submitted the results to the LAC EMS Commission and a physician advisory group for review. Of the 41 indicators approved by the expert panel, 22 would have resulted in changes to the current policy. All six involved asking family members about or honoring written and verbal Do Not Attempt Resuscitate requests, but only 4 of the 16 indicators based on clinical characteristics were included in the new policy. Ultimately, 10 of the 22 indicators that would have changed policy were approved and implemented.
Conclusions
By collaboration, a large EMS agency and a research team were able to develop and implement a revised resuscitation policy within 1 year.
Keywords: End-of-life, health policy, clinical practice guidelines, Emergency Medical Services
Many barriers exist to the translation of research to policy, and large gaps exist between evidence-based medicine and practice (Institute of Medicine [U.S.]. Committee on Quality of Health Care in America 2001). Documented obstacles to such transfer of information include limited contact between policy makers and researchers, little incentive for researchers to make their research policy-relevant, and lack of significance to the current policy environment (Jewell and Bero 2008). Dissemination of results is often limited to academic journals, which emphasize methods and limitations, rather than more easily interpretable summaries of research findings. A survey of state policy makers revealed that they receive too much information, and that the majority is neither timely nor framed in a policy-relevant manner (Sorian and Baugh 2002).
At the same time, well-documented facilitators exist to improve the policy process to incorporate up-to-date evidence. These include framing results in ways that link them to concrete impacts on costs, benefits, or specific populations, translating research results into policy-relevant products, and developing early collaborative relationships with decision makers to generate policy-relevant research (Jewell and Bero 2008). The Robert Wood Johnson Foundation's Synthesis Project was designed to strengthen the link between research and policy by having researchers synthesize evidence into readable formats that could be used by legislators and their staff (Colby et al. 2008).
Some experts have promoted community-partnered participatory research as a way to improve the relevance of research to the real world (Jones and Wells 2007). Such an approach emphasizes an equitable and long-term partnership between researchers and an outside group or community, in which knowledge is integrated and disseminated for the benefit of all involved (Ditto et al. 1996; Israel 2005; Minkler and Wallerstein 2008). It is a cyclical and iterative process by design, and the approach is tailored to the needs of the partners and the project.
In an effort to conduct research that would decrease unnecessary and potentially harmful cardiopulmonary resuscitation attempts, and facilitate subsequent translation into policy by our county, a health services research team formed an ongoing collaboration with leadership within the Los Angeles County Emergency Medical Services (LAC EMS) Agency, henceforth referred to as the EMS-UCLA Collaborative. Until 2007, when paramedics were called to the scene of a cardiac arrest, they would attempt resuscitation unless there were signs of obvious death, such as rigor mortis, or the family or nursing home staff could immediately produce a valid, written prehospital Do Not Attempt Resuscitate (DNAR) form. Most U.S. prehospital systems have not balanced the obvious potential benefits with the potential for harm when constructing policies regarding attempts at resuscitation after cardiac arrest.
Potential harms of indiscriminate resuscitation attempts include violating patient preferences, in which we resuscitate patients who would have chosen to forgo chest compressions and/or artificial respiration (Ditto et al. 1996). Attempts at resuscitation, when there is little hope for meaningful recovery, can also harm patients who may linger in intensive care settings, harm families who are often traumatized by those memories (Jones et al. 2004; Azoulay et al. 2005; Anderson et al. 2008), and could harm paramedics, emergency medical technicians (EMTs), and other providers who may experience moral and emotional conflict over providing potentially burdensome treatment to patients when they are dying (Meltzer and Huckabay 2004; Mobley et al. 2007).
In response, the EMS-UCLA Collaborative worked together to translate a set of evidence-based clinical standards, designed to allow paramedics to forgo resuscitation attempts in selected patients in whom the harm would probably exceed benefit, into a feasible policy to be implemented in the field. Elsewhere in this article, we describe the yearlong process of translating these standards into a new policy that would be appropriate and feasible to implement in the field, and that better reflected patient and family preferences. This includes a timeline and description of the members of the Collaborative and selected stakeholders, their acceptance or rejection of each standard, and the final changes to the revised policy. In addition, we explore reasons as to why stakeholders may or may not have voted to change certain types of clinical standards.
Methods
Setting
The LAC EMS Agency is one of the oldest and largest emergency medical systems in the country and coordinates all prehospital care in LAC. They make over 600,000 responses per year to 911 calls and coordinate prehospital care for 73 different hospitals. The agency utilizes a tiered response system, with over 18,000 certified EMS personnel employed by fire departments, law enforcement, ambulance companies, hospitals, and private organizations. Survival after nontraumatic cardiac arrest is low, at 1.4 percent overall (Eckstein, Stratton, and Chan 2005), although wide variability exists in outcomes by region in North America (Zive et al. 2011).
In California, counties have the primary responsibility for assuring that EMS systems are developed and implemented, and for designating a local EMS agency. In addition to planning, implementing, monitoring, and evaluating the local system, county-level EMS agencies are responsible for establishing operational policies and procedures; designating EMS base hospitals and specialty care centers; developing guidelines, standards, and protocols for patient treatment and transfer; certifying and accrediting prehospital medical care personnel; and approving EMS personnel training programs.
The LAC EMS Commission acts in an advisory capacity to the publicly elected LAC Board of Supervisors and the Director of Health Services regarding the agency's policies, programs, and standards. The EMS Commission includes representatives from the hospital, ambulance, medical, nursing, law enforcement, fire chief, and fire fighter associations, as well as a member appointed by each of the five publicly elected Board of Supervisors. Figure 1 describes the composition and organizational structure of LAC EMS in more detail.
Figure 1.
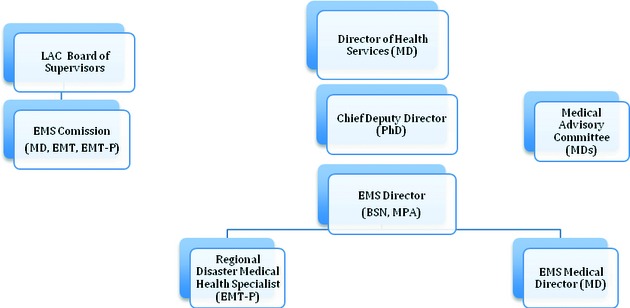
Los Angeles County Emergency Medical Services Agency Organizational Chart
Emergency Medical Service policies are routinely reviewed every 3 years, although changes to EMS policy are considered from any agency or individual at any time. The resuscitation policy, in particular, had been in place for several years and was updated regularly based on revisions to the American Heart Association guidelines. The EMS Agency Director and EMS Commission Chairperson assign new or changed policies to the appropriate subcommittees or other advisory groups (e.g., the Medical Council) for review and comment. Once the policy has been endorsed by the EMS Commission, it is signed by the EMS Agency Director and Medical Director and disseminated to EMS providers (see Figure 2).
Figure 2.

Policy Approval Process for Los Angeles County Emergency Medical Services Agency
Data Sources and Collection
The following documents were included in the analysis: final votes by the expert panel; and expired, draft, and final LAC EMS resuscitation policy documents. In addition, minutes from meetings of the EMS-UCLA Collaborative and the Medical Council, as well as personal electronic mail communications between members of the Collaborative, were reviewed.
Study Design and Analysis
We used many of the principles of participatory research, allowing the agency to identify an important problem, and co-designing a process to gather the best available evidence on the topic, with both partners involved in each step of the process. Paramedics identified the harms of indiscriminate attempts at resuscitation as an important problem in LAC. A resuscitation attempt was defined as the provision of airway support (by intubation or bag-valve mask), defibrillation, and administration of medications, including epinephrine, atropine, and antidysrhythmic agents. It was assumed that basic life support (BLS) would be initiated by a bystander or EMT, while the additional information was gathered to make a decision whether to attempt resuscitation. The indicators were only meant to apply to adults with out-of-hospital nontraumatic cardiac arrest, and they did not include indicators referring to halting attempts at resuscitation based on whether a patient had return of spontaneous circulation.
An expert panel used a modified Delphi technique to identify evidence-based clinical indicators for attempting resuscitation, defined as rate- or incidence-based measures designed to assess the quality of a structure, process, or outcomes in health care (Mainz 2003). Elsewhere in the article, we replace the word indicators with standards. The expert panel, who were chosen for their expertise in either resuscitation or end-of-life care included three academic emergency physicians, two community emergency physicians, one paramedic, one nurse who trains paramedics, one palliative care physician/ethicist, and a chaplain. Two of the academic emergency physicians were also members of the Medical Council, an advisory group to the agency comprised of emergency physicians with an interest in EMS policy. The indicators that were rated both appropriate and feasible by the expert panel were subsequently submitted to the EMS Commission for inclusion in the new policy. Policy documents and communications regarding the translation of these standards into a revised policy were collected prospectively and read in their entirety by the principal investigator (CRG), with selected review by coauthors, and using an iterative process of review, re-review, and discussion.
Study Procedures
The University of California, Los Angeles (UCLA) Institutional Review Board approved all study procedures. The EMS-UCLA Collaborative was established in early 2006, at which time, a team of four health services researchers, including board-certified physicians in Emergency Medicine, Internal Medicine, and Hospice and Palliative Medicine, and two members of LAC EMS leadership, including the Medical Director and Director of the EMS QI Committee, met in person. Two paramedics, one of whom is also a fire chief, and a paramedic nurse educator also participated. At the first meeting, leaders from LAC EMS, including the two paramedics, proposed revising the current resuscitation policy in response to perceived overuse of field resuscitation attempts. The researchers and EMS leadership jointly guided the development of evidence-based clinical standards to translate them into new protocols for EMS personnel. An expert panel was conducted on June 12, 2006, using the UCLA/RAND Appropriateness Method to assess the appropriateness and feasibility of forgoing attempts at resuscitation for selected patients with cardiac arrest (Grudzen et al. 2007). Standards that were approved by the panel were then submitted to LAC EMS leadership and the EMS Commission in Fall 2006 for inclusion in a putative new policy. The description of stakeholder review, votes by indicator class, and revision of the resuscitation policy was accomplished by review of the above documents.
Results
Selection of Evidence-Based Clinical Standards for Inclusion in the New Policy
Of these 41 evidence-based clinical standards submitted to LAC EMS in Fall 2006, 22 would have resulted in changes to the current resuscitation policy. Over the subsequent 6 months, LAC EMS leadership translated the indicators into a revised draft policy document and then submitted it for review to the Medical Council and the EMS Commission. Both groups had veto power and could block translation and implementation of any one standard. Leadership within the LAC EMS Agency then revised the policy based on their feedback, and resubmitted it to the EMS Commission for final approval. Members of the Collaborative were present at all major meetings.
Ten of the 22 clinical standards that were submitted to LAC EMS were incorporated into the new policy (see Table 1). These included three standards that require paramedics to inquire about DNAR status (A.1, A.2, and D.1), three that concerned respecting both written and verbal DNAR requests (A.4–A.6), and 4 of the 16 standards (B.5–B.8) that were based on clinical characteristics.
Table 1.
Fate of Indicators That Passed Appropriateness and Feasibility and Would Change Policy
| Indicator Class and Number* | Appropriateness | Feasibility | EMS Commission | Medical Council | Policy Change |
|---|---|---|---|---|---|
| A. Patient preferences | (1–9) | (1–9) | A/R | A/R | Y/N |
| A.1. IF EMS is called to a cardiac arrest in the home, THEN while proceeding to resuscitation they must ask if there is an Advance Directive | 9 | 7 | A | A | Y |
| A.2. IF EMS is called to a cardiac arrest in a long-term skilled nursing facility THEN while proceeding to resuscitation they must ask if there is an Advance Directive or DNR order | 9 | 9 | A | A | Y |
| A.4. IF EMS is called to a cardiac arrest in a long-term skilled nursing facility and there is no DNAR order in the chart, but an Advance Directive indicates a desire to forgo resuscitation, THEN EMS should forgo resuscitation | 9 | 9 | A | A | Y |
| A.5. IF EMS is called to a cardiac arrest in a home and a written Advance Directive indicates a desire to forgo resuscitation, THEN EMS should forgo resuscitation | 9 | 8 | A | A | Y |
| A.6. IF EMS is called to a cardiac arrest in the home or a public place and the apparent surrogate decision maker verbally requests no resuscitation and there is no written Advance Directive or DNAR form, THEN EMS should forgo resuscitation | 7 | 7 | A | A | Y |
| B. Asystole | (1–9) | (1–9) | A/R | A/R | Y/N |
| B.1. IF initial rhythm is asystole and patient is known by apparent surrogate decision maker to have a terminal illness, THEN forgo resuscitation | 9 | 8 | R | A | N |
| B.3a. IF initial rhythm is asystole, patient has a witnessed cardiac arrest, and apparent surrogate decision maker states patient is 70–79 years old and is not a hypothermia or drowning victim, THEN forgo resuscitation | 8 | 8 | R | A | N |
| B.3b. IF initial rhythm is asystole, patient has an unwitnessed cardiac arrest, and apparent surrogate decision maker states patient is 70–79 years old and is not a hypothermia or drowning victim, THEN forgo resuscitation | 8 | 8 | R | A | N |
| B.4a. IF initial rhythm is asystole, patient has a witnessed cardiac arrest, and apparent surrogate decision maker states patient is older than 80 years and is not a hypothermia or drowning victim, THEN forgo resuscitation | 9 | 8 | R | A | N |
| B.4b. IF initial rhythm is asystole, patient has an unwitnessed cardiac arrest, and apparent surrogate decision maker states patient is older than 80 years and is not a hypothermia or drowning victim, THEN forgo resuscitation | 9 | 8 | R | A | N |
| B.5. IF initial rhythm is asystole and patient has a time from witnessed collapse to ACLS without CPR that is 10–15 minutes and is not a hypothermia or drowning victim, THEN forgo resuscitation | 9 | 8 | A | A | Y |
| B.6. IF initial rhythm is asystole and patient has a time from witnessed collapse to ACLS without CPR that exceeds15 minutes, and is not a hypothermia or drowning victim, THEN forgo resuscitation | 8 | 8 | A | A | Y |
| B.7. IF initial rhythm is asystole and patient has an unwitnessed arrest, no bystander CPR BLS-response time is 10–15 minutes, and is not a hypothermia or drowning victim, THEN forgo resuscitation | 9 | 8 | A | A | Y |
| B.8. IF initial rhythm is asystole and patient has an unwitnessed arrest, no bystander CPR, BLS-response time that exceeds 15 minutes, and is not a hypothermia or drowning victim, THEN forgo resuscitation | 9 | 8 | A | A | Y |
| B.9a. IF initial rhythm is asystole, patient has a witnessed cardiac arrest, is <65 years old, and a long-term skilled nursing facility resident, THEN forgo resuscitation | 8 | 8 | R | A | N |
| B.9b. IF initial rhythm is asystole, patient has an unwitnessed cardiac arrest, is <65 years old, and a long-term skilled nursing facility resident, THEN forgo resuscitation | 8 | 8 | R | A | N |
| B.10a. IF initial rhythm is asystole, patient has a witnessed cardiac arrest, is 65 years or older, and a long-term skilled nursing facility resident, THEN forgo resuscitation | 8 | 8 | R | A | N |
| B.10b. IF initial rhythm is asystole, patient has an unwitnessed cardiac arrest, is 65 years or older, and is a long-term skilled nursing facility resident, THEN forgo resuscitation | 9 | 9 | R | A | N |
| C. PEA | (1–9) | (1–9) | A/R | A/R | Y/N |
| C.1. IF initial rhythm is PEA and patient is known by surrogate decision maker to have terminal illness, THEN forgo resuscitation | 8 | 7 | R | R | N |
| C.4b. IF initial rhythm is PEA, patient has an unwitnessed cardiac arrest, apparent surrogate decision maker states patient is older than 80 years, and is not a hypothermia or drowning victim, THEN forgo resuscitation | 7 | 7 | R | R | N |
| C.8. IF initial rhythm is PEA and patient has an unwitnessed arrest, no bystander CPR, BLS-response time that exceeds 15 minutes, and is not a hypothermia or drowning victim, THEN forgo resuscitation | 8 | 7 | A | R | N |
| D. Additional indicators† | |||||
| D.1. IF EMS is called to a cardiac arrest in the home, THEN while proceeding to resuscitation they must ask if there is a Prehospital DNAR | 9 | 8 | A | A | Y |
Notes.
Numbering corresponds to our original numbering system in prior publications that included all indicators.
Those added during the expert panel.
A, accepted; ACLS, advanced cardiac life support; BLS, basic life support; CPR, cardiopulmonary resuscitation; DNAR, do not attempt resuscitate; DNR, do not resuscitate; EMS, Emergency Medical Services; N, no; PEA, pulseless electrical activity; R, rejected; Y, yes.
All six standards that asked about (A.1, A.2, and D.1) or required following (A.4–A.6) written and verbal DNAR requests passed EMS Commission and Medical Council review. The standards that asked about and required following written DNAR requests were approved unanimously.
The agency implemented 4 of the 16 standards based on patient characteristics. The EMS Commission vetoed using terminal illness (B.1 and C.1), age (B.3a–B.4b and C.4b), or residence in a nursing home (B.9a–B.10b) as a reason to forgo a resuscitation attempt. These standards represented 11 of the 12 that were deemed appropriate and feasible by the expert panel, but they were not included in the new policy. The three standards concerning pulseless electrical activity, including one that was approved by the EMS Commission (C.8), were rejected by the Medical Council.
Translation of the Selected Standards to Policy
Leadership within LAC EMS then revised and rewrote the policy based on this feedback, which was submitted for final approval by the EMS Commission. The prehospital resuscitation policy was rewritten to include three new elements: the principles guiding the policy change, important definitions, such as advance health care directive (AHCD), and the circumstances under which a paramedic can forgo an attempt at resuscitation.
Guiding principles were explicitly stated on the first page of the new policy and included the following statements: (1) “Resuscitative efforts are of no benefit to patients whose physical condition precludes any possibility of successful resuscitation”; (2) “If there is any objection or disagreement by family members or prehospital personnel regarding terminating or withholding resuscitation, BLS resuscitation, including defibrillation, should continue or begin immediately, and paramedics should contact the base hospital for further directions.”
A list of the circumstances under which paramedics can forgo an attempt at resuscitation for adults included the following: (1) a valid DNAR; (2) a valid AHCD with one of the following present at scene: (a) an AHCD with written DNAR instructions, or (b) the agent identified in the AHCD requesting no resuscitation; (3) immediate family member present at scene: (a) with a Living Will or DPAHC on scene requesting no resuscitation, or (b) without said documents at scene, with full agreement of others if present, requesting no resuscitation; or (4) patient in asystole without cardiopulmonary resuscitation (CPR), and the estimated time from collapse to bystander CPR or EMS initiating BLS measures is greater than 10 minutes.
Stakeholder review recommended that documentation include “the name of the agent identified in the AHCD or immediate family member who made the decision to withhold or withdraw resuscitative measures, along with their signature on the EMS report form.” The following statement was also added in response to concern about family members at the scene: “prehospital personnel should remain on scene until law enforcement arrives, during this time when appropriate, the provider should provide grief support to family member(s).”
Implementation
The new policy was approved in February 2007 and went into effect July 1, 2007, approximately 1 year after submission to LAC EMS. The major changes to the policy include asking family and nursing home staff about DNAR status, respecting a verbal request, and the use of certain limited clinical criteria under which there is no chance of survival. The policy change was disseminated to paramedics within the agency not only through a written update but also via a 15-minute video in which the principal investigator (CRG) clarified and explained the rationale for the policy changes. This video was shown to all EMS providers who work within LAC, and it served as the basis for a longer discussion by nurse educators on the new resuscitation policy.
Discussion
Within 1 year, working collaboratively with LAC EMS, we were able to change a resuscitation policy that had been in place for years within our county. Ten of the 22 standards that were submitted to LAC EMS, and would have changed current resuscitation practice, were incorporated into the new policy. All the standards that addressed the need to respect patient preferences and asked about or required following written and verbal DNAR requests passed the EMS Commission and Medical Council review. Approval of the verbal DNAR request was based on Orange County, California, and King County, Washington, having recently adopted a similar verbal DNAR policy (Feder et al. 2006), and communication with their leadership that it had been successful and well received by the community.
On the other hand, LAC EMS implemented only 4 of 16 standards based on clinical characteristics. The EMS Commission rejected the use of terminal illness, age, or residence in a nursing home as a reason to forgo resuscitation. The Medical Council rejected clinical standards in which patients have cardiac electrical activity, but no pulse, a rhythm that is not uniformly fatal. In the end, the new policy included about half of the evidence-based standards that would have changed the old LAC EMS policy, as well as additional elements recommended by stakeholders. Their review of the revised policy was essential not only because it illustrated how the public would perceive such a policy but also because it resulted in the addition of important elements the expert panel overlooked. For example, the addition of language that recommended having paramedics provide grief support to family members until law enforcement arrives was an essential recommendation.
The success of this project, and its rapid translation of evidence into policy in LAC, was due in large part to the partnership between the research team and leadership at LAC EMS. Using many of the principles of participatory research, the research team worked collaboratively with LAC EMS from the outset to single out a significant and solvable problem, identify a strategy to gather the best evidence on the topic, analyze results, and translate the results into policy (Israel 2005; Minkler and Wallerstein 2008). The entire group met in person three to four times a year, regularly updated one another on any new developments, and worked together at each step, whether it be research or policy related.
Utilizing a highly collaborative approach, we were able to bridge two disciplines with often opposing objectives. While publication and objectivity are paramount in the world of research, policy makers face different constraints. The need for re-election and domination of narrow interest groups are real threats to their longevity (Brownson et al. 2006; Jewell and Bero 2008). Also, representative policy making is a culturally informed process and, in some sense, reflects broader community values. This might help explain why community representatives rejected policy elements that refer directly to specific populations, such as the terminally ill, the elderly, and nursing home residents. Independence and personal choice are highly valued, making utilitarian policies for specific subgroups highly unpopular. The EMS Commission felt that these populations were too heterogeneous and that it would be inequitable to forgo a resuscitation attempt based on these factors.
There was also disagreement among the medical experts. Although the expert panelists deemed it appropriate to forgo attempts at resuscitation in selected patients with pulseless electrical activity, the Medical Council subsequently voted against forgoing resuscitation attempts in this category. They only considered the sometimes quite small possibility of survival, and they did not explicitly consider the potential harm to EMS, family, and the public, when they rejected these three standards. This may have been due to a differing implicit threshold in the way the experts sorted patients into the DNAR categories. While the expert panel was satisfied with some uncertainty in the outcome in the setting of a research exercise, and appropriately weighed the potential benefits and harms, the Medical Council was more risk averse in making policy that would affect actual patients.
A subsequent evaluation of the revised policy demonstrates that it was well received by the agency and that it significantly reduced resuscitation attempts. Paramedics embraced the new policy and view the ability to forgo resuscitation attempts in the field as empowering and do not believe it presents harm to patients or families under most circumstances (Grudzen et al. 2009). In addition, a chart review revealed that paramedics were more likely to forgo resuscitation attempts after the policy change (13.3 versus 8.5 percent, p < .01). After adjustment for potential confounders (patient demographics, clinical characteristics, and EMS factors), as well as exclusion of patients with signs of irreversible death, paramedics are still significantly more likely to forgo a resuscitation attempt, and less likely to attempt resuscitation, after the policy change (OR: 1.67 [95% CI: 1.07, 2.61], p = .024; Grudzen et al. 2010).
We describe a collaborative and participatory approach to translate a set of evidence-based clinical standards into a new resuscitation policy. Nurturing such collaborations requires an immense investment of time and energy, as well as a long-term commitment to the project and one another. Numerous obstacles exist to the more widespread adoption of such work. Institutions that employ researchers need to recognize and foster these efforts by developing incentives to promote such collaborations, especially if they intend to be remain relevant in the real world. Policy makers need to develop relationships with and utilize researchers to make better evidence-based decisions, while recognizing their constraints as well, namely the need to publish and receive individual recognition. While recognizing the skills and constraints of these two groups is critical to making better policy, bridging their two worlds is only useful if it benefits those who matter most: patients.
Conclusions
By working closely together, LAC EMS leadership and a health services research team were able to implement a revised resuscitation policy throughout a large EMS agency within 1 year of its creation.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was supported by the California Health Care Foundation and the Robert Wood Johnson Clinical Scholars Program.
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Anderson WG, Arnold RM, Angus DC, Bryce CL. “Posttraumatic Stress and Complicated Grief in Family Members of Patients in the Intensive Care Unit”. Journal of General Internal Medicine. 2008;23(11):1871–6. doi: 10.1007/s11606-008-0770-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, Annane D, Bleichner G, Bollaert PE, Darmon M, Fassier T, Galliot R, Garrouste-Orgeas M, Goulenok C, Goldgran-Toledano D, Hayon J, Jourdain M, Kaidomar M, Laplace C, Larche J, Liotier J, Papazian L, Poisson C, Reignier J, Saidi F, Schlemmer B. “Risk of Post-Traumatic Stress Symptoms in Family Members of Intensive Care Unit Patients”. American Journal of Respiratory and Critical Care Medicine. 2005;171(9):987–94. doi: 10.1164/rccm.200409-1295OC. [DOI] [PubMed] [Google Scholar]
- Brownson RC, Royer C, Ewing R, McBride TD. “Researchers and Policymakers: Travelers in Parallel Universes”. American Journal of Preventive Medicine. 2006;30(2):164–72. doi: 10.1016/j.amepre.2005.10.004. [DOI] [PubMed] [Google Scholar]
- Colby DC, Quinn BC, Williams CH, Bilheimer LT, Goodell S. “Research Glut and Information Famine: Making Research Evidence More Useful for Policymakers”. Health Affairs (Millwood) 2008;27(4):1177–82. doi: 10.1377/hlthaff.27.4.1177. [DOI] [PubMed] [Google Scholar]
- Ditto PH, Druley JA, Moore KA, Danks JH, Smucker WD. “Fates Worse Than Death: The Role of Valued Life Activities in Health-State Evaluations”. Health Psychology. 1996;15(5):332–43. doi: 10.1037/0278-6133.15.5.332. [DOI] [PubMed] [Google Scholar]
- Eckstein M, Stratton SJ, Chan LS. “Cardiac Arrest Resuscitation Evaluation in Los Angeles: CARE-LA”. Annals of Emergency Medicine. 2005;45(5):504–9. doi: 10.1016/j.annemergmed.2004.11.024. [DOI] [PubMed] [Google Scholar]
- Feder S, Matheny RL, Rea RS, Jr, Loveless TD. “Withholding Resuscitation: A New Approach to Prehospital End-of-Life Decisions”. Annals of Internal Medicine. 2006;144(9):634–40. doi: 10.7326/0003-4819-144-9-200605020-00006. [DOI] [PubMed] [Google Scholar]
- Grudzen CR, Liddicoat R, Hoffman JR, Koenig W, Lorenz KA, Asch SM. “Developing Quality Indicators for the Appropriateness of Resuscitation in Prehospital Atraumatic Cardiac Arrest”. Prehospital Emergency Care. 2007;11(4):434–42. doi: 10.1080/10903120701536925. [DOI] [PubMed] [Google Scholar]
- Grudzen CR, Timmermans S, Koenig WJ, Torres JM, Hoffman JR, Lorenz KA, Asch SM. “Paramedic and Emergency Medical Technicians Views on Opportunities and Challenges When Forgoing and Halting Resuscitation in the Field”. Academic Emergency Medicine. 2009;16(6):532–8. doi: 10.1111/j.1553-2712.2009.00427.x. [DOI] [PubMed] [Google Scholar]
- Grudzen CR, Hoffman JR, Koenig WJ, Boscardin J, Lorenz KA, Asch SM. “The LA Story: What Happened after a New Policy Allowing Paramedics to Forgo Resuscitation Attempts in Prehospital Cardiac Arrest”. Resuscitation. 2010;81(6):685–90. doi: 10.1016/j.resuscitation.2010.02.011. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (U.S.). Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C: National Academy Press; 2001. [Google Scholar]
- Israel BA. Methods in Community-Based Participatory Research for Health. San Francisco, CA: Jossey-Bass; 2005. [Google Scholar]
- Jewell CJ, Bero LA. “‘Developing Good Taste in Evidence’: Facilitators of and Hindrances to Evidence-Informed Health Policymaking in State Government”. Milbank Quarterly. 2008;86(2):177–208. doi: 10.1111/j.1468-0009.2008.00519.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones L, Wells K. “Strategies for Academic and Clinician Engagement in Community-Participatory Partnered Research”. JAMA. 2007;297(4):407–10. doi: 10.1001/jama.297.4.407. [DOI] [PubMed] [Google Scholar]
- Jones C, Skirrow P, Griffiths RD, Humphris G, Ingleby S, Eddleston J, Waldmann C, Gager M. “Post-Traumatic Stress Disorder-Related Symptoms in Relatives of Patients Following Intensive Care”. Intensive Care Medicine. 2004;30(3):456–60. doi: 10.1007/s00134-003-2149-5. [DOI] [PubMed] [Google Scholar]
- Mainz J. “Defining and Classifying Clinical Indicators for Quality Improvement”. International Journal for Quality in Health Care. 2003;15(6):523–30. doi: 10.1093/intqhc/mzg081. [DOI] [PubMed] [Google Scholar]
- Meltzer LS, Huckabay LM. “Critical Care Nurses’ Perceptions of Futile Care and Its Effect on Burnout”. American Journal of Critical Care. 2004;13(3):202–8. [PubMed] [Google Scholar]
- Minkler M, Wallerstein N. Community-Based Participatory Research for Health: From Process to Outcomes. San Francisco: Jossey-Bass; 2008. [Google Scholar]
- Mobley MJ, Rady MY, Verheijde JL, Patel B, Larson JS. “The Relationship between Moral Distress and Perception of Futile Care in the Critical Care Unit”. Intensive & Critical Care Nursing. 2007;23(5):256–63. doi: 10.1016/j.iccn.2007.03.011. [DOI] [PubMed] [Google Scholar]
- Sorian R, Baugh T. “Power of Information: Closing the Gap between Research and Policy”. Health Affairs (Millwood) 2002;21(2):264–73. doi: 10.1377/hlthaff.21.2.264. [DOI] [PubMed] [Google Scholar]
- Zive D, Koprowicz K, Schmidt T, Stiell I, Sears G, Van Ottingham L, Idris A, Stephens S, Daya M. “Variation in Out-of-Hospital Cardiac Arrest Resuscitation and Transport Practices in the Resuscitation Outcomes Consortium: ROC Epistry-Cardiac Arrest”. Resuscitation. 2011;82(3):277–84. doi: 10.1016/j.resuscitation.2010.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


