Abstract
Objective
To investigate the relationship between Medicaid Personal Care Services (PCS) and caregivers' reports of activity (activities of daily living [ADL]) limitations for children with chronic health problems.
Data Sources/Study Setting
Primary data collected in 2008 and 2009. A state Medicaid program was the setting. The focus was children receiving Medicaid PCS.
Data Collection
Medicaid case managers assessed children to determine their need for PCS, using information provided by the child or informal caregivers. Two thousand seven hundred assessments were provided to researchers directly from case managers.
Principal Findings
Medical conditions and impairments explained 58 percent of the variance in the child's activity limitations. Activity limitations and problem behaviors explained 28 percent of the variance in PCS hours authorized. Which case manager completed the assessment also played a substantial role in determining hours of care.
Conclusions
Caregivers' reports of the severity of a child's activity limitations effectively summarize the effects of conditions and impairments on the child's ADL performance and have a significant impact on the level of services provided. Assessors often respond differently to children's characteristics and circumstances as they move from assessment to decisions concerning care provision. Our results imply that the provision of appropriate services may be enhanced when both case managers and caregivers play an active role in decisions concerning care provision.
Keywords: Medicaid personal care services, EPSDT, CSHCN, child and adolescent health, caregivers
An estimated 12.8 million children in the United States need “health and related services of a type or amount beyond that required by children generally” (McPherson et al. 1998; van Dyck et al. 2004). These children are disproportionately represented in public assistance programs; poor and disadvantaged, often lacking access to routine and family-centered health care (Newacheck et al. 1998; Mayer, Cockrell Skinner, and Slifkin 2004; Strickland et al. 2004). Those with greater functional limitations often have worse access to care (van Dyck et al. 2004).
Total annual health care expenditures for children with chronic illnesses or special health care needs (SHCN) are significantly higher than are those attributable to children without these conditions (Newacheck and Kim 2005). They are more likely than non-SHCN children to spend days in the hospital, visit an emergency room, have surgical procedures, and have visits with medical specialists (Newacheck, Inkelas, and Kim 2004; Boulet, Boyle, and Schieve 2009).
Family members usually provide the majority of care, assistance, and coordination of services for all children with special needs. A recent survey conducted by the National Alliance for Caregiving (2009) indicates that these caregivers spend an average of 29.7 hours per week helping with activities of daily living (ADLs) and other supportive activities, which limits their ability to earn income outside the home (van Dyck et al. 2004; Okumura et al. 2009). These issues are particularly pronounced for family or informal caregivers who are single parents (Rupp and Ressler 2009). Among all caregiver scenarios, families with children with SHCN experience the most adverse financial and medical effects of caregiving (Altman, Cooper, and Cunningham 1999).
The role of family caregivers across the life span has a long history as an important topic for researchers and policy makers (Levine et al. 2010). This interest in caregiving has involved a call for research on the population-based health outcomes of caregivers, the dynamics of caregiving across the life span, and the link of caregivers' health to the health and quality of life of care recipients. Talley and Crews (2007), in their discussion of caregiving and public health, indicate that informal caregiving is “… an enormous system of care in the United States and around the world.”
Unfortunately, little attention has focused on the collaborative element of home care involving the two systems that serve those receiving care in the community, the formal and the informal system. For those in the community with impairments or activity limitations, care often involves collaboration between formal (paid) health service providers and informal (unpaid) caregivers (Shewchuk and Elliott 2000; Carter 2008). An integral part of understanding how children with chronic health problems receive care in the community involves understanding how informal and formal care systems interact to structure the delivery of necessary formal health services.
In 2007, the Medicaid program supported medical care to almost 29 million children, and 19 cents of every Medicaid dollar went to pay for services to children (Kaiser Commission 2010). The vast majority of these expenditures were for standard medical services in families where informal caregiving was not an issue. However, a nontrivial portion of these Medicaid monies paid for home health services that complemented the efforts of unpaid caregivers helping children with SHCN living in low-income households.
In Texas, for example, in the state fiscal year beginning September 1, 2008 and ending August 31, 2009 (SFY 2009), only 0.24 percent of the children in the Medicaid program received Medicaid Personal Care Services (PCS) in their homes, but these same children accounted for 4.46 percent of total Medicaid (nonmanaged care) expenditures for children's health care. The average Medicaid expenditure for a child in Texas was U.S.$1,834 in SFY 2009. For children receiving PCS to supplement assistance provided by informal caregivers, the average annual Medicaid expenditure was U.S.$33,628.1 In SFY 2010, children in the PCS program increased to 0.31 percent of children receiving Medicaid and the cost of services increased by over U.S.$100 million to 6.03 percent of the Texas Medicaid Program's expenditures for children (Miller et al. 2011).
In the present study, we examined the degree to which the conditions, impairments, activity limitations, and problem behaviors of the child—as experienced and reported by the caregiver—were predictive of the amount of PCS authorized by Medicaid case managers. We also investigated the degree to which a case manager's discretion in translating a child's characteristics into a statement of need for care (hours) might account for unique variance in the hours authorized. The three specific research questions addressed were as follows:
What factors affected caregivers' reports of activity limitations requiring formal personal care assistance?
What impact did caregivers' input on activity (ADL) limitations have on decisions to provide Medicaid PCS resources?
How much variance in PCS hours was attributable to variation in indicators of children's status versus differences among case managers performing assessments?
METHODS
The Sample and Data Collection
Our target population was children ages 4–20 receiving PCS through the Medicaid PCS program. Children were eligible for the program if they had a condition that resulted in an activity, or ADL, limitation and the child's primary caregiver, usually a parent, was unable to provide the assistance needed by the child. The total population of children receiving Medicaid PCS included approximately 5,750 of the 2.4 million children receiving services supported by Medicaid in Texas SFY 2009. This number grew by almost 44 percent to just over 8,250 by SFY 2010.
Data were collected over a 6-month period by Medicaid case managers in each of Texas' 11 Health Regions.2 The data came from assessments conducted by the case managers during the course of their regular duties related to determining the need for PCS assistance for children in the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) Program. A total of 2,842 assessments were completed and transmitted to the research team; however, 83 assessments were not included in the analyses because of high levels of missing data or because no PCS hours were allocated to the children assessed (resulting in a final sample size of 2,759).
The training of case managers, typically master's-trained social workers (MSW), on the use of the assessment tool was 20 hours in duration. It included a detailed consideration of items, use of the instrument in example scenarios, and a group debriefing after case managers scored these scenarios. During data collection, research staff monitored assessments and provided feedback to case managers when coding errors or other problems were discovered.
Measures
The Personal Care Assessment Form for children 4–20 years of age (PCAF)3 was the assessment tool used in this effort. It was purpose built by the authors for the Texas Health and Human Services Commission (HHSC). The PCAF was based largely on variants of items included in the Minimum Data Set (MDS) for Nursing Home Resident Assessment (Hawes et al. 1997), developed for the Centers for Medicare, and Medicaid Services, or the Minimum Data Set for Home Care (MDS-HC©) developed by interRAI (Morris et al. 1997).4
Both the MDS and the MDS-HC© were developed for use with frail elderly and have proven reliability and validity when used with older populations (Morris et al. 1990, 1996; Hawes et al. 1995). The development of the PCAF required the addition of items specific to the needs of children and a reformulation of other items so they applied to the EPSDT population. All information about a child's health status used in this research came from caregiver/child reports recorded by a case manager or from a case manager's unstructured observations of the child during the assessment process. Children who were old enough to provide information elaborated on their caregivers' responses.
The dependent variable in our analyses was the number of PCS hours authorized for a child by a case manager. Case managers completed a 7-day 24-hour flow sheet that identified the PCS hours needed by a child, based on information obtained during the assessment with the PCAF.
Our major independent variable was a scale reflecting the intensity of a child's activity limitations (i.e., need for ADL assistance). The PCAF included 10 ADLs: bed mobility, positioning, eating, transfers, locomotion inside the dwelling, locomotion outside the dwelling, toilet use, dressing, personal hygiene, and bathing. All items referenced ADL performance over a 7-day period. All ADL items used a response set that ranged from total independence (0) to total dependence (5).
In addition, respondents were asked, for each ADL, if any limitation in the child's ability to perform the activity was affected by the child's conditions or impairments. If the performance of an ADL was not affected, then the child was considered independent for the purposes of PCS allocation for that ADL. A 4-year-old is not expected to be independent in dressing. If the level of assistance provided to a 4-year-old was not affected by the child's conditions or impairments, then the 4-year-old was coded as independent in dressing. The caregiver provided only the assistance one would expect to provide a 4-year-old. However, dressing the child might have required more intense assistance, taken longer, or required two people because of the child's medical conditions or impairments. If that was the case, then the child received the code for the level of assistance provided (e.g., limited assistance, regular hands-on help, etc.). This allowed the research team to distinguish between limitations resulting from the child's age or developmental stage and limitations resulting from conditions or impairments. An additive scale was constructed based on the 10 ADL items; this scale displayed excellent internal consistency (α = 0.93).
Following the World Health Organization's (WHO) International Classification of Function, Disability, and Health (ICF) model, diagnoses were identified as “conditions” (e.g., cerebral palsy, epilepsy, asthma). Problems that might be associated with one or more conditions (e.g., shortness of breath, paralysis, amputation) were considered as “impairments” (World Health Organization 2001). A dichotomous measure of the presence of a condition that significantly affected the care time awarded was constructed (0=none of these conditions diagnosed; 1=one or more of these conditions diagnosed) using 10 conditions: cerebral palsy, congenital heart disorder, cystic fibrosis, epilepsy/chronic seizure disorder, macro/microcephaly, muscular dystrophy, any paralysis, spinal cord dysfunction, substance abuse-related problems at birth, and traumatic brain injury. All of these conditions exhibited low prevalence. If they had been modeled as separate items, rather than as a group, their prevalence would have made it difficult for the individual items to achieve statistical significance. Because a small number of children presented with more than one of these conditions, the variable was constructed to indicate the presence or absence of any condition.
Similarly, a dichotomous measure indicating the presence of any of four impairments was included in the model. These impairments, which may have been caused by a number of different conditions, significantly affected the amount of formal care authorized. The dichotomous measure included impairments: bed-bound/chair-fast, contractures, other limitations in range of motion, and recurrent aspirations. These impairments were combined into a single, dichotomous measure because each condition alone exhibited low prevalence.
Impairments with relatively high prevalence were included in the model as individual items. A dichotomous measure of intellectual disability (ID) was used (0=no ID diagnosis; 1=ID diagnosis). Separately, a measure of cognitive impairment was developed by summing six items: short-term memory, long-term memory, procedural memory, daily decision making, making oneself understood, and the ability to understand others (α = 0.85). A dichotomous measure of two-person assistance with any ADL limitation was constructed (0=no two-person assistance; 1=any two-person assistance with an ADL). Incontinence was represented by a dichotomous item (0=continent; 1=any incontinence of bowel or bladder).
Age was calculated in years using the assessment date and child's date of birth for use in subsequent analyses. All children were Medicaid recipients living in low-income households. No other information on socioeconomic status was available.
Another scale was created from items concerning problematic behaviors in which children often engage to express fears, anxiety, or needs. Problem behaviors can affect caregivers' perceptions of children's needs. Externalizing behaviors such as aggression or resisting care may make children with special needs more difficult care recipients (Fournier et al. 2010a). Although behavioral problems are often overlooked in studies of children of SCHN, over half the children in the Texas PCS program had a co-occurring medical and behavioral/psychiatric condition (Fournier et al. 2010b). Our “externalizing” behavior scale was created by summing items identified as externalizing behaviors (e.g., verbally abusive, bullying/menacing behavior, injury to animals, etc.); these 13 items displayed good internal consistency (α = 0.83). Previous research also indicates that these behaviors act as mediators between limitations and hours of care (Fournier et al. 2010a).
Finally, the analyses included a dichotomous measure of caregiver physical limitations (0=no physical limitations; 1=unable to assist child because of physical limitations). Table 1 lists the variables included in our analyses and the coding strategy for each variable.
Table 1.
Measures Used in the Analyses (All Data Derived from the PCAF)
| Child Characteristics | Coding |
|---|---|
| Gender | Male=0 |
| Female=1 | |
| Medical conditions | No special medical conditions=0 |
| ≥1 special medical conditions=1 | |
| Health impairments | No special health impairments=0 |
| ≥1 special health impairments=1 | |
| Intellectual disability (ID) diagnosis | No ID diagnosed=0 |
| ID diagnosed=1 | |
| Two-person assistance with ADLs | No two-person assistance=0 |
| Any two-person assistance=1 | |
| Urinary or bowel incontinence | Continent=0 |
| Any incontinence=1 | |
| Caregiver limitations | No physical limitations=0 |
| Physical limitations=1 | |
| Case manager ID | Dummy variables for each case manager with more than one assessment. All those with one assessment became the reference category. |
| Continuous variables | |
| PCS hours authorized | Continuous variable |
| Activity (ADL) limitations | Continuous variable (higher scores mean more highly impaired) |
| Cognitive skills scale | Continuous variable (higher scores mean more highly impaired) |
| Externalizing behaviors | Continuous variable (higher score mean more problem behaviors) |
| Age | Continuous variable |
Note. ADL, activities of daily living; PCF, Personal Care Assessment Form.
Analysis Strategy
The conceptual model underlying our analyses is the model offered by the WHO in its ICF framework and supported by previous research in this field (World Health Organization 2001; Simeonsson et al. 2003; Lollar and Simeonsson 2005; Fournier et al. 2010a). In this use of that model, conditions refer to specific disease diagnoses (e.g., cystic fibrosis). Health problems that may result from a variety of conditions (e.g., being bedfast, incontinence) are considered impairments. Limitations are problems that the children experienced in performing the ADLs.
We use structural equation modeling (SEM) to estimate the effects of conditions, impairments, and limitations on the hours of personal care hours authorized by Medicaid case managers for children with chronic health conditions. The SEM models were developed using maximum likelihood (ML) estimation in IBM® SPSS®Amos 18 (software designed to perform SEM). To test the model fit of our a priori model, four fit indices were used: (a) chi-squared test of model fit (χ2), (b) comparative fit index (CFI), (c) Tucker–Lewis Index (TLI), and (d) root mean squared error of approximation (RMSEA). The RMSEA was used as a measure of absolute fit, and the CFI and TLI were used to measure incremental fit. We considered the model fit adequately when CFI and TLI values were above 0.90, and good fit was indicated if these indicators were above 0.95; for the RMSEA, scores below 0.08 typically indicate adequate fit, and scores below 0.05 indicate good fit. (Browne and Cudeck 1993; Hu and Bentler 1995).
“How much variance in PCS hours was attributable to variation in indicators of children's status versus differences among case managers performing assessments?” was our third research issue. We used an approach much different than SEM to investigate this issue. To determine the degree to which individual child characteristics and differences among case managers explained the variance in hours authorized, we fit a multilevel model to our data. Multilevel models allow one to analyze variation arising from data captured at different level of aggregation (Kreft and de Leeuw 1998). Level 1 in our model was composed of children's characteristics. Level 2 was the identity of the case manager completing the assessment. The data were analyzed using models with varying intercepts and with varying slopes. The results of these two analyses did not differ significantly. The aspect of the model on which we focused was the amount of the total variance explained by each level in the analysis. The results discussed were calculated using a varying intercepts model.
RESULTS
Table 2 presents descriptive data for 2,759 children receiving PCS during the study period. Fifty-eight percent of the children were female. A majority of the children (56 percent) had a condition with a significant effect on the care time awarded, while 41 percent had an impairment that had a significant effect on the number of PCS hours authorized. Almost half had an identified intellectual disability. The mean level of ADL impairment was 24.9 on a scale ranging from 0 to 50 (SD=15.34). A majority (70 percent) were incontinent, while 20 percent needed two-person assistance with some ADL. About half (49 percent) of caregivers reported that their physical limitations restricted the amount of care they could provide. On average, case managers authorized 25.4 (SD=14.81) hours of formal PCS care per child per week.
Table 2.
Descriptive Data for the Sample of Children Receiving Personal Care Services (PCS) (n = 2,759)
| Child Characteristics | Response | Frequency | Percentage* |
|---|---|---|---|
| Gender | Male | 1,154 | 42.3 |
| Female | 1,577 | 57.7 | |
| Medical conditions | No special medical conditions | 1,220 | 44.2 |
| One or more special medical conditions | 1,539 | 55.8 | |
| Health impairments | No special health impairments | 1,640 | 59.4 |
| One or more special health impairments | 1,119 | 40.6 | |
| Intellectual disability (ID) diagnosis | No ID diagnosed | 1,423 | 51.6 |
| ID diagnosed | 1,336 | 48.4 | |
| Two-person assistance with ADLs | No two-person assistance received | 2,208 | 80.2 |
| Any two-person assistance received | 545 | 19.8 | |
| Urinary or bowel incontinence | Continent | 816 | 29.6 |
| Any incontinence | 1,939 | 70.4 | |
| Caregiver limitations | No physical limitations | 1,215 | 51.0 |
| Physical limitations | 1,167 | 49.0 |
| Continuous Variables | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| PCS hours authorized | 25.4 | 14.81 | 1.25 | 105 |
| Activity (ADL) limitations | 24.9 | 15.34 | 0 | 50 |
| Cognitive skills scale | 7.1 | 3.69 | 0 | 12 |
| Externalizing behaviors | 3.8 | 4.73 | 0 | 24 |
| Age | 12.1 | 4.93 | 4 | 20 |
Percentages for each variable are based on nonmissing cases.
The a priori SEM model for the analysis is presented in Figure 1. The a priori model implies that the presence of one or more special conditions, the presence of one or more impairments, the presence of an intellectual disability, the presence of cognitive difficulties, the need for two-person ADL assistance, and incontinence will have a direct effect on activity limitations. It implies that activity limitations have a direct effect on the number of hours authorized, and an indirect effect mediated by externalizing behaviors. We also hypothesized that age and caregiver limitations would independently affect PCS hours. The a priori model is based on relatively similar work on a much smaller database (Fournier et al. 2010a).
Figure 1.
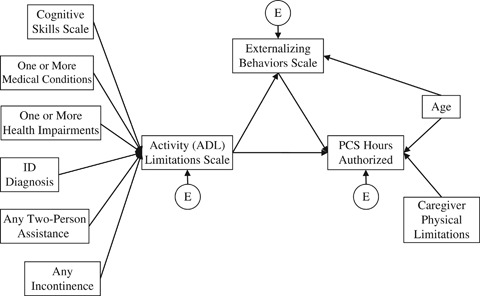
A Priori Structural Equation Model for Caregiver Reports and PCS Hours Authorizations
Note. Es are Associated Errors.
The a priori model exhibited poor model fit across the various fit indices (χ2[44, n = 2,759]=2,799.022, p<.001; CFI=0.562; TLI=0.343; RMSEA=0.151). Modification indices were examined, and they suggested a number of relationships required to fit the model to the data. These changes were determined to be theoretically justifiable and included in the corrected, best-fit model in Figure 2. Figure 2 is structured to provide a simple and readable model presentation. However, full path and covariance statistics are available from the first author. χ2 test of model fit for this corrected model was statistically significant, indicating that the model did not fit the data perfectly, (χ2[25, n = 2,759]=152.357, p<.001). However, this test is especially sensitive to sample sizes, and this rejection of model fit was expected (Hu and Bentler 1995). The CFI, TLI, and RMSEA fit indices were 0.98, 0.947, and 0.043, respectively. Based on these results we determined that the model had good fit, which allowed for interpretation of the path coefficients.
Figure 2.
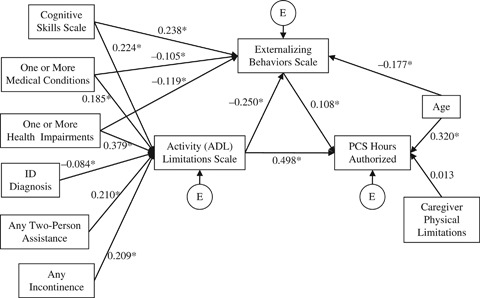
Corrected, Best-Fit Structural Equation Model for Caregiver Reports and PCS Hours Authorizations
Notes. Standardized Coefficients are presented. Es are Associated Errors. *p<0.05. Health Conditions: 0=No health conditions, 1=1 or more health conditions; Health Impairments: 0=No special health impairments, 1=1 or more health impairments; Intellectual Disability (ID) Diagnosis: 0=No I.D. diagnosed, 1=I.D. diagnosed; Two-person assistance with ADLs: 0=No two-person assistance=0, 1=Any two-person assistance; Urinary or Bowel Incontinence: 0=Continent, 1=Any incontinence; Caregiver Physical Limitations: 0=No physical limitations, 1=Physical limitations; PCS Hours Authorized: Continuous variable; Activity (ADL) Limitation Scale: Continuous variable (higher scores mean more highly impaired); Cognitive Skills Scale: Continuous variable (higher scores mean more highly impaired); Externalizing Behaviors Scale: Continuous variable (higher score mean more problem behaviors); Age: Continuous variable.
The first of our research questions was, “What factors affected caregivers' reports of activity (ADL) limitations requiring formal personal care assistance?” Figure 2 provides considerable insight into this issue. The caregivers' reports of a child's functional status are affected by medical conditions, health impairments, intellectual disabilities, cognitive skills, need for two-person assistance, and incontinence. These significant relationships accounted for 58 percent of the variance in the level of reported ADL impairment (R2=0.579). The relationships suggest that higher levels of activity limitations resulted from the presence of one or more special medical conditions (B = 0.185), the presence of one or more important health impairments (B = 0.379), poorer cognitive skills (B = 0.224), the need for two-person assistance (B = 0.210), and incontinence (B = 0.209). The presence of an intellectual disability (B=−0.084) had a small but significant negative effect on ADLs.
Our second research issue was, “What impact did caregivers' input on activity limitations have on decisions to provide Medicaid PCS resources?” The results in Figure 2 also support the assumption that the number of authorized PCS hours for a child is significantly affected by caregiver reports of a child's level of ADL impairment, age, and externalizing behaviors. These significant relationships accounted for 29 percent of the variance in the number of authorized PCS hours (R2=0.294). A greater number of PCS hours were requested for children with more severe ADL impairment (B = 0.498), those exhibiting more externalizing behaviors (B = 0.108), and those who were older (B = 0.320). However, the model indicated that caregiver limitations were not significantly linked to the number of hours authorized (B = 0.013, p > .05).
In addition, greater activity limitations were predictive of fewer externalizing behaviors (B=−0.250). The presence of one or more special medical conditions (B=−0.105), one or more impairments (B=−0.119), and greater age (B=−0.177) reduced externalizing behavior. However, poorer cognitive function was positively correlated with higher levels of these behaviors (B = 0.238). These significant relationships accounted for 20 percent of the variance in what we have identified as externalizing behaviors (R2=0.200).
“How much variance in PCS hours was attributable to variation in indicators of children's status versus differences among case managers performing assessments?” was our third research question. To investigate this issue, we estimated a multilevel model (Kreft and de Leeuw 1998; Rabe-Hesketh and Skrondal 2008). Multilevel models allow one to analyze variation arising from data captured at different levels of aggregation. In this analysis, the level-1 data on children's characteristics are nested within level-2 data on the identity of the case manager performing the assessment. The results of the multilevel models were calculated using a varying-intercepts model. A varying-intercepts model adjusts for the number of PCS hours being systematically higher or lower for some case managers (Rabe-Hesketh and Skrondal 2008).
Our focus was exploring the percentage of total variance attributed to each level in the model. We first analyzed a null model without covariates (e.g., children's characteristics) in the first level. The null model indicated the need for a multilevel design by showing significant level-2 variation in the allocation of PCS hours across case managers. Then, considering the explained variance for each level separately, case manager identity (level-2) explained 22 percent of the total variance. Children's characteristics explained 27 percent of the total variance (Snijders and Bosker 1999; Rabe-Hesketh and Skrondal 2008).5
DISCUSSION
The needs of individuals with chronic health problems who receive care in community settings are almost always met through a combination of formal and informal care processes. For health services researchers, how these processes interact in the allocation of public resources is an important issue. We investigated this interaction or collaboration in the context of the provision of PCS for children in Medicaid's EPSDT Program. Meeting the care needs of those children with serious chronic conditions who live in the community in low-income households involves collaboration between the child's network of informal, or unpaid support, and representatives of the Medicaid program. How that collaboration operates in practice has largely been unexplored. This research sheds some light on three related issues.
What factors affected caregivers' reports of activity limitations requiring formal personal care assistance?
As previous research indicates, caregivers' reports of a child's activity limitations can be well summarized in a single scale reflecting the intensity of the child's activity limitations (Phillips et al., in press). Such a scale, as our results demonstrate, constitutes a good summary of the burden on activities that the child's conditions or impairments create. The child's medical conditions, behavioral or psychological impairments, and other health problems significantly affected the scale summarizing her or his activity limitations, explaining over half the variance in the scale.
The presence of ID indirectly leads to fewer hours. This result may largely stem from the research team's lack of information on the severity of the ID diagnosis. Previous research on children receiving PCS indicates that those with severe ID do receive more hours of care. But the simple presence of an ID diagnosis has no such effect (Fournier et al. 2010a). The second somewhat surprising finding was the lack of a significant relationship between hours and the presence of a physical limitation for the caregiver. This finding may reflect the fact that for the child to be included in the population, the caregiver was required to have some type of limitation in their ability to assist the child.
What impact did caregivers' input on activity (ADL) limitations have on decisions to provide Medicaid PCS resources?
Caregiver reports of activity limitations and externalizing behaviors have substantial effects on case managers' decisions on the allocation of PCS hours, accounting for 29 percent of the variance. This level of explained variance is very similar to that seen in service provision to the frail elderly in community settings. The model used in research on formal home care costs for Michigan elders explained 26 percent of the variance in home care costs (Bjorkgren, Fries, and Shugarman 2000). A model using only cognition and ADL limitations explained 29 percent of the variance in PCS allocated to a group of frail older persons in Texas (Phillips et al. 2008). In a study of hours of home care for older persons in 11 countries, the average R2 was 0.22 (Carpenter et al. 2004). Future gains in explanatory power may result when researchers use a more extensive array of caregiver characteristics and the characteristics of the household environment than were available in these data.
How much variance in PCS hours was attributable to variation in indicators of children's status versus differences among case managers performing assessments?
The discretion available to individual case managers involved in the EPSDT program is quite important in the allocation of PCS resources. The results of the multilevel model indicated that children's characteristics were the most important factor in determining personal care hours. However, the multilevel models also indicated that case managers often translated assessment results into personal care hours in very different ways. These results indicate that the authorization of PCS for children facing chronic conditions and living in low-income households was a collaborative process.
The results return one to the reality noted at the outset of the paper. Good care for individuals with chronic conditions or impairments who live at home requires collaboration, or a partnership, between formal and informal caregivers. The intimate knowledge of an individual's care needs available to informal caregivers must be effectively communicated (via appropriate assessment) to the formal caregiver. The formal caregiver, or program representative, must translate this knowledge into a policy decision concerning the allocation of program resources.
The results also bring a serious policy question into focus. How much variation in service allocation should be driven by differences among case managers in the ways in which they interpret assessment information, or how far they reach outside the assessment tool for information, to determine the correct course of action? Home environments vary widely, and no standardized assessment tool will ever capture all the nuances of household and child circumstances one finds in a home care population. Discretion or clinical judgment by program staff must identify and respond to those nuances.
At the same time, unrestrained discretion related only to the characteristics of the case manager, and not the child's needs, might seriously affect a program's efforts to provide equitable, efficient, and effective services. When two very similar children assessed by different program staff receive different levels of services, then program resources may not be equitably distributed. One of those program participants may be receiving more resources than necessary, which will adversely affect program efficiency. Alternatively, one participant may be receiving fewer resources than needed, which adversely affects the participant and undercuts any program effectiveness.
This research can provide no resolution to the issue of what amount of discretion should be available to such decision makers. This is an issue in all care provision settings, though especially in home care settings. These results indicate that variations related to who assesses a child are not a trivial matter in the EPSDT program. They also indicate that caregiver's reports about the activity limitations of the children for whom they care are, as one would hope, largely driven by the child's conditions and impairments, and that program staff use caregiver reports to assist in their determinations of a child's care needs.
This study has several limitations. The sample represented one group of children in one state at one point in time. Whether our model applies to other settings, other groups, or other health services will only become apparent with further investigation. Our models are a combination, as are all models, of estimations and assumptions. We made what, based on previous research, we believe to be reasonable assumptions and have drawn what we consider reasonable conclusions from these analyses. Only further research on the important relationship between formal and informal caregivers and on the care of vulnerable populations such as children with SHCN will allow these assumptions and conclusions to be evaluated in different contexts.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The PCAF instruments were developed with commentary and review from a wide range of individuals involved in advocating for or providing services to children in Texas. The authors, however, would like to give special acknowledgement to Marianna Zolondek, Ryan Keyser, and Billy Millwee of the Texas Health and Human Services Commission for their support and leadership in this effort to assure that children in the Medicaid program receive the services they require. We thank our colleagues at interRAI for permission to use parts of the interRAI suite of instruments to develop an assessment tailored to understanding the needs and strengths of children. The authors assume full responsibility for all aspects of this work. It does not necessarily reflect the policies or opinions of any supporting organization or individuals.
NOTES
Excludes Medicaid Managed Care enrollees.
Nine of the 11 state health regions provided data from September 2008 through February 2009. Implementation was delayed in two regions because of the demands placed on HHSC staff by hurricane damage. These regions supplied data from December 2008 through March 2009.
Copies of the PCAF instruments, discussion of the project, and previous research can be found on the Internet.
InterRAI is an international organization of health professionals in over 30 countries dedicated to the development of assessment instruments for vulnerable populations around the world. Governmental agencies, researchers, and health care providers are allowed, under agreement with interRAI, free use of all assessment and treatment planning material developed by interRAI. More information is available at http://www.interRAI.org.
Additional analyses using HLM indicated that the nesting did not affect our SEM results.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Altman B, Cooper P, Cunningham P. “The Case of Disability in the Family: Impact on Health Care Utilization and Expenditures for Nondisabled Members”. Milbank Quarterly. 1999;77(1):39–75. doi: 10.1111/1468-0009.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjorkgren M, Fries B, Shugarman L. “A RUG-III Case-mix System for Home Care”. Canadian Journal on Aging. 2000;19:106–25. [Google Scholar]
- Boulet S, Boyle C, Schieve L. “Health Care Use and Health and Functional Impact of Developmental Disabilities among US Children, 1997–2005”. Archives of Pediatrics and Adolescent Medicine. 2009;163(1):19–26. doi: 10.1001/archpediatrics.2008.506. [DOI] [PubMed] [Google Scholar]
- Browne M, Cudeck R. “Alternative Ways of Assessing Model Fit.”. In: Bollen KA, Long SJ, editors. Testing Structural Equation Models. Newbury Park, CA: Sage Publications Inc; 1993. pp. 136–62. [Google Scholar]
- Carpenter I, Gambassi G, Topinkova E, Shroll M, Finne-Soveri H, Henrar J, Garms-Homolova V, Jonsson P, Frijters D, Ljunggren G, Sorbye LW, Wagner C, Onder G, Pedone C, Bernabei R. “Community Care in Europe. The Aged in HOme Care Project (AdHOC)”. Aging Clinical and Experimental Research. 2004;16:259–69. doi: 10.1007/BF03324550. [DOI] [PubMed] [Google Scholar]
- Carter R. “Addressing the Caregiver Crisis”. Preventing Chronic Disease. 2008;5(1):1–2. http://www.cdc.gov/issues/2008/jan/07_0162.htm. [PMC free article] [PubMed] [Google Scholar]
- Fournier CJ, Davis M, Patnaik A, Elliott TR, Dyer JA, Jasek E, Phillips CD. “Modeling Caregivers' Perceptions of Children's Need for Formal Care: Physical Function, Intellectual Disability Level, and Behavior”. Disability and Health Journal. 2010a;3:213–21. doi: 10.1016/j.dhjo.2009.10.005. [DOI] [PubMed] [Google Scholar]
- Fournier CJ, Elliott TR, Patnaik A, Dyer JA, Naiser E, Hawes C, Phillips CD. “Children with Special Health Care Needs Living in the Community: Personal Care Services and Psychological Issues”. Texas Psychologist. 2010b;60(2):4–6. [Google Scholar]
- Hawes C, Morris J, Phillips C, Fries B, Murphy K, Mor V. “Development of the Nursing Home Resident Assessment Instrument in the USA”. Age and Ageing. 1997;26(suppl 2):19–25. doi: 10.1093/ageing/26.suppl_2.19. [DOI] [PubMed] [Google Scholar]
- Hawes C, Morris J, Phillips C, Mor V, Fries B, Nonemaker S. “Reliability Estimates for the Minimum Data Set for Nursing Home Resident Assessment and Care Screening (MDS)”. The Gerontologist. 1995;35(2):172–78. doi: 10.1093/geront/35.2.172. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler P. “Evaluating Model Fit.”. In: Hoyle RH, editor. Structural Equation Modeling: Concepts, Issues, and Applications. Thousand Oaks, CA: Sage Publications Inc; 1995. pp. 76–99. [Google Scholar]
- Kaiser Commission. Medicaid and the Uninsured: Health Coverage of Children: The Role of Medicaid and CHIP. Washington, DC: Kaiser Commission; 2010. [Google Scholar]
- Kreft I, de Leeuw J. Introducing Multilevel Modeling. Thousand Oaks, CA: Sage Publications Inc; 2002. [Google Scholar]
- Levine C, Halper D, Peist A, Gould DA. “Bridging Troubled Waters: Family Caregivers, Transitions, and Long-term Care”. Health Affairs. 2010;29(1):116–24. doi: 10.1377/hlthaff.2009.0520. [DOI] [PubMed] [Google Scholar]
- Lollar DJ, Simeonsson R. “Diagnosis to Function: Classification for Children and Youths”. Journal of Developmental and Behavioral Pediatrics. 2005;26(4):323–30. doi: 10.1097/00004703-200508000-00012. [DOI] [PubMed] [Google Scholar]
- Mayer M, Cockrell Skinner A, Slifkin R. “Unmet Need for Routine and Specialty Care: Data from the National Survey of Children with Special Health Care Needs”. Pediatrics. 2004;113(2):e109–15. doi: 10.1542/peds.113.2.e109. [DOI] [PubMed] [Google Scholar]
- McPherson M, Arango P, Fox H, Lauver C, McManus M, Newacheck P, Perrin J, Shonkoff J, Strickland B. “A New Definition of Children with Special Health Care Needs”. Pediatrics. 1998;102(1):137–39. doi: 10.1542/peds.102.1.137. [DOI] [PubMed] [Google Scholar]
- Miller TR, Phillips CD, Patnaik A, Dyer J, Fournier C, Elliott T, Naiser E. Medicaid Expenditures for Children in Texas Receiving Medicaid Personal Services, September 2008–August 2010. College Station: Texas A&M Health Science Center; 2011. [Google Scholar]
- Morris J, Fries B, Carpenter G, Bernabei R. “The RAI-HC Assessment Tool: An International Reliability Trial”. The Gerontologist. 1996;36(suppl 1):291. [Google Scholar]
- Morris J, Fries B, Steel K, Ikegami N, Bernabei R, Carpenter G, Gilgen R, Hirdes J, Topinková E. “Comprehensive Clinical Assessment in Community Setting: Applicability of the MDS-HC”. Journal of the American Geriatrics Society. 1997;45(8):1017–24. doi: 10.1111/j.1532-5415.1997.tb02975.x. [DOI] [PubMed] [Google Scholar]
- Morris J, Hawes C, Fries B, Phillips C, Mor V, Katz S, Murphy K, Drugovich M, Friedlob A. “Designing the National Resident Assessment Instrument for Nursing Homes”. The Gerontologist. 1990;30(3):293–307. doi: 10.1093/geront/30.3.293. [DOI] [PubMed] [Google Scholar]
- National Alliance for Caregiving. Caregivers of Children: A Focused Look at Those Caring for a Child with Special Needs under the Age of 18. Bethesda, MD: The MetLife Foundation; 2009. [Google Scholar]
- Newacheck P, Inkelas M, Kim S. “Health Services Use and Health Care Expenditures for Children with Disabilities”. Pediatrics. 2004;114(1):79–85. doi: 10.1542/peds.114.1.79. [DOI] [PubMed] [Google Scholar]
- Newacheck P, Kim S. “A National Profile of Health Care Utilization and Expenditures for Children with Special Health Care Needs”. Archives of Pediatrics and Adolescent Medicine. 2005;159(1):10–17. doi: 10.1001/archpedi.159.1.10. [DOI] [PubMed] [Google Scholar]
- Newacheck P, Strickland B, Shonkoff J, Perrin J, McPherson M, McManus M, Lauver C, Fox H, Arango P. “An Epidemiologic Profile of Children with Special Health Care Needs”. Pediatrics. 1998;102(1):117–23. doi: 10.1542/peds.102.1.117. [DOI] [PubMed] [Google Scholar]
- Okumura MD, Van Cleave J, Gnanasekaran S, Houtrow A. “Understanding Factors Associated with Work Loss for Families Caring for CSHCN”. Pediatrics. 2009;124:S392–98. doi: 10.1542/peds.2009-1255J. [DOI] [PubMed] [Google Scholar]
- Phillips C, Dyer J, Janousek V, Halperin L, Hawes C. “Providing Appropriate Services to Individuals in the Community: A Preliminary Case-mix Model for Allocating Personal Care Services”. Journal of Health and Human Services Administration. 2008;30(4):378–401. [PubMed] [Google Scholar]
- Phillips CD, Patnaik A, Dyer JA, Naiser E, Hawes C, Fournier CJ, Elliott TR. “Reliability and the Measurement of Actvity Limitations (ADLs) for Children with Special Health Care Needs (CSHCN) Living in the Community. Disability and Rehabilitation. doi: 10.3109/09638288.2011.555596. in press. [DOI] [PubMed] [Google Scholar]
- Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using Stata. College Station, TX: Stata Press; 2008. [Google Scholar]
- Rupp K, Ressler S. “Family Caregiving and Employment among Parents of Children with Disabilities on SSI”. Journal of Vocational Rehabilitation. 2009;30(3):153–75. [Google Scholar]
- Shewchuk R, Elliott TR. “Family Caregiving in Chronic Disease and Disability: Implications for Rehabilitation Psychology.”. In: Frank RG, Elliott TR, editors. Handbook of Rehabilitation Psychology. Washington, DC: American Psychological Association Press; 2000. pp. 553–63. [Google Scholar]
- Simeonsson R, Leonardi M, Lollar D, Bjorck-Akesson E, Hollenweger J, Martinuzzi A. “Applying the International Classification of Functioning, Disability and Health (ICF) to Measure Childhood Disability”. Disability and Rehabilitation. 2003;25(11):602–10. doi: 10.1080/0963828031000137117. [DOI] [PubMed] [Google Scholar]
- Snijders TA, Bosker R. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. Thousand Oaks, CA: Sage Publications Inc; 1999. [Google Scholar]
- Strickland B, McPherson M, Weissman G, Dyck P, Huang Z, Newacheck P. “Access to the Medical Home: Results of the National Survey of Children with Special Health Care Needs”. Pediatrics. 2004;113(5):1485–92. [PubMed] [Google Scholar]
- Talley R, Crews J. “Framing the Public Health of Caregiving”. American Journal of Public Health. 2007;97(2):224–28. doi: 10.2105/AJPH.2004.059337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Dyck P, Kogan M, McPherson M, Weissman G, Newacheck P. “Prevalence and Characteristics of Children with Special Health Care Needs”. Archives of Pediatrics and Adolescent Medicine. 2004;158(9):884–90. doi: 10.1001/archpedi.158.9.884. [DOI] [PubMed] [Google Scholar]
- World Health Organization. 2001. “International Classification of Functioning, Disability and Health (ICF)” [accessed on February 8, 2011]. Available at http://www.who.int/classifications/icf/en/index.html.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


